-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Surgical treatment of alveolar echinococcosis: a single centre experience and systematic review of the literature
Chirurgická léčba alveolární echinokokózy: naše zkušenost a systematický přehled literatury
Úvod: Alveolární echinokokóza (AE) je zoonóza, jejíž příčinou je Echinococcus multilocularis. Její primární výskyt je téměř výhradně v játrech. Svým chováním alveokok imituje nádorové bujení. Krevním či lymfatickým řečištěm je schopen metastazovat do vzdálených orgánů. Vzhledem k dlouhé inkubační době a nevýrazným příznakům je průběh echinokokózy zpočátku asymptomatický. Další klinické příznaky odpovídají uložení parazita. Diagnostika echinokokózy je založena na anamnéze, klinické symptomatologii, laboratorních vyšetřeních a sérologii, výsledcích zobrazovacích metod a definitivních histologických závěrech. Terapeutickou metodou volby je chirurgické odstranění parazitární hmoty s dostatečným lemem okolní zdravé tkáně, doplněnou pooperační chemoterapií.
Kazuistika: Předkládáme případ onemocnění alveolární echinokokózou u 30ti leté ženy, u které bylo provedeno operační odstranění mnohočetných jaterních ložisek alveokoka. Po 2 letech od operace došlo k recidivě onemocnění s dalším následným operačním řešením.
Závěr: Alveolární echinokokóza je onemocnění, které má vysoký potenciál úplného vyléčení, v případě včasné diagnostiky a přísného dodržení doporučených terapeutických postupů.
Klíčová slova:
Echinococcus granulosus – Echinococcus multilocularis – jaterní cysty – hydatida – alveolární echonokokóza
Authors: H. Kristianova 1; L. Kolarova 2; Z. Krska 1; K. Chrz 1; P. Dytrych 1
Authors place of work: 1st Department of Surgery, General University Hospital and the 1st Medical Faculty of Charles University, Prague 1; Department of Immunology and Microbiology, General University Hospital and the 1st Medical Faculty of Charles, University, Prague 2
Published in the journal: Rozhl. Chir., 2019, roč. 98, č. 4, s. 167-173.
Category: Kazuistika
Summary
Introduction: Alveolar echinococcosis (AE) is a zoonosis caused by Echinococcus multilocularis. AE is primarily localised in the liver. Echinococcus multilocularis imitates tumour-like behaviour. It can metastasise through blood or lymphatic system to distant organs. Echinococcosis often remains asymptomatic due to its long incubation period and indistinct symptoms. Clinical symptoms are determined by the parasite’s location. Diagnosis of echinococcosis is based on medical history, clinical symptoms, laboratory tests, serology results, imaging methods and final histology findings. Surgical removal of the cyst with a safety margin, followed by chemotherapy is the therapeutic method of choice.
Case report: We present a case report of alveolar echinococcosis in a thirty-year-old female patient in whom we surgically removed multiple liver foci of alveolar echinococcosis. The disease recurred after two years and required another surgical intervention.
Conclusions: Alveolar echinococcosis is a disease with a high potential for a complete cure provided that it is diagnosed early and that the recommended therapeutic procedures are strictly adhered to.
Keywords:
Echinococcus granulosus – Echinococcus multilocularis – liver cyst – hydatid – alveolar echinococcosis
Introduction
Echinococcosis is a cosmopolitan zoonosis caused by tapeworms of the Echinococcus genus. Humans are infected when eggs of the parasite are ingested. The eggs are released in the stool of carnivores (dogs, foxes, etc.) in whose intestines sexually mature parasites reside.
Larvae (metacestodes) of all known Echinococcus spp. cause various forms of infections.
The following forms are most clinically significant:
Cystic echinococcosis (hydatid disease, CE) – the disease develops cysts (hydatid cysts) that are clearly separated from the surrounding tissue. Hydatid disease is caused by Echinococcus granulosus sensu lato. The cysts are most commonly located in liver and lungs.
Alveolar echinococcosis (AE) – presents unclearly delimited foci (alveolococcus) located in liver (in 99% of cases). AE is caused by Echinococcus multilocularis and its incidence has been so far constrained to the northern hemisphere.
Polycystic echinococcosis – presents multiple foci predominantly in liver. This disease is caused by Echinococcus vogeli and Echinococcus oligharthrus and it is known from South America.
Very slow growth of the larval stage is typical for all forms of this disease. This slow growth is the reason for the long incubation period and asymptomatic course at the onset of the disease.
The incubation period of alveolar echinococcosis (AE) is estimated as 5−15 years but incubation periods of 30 years are no exception. The most frequent location of the alveolar echinococcosis is primarily in the right liver lobe [1]. Extrahepatic location is rare [2]. The parasite does not form a solitary cyst; due to its exogenous gemmation it penetrates into the surrounding tissue. It presents tumour-like features and can form metastases in distant organs through the blood and lymphatic system. Chronic stage of the infection affects surrounding as well as distant organs [3,4]. Untreated alveolar echinococcosis is lethal [1].
Diagnosis of echinococcosis is based on clinical data, laboratory tests and medical history. Imaging methods demonstrate foci with irregular margins and possible necrosis and calcifications located in the centre. Histological examination of tissue biopsy establishes parasite clusters surrounded by a laminar membrane. Suspicion of AE is expressed based on imaging methods (USG, CT, MRI, PET CT) or serology tests (ELISA, Western blot). The final diagnosis is concluded either by positive results of both examination methods or by positive results of one the above presented method together with confirmed histopathological or molecular tests (PCR).
Conditions including cystic echinococcosis, hepatocellular carcinoma, amoebic liver abscess or haemangioma must be excluded before the treatment is initiated.
Treatment indications are based on features of the larval stage, experience of the medical team, material equipment and general condition of the patient. Surgical removal of alveolar echinococcosis [5,6] accompanied by subsequent chemotherapy with albendazole is the method of choice with a potential for a complete cure.
Human AE has been diagnosed in the Czech Republic since 2007 [3]. The total of 27 patients were diagnosed until 2015 and all patients suffered from an advanced stage of chronic disease [7]. As alveolar echinococcosis is not considered in the course of primary examinations, we present a liver disease case in one thirty-year-old female patient in whom we performed radical resection of the foci.
Case report
The thirty-year-old female patient from Central Europe, living the Czech Republic for more than 10 years started to experience pressure in the epigastrium when pregnant in 2012. She aborted in the 6th week of pregnancy. She was examined by a gastroenterologist who detected tough resistance in the epigastrium and hepatomegaly (liver exceeded the costal arch structure by 4 cm). Following CT scans demonstrated multiple bulky lobed foci with central calcifications and necrosis in both liver lobes. The mass in the right liver lobe was 80 mm in diameter and the mass in the left liver lobe was 110 mm in diameter. Two additional smaller lesions were detected in the 7th segment.
MRI (Fig. 1) and PET/CT (Fig. 2) scans showed alveolar echinococcosis at the end of May 2013. Subsequent serology tests using ELISA (IgG) technique repeatedly confirmed anti-E. multilocularis, anti-E. granulosus and anti-Taenia solium antibodies. Western blot test detected specific anti-E. multilocularis antibodies. The final diagnosis of alveolar echinococcosis was established based on these test results.
Fig. 1. MRI images prior to surgical intervention 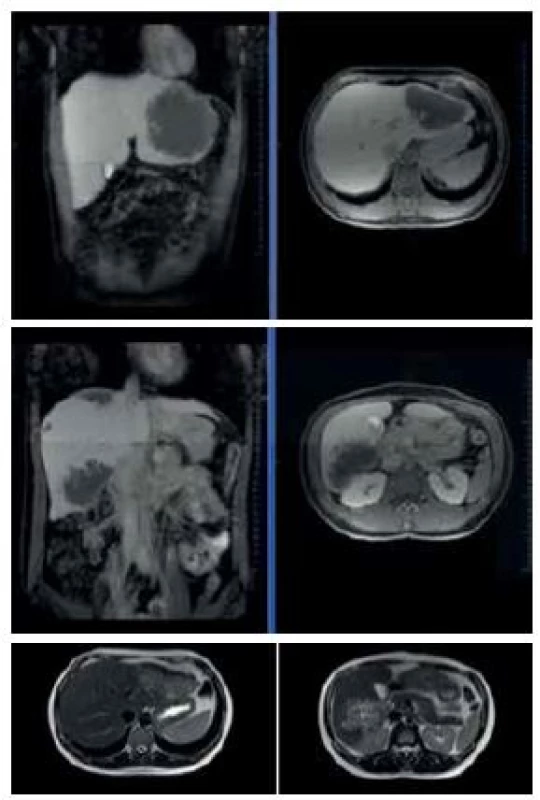
Fig. 2. PET/CT scans prior to surgical intervention 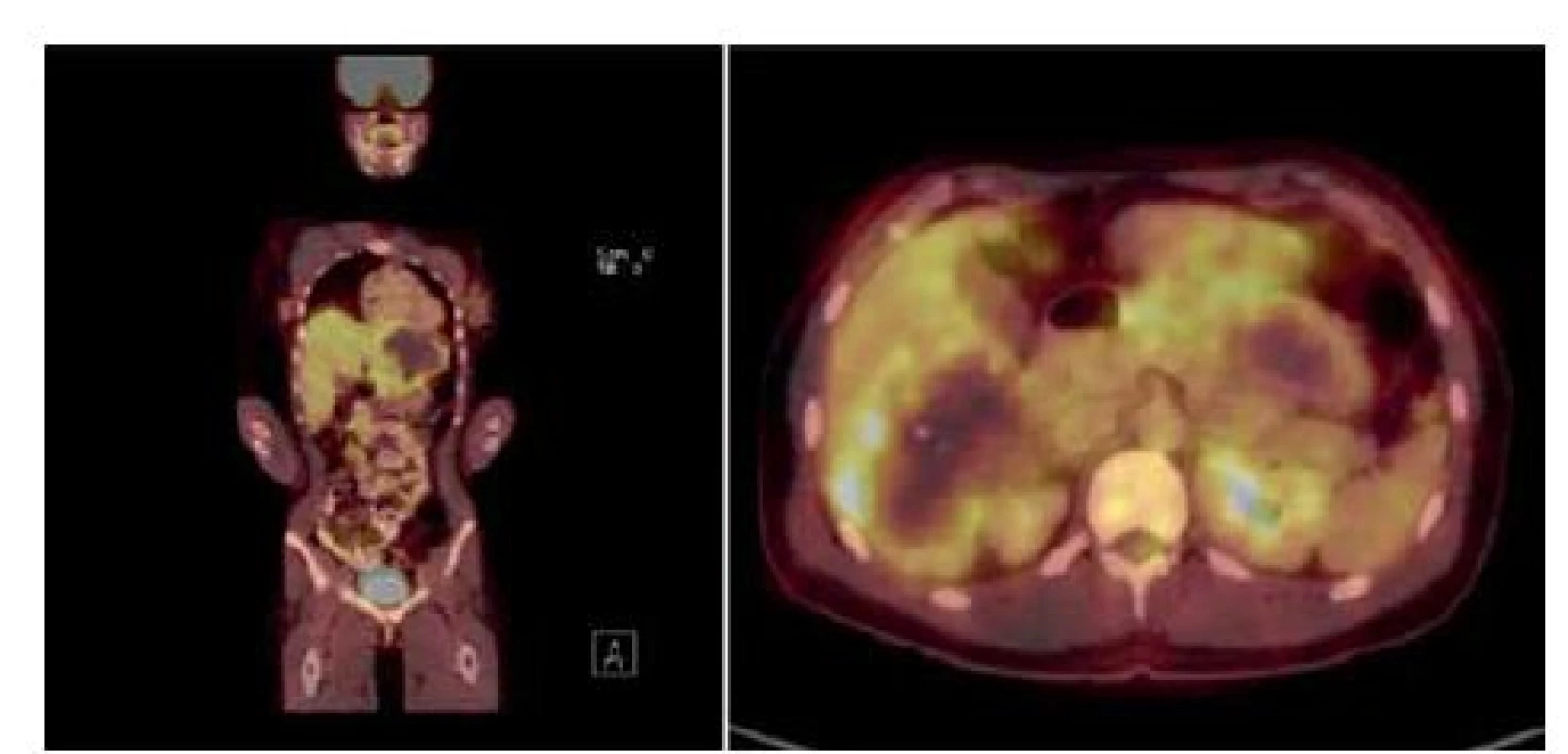
The patient was treated with the antihelminthic agent mebendazole (Wermox) dosed 300 mg bid from May until June 2013. Albendazole (Zentel) dosed 400 mg bid was administered from June until August 2013. Mild elevation of GGT levels occurred after initiation of the therapy. Surgical intervention was indicated due to the risk of exogenous spread of the infection.
The surgical procedure was performed in August 2013. In the course of surgery a structure 100 mm in diameter was detected in the left liver lobe (Fig. 3), structures sized 40 a 60 mm in diameter were found in segments VI and VII, and a structure sized 50 mm in diameter in segment VIII. Non-anatomical resection was performed (Figs. 4, 5) with preservation of segments I and IV in the left lobe and of segment V and portions of segments VI and VII in the right liver lobe. The residual liver volume was found to be sufficient. Initial Pugh-Child score A – 5 points (Tab. 1). The patient was transferred for further care to an infectiologist on the 17th postoperative day.
Tab. 1. Child-Pugh classification 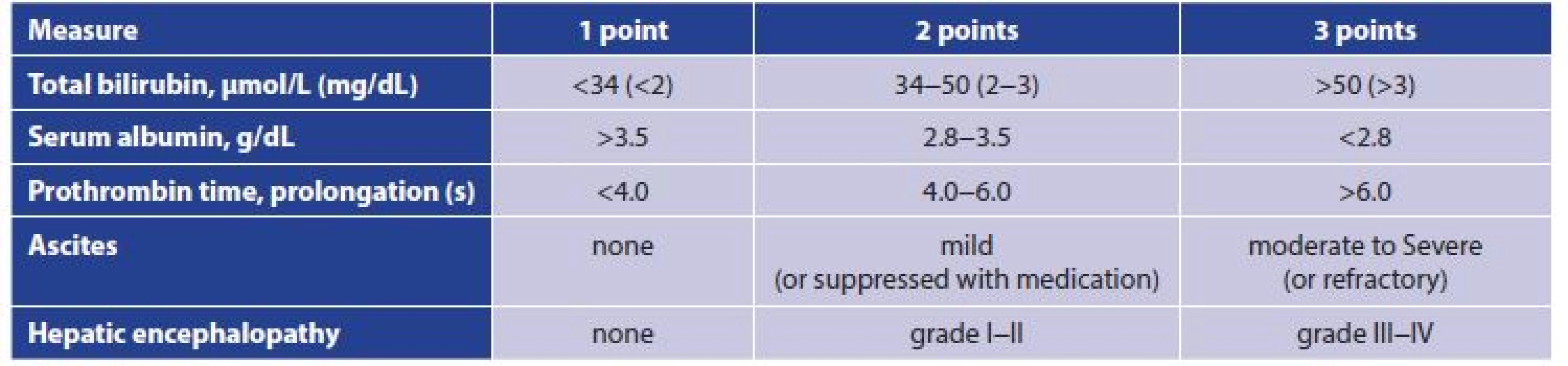
Fig. 3. Findings during surgical intervention – cyst in the left liver lobe 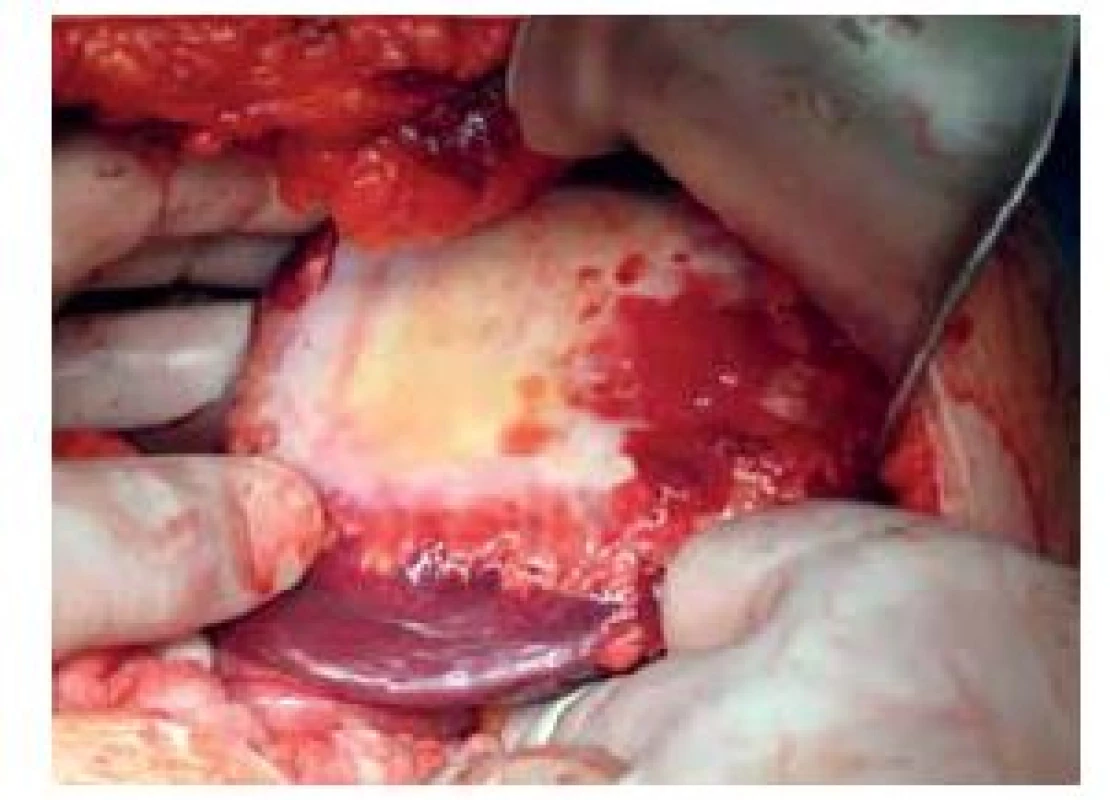
Fig. 4. Finding during surgical intervention; liver cysts 
Albendazole was subsequently administered at dose 400 mg bid for six months. Control PET/CT scan (Fig. 6) demonstrated a lesion in liver after two years. Recurrence of the echinococcus cyst was established. Surgical intervention was performed after prior administration of albendazole with resection of the lesion at the border of segments V and VI with a safety margin (Fig. 7). Given that the lesion was in close contact with liver hilum only limited resection of the liver parenchyma was conducted. Histology of tissue biopsy established recurrence of alveolar echinococcosis. The patient is currently free of any complaints and has been taking albendazole 400 mg bid.
Tab. 2. PET/CT scans prior to the second surgical intervention – recurrence 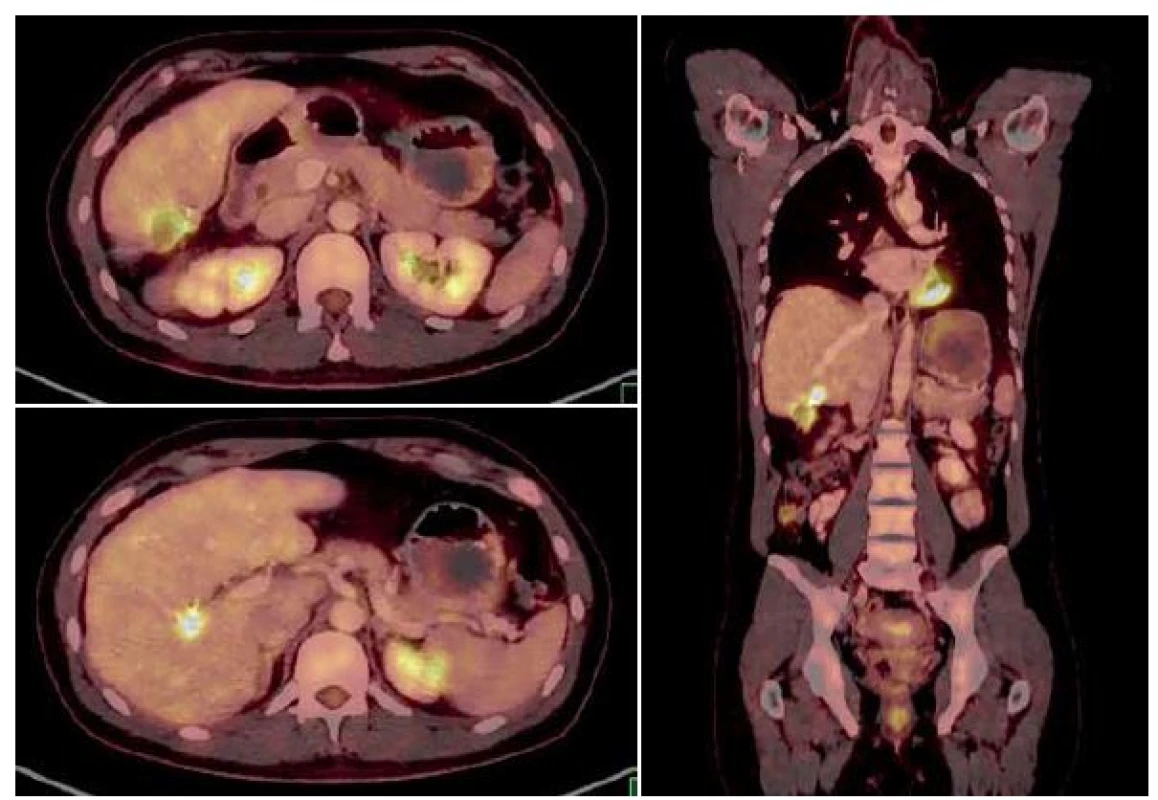
Fig. 6. Finding during the second surgical intervention 
Disease was staged as P1N0M0 (Tab. 2) according to the International Classification of Diseases [1].
Tab. 3. Classification and staging of alveolar echinococcosis 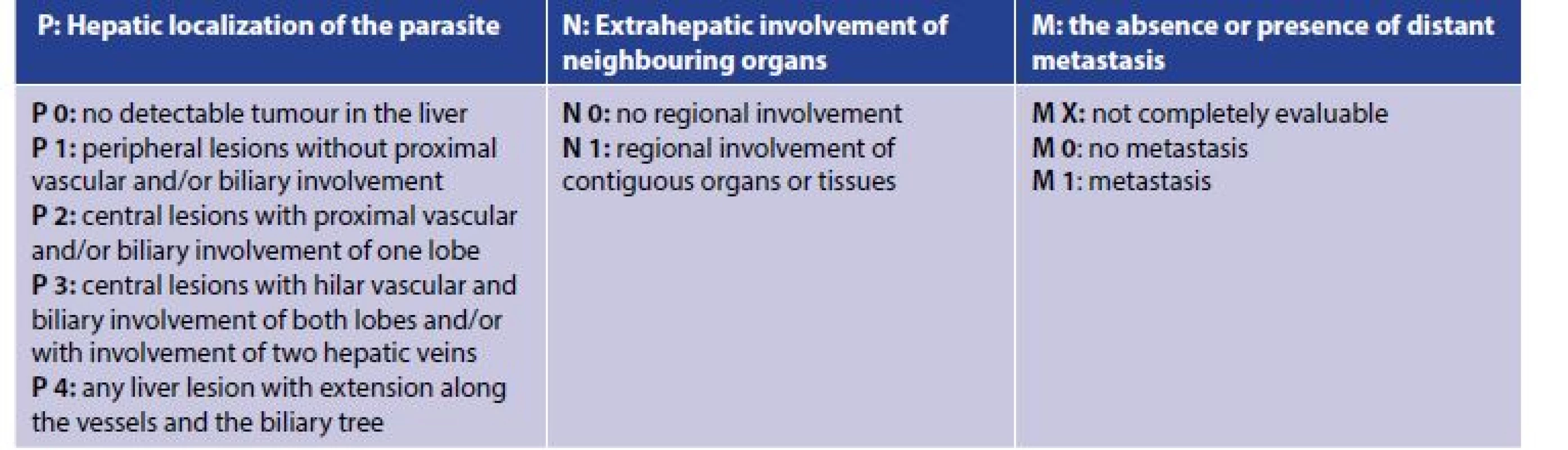
Discussion
Alveolar echinococcosis is a fairly rare disease in our region. Only two cases were presented in the last century, namely in 1928 [8] and 1979 [9]. Since 2007, 36 cases have been diagnosed [3]. The current increase in the number of infections, observed also in neighbouring countries [10,11], is related to the rising risk of infection with eggs of E. multilocularis in sylvatic as well as in urbanised regions [2].
Clinical manifestation depends on location of the cyst. Typical initial symptoms of the infection are difficult to determine due to the long incubation period of alveolar echinococcosis. The patient in our case report experienced only pressure in the epigastrium, which corresponds to literature data [2]. Apart from this symptom frequent signs include loss of appetite, abdominal pain or dyspepsia, and hepatomegaly with an abdominal tumorous mass. Up to one third of patients presents jaundice [2]. Biliary complications occur in 45% of patients [12]. Bacterial cholangitis is a significant complication of alveolar echinococcosis. Invading metacestodes cause obstruction of the biliary system resulting in chronic infection and possible secondary cirrhosis. Endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic biliary drainage are recommended in case of such complications [13]. Advanced stage of the disease features liver dysfunction with portal hypertension. Liver infection features formation of tumour-like masses consisting of minute multiple cystoids aggregated by fibrotic tissue. As there is no eradication therapy but only therapy that stops the growth of the parasite, the only curative treatment consists in surgical removal of the masses like in case of malignancy. The aim of surgical resection is to completely remove the undamaged parasitic mass with a 2cm safety margin [14]. Curative surgical intervention is indicated only if complete resection of all liver foci with a safety margin is feasible and if there are no irremovable foci in other organs or extrahepatic tissues [1,14].
The possibility of radical liver resection depends on the size and number of masses as well as on the residual volume of the healthy liver parenchyma. Alveolar echinococcosis causes a slow progression of the parasitic mass and late onset of the biliary cirrhosis. Metacestodes of E. multilocularis present a unique pro-proliferative effect on the liver tissue resulting in easier hypertrophy of the unaffected liver tissue and allowing for liver resection or autotransplantation more frequently than in other patients with liver tumours [15]. However, due to long clinical latency several cases are diagnosed in advanced stages where resection cannot be performed. Thus resection is possible only in 35−40% of cases [16,17].
Due to frequent involvement of the common hepatic duct resection of the bifurcation with subsequent reconstruction of the biliary system using Roux-en-Y loop is often necessary [14]. The right hemihepatectomy is indicated, sometimes extended with resection of segments I and IV. Left hemihepatectomy is rarely indicated. If affected, resection of the diaphragm or a portion of the inferior vena cava or removal of retroduodenal and retropancreatic lymph nodes may be indicated [18].
Surgical intervention was indicated in almost every patient in the past but the curative effect was evidenced only in 30% of cases in which a complete removal of parasitic masses was achieved [19].
The aim of palliative surgery is to confirm diagnosis, drain the necrotic cavity which is often present in the centre of the mass resulting in possible bacterial infection, reduce parasitic mass and reduce the risk of biliary or vascular obstruction. Palliative resection is recommended to enhance the effect of antihelmintics [6,12]. The reasons for resection include extended liver involvement, distant metastases or direct invasion in hepatic hilum, inferior vena cava, diaphragm or retroperitoneal space [20].
Kadry et al. reported a similar rate of complications after debulking procedures, stand-alone therapy with benzimidazole (p=0.7) and more frequent progression of liver alveolar echinococcosis compared to curative resections (p=0.008). They concluded that debulking did not present any advantage in the treatment of alveolar echinococcosis [21]. Moreover, these surgical procedures could generate complications affecting the quality of life and the survival rate and result in difficulties encountered during later liver transplant [19].
There has been a tendency to substitute other palliative procedures such as billiodigestive anastomosis, external drainage and portocaval anastomosis with less invasive non-surgical interventions (endoscopic or radiologic) over the past decades. Current recommendations to avoid palliative surgical procedures and to choose percutaneous techniques come essentially from the retrospective single-centre trials in patients with alveolar echinococcosis [12,14,21,22]. As revealed by the follow-up of individual cases after percutaneous drainage, the cavities became significantly smaller despite fibrous and calcified features of their margins. This fact can lead to reconsideration of resection possibility several weeks or months after drainage [23]. Percutaneous drainage is indicated in case of infectious complications. It is a method of choice to prevent sepsis and septic shock. Thus it should be performed as soon as possible [22].
No considerable survival rate has been evidenced in case of systemic palliative therapy. Nevertheless, palliative surgery remains an option for complications that cannot be managed by conservative or interventional techniques [17].
Indications for liver transplant include otherwise insoluble and life threatening complications such as severe liver failure, end stage liver disease, chronic cholestasis, secondary biliary cirrhosis, portal hypertension with gastrointestinal bleeding, Budd-Chiari syndrome due to infiltration or compression of hepatic veins or recurrent life threatening cholangitis. Another indication for liver transplant is a situation where radical liver resection is not technically possible [1,15,16]. This situation is caused by: scary tissue around the anatomical structures (diaphragm, inferior vena cava, right atrium), dilated hepatic veins or conditions after prior palliative surgical interventions.
All the above stated conditions technically complicate possible secondary liver transplant and are moreover associated with a significantly higher risk of recurrence. Thus, it is recommended to prefer percutaneous or endoscopic approach to an open revision of the abdominal cavity in cases of infectious complications [16].
Immunosuppression and suspension of systemic administration of benzimidazole during the perioperative period increase the risk of recurrence or progression of the extrahepatic disease. Uncertainty of a complete cure is another reason for suggesting a liver transplant, although only in patients with significantly symptomatic alveolar echinococcosis. Higher doses of albendazole seem to stabilize those forms of incurable disease in patients with asymptomatic or pauci-symptomatic disease [22].
Bresson-Hadni presents five-year survival rate 71% in 47 patients and five-year disease free interval in 58% of patients after liver transplant. The frequency of prior surgical procedures or interventions was 72% and 74% in this cohort. 15 transplants were considered as palliative due to non-removable residual parasite mass or known distant metastases of alveolar echinococcosis [16].
Albendazole administration is usually initiated after the diagnosis of alveolar echinococcosis. The recommended duration of the therapy after radical resection is 2 years [21]. Albendazole therapy is recommended prior to liver transplant to firstly assess tolerance of the drug and secondly to stabilize the disease in patients awaiting liver transplant [16,22]. Lifelong therapy or at least two-year chemotherapy (with no signs of recur-
rence) is recommended after liver transplant. This therapy should be initiated by the end of the first month after the transplant and after stabilisation of liver function tests [16].Conclusion
Alveolar echinococcosis is a disease which often proceeds to an inoperable stage due to its long asymptomatic course. Early diagnosis and adherence to the recommended therapeutic procedures has a high potential for a complete cure of this disease. The principle of successful treatment is based on an exact preoperative diagnosis and on exact aetiology and location of the parasite excluding the extrahepatic location. A complete preoperative diagnostic procedure was undertaken in the case of our patient. The finding was assessed as resectable. Liver lesions were completely resected. One lesion was not resected with the 2cm safety margin due to its unfavourable localisation close to hepatic hilum. Another difficulty arose during postoperative chemotherapy. The recommended two-year chemotherapy was not completed and chemotherapy was discontinued after six months because the health insurance company refused to cover the cost of treatment. All these deviations from the recommended procedures resulted in recurrence of the disease. The current medical condition of the patient is stable. The patient has been regularly followed and no signs of recurrence have been observed.
Conflict of interests
The authors declare that they have not conflict of interest in connection with this paper and that the article has not been published in any other journal.
MUDr. Kristianová Hana
1st Department of Surgery
General University Hospital
and the 1st MF of Charles University
U Nemocnice 499/2
128 05 Prague 2
e-mail: hana. kristianova@vfn.cz
Zdroje
-
Brunetti E, Kern P, Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta tropica 2010;114 : 1−16. doi: 10.1016/j.actatropica.2009.11.001
-
Kern P, Bardonnet K, Renner E, et al. European Echinococcosis Registry: human alveolar echinococcosis, Europe, 1982–2000. Emerg Infect Dis 2003; 9 : 343–9. doi: 10.3201/eid0903.020341
-
Kolářová L, Matějů J, Honzáková L, et al. Humánní alveolární echinokokóza a přehled výskytu tasemnice Echinococcus multilocularis u zvířat v České republice. Epidemiologie, mikrobiologie, imunulogie 2017;4 : 163−72.
-
Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17 : 107−35. doi: 10.1128/CMR.17.1.107-135.2004
-
Eckert J, Gemmell MA, Meslin FX, et al. WHO/OIE manual on echinococcosis in humans and animals: a public health problem of global concern. Paris, WHO/OIE 2001.
-
World Health Organization. Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull WHO 1996;74 : 231–242.
-
National Reference Laboratory for Tissue Helminthoses of the Czech Republic, 2016.
-
Bartoš V. Alveolar echinococcosis in the liver. Casopis lek Ces. 1928;67 : 1063.
-
Šlais J, Mádle A, Vanka K, et al. Alveolar hydatidosis (echinococcosis) diagnosed by liver puncture biopsy. Cas lek Cesk. 1979;118 : 472–5.
-
Nahorski W, Knap J, Pawlowski ZS, et al. Human alveolar echinococcosis in Poland 1990–2011. PLOS Negl Trop Dis. 2013;7 : 1986. doi: 10.1371/journal.pntd.0001986.
-
Antolová D, Miterpáková M, Radoňak J, et al. Alveolar echinococcosis in a highly endemic area of Northern Slovakia between 2000 and 2013. Euro Surveill. 2014;19. doi: 10.2807/1560-7917.ES2014.19.34.20882.
-
Bresson-Hadni S, Vuitton DA, Bartholomot B, et al. A twenty-year history of alveolar echinococcosis: analysis of a series of 117 patients from eastern France. European Journal of Gastroenterology and Hepatology 2000;12 : 327–36.
-
Tamarozzi F, Vuitton L, Brunetti E, et al. Non-surgical and non-chemical attempts to treat echinococcosis: do they work? Parasite 2014;21 : 75. doi: 10.1051/parasite/2014071
-
Buttenschoen K, Carli Buttenschoen D, Gruener B, et a. Long-term experience on surgical treatment of alveolar echinococcosis. Langenbecks Arch Surg. 2009;394 : 689−98. doi: 10.1007/s00423-008-0392-5
-
Wen H, Dong JH, Zhang JH, et al. Ex vivo liver resection followed by autotransplantation for end-stage hepatic alveolar echinococcosis. Chin Med J. (Engl) 2011;124 : 2813−17. doi: 10.3760/cma.j.issn.0366-6999.2011.18.003
-
Bresson-Hadni S, Koch S, Miguet JP, et al. European group of clinicians. Indications and results of liver transplantation for Echinococcus alveolar infection: an overview. Langenbecks Arch Surg. 2003;388 : 231−8. doi: 10.1007/s00423-003-0394-2
-
Buttenschoen K, Gruener B, Carli Buttenschoen D, et al. Palliative operation for the treatment of alveolar echinococcosis. Langenbecks Arch Surg. 2009;394 : 199−204. doi: 10.1007/s00423-008-0367-6
-
Heyd B, Weise L, Bettschart V, Gillet M. Surgical treatment of hepatic alveolar echinococcosis. Chirurg 2000;71 : 16−20.
-
Vuitton DA, Bresson-Hadni S. Alveolar echinococcosis: evaluation of the therapeutic strategies. Expert Opinion on Orphan Drugs 2014;2 : 67–86. doi: 10.1517/21678707.2014.870033
-
Sato N, Uchino J, Takahashi M, et al. Surgery and outcome of alveolar echinococcosis of the liver: historical comparison of mass screening systems in Japan. Int Surg. 1997;82 : 201–4.
-
Kadry Z, Renner EC, Bachmann LM, et al. Evaluation of treatment and long-term follow-up in patients with hepatic alveolar echinococcosis. British Journal of Surgery 2005; 92 : 1110–6. doi: 10.1002/bjs.4998
-
Bresson-Hadni S, Delabrousse E, Blagosklonov O, et al. Imaging aspects and non-surgical interventional treatment in human alveolar echinococcosis. Parasitology International 2006;55 : 267–72. doi: 10.1016/j.parint.2005.11.053
-
Mantion G, Bresson-Hadni S, Vuitton DA, et al. Treatment of alveolar echinococcosis: a multidisciplinary task. Bulletin de l’Académie Nationale de Médecine 2008;192 : 1151–7.
Štítky
Chirurgie všeobecná Ortopedie Urgentní medicína
Článek vyšel v časopiseRozhledy v chirurgii
Nejčtenější tento týden
2019 Číslo 4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Hojení análních fisur urychlí čípky a gel
- Stillova choroba: vzácné a závažné systémové onemocnění
-
Všechny články tohoto čísla
- Komplikované nitrobřišní infekce
- Komentář k editorialu prof. P. Pafka Všeobecná chirurgie?
- Principles of antibiotic therapy
- The role of new antibiotics in intra-abdominal infections in the era of multi-resistant bacteria
- Negative pressure therapy with the ULTRAVAC instillation in the therapy of infected laparotomies with fascitis − temporary results of a prospective randomized study
- Growth of colorectal liver metastases is not accelerated by intraportal administration of stem cells after portal vein embolization
- Surgical treatment of alveolar echinococcosis: a single centre experience and systematic review of the literature
- Hájkova cena pro rok 2018
- Acute mesenteric ischemia with necrosis of entire small intestine
- Hemangiomatosis of the greater omentum – a case report
- Zbiroh 2019
- Umíme předcházet infekcím v místě operačního výkonu?
- Rozhledy v chirurgii
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Principles of antibiotic therapy
- Acute mesenteric ischemia with necrosis of entire small intestine
- The role of new antibiotics in intra-abdominal infections in the era of multi-resistant bacteria
- Hemangiomatosis of the greater omentum – a case report
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




