-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaProspects for passive immunity to prevent HIV infection
In a Perspective, Lynn Morris and Nonhlanhla Mkhize discuss the prospects for broadly neutralizing antibodies to be used in preventing HIV infection.
Published in the journal: . PLoS Med 14(11): e32767. doi:10.1371/journal.pmed.1002436
Category: Perspective
doi: https://doi.org/10.1371/journal.pmed.1002436Summary
In a Perspective, Lynn Morris and Nonhlanhla Mkhize discuss the prospects for broadly neutralizing antibodies to be used in preventing HIV infection.
The need for better HIV prevention tools
Despite the widespread global rollout of antiretroviral therapy and its ability to reduce onward HIV transmission, an alarming 1.8 million new HIV infections are estimated to have occurred in 2016 [1]. Effective methods to prevent HIV infection include condom use and pre-exposure prophylaxis (PrEP) with antiretroviral drugs; however, owing to barriers such as adherence, an effective vaccine would be the most definitive solution to the ongoing burden of HIV infection. Yet researchers have struggled to design a prophylactic vaccine able to induce protective immunity. This highlights the urgency of developing new tools to prevent HIV infections and achieve control of the global epidemic [2]. One such approach is passive immunization with protective antibodies, a strategy that has been used against infectious diseases for over 100 years and has proven useful for post-exposure prophylaxis or against pathogens where no vaccines yet exist [3]. The flourishing field of antibody therapeutics, together with the identification of a growing number of broad and potent HIV monoclonal antibodies, presents an extraordinary opportunity to use this approach for HIV prevention. The protective and therapeutic effects of a number of these broadly neutralizing antibodies (bNAbs) have been well demonstrated in animal studies [4]. Furthermore, bNAbs have been shown to have modest antiviral effects in HIV-infected humans, both in reducing viremia and delaying viral rebound after interruption of antiretroviral treatment [5–7]. What is not yet known is whether bNAbs are able to protect uninfected humans from acquiring HIV.
Ramping up to AMP
The first bNAb to be tested for efficacy in HIV prevention is VRC01, which was isolated in 2010 following the advent of single-cell technologies that enabled the discovery of a new generation of bNAbs. It targets the CD4 binding site (CD4bs) on the HIV envelope and neutralizes 90% of circulating HIV isolates [8]. VRC01 was shown to be safe and well tolerated in adults in 2 small clinical trials [9,10], as well as in infants in an ongoing phase 1 trial evaluating the potential for preventing mother-to-child transmission [11]. Importantly, VRC01 retains its functional activity following passive infusion with trough levels expected to neutralize the majority of circulating HIV strains [10].
VRC01 is now being tested in 2,700 high-risk homosexual men in the Americas and 1,500 heterosexual women in Africa in 2 separate Antibody Mediated Prevention (AMP) protocols [12]. In these trials, participants receive a total of 10 intravenous infusions of VRC01 once every 8 weeks at a higher (30 mg/kg) or lower (10 mg/kg) dose. Protective efficacy will be assessed by comparing the number of breakthrough HIV infections in the VRC01 groups to a placebo group, while the difference between the 2 dose groups will help to define a protective titer. As a further test of efficacy, viral sensitivity to VRC01 will be assessed in the laboratory. Since natural resistance to VRC01 exists, it will be important to establish whether breakthrough HIV infections are due to preexisting viral resistance or early adaptive escape from VRC01. The AMP proof-of-concept studies have been designed with the explicit purpose of testing whether a bNAb can prevent HIV infection, with results expected by 2020.
Improved bNAbs in the pipeline
In the past few years, a large number of broader and more potent bNAbs have been isolated, some of which are already in clinical development, including VRC07-523, a CD4bs antibody related to VRC01 [13]. This antibody has been further engineered to include mutations in the Fc region that enhance binding to the neonatal Fc receptor and extend its half-life by up to 6 months [14]. Antibodies targeting other epitopes on the HIV envelope are also being developed for clinical use, including PGT121 and 10–1074 that bind to the high-mannose patch near the V3 region of gp120, as well as the V2 apex antibodies PGDM1400 and CAP256-VRC26.25 that have shown promise in animal studies [15]. Other single antibodies, such as 10E8, that target the membrane proximal external region of gp41, as well as the more recently isolated CD4bs antibody N6, are able to neutralize 98% of global HIV isolates [16]. Bispecific neutralizing antibodies (biNAbs) that are designed to recognize 2 distinct epitopes combine the breadth and potency of the parental antibodies and in some cases have shown synergistic activity [17,18]. Those that target both viral and host cellular proteins, either CD4 or CCR5 viral receptors, have demonstrated dramatically increased potency, probably by pre-positioning the biNAb at the site of viral entry. A recent study of a trispecific antibody (VRC01/PGDM1400/10E8), which combines the breadth and potency of 3 antibodies into one molecule, demonstrated protection in non-human primates against a mixture of SHIVs that were differentially sensitive to the single antibodies [19]. However, while bi - and trispecific antibodies herald new possibilities for improved efficacy, artificial modifications could increase their antigenicity and negatively impact pharmacokinetic properties and safety profiles, but this remains to be tested.
Challenges of using bNAbs for prevention
Given that no single bNAb can neutralize 100% of viruses, the wisdom of using bNAbs for HIV prevention has been questioned. Added to this is the observation that global viruses exhibit a wide range of sensitivities to individual bNAbs, and neutralization escape from single antibodies can occur readily and rapidly. These concerns could be overcome by combining 3–4 bNAbs that together can cover 100% of viruses [20], although this will substantially increase the cost of the product. The cost of bNAbs is especially important in the era of relatively cheap antiretroviral drugs being used for PrEP to prevent HIV infection. However, drugs have significant side effects, and daily dosing demands high levels of adherence [21] although this concern may be circumvented if long-acting cabotegravir, also being tested on an 8-week dosing schedule, is shown to be efficacious. Nonetheless, antibodies with their excellent safety record and potentially longer half-life could fill a unique niche and increase the options available to those seeking to protect themselves from HIV infection. Furthermore, antibodies possess other functional activities mediated through their Fc regions, such as antibody-dependent cellular cytotoxicity and phagocytosis, that may contribute to protective efficacy [22]. Although the current modality of multiple intravenous infusions has not proven to be a barrier in the clinical experience with VRC01, it is unlikely to be feasible on a population level. Subcutaneous administration could make delivery of bNAbs more practical, but this is only possible with highly potent bNAbs, a property that can also be improved through antibody engineering. Other factors that may undermine the success of bNAbs is our incomplete understanding of mucosal transmission events and the ability of HIV to infect and spread through infected cells or via cell—cell transmission, where bNAbs may less effective [23].
The future of HIV prevention
The prospect for bNAbs becoming part of the toolbox for reducing new HIV infections will depend on the outcome of the AMP trials and on subsequent testing of broader and more potent bNAbs with longer half-lives as well as lower manufacturing costs. However, even assuming success in ongoing clinical evaluation, it is likely that bNAbs will only be used in selected population groups when they are most at risk, such as young women in Africa or individuals who suspect that they may become exposed to HIV. In this scenario, bNAb administrations every 4–6 months may be a feasible option for a defined time period, akin to the widespread use of medroxyprogesterone acetate for birth control.
Importantly, positive findings from the AMP trials would confirm antibody neutralization as a correlate of protective efficacy, which is critical information as this assumption underlies many HIV envelope immunogen design efforts. In addition, defining antibody levels in the blood and mucosal tissues able to confer protection against HIV infection will also be useful. Of course, this evidence comes with certain caveats because a vaccine would induce multiple antibody specificities, unlike VRC01 that targets a single neutralization-sensitive epitope, and furthermore, active immunization induces innate and adaptive T-cell responses that are not imparted by passive immunization. Nevertheless, minimal protective antibody titers determined in the AMP studies could be used as a benchmark to identify the most promising vaccine candidates at an early stage and thereby accelerate the vaccine discovery process.
The pace of progress in development of bNAbs so far, from the discovery of VRC01 to conducting the AMP efficacy trials, has been impressive. Results from this field hold promise not only for a new weapon in the fight against HIV (Fig 1) but also potentially may assist progress in the vaccine field. Contingent on further advances in scientific and clinical studies, the prospects for use of bNAbs as biological drugs for long-term PrEP represent an exciting and innovative approach to tackling the devastating global HIV epidemic. Vector-based delivery is also being explored for sustained production of protective levels of bNAbs [24]. As such, passive immunization could contribute to HIV prevention efforts until a safe and effective HIV vaccine is developed.
Fig. 1. Another possible weapon against HIV. 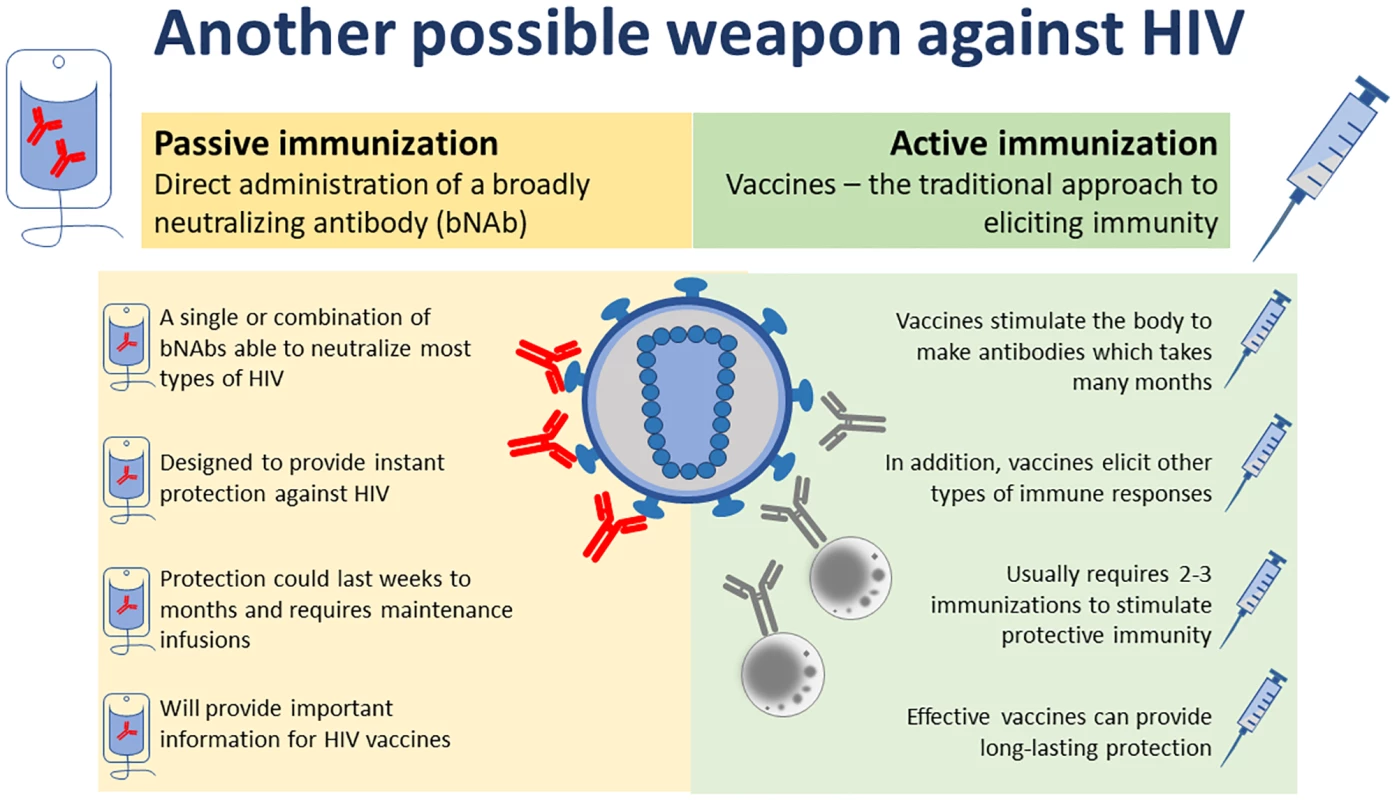
An illustration of the principles of using a monoclonal antibody as passive immunization to prevent HIV infection, as compared with the more traditional vaccine approach of active immunization. Created by Nolo Moima, Sunday Times, and Carina Kriel, NICD.
Zdroje
1. UNAIDS. Fact sheet—Latest statistics on the status of the AIDS epidemic. [cited 22 September 2017]. http://www.unaids.org/en/resources/fact-sheet
2. Corey L, Gray GE. Preventing acquisition of HIV is the only path to an AIDS-free generation. Proc Natl Acad Sci U S A. 2017;114(15):3798–800. doi: 10.1073/pnas.1703236114 28360202
3. Graham BS, Ambrosino DM. History of passive antibody administration for prevention and treatment of infectious diseases. Curr Opin HIV AIDS. 2015;10(3):129–34. doi: 10.1097/COH.0000000000000154 25760933
4. Pegu A, Hessell AJ, Mascola JR, Haigwood NL. Use of broadly neutralizing antibodies for HIV-1 prevention. Immunol Rev. 2017;275(1):296–312. doi: 10.1111/imr.12511 28133803
5. Bar KJ, Sneller MC, Harrison LJ, Justement JS, Overton ET, Petrone ME, et al. Effect of HIV Antibody VRC01 on Viral Rebound after Treatment Interruption. N Engl J Med. 2016;375(21):2037–50. doi: 10.1056/NEJMoa1608243 27959728
6. Caskey M, Klein F, Lorenzi JC, Seaman MS, West AP Jr, Buckley N, et al. Viraemia suppressed in HIV-1-infected humans by broadly neutralizing antibody 3BNC117. Nature. 2015;522(7557):487–91. doi: 10.1038/nature14411 25855300
7. Lynch RM, Boritz E, Coates EE, DeZure A, Madden P, Costner P, et al. Virologic effects of broadly neutralizing antibody VRC01 administration during chronic HIV-1 infection. Sci Transl Med. 2015;7(319):319ra206. doi: 10.1126/scitranslmed.aad5752 26702094
8. Wu X, Yang Z-Y, Li Y, Hogerkorp C-M, Schief WR, Seaman MS, et al. Rational Design of Envelope Identifies Broadly Neutralizing Human Monoclonal Antibodies to HIV-1. Science. 2010;329(5993):856–61. doi: 10.1126/science.1187659 20616233
9. Ledgerwood JE, Coates EE, Yamshchikov G, Saunders JG, Holman L, Enama ME, et al. Safety, pharmacokinetics and neutralization of the broadly neutralizing HIV-1 human monoclonal antibody VRC01 in healthy adults. Clin Exp Immunol. 2015;182(3):289–301. doi: 10.1111/cei.12692 26332605
10. Mayer KH, Seaton KE, Huang Y, Grunenberg N, Isaacs A, Allen M, et al. Safety, pharmacokinetics, and immunological activities of multiple intravenous or subcutaneous doses of an anti-HIV monoclonal antibody, VRC01, administered to HIV-uninfected adults: Results of a phase 1 randomized trial. PLoS Med. 2017;14(11):e1002435. https://doi.org/10.1371/journal.pmed.1002435
11. Coleen K, Cunningham EJM, Capparelli EV, Muresan P, Perlowski C, Valentine M, et al. Safety and pharmacokinetics of the monoclonal antibody, VRC01, in HIV-exposed newborns. Conference on Retroviruses and Opportunistic Infections (CROI). 2017. Poster P1112: http://impaactnetwork.org/publications/croi2017.html
12. The AMP HIV Prevention Study. [cited 22 September 2017]. https://ampstudy.org.za/
13. Rudicell RS, Kwon YD, Ko SY, Pegu A, Louder MK, Georgiev IS, et al. Enhanced potency of a broadly neutralizing HIV-1 antibody in vitro improves protection against lentiviral infection in vivo. J Virol. 2014;88(21):12669–82. doi: 10.1128/JVI.02213-14 25142607
14. Ko SY, Pegu A, Rudicell RS, Yang ZY, Joyce MG, Chen X, et al. Enhanced neonatal Fc receptor function improves protection against primate SHIV infection. Nature. 2014;514(7524):642–5. doi: 10.1038/nature13612 25119033
15. Julg B, Tartaglia LJ, Keele BF, Wagh K, Pegu A, Sok D, et al. Broadly neutralizing antibodies targeting the HIV-1 envelope V2 apex confer protection against a clade C SHIV challenge. Sci Transl Med. 2017;9(406):eaal1321. doi: 10.1126/scitranslmed.aal1321 28878010
16. Huang J, Kang BH, Ishida E, Zhou T, Griesman T, Sheng Z, et al. Identification of a CD4-Binding-Site Antibody to HIV that Evolved Near-Pan Neutralization Breadth. Immunity. 2016;45(5):1108–21. doi: 10.1016/j.immuni.2016.10.027 27851912
17. Bournazos S, Gazumyan A, Seaman MS, Nussenzweig MC, Ravetch JV. Bispecific Anti-HIV-1 Antibodies with Enhanced Breadth and Potency. Cell. 2016;165(7):1609–20. doi: 10.1016/j.cell.2016.04.050 27315478
18. Huang Y, Yu J, Lanzi A, Yao X, Andrews CD, Tsai L, et al. Engineered Bispecific Antibodies with Exquisite HIV-1-Neutralizing Activity. Cell. 2016;165(7):1621–31. doi: 10.1016/j.cell.2016.05.024 27315479
19. Xu L, Pegu A, Rao E, Doria-Rose N, Beninga J, McKee K, et al. Trispecific broadly neutralizing HIV antibodies mediate potent SHIV protection in macaques. Science. 2017;358 : 85–90. doi: 10.1126/science.aan8630 28931639
20. Wagh K, Bhattacharya T, Williamson C, Robles A, Bayne M, Garrity J, et al. Optimal Combinations of Broadly Neutralizing Antibodies for Prevention and Treatment of HIV-1 Clade C Infection. PLoS Pathog. 2016;12(3):e1005520. doi: 10.1371/journal.ppat.1005520 27028935
21. Hankins CA, Dybul MR. The promise of pre-exposure prophylaxis with antiretroviral drugs to prevent HIV transmission: a review. Current opinion in HIV and AIDS. 2013 Jan;8(1):50–8. doi: 10.1097/COH.0b013e32835b809d 23201856. Epub 2012/12/04. eng.
22. Hessell AJ, Hangartner L, Hunter M, Havenith CE, Beurskens FJ, Bakker JM, et al. Fc receptor but not complement binding is important in antibody protection against HIV. Nature. 2007;449(7158):101–4. doi: 10.1038/nature06106 17805298
23. Abela IA, Berlinger L, Schanz M, Reynell L, Gunthard HF, Rusert P, et al. Cell-cell transmission enables HIV-1 to evade inhibition by potent CD4bs directed antibodies. PLoS Pathog. 2012;8(4):e1002634. doi: 10.1371/journal.ppat.1002634 22496655
24. Brady JM, Baltimore D, Balazs AB. Antibody gene transfer with adeno-associated viral vectors as a method for HIV prevention. Immunol Rev. 2017;275(1):324–33. doi: 10.1111/imr.12478 28133808
Štítky
Interní lékařství
Článek Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort studyČlánek Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 11- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Ferinject: správně indikovat, správně podat, správně vykázat
- Optimální dávkování apixabanu v léčbě fibrilace síní
-
Všechny články tohoto čísla
- Labour trafficking: Challenges and opportunities from an occupational health perspective
- The end of HIV: Still a very long way to go, but progress continues
- Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort study
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
- Treatment guidelines and early loss from care for people living with HIV in Cape Town, South Africa: A retrospective cohort study
- Perinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study
- Core Outcome Set-STAndards for Development: The COS-STAD recommendations
- Closing the gaps in the HIV care continuum
- Association between the 2012 Health and Social Care Act and specialist visits and hospitalisations in England: A controlled interrupted time series analysis
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Sexual exploitation of unaccompanied migrant and refugee boys in Greece: Approaches to prevention
- Child sex trafficking in the United States: Challenges for the healthcare provider
- The expanding epidemic of HIV-1 in the Russian Federation
- Cardiovascular disease (CVD) and chronic kidney disease (CKD) event rates in HIV-positive persons at high predicted CVD and CKD risk: A prospective analysis of the D:A:D observational study
- Validity of a minimally invasive autopsy for cause of death determination in maternal deaths in Mozambique: An observational study
- malERA: An updated research agenda for malaria elimination and eradication
- malERA: An updated research agenda for health systems and policy research in malaria elimination and eradication
- A combination intervention strategy to improve linkage to and retention in HIV care following diagnosis in Mozambique: A cluster-randomized study
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- malERA: An updated research agenda for basic science and enabling technologies in malaria elimination and eradication
- Human trafficking and exploitation: A global health concern
- Virological response and resistance among HIV-infected children receiving long-term antiretroviral therapy without virological monitoring in Uganda and Zimbabwe: Observational analyses within the randomised ARROW trial
- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Lansoprazole use and tuberculosis incidence in the United Kingdom Clinical Practice Research Datalink: A population based cohort
- malERA: An updated research agenda for insecticide and drug resistance in malaria elimination and eradication
- Safety, pharmacokinetics, and immunological activities of multiple intravenous or subcutaneous doses of an anti-HIV monoclonal antibody, VRC01, administered to HIV-uninfected adults: Results of a phase 1 randomized trial
- HIV prevalence and behavioral and psychosocial factors among transgender women and cisgender men who have sex with men in 8 African countries: A cross-sectional analysis
- Treatment eligibility and retention in clinical HIV care: A regression discontinuity study in South Africa
- malERA: An updated research agenda for characterising the reservoir and measuring transmission in malaria elimination and eradication
- Effectiveness of a combination strategy for linkage and retention in adult HIV care in Swaziland: The Link4Health cluster randomized trial
- The value of confirmatory testing in early infant HIV diagnosis programmes in South Africa: A cost-effectiveness analysis
- HIV self-testing among female sex workers in Zambia: A cluster randomized controlled trial
- The US President's Malaria Initiative, transmission and mortality: A modelling study
- Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study
- Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: A cluster-randomized controlled health systems trial
- malERA: An updated research agenda for diagnostics, drugs, vaccines, and vector control in malaria elimination and eradication
- malERA: An updated research agenda for combination interventions and modelling in malaria elimination and eradication
- HIV-1 persistence following extremely early initiation of antiretroviral therapy (ART) during acute HIV-1 infection: An observational study
- Respondent-driven sampling for identification of HIV- and HCV-infected people who inject drugs and men who have sex with men in India: A cross-sectional, community-based analysis
- Extensive virologic and immunologic characterization in an HIV-infected individual following allogeneic stem cell transplant and analytic cessation of antiretroviral therapy: A case study
- Measuring success: The challenge of social protection in helping eliminate tuberculosis
- Prospects for passive immunity to prevent HIV infection
- Reaching global HIV/AIDS goals: What got us here, won't get us there
- Evidence-based restructuring of health and social care
- Extreme exploitation in Southeast Asia waters: Challenges in progressing towards universal health coverage for migrant workers
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Revma Focus: Spondyloartritidy
nový kurz
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



