-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
Authors: M. Veith; M. Penčák; A. Ernest; Z. Straňák
Authors place of work: Oftalmologická klinika FN Královské Vinohrady a 3. LF Univerzity Karlovy Praha, Šrobárova 50, 100 34, Praha 10, Přednosta: doc. MUDr. Pavel Studený, Ph. D., MHA
Published in the journal: Čes. a slov. Oftal., 75, 2019, No. 4, p. 182-187
Category: Původní práce
doi: https://doi.org/10.31348/2019/4/2Summary
Purpose: To evaluate the effect of one intravitreal injection of expansile gas in the treatment of vitreomacular traction (VMT).
Methods: A retrospective review of eyes with VMT treated with singl injection of 0,3 ml of 100% C3F8 gas was performed. The procedure was performed on an outpatient basis under topical anesthesia.
Results: Twelve consecutive patient (14 eyes) with symptomatic VMT underwent pneumatic vitreolysis. Mean extend of vitreomacular adhesion was 490,5 µm (408-751). A posterior vitreous detachment developed in 13 eyes (92,9 %) after a single gas injection, in 11 eyes (84,6 %) during the first month of follow-up, in 2 eyes within two month of injection. Mean baseline and last BCVA were 0,5 (0,16-0,18) and 0,67 (0,2-1,0) respectively (p < 0,001). Mean folow-up time was 5,8 (1-16) months. The procedure was also successful in two eyes, which where previously unsuccessfuly treated with ocriplasmin. One eye formed a macular hole. There were no other complication.
Conclucion: Intravitreal injection of C3F8 is an effective, safe and inexpensive therapy of vitreomacular traction.
Keywords:
posterior vitreous membrane – vitreomacular traction – intravitreal injection – perfluoropropane – C3F8
INTRODUCTION
Adhesion of the vitreous body to the retina is strongest in the macula, on the optic nerve disc, along the large vascular trunks and in the region of the vitreous base. Above all, vitreoretinal adhesion in the macula is of exceptional significance, because changes in this region may lead to a decrease of visual acuity (VA).
Ageing of the eye leads to liquefaction of the vitreous body and weakening of vitreoretinal adhesions, with a possible detachment of the posterior vitreous membrane (PVM) from the membrana limitans interna (MLI) (19, 2). Incomplete separation of the PVM in the macular landscape may lead to the development of vitreomacular traction (VMT; or symptomatic vitreomacular adhesion – VMA), idiopathic lamellar or complete macular hole (MH), cystoid macular edema (CME) or epiretinal membrane (ERM).
By disrupting the retinal architecture, vitreomacular traction may cause a decrease of visual acuity, metamorphopsia, micropsia or photopsia. Upon fresh identification of vitreomacular traction, observation is usually recommended. However, spontaneous release of traction occurs only rarely (7). If traction persists and the patient perceives damage to visual functions, nowadays we are able to offer a number of options for solution. Previously the only option for treatment was surgical intervention by means of pars plana vitrectomy (PPV). This provides a high success rate, but is linked with potential risks such as endophthalmitis, retinal crack or detachment and the development of cataract (11, 12, 13, 14). A newer option is pharmacological vitreolysis with the aid of ocriplasmin (Jetrea; TromboGenics NV, Leuven, Belgium). This concerns a recombinant enzyme with a proteolytic effect regarding protein components of the vitreous body and vitreoretinal interface (20). Ocriplasmin is determined for single-use intravitreal administration in a dose of 0.125 µg (0.1 ml of diluted solution).
Pneumatic vitreolysis is the term used to describe intravitreal application of expansive gas with the purpose of inducing release of the PVM (10). The precise mechanism of this induction by intravitreal injection of gas is unknown. It is assumed that the initial expansion and subsequent contraction of the gas bubble destabilises the vitreous gel. Movements of the bubble accelerate the process of liquefaction of the vitreous body, which is the fundamental prerequisite for the development of release of the PVM (8).
METHOD AND COHORT
In this study we retrospectively evaluate the results of treatment of patients with VMT, which consisted of expansive gas applied intravitreally. All the patients were examined on a slit lamp, including biomicroscopy of the posterior segment of the eye in artificial mydriasis. Intraocular pressure (IOP) was measured by a noncontact method. Best corrected visual acuity (BCVA) was measured with the aid of ETDRS optotypes. Diagnosis of VMT was confirmed with the aid of spectral domain optical coherence tomography (SD-OCT) (Spectralis OCT, Heidelberg Engineering, Heidelberg, Germany). We indicated symptomatic patients with a range of traction up to 1500 µm for application of the gas (also indication limitation of payment of ocriplasmin). In our evaluated cohort we included all patients who we had indicated for this treatment (including patients with diabetic retinopathy and patients following previous unsuccessful application of ocriplasmin).
We performed the procedure in outpatient care under topical anaesthesia (Benoxi 0.4%, Unimed Pharma) in an operating theatre with the aid of a surgical microscope. The surrounding area of the eye and the conjunctival sac was disinfected with 5% povidone-iodine solution, the operating field was covered with a sterile screen, and a speculum was applied. At the beginning of the procedure we performed paracentesis of the cornea and hypotoned the eye. Subsequently 0.3 ml of 100% perfluoropropane (C3F8) was applied to all the patients. The gas was applied intravitreally via the pars plana in the lower temporal quadrant 3.5 mm from the limbus with the aid of a 30-gauge needle. Perfusion of the central retinal artery was subsequently checked, and according to requirement we again performed further discharge of the intraocular fluid from the anterior chamber via the paracentesis. After completing the procedure the patient remained in a prone position for 10 minutes, and then in a supine position for further 10 minutes. The patient was administered 1 tablet of Diluran (Zentiva) after he procedure as prevention against elevation of IOP. The patient was subsequently discharged from the centre with an appointment for a follow-up examination, without special regime measures and without local antibiotic or anti-inflammatory treatment.
In this cohort always only one injection of gas into the evaluated eye was applied in all patients.
At the follow-ups, the same examinations were performed as at the indication visit, the first examination with OCT was performed within one month of the procedure, and we indicated further follow-ups individually according to the current finding.
We primarily evaluate the success rate of release of VMT on SD-OCT, and further also change of visual acuity and the incidence of complications.
The observed cohort consists of 14 eyes of 12 patients (8 women, 4 men) with an average age of 72.2 years (65-82). The average observation period is 5.8 months (1-16). The average width of vitreoretinal adhesion was 490.5 µm (408-751). Two eyes had previously been treated unsuccessfully with ocriplasmin. 11 eyes were phakic, 3 pseudophakic, two patients underwent the procedure on both eyes with an interval between treatments (detailed data and results are presented in table 1). A paired t-test for dependent samples was used for statistical evaluation of changes of BCVA.
Tab. 1. Characteristics of cohort and results 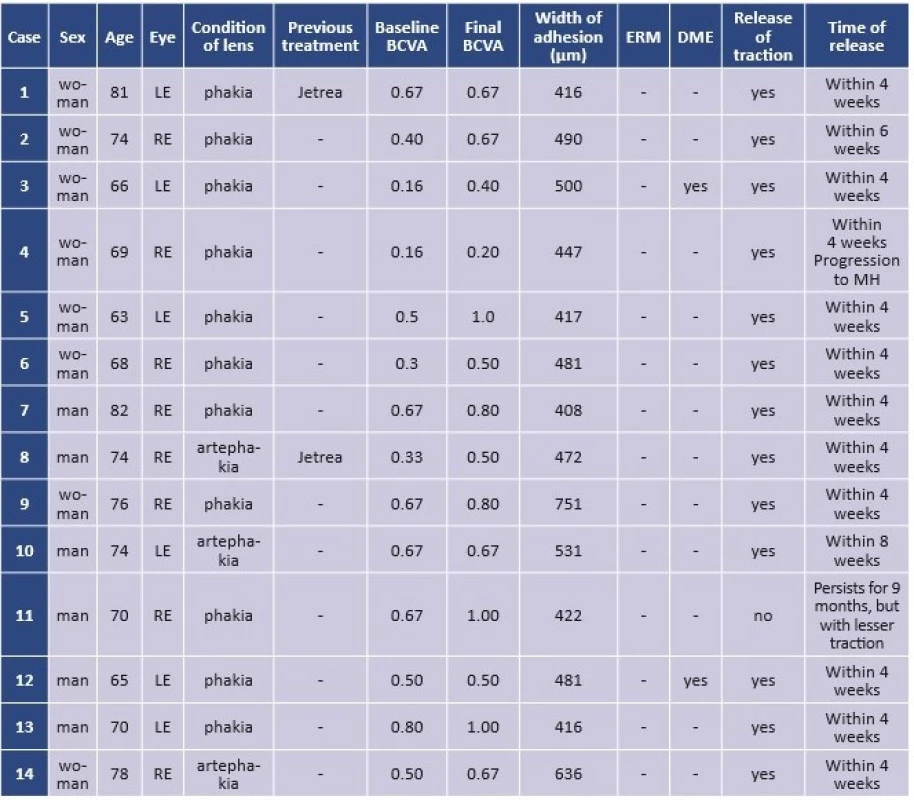
BCVA – best corrected visual acuity; ERM – epiretinal membrane; DME – diabetic macular edema; MH – macular hole; RE – right eye; LE – left eye Fig. 1. Vitreomacular traction before procedure 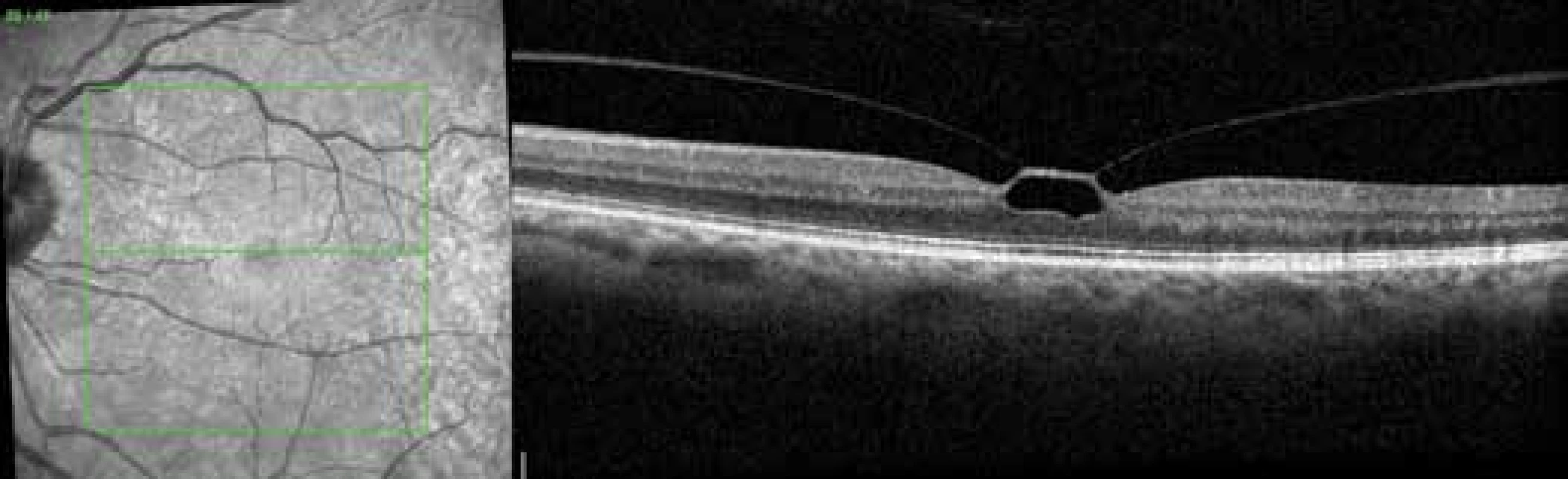
Fig. 2. Finding on OCT 1 month after application of perfluoropropane 
Fig. 3. Finding on OCT 6 months after application of perfluoropropane 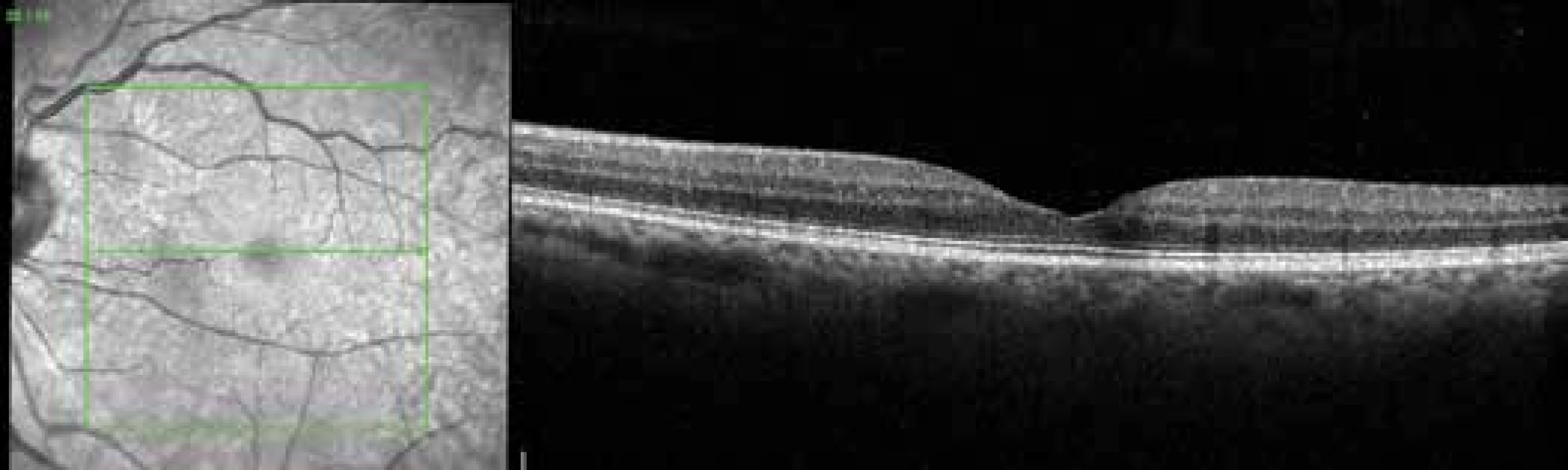
RESULTS
After one application of C3F8 the treatment succeeded in releasing vitreomacular traction in 13 eyes (92.9%), of which in 11 eyes (84.6%) this took place within the first month of observation, and in the other two eyes within two months of the procedure. In one eye VMT persists even after 9 months of observation, although it is lesser, and visual acuity has improved. Release of traction was achieved in both eyes following previous unsuccessful application of ocriplasmin. In one eye release of traction took place simultaneously with the development of macular hole, in this case we indicated PPV. Best corrected visual acuity improved from an average baseline value of 0.50 (0.16-0.18) to 0.67 (0.2-1.0) (p < 0.001). Improvement of BCVA was achieved in 11 eyes (78.6%), in three it remained the same, deterioration did not occur in any of the operated eyes. The gas bubble was absorbed according to the references of the patients within the range of 8-10 weeks. The IOP values within the observed period were within the normal range, without the necessity of anti-glaucomatous therapy. Other than the development of MH we did not record any other potential complications within the observed period.
DISCUSSION
The traditional main approaches in the solution of vitreomacular traction have been observation or pars plana vitrectomy. We usually choose observation in the case of stable mild forms of the pathology, with the possibility of spontaneous release of VMT (11, 17). However, this takes place in approximately only 11% of eyes over the course of 5 years, whereas in 64% of eyes visual acuity decreases during this period by a minimum of 2 rows of a Snellen chart (7, 11). Spontaneous release is less probable in the case of eyes with simultaneous presence of ERM or with a larger extent of vitreomacular adhesion, and in addition there is a risk of progression to macular hole (11, 16).
After PPV visual acuity improves by an average of 0.25 logMAR, i.e. by almost two rows of a Snellen chart (14). However, with regard to the fact that many patients suffer primarily from metamorphopsia, the patient profits from a surgical procedure by the reduction or elimination of metamorphopsia alone even if the visual acuity stays the same. Nonetheless, a potential serious risk of PPV is development of postoperative retinal detachment, which occurs in 2.4-4-6% of eyes (12, 14). This relatively high percentage is linked among other factors with the fact that during the procedure we must perform surgical release of the attached vitreous body, in which a retinal crack may occur. If this is not identified and treated during the surgery, this progresses to retinal detachment. Another adverse effect of PPV is the occurrence and progression of cataract in two thirds of eyes within the course of 2 years (13, 14). On the other hand, the greatest advantages of PPV include removal of vitreous opacifications (21).
At present we do not have any diagnostic method available which could help us decide in which cases to choose observation with a high probability of spontaneous release, and conversely where timely surgical intervention would be more advantageous due to the high risk of progression to macular hole. For this reason it is desirable to have therapeutic methods available which will be more proactive than mere observation, but less invasive than pars plana vitrectomy.
This requirement is met by intravitreal application of ocriplasmin (Jetrea; TromboGenics NV, Leuven, Belgium). This concerns a recombinant protease, which dissolves the protein matrix of the vitreoretinal interface and thereby releases adhesion of the vitreous body to the MLI (6, 20). However, its effectiveness is relatively low. In the double-blind, randomised, multicentric clinical trial MIVI-TRUST, release of VMA was achieved in only 26.5% of cases (20) after one intravitreal application of 125 µg of ocriplasmin. However, if stricter selection of the indicated patients is applied, we may obtain better results. In the double-blind, randomised, multicentric clinical trial OASIS, release of VMA was achieved in 47.1% of eyes after 28 days (5) in patients with VMA < 1.500 µm, without simultaneous presence of ERM. However, this treatment is very expensive, and furthermore it is linked with certain side effects such as temporary loss of sight, changes of the zones of ellipsoids on SD-OCT, disorders of colour vision, blind spots in the visual field and changes of electroretinogram (15, 20).
Pneumatic vitreolysis is therefore offered as a further alternative treatment of VMT. The first author to publish experiences with the use of intravitreal application of gas to induce release of the PVM was Chan (9). Release of the PVM was achieved in 96% of eyes, and closure of MH was achieved in 57% of eyes.
In the MIVI-TRUST study, release of VMT was achieved after the application of ocriplasmin especially in phakic patients (34% vs. 13%) (20). In comparison with this, Steinle et al. achieved similar results by the application of C3F8 in phakic and pseudophakic eyes (89% vs. 75%, p = 0.3173), and furthermore release of traction occurred also in 83% of eyes with simultaneous presence of ERM (21). In the MIVI-TRUST study release of traction was achieved in only 8.7% of patients with simultaneous presence of ERM (20).
In a cohort of 50 eyes with VMT, Chan et al. achieved release of traction in 43 eyes (86.0%) after one application of C3F8, in which a prognostically negative factor was also simultaneous presence of an epiretinal membrane (release in 50% of eyes), as well as diabetes mellitus (release in 25%) (8).
In our cohort release of traction occurred in 92.9% of eyes. This success was contributed to especially by the lesser extent of vitreomacular adhesion (average 490.5 µm), the absence of ERM and the low representation of patients with DR. In 11 of the 13 successful procedures (84.6%) in our cohort, release of VMT was achieved within the first month of observation, in two eyes traction was released later. Rodrigues et al. recorded release of VMT in 20% of eyes over the course of 6 months (18). In the cohort of Chan et al., traction was released in 16% of eyes over the course of 5-9 weeks (8). It is therefore advisable to wait before indicating PPV.
The process of liquefaction of the vitreous body is probably not influenced so much by the size of the gas bubble as by the duration of its effect. In addition to C3F8 it is also possible to apply SF6 into the vitreous chamber. However, there are few published cohorts, and the effectiveness appears to be rather lower in comparison with C3F8, which could be in connection with the shorter duration of its effect. Day et al. recorded release of VMT after the application of SF6 in 55.6% of eyes (4). Čokl et al. compared the effect of both gasses in a prospective study (3). With the aid of C3F8 they achieved release of VMT in 62% of eyes, whereas after application of SF6 traction was released in only 21.4% of eyes. C3F8 was more effective in eyes with an extent of vitreomacular adhesion of > 500 µm (p = 0.001), in the case of adhesions of lesser extent the effect of both gases was comparable. Experiences with the use of SF6 were published also by Buzzacco. Release of VMT was achieved in 83% of eyes. However, the cohort numbered only 6 eyes (1).
Pneumatic vitreolysis can be performed also on eyes in which previous treatment with ocriplasmin has failed. Steinle et al. achieved release of traction in 83% of eyes on which ocriplasmin had previously been applied without success (21). Chan achieved a 66.7% success rate on these eyes (8). Our cohort included 2 eyes in which traction persisted after the application of ocriplasmin (14 and 6 months respectively), after the application of C3F8 traction was released in both eyes.
The advantage of pneumatic vitreolysis in comparison with PPV is its low price, topical anaesthesia, and the minimal risk of development of cataract. In our cohort we did not record progression of cataract in any case. This is in part thanks to the fact that at its maximum size the gas bubble occupies approximately 30-40% of the vitreous cavity, and is therefore in minimal contact with the posterior capsule of the lens. A second reason is the short observation period of our cohort (average 5.8 months). Tornambe published a 12-year analysis of 302 cases of pneumatic retinopexy, and recorded an incidence of cataract in only 1 % of cases (22).
Another risk of pneumatic vitreolysis may be retinal detachment as a consequence of the occurrence of a retinal crack following rapid release of the PVM. However, in the published cohorts this complication occurs only rarely, which may partially be due to the rather smaller cohorts. In our cohort this complication also did not appear. Chan et al. recorded retinal detachment in 1 eye out of 35 (8). The risk of retinal crack can be reduced by careful preoperative examination of the retina and laser treatment of risk peripheral degenerations before the procedure.
A further potential complication is progression of VMT to macular hole. Chan et al. recorded this in 1 eye out of 35 (2.9%) (8), in our cohort the development of MH also occurred in 1 eye (7.1%).
CONCLUSION
In the presented cohort we verified the effectiveness and safety of pneumatic vitreolysis in a selected group of patients with a lesser extent of vitreomacular adhesion. Release of VMT was accompanied by an improvement of visual acuity, the incidence of adverse effects was minimal. In order to set precise indication parameters, the success rate and safety of this method, it would be suitable to conduct a prospective randomised trial. Pars plana vitrectomy appears to us to be a suitable method of second choice, following the failure of pneumatic vitreolysis, or it can be used as the primary method in patients with a larger extent of vitreomacular adhesion, with epiretinal membrane or upon larger opacification of the vitreous body.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received: 29.5.2019
Accepted: 2.7.2019
Available on-line: 6.1.2020
MUDr. Miroslav Veith
Oftalmologická klinika FN Královské Vinohrady
Šrobárova 50
100 34, Praha 10
Zdroje
1. Buzzacco DM., Patel SS.: Treatment of Symptomatic Vitreomacular Adhesion with Expansile Sulfur Hexafluoride (SF6) Gas. Open Ophthalmol J, 11; 2017 : 80-83.
2. Cigánek P., Matoušková L., Kousal B.: Dynamic vitreomacular traction. Cesk Slov Oftalmol, 71; 2015 : 23-28
3. Čokl N., Globočnik Petrovič M.: Intravitreal Injection of Perfluoropropane is More Efficacious than Sulfur Hexafluoride In Releasing Vitreomacular Traction. Acta Clin Croat, 57; 2018 : 327-334.
4. Day S., Martinez JA., Nixon PA., et al.: Intravitreal sulfir hexafluoride injection for the treatment of vitreomacular traction syndrome. Retina, 36; 2016 : 733-737.
5. Dugel PU., Tolentino M., Feiner L., et al.: Results of the 2-Year Ocriplasmin for Treatment for Symptomatic Vitreomacular Adhesion Including Macular Hole (OASIS) Randomized Trial. Ophthalmology, 123; 2016 : 2232-2247.
6. Gandorfer A.: Enzymatic vitreous disruption. Eye (Lond), 22; 2008 : 1273-1277.
7. Hikichi T., Yoshida A., Trempe CL.: Course of vitreomacular traction syndrome. Am J Ophthalmol, 119; 1995 : 55-61.
8. Chan CK., Crosson JN., Mein CE., et al.: Pneumatic vitreolysis for relief of vitreomacular traction. Retina, 37; 2017 : 1820-1831.
9. Chan CK., Wessels IF., Friedrichsen EJ.: Treatment of idiopathic macular holes by induced posterior vitreous detachment. Ophthalmology, 102; 1995 : 757-767.
10. Johnson MW.: How should we release vitreomacular traction: surgically, pharmacologically, or pneumatically? Am J Ophthalmol, 155; 2013 : 203-205.
11. Jackson TL., Donachie PH., Johnston RL.: Electronic medical record database study of vitrectomy and observation for vitreomacular traction. Retina, 36; 2016 : 1897-905.
12. Jackson TL., Donachie PHJ., Sparrow JM., et al.: United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: report 2, macular hole. Ophthalmology, 120; 2013 : 629-634.
13. Jackson TL., Donachie PH., Sparrow JM., et al.: United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: report 1; casemix, complication, and cataract. Eye (Lond), 27; 2013 : 644-651.
14. Jackson TL., Nicod E., Angelis A., et al.: Pars plana vitrectomy for vitreomacular traction syndrome: a systematic review and metaanalysis of safety and efficacy. Retina, 33; 2013 : 2012-2017.
15. Kang SW., et al.: Induction of vitreolysis and vitreous detachment with hyaluronidase and perfluoropropane gas. Korean J Ophthalmol, 9; 1995 : 69-78.
16. Odrobina D., Michalewska Z., Michalewski J., et al.: Long-term evaluation of vitreomacular traction disorder in spectral-domain optical coherence tomography. Retina, 31; 2011 : 324-331.
17. Rodríguez A., Infante R., Rodríguez FJ., et al.: Spontaneous separation in idiopathic vitreomacular traction syndrome associated with contralateral full-thickness macular hole. Eur J Ophthalmol, 16; 2006 : 733-740.
18. Rodrigues IA., Stangos AN., McHugh DA., et al.: Intravitreal injection of expansile perfluoropropane (C3F8) for the treatment of vitreomacular traction. Am J Ophthalmol, 155; 2013 : 270-276.
19. Sebag J.: Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol, 242; 2004 : 690-698.
20. Stalmans P., Benz MS., Gandorfer A., et al.: Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med, 367; 2012 : 606-615.
21. Steinle NC., Dhoot DS., Quezada Ruiz C., et al.: Treament of vitreomacular traction with intravitreal perfluoropropane (C3F8) injection. Retina, 37; 2017 : 643-650.
22. Tornambe PE.: Pneumatic retinopexi: the evolution of case selection and surgical technique. A twelve-year study of 302 eyes. Trans Am Ophthalmol Soc, 95; 1997 : 551-578.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2019 Číslo 4- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Konjunktivitida a původce Corynebacterium macginleyi – kazuistika
-
Všechny články tohoto čísla
- Slovo vedoucího redaktora
- Late postoperative opacification of a hydrophobic acrylic intraocular lens AcryNovaTMPC 610Y
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Ranibizumab in macular oedema secondary to branch retinal vein occlusion – 24 months of treatment
- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- SIMULTANEOUS BILATERAL ACUTE ANGLE-CLOSURE GLAUCOMA IN MILLER FISHER SYNDROME
- Lichen planus as a possible rare cause of an ocular disease
- Výročie narodenia prof. MUDr. Milana Izáka, PhD, FEBO
- Panu docentovi s láskou...
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- NEUROFIBROMATOSIS TYPE 1 AND OPTIC PATHWAY GLIOMA
- Treatment of Vitreomacular Traction with Intravitreal Injection of Perfluoropropane
- Lichen planus as a possible rare cause of an ocular disease
- Doc. MUDr. Vladimír Krásnik, PhD oslavuje 60-tku
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




