-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Reaching global HIV/AIDS goals: What got us here, won't get us there
In a Perspective, Wafaa El-Sadr and colleagues discuss tailored approaches to treatment and prevention of HIV infection.
Published in the journal: . PLoS Med 14(11): e32767. doi:10.1371/journal.pmed.1002421
Category: Perspective
doi: https://doi.org/10.1371/journal.pmed.1002421Summary
In a Perspective, Wafaa El-Sadr and colleagues discuss tailored approaches to treatment and prevention of HIV infection.
Much accomplished, but much more needed
A decade ago, today’s progress towards confronting the global HIV epidemic would have been unimaginable. A remarkable global mobilization of resources through the United States President’s Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund for AIDS, Tuberculosis and Malaria, combined with the commitment of affected countries and communities, has enabled 19.5 million persons living with HIV (PLHIV) to access life-saving antiretroviral therapy (ART) [1]. This has resulted in decreasing HIV-related morbidity and mortality and contributed to a significant decline in the number of new infections [1].
Despite earlier concerns about the feasibility of scaling up HIV services in resource-limited settings, the majority of PLHIV accessing ART are in sub-Saharan Africa, where many countries have austere health systems characterized by scarce healthcare providers and weak laboratory, infrastructure, drug procurement, monitoring, and governance systems [2]. One of the critical enablers of this achievement was the adoption of the public health approach to HIV service delivery [2]. This strategy used simple evidence-based algorithms for HIV testing, prevention, and treatment; employed a single first-line antiretroviral regimen, standardized laboratory tests, and testing schedules; and involved streamlined data monitoring systems [3]. The simplicity and consistency of this approach enabled HIV services to be provided by nonphysician clinicians and facilitated the establishment of simplified laboratory and medication procurement systems, enabling the successful scale-up of treatment [3].
By facilitating the successful scale-up of HIV services, the public health approach is arguably “what got us here,” to a context in which more than half of all PLHIV are accessing treatment [1]. However, in order to reach ambitious global targets and achieve epidemic control, much more must be done—and swiftly. Not only must the number of PLHIV accessing ART increase substantially to reach 30 million people by 2020, but the quality of HIV services must be enhanced and effective primary prevention interventions must be brought to scale [1]. Challenges include reaching diverse patient populations, retaining them in either treatment or prevention programs, supporting adherence to ART and prevention methods, and addressing long wait times and health facility crowding, a problem for both recipients of care and health workers. In addition, concern over the plateauing of global resources highlights the vital importance of efficiency and cost-effectiveness as a possible way to address this enormous challenge [1].
Differentiated care for people living with HIV
Differentiated care may be an important step towards addressing health system and individual barriers to achieve HIV treatment goals [4]. Whereas earlier efforts, anchored in the public health approach, often distinguished only 2 groups of adult patients—pregnant and nonpregnant—differentiated care models tailor service frequency, service location, service intensity, and type of service provider for more categories of PLHIV [4]. The goal of differentiated care is to provide client-centered services that encourage engagement, adherence, and retention in care while also maximizing efficiency.
The most urgent need has been to develop models of care for PLHIV who are stable on ART, generally defined by high adherence, evidence of favorable immunological response, and/or virological suppression [5]. By their sheer numbers, such patients represent the vast majority of visits to health facilities and contribute the most to provider workload, despite the fact that they do not require frequent clinical assessment. Moreover, requiring stable patients to repeatedly return to health facilities overlooks their needs and priorities and may itself be a barrier to retention in care and adherence to treatment. Differentiated care for stable patients includes group models, such as facility-based adherence clubs and community-based antiretroviral groups, as well as individual models, such as facility-based fast-track appointments, increased visit spacing, and community-based ART pickup [6]. These approaches recognize that successful treatment of a chronic disease, such as HIV, depends on patient self-management, often enhanced by the support provided by families and communities [6].
There is also high interest in developing differentiated care for other groups of PLHIV including pregnant women, PLHIV with advanced HIV disease, adolescents, men, migrant and mobile populations, and key populations, such as men who have sex with men, sex workers, and people who inject drugs. Although these groups bear a disproportionate burden of HIV infections, many face structural and psychosocial barriers, such as stigma, discrimination, and insensitive providers, that stand in the way of achieving optimal access to and engagement with care [7]. Other groups of PLHIV face difficulties in remaining in care due to competing priorities. For example, while the scale-up of ART for pregnant HIV-positive women has been impressive, their retention in care, particularly postpartum, remains suboptimal [8]. In a cohort study conducted in Cape Town, postpartum HIV-positive women were offered the option of following up via a differentiated service delivery model (community adherence clubs) or at their primary care clinic [8]. The majority preferred the adherence club model, with encouraging short-term outcomes.
Differentiated approaches to prevention
Achieving epidemic control is also critically dependent on HIV prevention. Primary prevention of HIV acquisition is required in addition to optimizing the potential of HIV treatment as a prevention tool [1]. Between 21% and 96% of new HIV infections occur among key populations and their sexual partners [9], and the enormous structural and societal barriers described above affect access to prevention services as well as treatment. Interventions to engage key populations have been shown to alleviate some of these impediments. For example, a study conducted in Kenya showed that the use of sex worker peer educators led to an increase in safer sexual behaviors and noted that individuals who participated in more peer education sessions achieved higher levels of protection [10]. Another study, also conducted in Kenya, demonstrated the feasibility of training health workers to better understand the needs of men who have sex with men [11]. Despite these successes, novel and effective strategies remain urgently needed to decrease HIV incidence amongst key and priority populations, and engaging members of these communities in designing and testing primary prevention initiatives is a priority.
The way forward
As the expression goes, “What got us here won’t get us there.” Attaining epidemic control will require continued rapid expansion of the number of PLHIV on treatment, engaging populations at risk for HIV infection, improvement of the quality of HIV services, and new approaches to program design and implementation (Fig 1). The scale-up of differentiated care has the potential to relieve crowded health facilities and overworked providers by moving stable patients on ART to more patient-centered models, enhancing both efficiency and quality. Differentiated care can also facilitate the engagement of other groups of PLHIV in models of service provision that meet their specific clinical and psychosocial needs. At the same time, innovations are urgently needed in the development of differentiated prevention delivery models that address the needs of specific groups at substantial risk for HIV infection. In addition, it is now more important than ever to utilize population-based, programmatic, and research data in shaping programs and prioritizing populations [12]. For instance, disaggregation of seemingly favorable national population HIV data by sex and age shows important gaps in the HIV care and HIV prevention continua for men and youth living with HIV.
Fig. 1. Framework for achievement of HIV epidemic control. 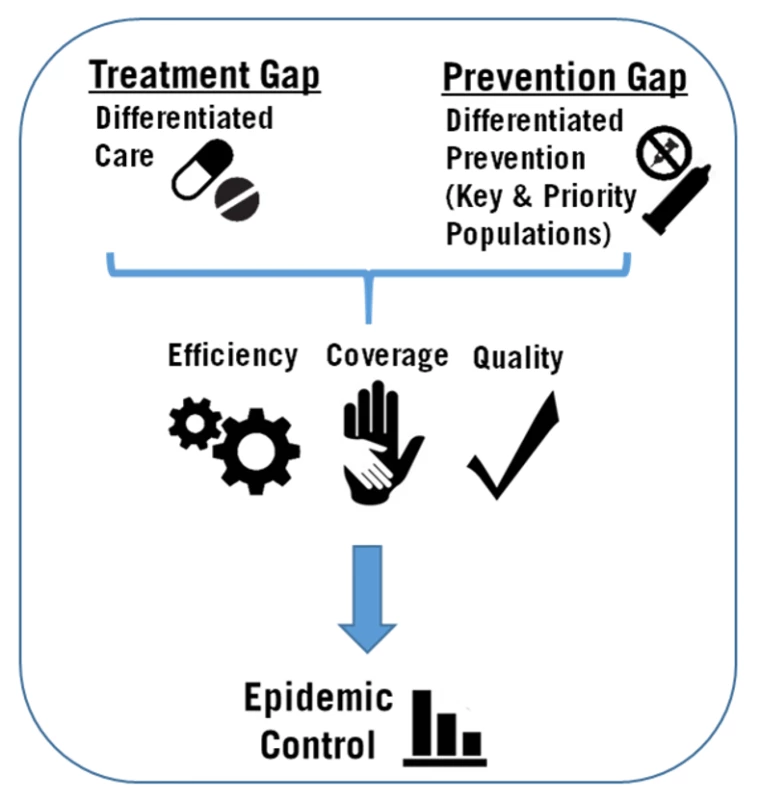
It is important to note that creating a multitude of service delivery models, some overly complicated, risks undermining the public health approach that has been so vital to the success of HIV programs. Abandoning the public health approach by “overdifferentiating” may be as problematic as a one-size-fits-all approach [2]. Caution is required to avoid service models that disrupt the simple, streamlined approaches to health worker training, procurement, laboratory systems, and monitoring and evaluation strategies that were so central to successful HIV program expansion. As differentiated service delivery models are taken to scale, it will be critically important to evaluate their effects on individual and programmatic outcomes, client satisfaction, health provider productivity and satisfaction, and laboratory, procurement, and monitoring systems—as well as on the affordability and cost-effectiveness of specific models of care and prevention. Fundamentally, the essence of the public health approach is that it is anchored in the realities of resource-constrained health systems. Designing, implementing, and scaling up new service models that are person centered and informed by data and evidence will enable the achievement of high coverage, quality, and efficiency—paving the way towards epidemic control.
Zdroje
1. UNAIDS. Ending AIDS: Progress Towards the 90-90-90 Targets. Geneva: 2017.
2. El-Sadr WM, Rabkin M, DeCock KM. Population health and individualized care in the global AIDS response: synergy or conflict? AIDS. 2016;30(14):2145–8. doi: 10.1097/QAD.0000000000001192 27367489
3. De Cock KM, El-Sadr WM, Ghebreyesus TA. Game changers: why did the scale-up of HIV treatment work despite weak health systems? J Acquir Immune Defic Syndr. 2011;57:S61–S3. doi: 10.1097/QAI.0b013e3182217f00 21857297
4. Grimsrud A, Bygrave H, Doherty M, Ehrenkranz P, Ellman T, Ferris R, et al. Reimagining HIV service delivery: the role of differentiated care from prevention to suppression. J Int AIDS Soc. 2016;19(1):21484. doi: 10.7448/IAS.19.1.21484 27914186
5. Waldrop G, Doherty M, Vitoria M, Ford N. Stable patients and patients with advanced disease: consensus definitions to support sustained scale up of antiretroviral therapy. Trop Med Int Health. 2016;21(9):1124–30. doi: 10.1111/tmi.12746 27371814
6. Bemelmans M, Baert S, Goemaere E, Wilkinson L, Vandendyck M, van Cutsem G, et al. Community-supported models of care for people on HIV treatment in sub-Saharan Africa. Trop Med Int Health. 2014;19(8):968–77. doi: 10.1111/tmi.12332 24889337
7. Macdonald V, Verster A, Baggaley R. A call for differentiated approaches to delivering HIV services to key populations. J Int AIDS Soc. 2017;20(Suppl 4):28–31.
8. Myer L, Iyun V, Zerbe A, Phillips TK, Brittain K, Mukonda E, et al. Differentiated models of care for postpartum women on antiretroviral therapy in Cape Town, South Africa: a cohort study. J Int AIDS Soc. 2017;20(Suppl 4):32–40.
9. UNAIDS. Global AIDS Update. Geneva. 2016.
10. Luchters S, Chersich MF, Rinyiru A, Barasa MS, King'ola N, Mandaliya K, et al. Impact of five years of peer-mediated interventions on sexual behavior and sexually transmitted infections among female sex workers in Mombasa, Kenya. BMC Public Health. 2008;8 : 143. doi: 10.1186/1471-2458-8-143 18445258
11. van der Elst EM, Smith AD, Gichuru E, Wahome E, Musyoki H, Muraguri N, et al. Men who have sex with men sensitivity training reduces homoprejudice and increases knowledge among Kenyan healthcare providers in coastal Kenya. J Int AIDS Soc. 2013;16(4Suppl 3):18748.
12. ICAP at Columbia University. Population HIV Impact Assessment (PHIA) 2017. Available from: http://phia.icap.columbia.edu/.
Štítky
Interní lékařství
Článek Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort studyČlánek Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2017 Číslo 11- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- Labour trafficking: Challenges and opportunities from an occupational health perspective
- The end of HIV: Still a very long way to go, but progress continues
- Contemporary disengagement from antiretroviral therapy in Khayelitsha, South Africa: A cohort study
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
- Treatment guidelines and early loss from care for people living with HIV in Cape Town, South Africa: A retrospective cohort study
- Perinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study
- Core Outcome Set-STAndards for Development: The COS-STAD recommendations
- Closing the gaps in the HIV care continuum
- Association between the 2012 Health and Social Care Act and specialist visits and hospitalisations in England: A controlled interrupted time series analysis
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Sexual exploitation of unaccompanied migrant and refugee boys in Greece: Approaches to prevention
- Child sex trafficking in the United States: Challenges for the healthcare provider
- The expanding epidemic of HIV-1 in the Russian Federation
- Cardiovascular disease (CVD) and chronic kidney disease (CKD) event rates in HIV-positive persons at high predicted CVD and CKD risk: A prospective analysis of the D:A:D observational study
- Validity of a minimally invasive autopsy for cause of death determination in maternal deaths in Mozambique: An observational study
- malERA: An updated research agenda for malaria elimination and eradication
- malERA: An updated research agenda for health systems and policy research in malaria elimination and eradication
- A combination intervention strategy to improve linkage to and retention in HIV care following diagnosis in Mozambique: A cluster-randomized study
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- malERA: An updated research agenda for basic science and enabling technologies in malaria elimination and eradication
- Human trafficking and exploitation: A global health concern
- Virological response and resistance among HIV-infected children receiving long-term antiretroviral therapy without virological monitoring in Uganda and Zimbabwe: Observational analyses within the randomised ARROW trial
- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Lansoprazole use and tuberculosis incidence in the United Kingdom Clinical Practice Research Datalink: A population based cohort
- malERA: An updated research agenda for insecticide and drug resistance in malaria elimination and eradication
- Safety, pharmacokinetics, and immunological activities of multiple intravenous or subcutaneous doses of an anti-HIV monoclonal antibody, VRC01, administered to HIV-uninfected adults: Results of a phase 1 randomized trial
- HIV prevalence and behavioral and psychosocial factors among transgender women and cisgender men who have sex with men in 8 African countries: A cross-sectional analysis
- Treatment eligibility and retention in clinical HIV care: A regression discontinuity study in South Africa
- malERA: An updated research agenda for characterising the reservoir and measuring transmission in malaria elimination and eradication
- Effectiveness of a combination strategy for linkage and retention in adult HIV care in Swaziland: The Link4Health cluster randomized trial
- The value of confirmatory testing in early infant HIV diagnosis programmes in South Africa: A cost-effectiveness analysis
- HIV self-testing among female sex workers in Zambia: A cluster randomized controlled trial
- The US President's Malaria Initiative, transmission and mortality: A modelling study
- Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study
- Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: A cluster-randomized controlled health systems trial
- malERA: An updated research agenda for diagnostics, drugs, vaccines, and vector control in malaria elimination and eradication
- malERA: An updated research agenda for combination interventions and modelling in malaria elimination and eradication
- HIV-1 persistence following extremely early initiation of antiretroviral therapy (ART) during acute HIV-1 infection: An observational study
- Respondent-driven sampling for identification of HIV- and HCV-infected people who inject drugs and men who have sex with men in India: A cross-sectional, community-based analysis
- Extensive virologic and immunologic characterization in an HIV-infected individual following allogeneic stem cell transplant and analytic cessation of antiretroviral therapy: A case study
- Measuring success: The challenge of social protection in helping eliminate tuberculosis
- Prospects for passive immunity to prevent HIV infection
- Reaching global HIV/AIDS goals: What got us here, won't get us there
- Evidence-based restructuring of health and social care
- Extreme exploitation in Southeast Asia waters: Challenges in progressing towards universal health coverage for migrant workers
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Postmenopausal hormone therapy and risk of stroke: A pooled analysis of data from population-based cohort studies
- Bioequivalence between innovator and generic tacrolimus in liver and kidney transplant recipients: A randomized, crossover clinical trial
- HIV pre-exposure prophylaxis and early antiretroviral treatment among female sex workers in South Africa: Results from a prospective observational demonstration project
- Bioequivalence of twice-daily oral tacrolimus in transplant recipients: More evidence for consensus?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



