-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Utilisation of Electrical Impedance Tomography in Breast Cancer Diagnosis
Využitie elektroimpedančnej tomografie v diagnostike karcinómu prsníka
Východiská:
Rakovina prsníka predstavuje celosvetovo závažný zdravotný a sociálny problém. Včasná diagnostika je kľúčom k úspechu liečby tejto malignity. Hlavnou úlohou tejto štúdie bolo zhodnotiť možnosti novej lacnej neinvazívnej techniky, tzv. elektroimpedančnej tomografie (EIT), a určiť, či implementácia EIT môže kvalitatívne doplniť existujúce klasické zobrazovacie metódy v procese diagnostiky karcinómu prsníka.Materiál a metódy:
Do štúdie boli zaradené náhodne vybrané pacientky z tých, ktoré mali podozrivé mamografické a/alebo sonografické nálezy. Celkovo sa štúdie zúčastnilo 808 pacientok vo veku 18–94 rokov (priemer 54). Kritériá na vylúčenie zo štúdie boli: predchádzajúce operácie na prsníkoch, core-cut biopsia alebo punkčná aspiračná biopsia počas posledných 1 a 3 mesiacov. Najviac boli vylúčené pacientky s implantovaným kardiostimulátorom a pacientky, ktoré pred tým podstúpili rádioterapiu a/alebo chemoterapiu. EIT vyšetrenie bolo vykonané pomocou elektroimpedančného mamografu MEIK, ktorý bol vyvinutý v Ústave rádiotechniky a elektroniky Ruskej akadémie vied.Výsledky:
Senzitivita EIT bola 87 %, mamografie (MMG) 89 %, sonografie (USG) 91 %, špecificita EIT bola 85 %, MMG 91% a USG 84 %. Negatívna prediktívna hodnota (NPV) všetkých troch metód preukázala takmer rovnaké hodnoty, s miernou výhodou USG. Najvyššiu pozitívnu prediktívnu hodnota (PPV) ukázala MMG (83 %), najnižšiu EIT (63 %). V kombinácii EIT + MMG a EIT + USG citlivosť sa zvýšila do 96 %, resp. 98 %. Špecificita EIT + MMG dosiahla 79 % a EIT + USG 71 %. NPV pre ETI + MMG a EIT + USG ukázala rovnaké hodnoty. PPV pre kombináciu EIT + MMG bola 65 % a pre kombináciu EIT+USG 58 %.Závery:
Výsledky našej štúdie sú veľmi podobné výsledkom získaným v predchádzajúcich analogických štúdiách. Je zrejmé, že EIT je sľubná metóda a zaslúži si pozornosť odborníkov, ale je taktiež zrejmé, že nemôže nahradiť MMG a/alebo USG, pretože neposkytuje informáciu o štrukturálnych zmenách v prsníku. Môže však poskytnúť užitočné informácie o metabolických procesoch v tele. Na to, aby vyšetrenie EIT preukázalo svoj plný potenciál, sú potrebné určité zlepšenia.Kľúčové slová:
karcinóm prsníka – elektroimpedančná tomografia – mamografia – sonografia – diagnostika
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do bi omedicínských časopisů.Obdrženo:
10.5.2011Přijato:
12.10.2011
Authors: O. Raneta 1; D. Ondruš 1; V. Bella 2
Authors place of work: 1st Department of Oncology, Faculty of Medicine, Comenius University, St. Elisabeth Cancer Institute, Bratislava, Slovak Republic 1; Out Patient Department of Mammology, St. Elisabeth Cancer Institute, Bratislava, Slovak Republic 2
Published in the journal: Klin Onkol 2012; 25(1): 36-41
Category: Původní práce
Summary
Backgrounds:
Breast cancer presents a serious medical and social problem worldwide. Early detection is key to effective breast cancer treatment. Therefore, scientists are consistently looking for new diagnostic techniques that would be more efficient, easy to use and safe for the patient. The main task of this study was to evaluate the feasibility of a novel low-cost non-invasive technique called electrical impedance tomography (EIT) and to determine whether EIT can qualitatively supplement the existing traditional imaging techniques in the process of breast cancer diagnostics.Patients and Methods:
Randomly selected patients with mammographic and/or sonographic abnormalities were involved into the study. In total, 808 patients aged 18–94 (mean 54) years participated in the survey. Exclusion criteria involved previous breast surgery, breast core biopsy or fine needle aspiration within the last 1 and 3 months, respectively. Furthermore, patients with implanted electrically powered devices (cardioverter, pacemaker) and patients previously treated by chemo-radiotherapy were also excluded. The EIT examination was performed using the electrical impedance computer mammograph MEIK developed by the Institute of Radio Engineering and Electronics, Russian Academy of Sciences.Results:
The following results were obtained: sensitivity of EIT was 87%, X-ray mammography (MMG) 89% and ultrasonography (USG) 91%; specificity of EIT was 85%, MMG 91% and USG 84%. Negative predictive value (NPV) of all three modalities showed nearly equal values, with slight advantage of the USG. MMG had the highest positive predictive (PPV) value (83%), EIT had the lowest (63%). Sensitivity increased to 96% and 98%, respectively, when combinations EIT + MMG and EIT + USG were used. The specificity increased to 79% for EIT + MMG and 71% for EIT + USG. EIT + MMG and EIT + USG NPV remained the same. PPV was 65% and 58%, respectively for the EIT + MMG and EIT + USG combination.Conclusion:
Our study findings are comparable to those of other similar studies. Although the EIT is a promising method and deserves close attention of specialists, it cannot replace MMG and/or USG examination as it does not provide information on structural changes to the breast. It can, however, provide very useful additional information about metabolic processes in the body. But in order to show its full potential some improvements should be held.Key words:
breast cancer – electrical impedance tomography – mammography – ultrasonography – diagnosticsIntroduction
Breast cancer remains a serious medical and social problem in many developed countries, but in recent years, its incidence has begun to increase also in the developing countries. On a global scale it is the 2nd most common cancer at all and is the 5th most common cancer-related death in both sexes [1,2].
Study of early diagnosis of malignant tumors showed the necessity for screening programs, whose main task would be to identify the disease before the onset of symptoms about which the patient subsequently would need a medical care.
Currently, instrumental methods of breast disease diagnostics can be divided into two groups. To the first group belong X-ray mammography (MMG) and ultrasonography (USG). These methods are based on a study of the mammary gland anatomy. They determine the presence or absence of the pathology in the organ’s structure.
To the second group belong diagnostic methods, based on physiology, on the peculiarities of metabolism in breast tissues in norm and pathology. These methods include electrical impedance tomography (EIT).
The EIT is an imaging technology aiming at exploiting the difference in the passive electrical properties (impedance) of living tissues in order to generate a tomographic image. EIT and its employment in biology and medicine has been intensively investigated for nearly 20 years, but it became just recently implemented as a useful tool in the health care praxis including breast cancer detection [3]. The principle of EIT is based on the different electrical storage potential of normal and pathologically altered tissues allowing to image differences in the tissue conductivity and permittivity inferred from the body surface electrical measurements. In praxis, small currents are applied to a part of the subject’s body through conducting electrodes attached to the skin and the resulting electrical potentials are measured and visualized. Since breast cancer show increased electrical conductivity and permittivity values that the surrounding normal tissue [4–7], EIT became a sensitive perspective imaging technology in the breast cancer detection.
Materials and Methods
Patients
Randomly selected patients from those with mammographic and/or sonographic abnormalities were involved into the study. In total, 808 patients aged 18–94 (mean 54) years signed informational agreement and participated in the survey. Exclusion criteria involved previous breast surgery, breast core biopsy or fine needle aspiration within the last 1 and 3 months, respectively. Furthermore, patients with implanted electrically powered devices (cardioverter, pacemaker) and patients previously treated by chemo-radiotherapy were also not involved.
EIT imaging
The EIT examination was performed by means of the electrical impedance computer mammograph MEIK (Fig. 1) developed by the Institute of Radio Engineering and Electronics, Russian academy of sciences. Patients during the examination were in the supine position. Before current application, the examined breast was moistened by water. By means of one out of 256 electrodes of the matrix, weak alternative current (0.5 mA) with a frequency of 50 kHz was applied to the inspected breast and subsequently the surface distribution of electric potentials were recorded and the signals were re-worked to electronic impedance images. The breast has been scanned every 8 mm with the depth of 8 cm.
Fig. 1. Electrical impedance mammograph MEIK. 
In the EIT images, the impedance (tissue conductivity) is reflected by differences in shades of gray scale with smooth transition from dark (hyper-impedance) to light (hypo-impedance) areas. It is known that benign tumours develop from the tissue elements of an unaffected breast, hence there is no difference in electrical properties of tissue of a healthy breast and benign tumours. That’s why benign tumours of small size (less than 1 cm), as a rule, are not visualized on the electrical impedance tomograms. Tumours over 1 cm, primarily cystic lesions are shown as hyper-impedance areas with electrical conductivity below 0.95 conventional units. Its value is similar to the electrical conductivity of the normal glandular tissue of the breast. Focal changes presented in the EIT images in form of light hypo-impedance spots with electrical conductivity exceeding 0.95 conventional units appear in the probable place of the malignant tumour location (Fig. 2).
Fig. 2. Electrical impedance tomogram of the left mammary gland. A 51-year-old patient. Postmenopause – 1 year. Focal changes in the lower-lateral quadrant. 
Results
In our study 808 women were involved. Subsequently, benign changes of mammary glands were identified in 622 of the patients and breast cancer – in 184. Benign diseases were as follows: mastopathy in 410 (66%), fibroadenoma in 133 (21%), hyperplasia/metaplasia in 8 (1.2%), cystic lesions in 49 (8%), adenosis in 12 (2%), lipoma in 10 (1.6%) patients. From the malignant lesions were identified: 14 (8%) with ductal carcinoma in situ, 145 (79%) with invasive ductal carcinoma, 16 (9%) with invasive lobular carcinoma, 6 (3%) with mucinoid adenocarcinoma, three (1.6%) with invasive tubular carcinoma.
In total 808 EIT, 657 MMG and 571 USG investigations were analyzed. In 116 cases (14%) EIT showed a false diagnosis. At the MMG and USG false diagnosis was established in 62 (9%) and 77 (13%) cases, respectively. The fraction of false diagnoses in benign diseases was as follows: for EIT – 92 (15%) for MMG – 43 (9%), USG – 63 (15%). Among the malignant lesions the share of false diagnoses was: for the EIT – 24 (13%) for MMG – 19 (12%), USG – 14 (9%). The distribution of false diagnoses of individual pathology is presented in tab. 1.
Tab. 1. Results of MG, USG and EIT examination related to histopathology results. 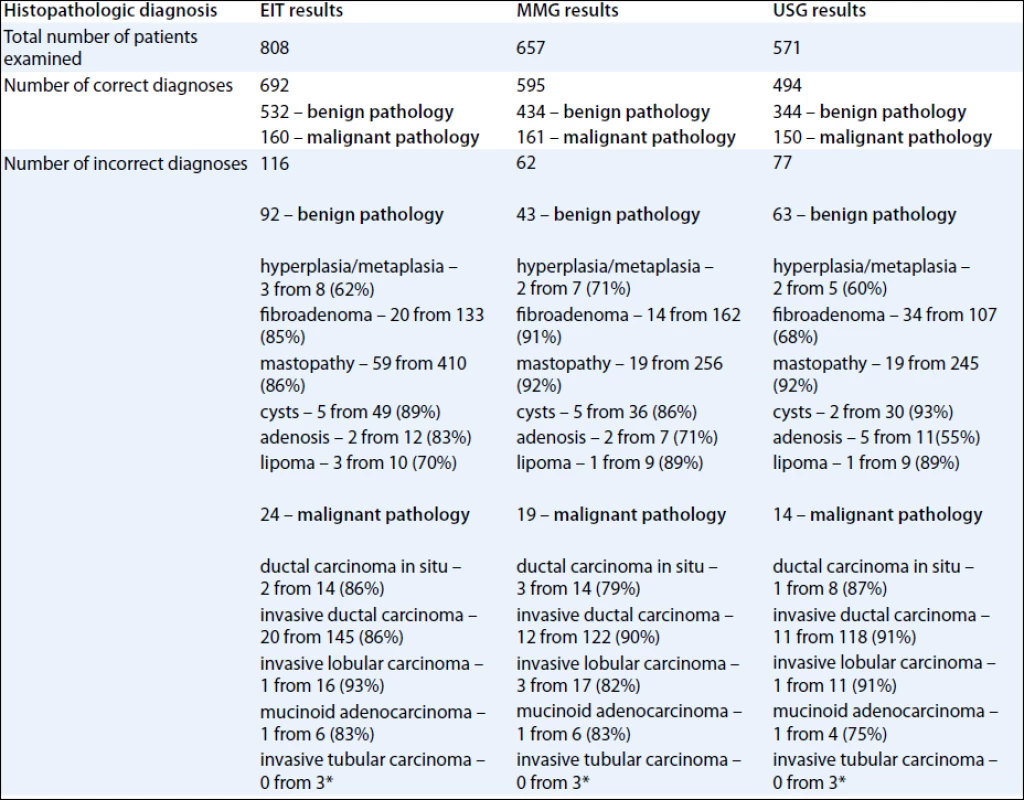
* not counted because of insufficient number of data Additionally, we analysed the false--negative EIT results in correlation with the clinical stage of the process. 20 false diagnoses of invasive ductal carcinoma were distributed according to the following stages: 11 (55%) cases were in T0–T1 stage; 7 (35%) cases – in T2 stage; two (10%) cases – in T3 stage. False-negative diagnoses of invasive lobular carcinoma (one case) and mucinoid adenocarcinoma (one case) also were in T1 stage. All cancers in T4 stage (5 cases) were diagnosed correctly. Thus, the dependence of the EIT sensitivity from the stage of the disease was clearly defined.
The results of our study showed that the sensitivity of the EIT (87%) was lower than of MMG (89%) and USG (91%), but this difference is insignificant. The specificity of the EIT and USG showed almost equal values (85% and 84%, respectively) and specificity of MMG reached 91%.
Negative predictive value (NPV) of all three modalities showed nearly equal values, with slight advantage of the USG. The highest positive predictive value (PPV) had MMG (83%), the lowest – EIT (63%). In combinations EIT + MMG and EIT + USG sensitivity increased to 96% and 98%, respectively. The specificity of EIT + MMG amounted to 79% and of EIT + USG – to 71%. NPV of EIT + MMG and EIT + USG showed equal values. PPV in combination EIT + MMG was 65%, and in combination EIT + USG – 58% (Tab. 2).
Tab. 2. Statistical data for EIT, MG, USG alone and in combination EIT + MG and EIT + USG. 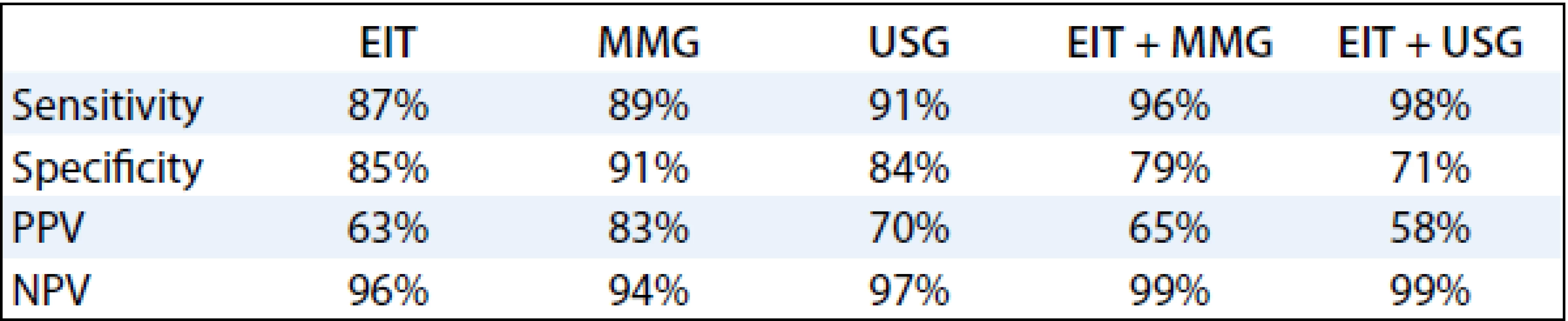
Discussion
MMG screening is currently considered the best method available for mass screening in the early detection of breast cancer [8]. Systematic MMG screening in women aged 50–69 years can reduce mortality rates up to 30% [9]. Sensitivity and specificity of MMG is in direct dependence on breast density, which limits its use at a young age [10,11]. MMG is accompanied by some inconveniences. It requires a special spacious room, has a high cost of maintenance and requires breast compression, which causes discomfort to the patient. Furthermore, examination of the patient is accompanied by radiation, which causes a lot of concerns about scientists [12,13]. In addition, MMG examination performed repeatedly by regular check-ups is leading to onset of psychosocial distress, anxio-depressive syndrome and emotional, cognitive and functional disorders mainly due to fear from cancer detection and progression [14,15].
USG examination is typically used as an auxiliary method after performed MMG or clinical breast examination. It is suitable to examine the young and the pregnant women and to guide biopsies [16]. But a big disadvantage of this method is that it is totally machine - and operator-dependent method [17].
MMG and USG report about the structural changes – about the size of the tumor, its localization, the presence of microcalcifications, and so on. EIT gives to the doctor additional information about the physiological processes taking place in the breast, the presence of metabolic changes in the tissue, disrupting of the electrical properties of the cells. This information can be very valuable, especially between rounds of screening, that last from 12 to 24 months, i.e. rather long period of time.
It is known that the percentage of breast cancer detected between rounds of screening (so-called interval cancers), is an important indicator of its effectiveness. In England, MMG has been held for nearly 30 years, and involves more than 75% of invited women. The Advisory Committee on Breast Cancer Screening conduct the study in which 1,000 women participated. For 10 years these women took part in screening, which revealed 36 cancers: 20 – during screening examinations and 16 – between rounds of screening. Thus, the proportion of interval cancers in England was 33% of all diagnosed cancers [18]. Comparable data were also obtained in other countries [19–21]. Particularly high rate of interval cancer was in the age group 40–49 years, reaching according to the Swedish trials 65.7% [22]. Our study showed that the combined use of MMG and EIT considerably reduces false-negative results and leads the sensitivity to 96%, and in the combination EIT + USG the sensitivity increases to 98%.
Taking into account these data, as well as the fact that this technology is non--invasive and free of radiation, we consider it appropriate to use EIT for preventive check-ups of the female population between rounds of screening in order to isolate patients at risk; in examination of pregnant and lactating women and women with high risk of carcinogenesis (BRCA1, BRCA2 genes) and as an additional method in the algorithm of complex breast cancer diagnostics, including and in young women. However, it should keep in mind that the young woman’s breast has a rich vascularization and therefore a higher electrical conductivity of the tissue, which may affect the outcome of the study. Tofts et al [23] proved, that highly vascularized tumors are characterised by a significantly increased permeability. Therefore a higher vascularization might lead to an increased conductance because of the higher permeability of the cell membranes and thereby increase the number of false-positive results. In turn, Stojadinovic et al [24] presented preliminary results on the use of EIT for the early detection of breast cancer in young women. They stated that EIT appears promising for early detection of breast cancer, and identification of young women at increased risk for having the disease at the time of screening.
The results of our study have shown that EIT deserves the close attention and is a promising method, but in order to show its full potential some improvements should be held. A major shortcoming of this technique is poor differentiation among various benign tumors, and in some cases, the separation of malignant tumours from benign lesions. More data are required to better categorize the information contained in EIT images.
Conclusion
The findings of our study are very similar to data from previous analogous studies. Obviously, the EIT has several advantages and deserves the close attention of specialists, but it cannot replace MMG or USG, because it does not give the information about the structural changes of the breast, which is extremely necessary to the doctor. However, it can provide additional very useful information about the metabolic processes in the body. This information can often be decisive in elaboration of the treatment strategies and in the management of the patient. Although this technology will probably never become the gold standard that MMG is today, further clinical study may lead to EIT being replaced from category “an controversial experimental modality” to category “an acceptable and widely used adjunct modality”.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Olga Raneta, MD.
1st Department of Oncology
Faculty of Medicine
Comenius University
St. Elisabeth Cancer Institute
Heydukova 10
812 50 Bratislava
Slovak Republic
e-mail: olga_raneta@hotmail.com
Submitted: 10. 5. 2011
Accepted: 12. 10. 2011
Zdroje
1. Ondrusova M. Breast cancer epidemiology. Onkológia 2009; 4(2): 72–75.
2. Plesko I. Current global and local knowledge and problems of epidemiology of malignant tumors. Onkológia 2006; 1(1): 8–13.
3. Hope TA, Iles SE. Technology review: the use of electrical impedance scanning in the detection of breast cancer. Breast Cancer Res 2004; 6(2): 69–74.
4. Surowiec AJ, Stuchly SS, Barr JB et al. Dielectric properties of breast carcinoma and the surrounding tissues. IEEE Trans Biomed Eng 1988; 35(4): 257–263.
5. Jossinet J. The impedivity of freshly excised human breast tissue. Physiol Meas 1998; 19(1): 61–75.
6. Singh B, Smith CW, Hughes R. In vivo dielectric spectrometer. Med Biol Comput 1979; 17(1): 45–60.
7. Jossinet J. Variability of impedivity in normal and pathological breast tissue. Med Biol Eng Comput 1996; 34(5): 346–350.
8. Prasad SN, Houserkova D, Campbell J. Breast imaging using 3D electrical impedance tomography. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2008; 152(1): 151–154.
9. Lehotská V, Príkazská M. Mammography – importance, possibilities, technical trends, current situation and perspective. Onkológia 2006; 1(1): 19–21.
10. Mushlin AI, Kouides RW, Shapiro DE. Estimating the accuracy of screening mammography: a meta-analysis. Am J Prev Med 1998; 14(2): 143–153.
11. Carney PA, Miglioretti DL, Yankaskas BC et al. Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med 2003; 138(3): 168–175.
12. Armstrong K, Moye E, Williams S et al. Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians. Ann Intern Med 2007; 146(7): 516–526.
13. Mettler FA, Upton AC, Kelsey CA et al. Benefits versus risks from mammography: a critical reassessment. Cancer 1996; 77(5): 903–909.
14. Bencova V, Svec J, Bella V. The role of psychosocial oncology in the health care of breast cancer survivors. Bratisl Lek Listy 2009; 110(6): 374.
15. Bencova, V, Mrazova A, Svec J. Psychosocial morbidi-ty – an unfilled gap in the undergraduate courses of medicine and nursing. Clin Social Work 2010; 1–2 : 38–42.
16. Sehgal CM, Weinstein SP, Arger PH et al. A review of breast ultrasound. J Mammary Gland Biol Neoplasia 2006; 11(2): 113–123.
17. Nover AB, Jagtap S, Anjum W et al. Modern breast cancer detection: a technological review. Int J Biomed Imaging 2009; 2009 : 902326.
18. NHS Cancer Screening Programmes. Screening for Breast Cancer in England: Past and Future. NHSBSP Publication No 61; c2006-02 [updated 2006 February; cited 2011 Aug 9]. Available from: http://www.cancerscreening.nhs.uk/breastscreen/publications/nhsbsp61.html.
19. Shapiro S. Evidence on screening for breast cancer from a randomized trial. Cancer 1977; 39 (Suppl 6): 2772–2782.
20. Frisell J, Glas U, Hellström L et al. Randomized mammographic screening for breast cancer in Stockholm. Design, first round results and comparisons. Breast Cancer Res Treat 1986; 8(1): 45–54.
21. Frisell J, Eklund G, Hellström L et al. Analysis of interval breast carcinomas in a randomized screening trial in Stockholm. Breast Cancer Res Treat 1987; 9(3): 219–225.
22. Tabàr L, Fagerberg G, Duffy SW et al. Update of the Swedish two-county program of mammographic screening for breast cancer. Radiol Clin North Am 1992; 30(1): 187–210.
23. Tofts PS, Berkowitz B, Schnall MD. Quantitative analysis of dynamic Gd-DTPA enhancement in breast tumors using a permeability model. Magn Reson Med 1995; 33(4): 564–568.
24. Stojadinovic A, Nissan A, Gallimidi Z et al. Electrical impedance scanning for the early detection of breast cancer in young women: preliminary results of a multicenter prospective clinical trial. J Clin Oncol 2005; 23(12): 2703–2715.
Štítky
Dětská onkologie Chirurgie všeobecná Onkologie
Článek vyšel v časopiseKlinická onkologie
Nejčtenější tento týden
2012 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Nejasný stín na plicích – kazuistika
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
-
Všechny články tohoto čísla
- Comparative Plasma Proteomic Analysis of Patients with Multiple Myeloma Treated with Bortezomib-based Regimens
- Identification of Molecular Markers in Children with Acute Myeloid Leukemia (AML)
- Editorial
- Utilisation of Electrical Impedance Tomography in Breast Cancer Diagnosis
- The Incidence of Malignancies and Surveillance of Hematopoietic Stem Cells Donors – the Results of the Haemato-Oncology Department University Hospital in Plzen (Pilsen) and Czech National Marrow Donors Registry Observation
- Six-year Follow-up of a Patient with Multiple Angiomatosis Involving Skeleton, Thoracic and Abdominal Cavities and the Gut Wall
- Nové možnosti vzdělávání českých chirurgů v onkochirurgii
- Erratum
- Recenze
- Tematický seznam publikací vydaných v Klinické onkologii v roce 2011
- Venous Access Devices in Oncology
- Klinická onkologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Venous Access Devices in Oncology
- Utilisation of Electrical Impedance Tomography in Breast Cancer Diagnosis
- Identification of Molecular Markers in Children with Acute Myeloid Leukemia (AML)
- Six-year Follow-up of a Patient with Multiple Angiomatosis Involving Skeleton, Thoracic and Abdominal Cavities and the Gut Wall
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



