-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Reducing Vulnerability to Climate Change in Sub-Saharan Africa: The Need for Better Evidence
article has not abstract
Published in the journal: . PLoS Med 10(1): e32767. doi:10.1371/journal.pmed.1001374
Category: Essay
doi: https://doi.org/10.1371/journal.pmed.1001374Summary
article has not abstract
Summary Points
-
Sub-Saharan Africa (SSA) has contributed the least of any world region to the global accumulation of greenhouse gas emissions yet will be more vulnerable to the impacts of climate change than any other.
-
Despite the growing awareness of Africa's vulnerability to climate change, there is very little empirical evidence on the health effects of climate change in SSA.
-
A cross-disciplinary research agenda needs to be developed to enhance understanding of the health effects of climate change in different settings within SSA linking meteorology, climatology, other relevant sectors and health.
-
Adaptive capacity needs to be built through health systems strengthening, and developing more resilient health facilities and supply chains.
-
The health dividend of many actions to reduce greenhouse gas emissions needs to be better understood and appreciated by the climate change and public health communities.
Introduction
Sub-Saharan Africa (SSA) has contributed the least of any world region to the global accumulation of greenhouse gas emissions; however, this region will probably be more vulnerable to the impacts of climate change than any other [1]. Less than 7% of the world's total emissions of greenhouse gases emanate from the African continent [2]; thus the continent contributes very little overall to climate change. Yet the highest regional burden of climate change is likely to be borne by SSA, with 34% of the global disability adjusted life years (DALYs) attributable to the effects of climate change in the region [3]. The impacts of climate change are likely to be concentrated in low-income countries where poor populations already have compromised heath prospects, health systems are weak, and where the capacity to adapt and address vulnerabilities is limited. However, to mount a proper response there are some fundamental constraints that need to be addressed, which we further discuss in this Essay.
The Limited Evidence On Climate Change And Health In Sub-Saharan Africa
Despite the growing awareness of SSA's vulnerability to climate change, there is very little empirical evidence published about the effects of climate change on population health in SSA [4]. Some attention has been given to potential increased incidence of vector-borne diseases such as malaria, particularly in highland areas in East Africa [5],[6]. Although this finding has been contested, increased temperatures together with changes in precipitation may exacerbate malaria epidemics and lead to the spread of malaria beyond its normal transmission zone [7]. Overall, though, any possible effect of climate change on malaria is likely to be two orders of magnitude smaller than those that can be achieved by the effective scale-up of key control measures [8]. It is likely that climate change will alter the ecology and transmission patterns of climate-sensitive, parasitic infections such as schistomiasis, trypanosomiasis, and leishmaniasis, and other diseases such as cholera, diarrhoeal infections, and Rift Valley fever [9]; but the overall impacts on health are unclear.
More significantly, climate change may impact seriously on environmentally sensitive sectors such as water, agriculture, and food production and adversely affect human health and vulnerability to disease as a result [10]. Changing temperatures, humidity, and precipitation are expected to disrupt agricultural production systems, reducing food production and leading to higher levels of malnutrition, which in turn can increase vulnerability to disease. Significant rainfall reductions observed in critical crop-growing areas in East Africa have caused severe drought, resulting in loss of agricultural productivity and famine [11]. Countries like Botswana that have already experienced frequent droughts have seen a large number of people abandoning crop production and moving either to cities or informal settlements [7],[11]. These changes now need to be better understood, with more rigorous assessments and building of evidence.
Countries In The Region Are Ill-Prepared To Cope With Climate Change
Although African governments have made firm commitments at various forums to adapt to climate change, many are still considered ill-prepared to cope with the negative consequences of climate variability and change [12]. An Action Plan has been prepared [13] covering the following elements: baseline risk and capacity assessments; capacity building; integrated environment and health surveillance; awareness raising and social mobilization; public health oriented environmental management; scaling up of existing public health interventions; strengthening of partnerships; and promotion of research. However, more investment is required if these proposals are to become reality across all countries in SSA.
The United Nations Framework Convention on Climate Change (UNFCCC) initiated National Adaptation Programs of Action (NAPAs) in 2002 in least developed countries to help prioritise adaptation activities. Of the 47 NAPAS submitted to UNFCC as of January 2012, 33 (70%) were from SSA countries and 15 (45%) of these list health as a priority. Table 1 groups health sector adaption projects from those SSA countries that listed health as a priority; this grouping shows that the most frequently listed projects are malaria control, waterborne disease control, health systems strengthening, improved access to safe drinking water and sanitation, as well as establishment of health surveillance and early warning systems for disaster preparedness and response. However, a World Health Organization (WHO) assessment of these interventions concluded that only a few of them were likely to be effective [14].
Tab. 1. 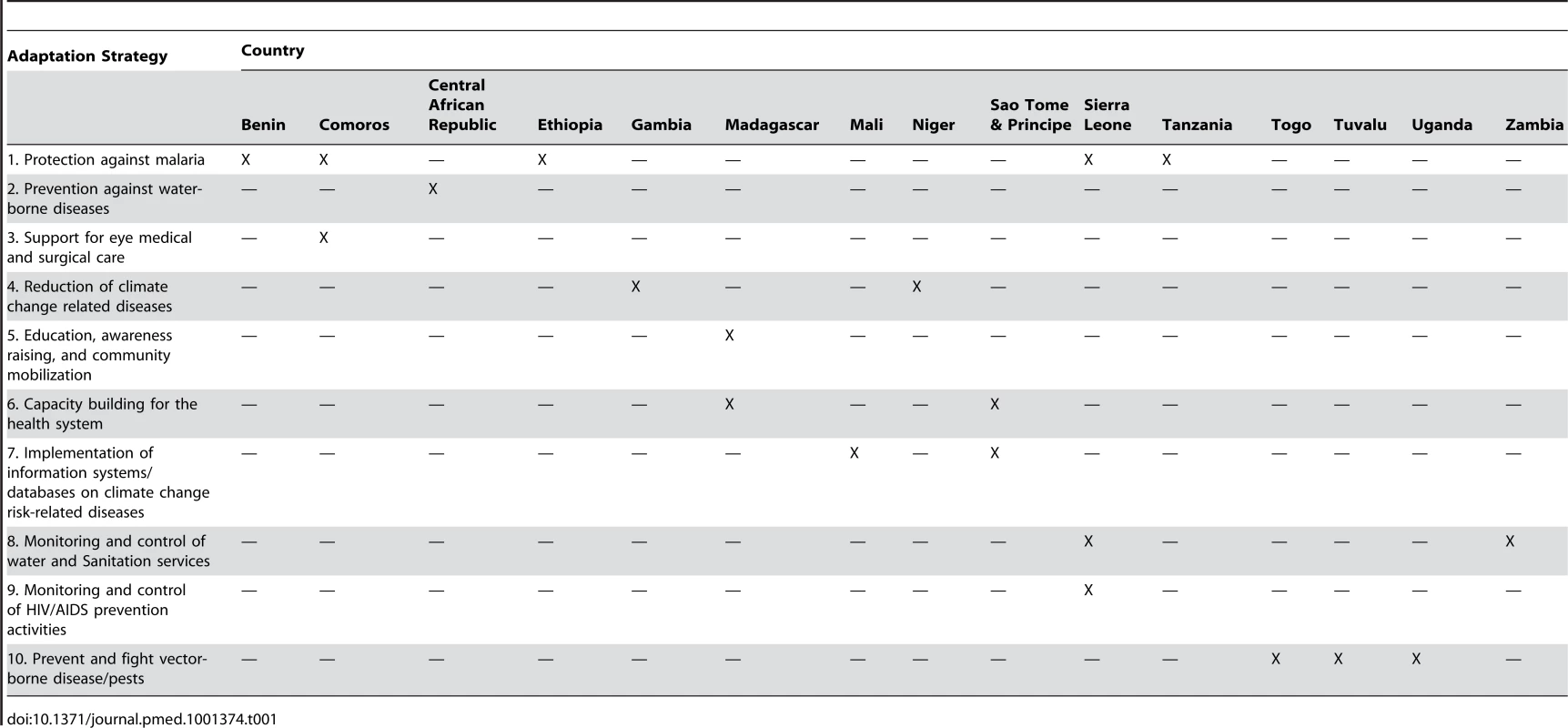
Health adaptation strategies proposed by sub-Saharan African countries in their national adaptation programs of action (January 2012). There are also several multi-country projects that specifically aim to support adaptation within the region; however, a recent review of current and planned adaptation actions [15] concluded that “None of the regional projects identified has as strong focus on freshwater resources, forestry and human health.”
When funds are mobilised across all sectors (summarised in Table 2]), the gap between funding approved and funding disbursed suggests bottlenecks in program implementation [16]. Although the Least Developed Countries Fund (LDCF) has approved the largest volume of adaptation finance for SSA to date, the funding is unevenly distributed across sectors. Table 3 shows that only 4% of funds are allocated to the health sector [17].
Tab. 2. 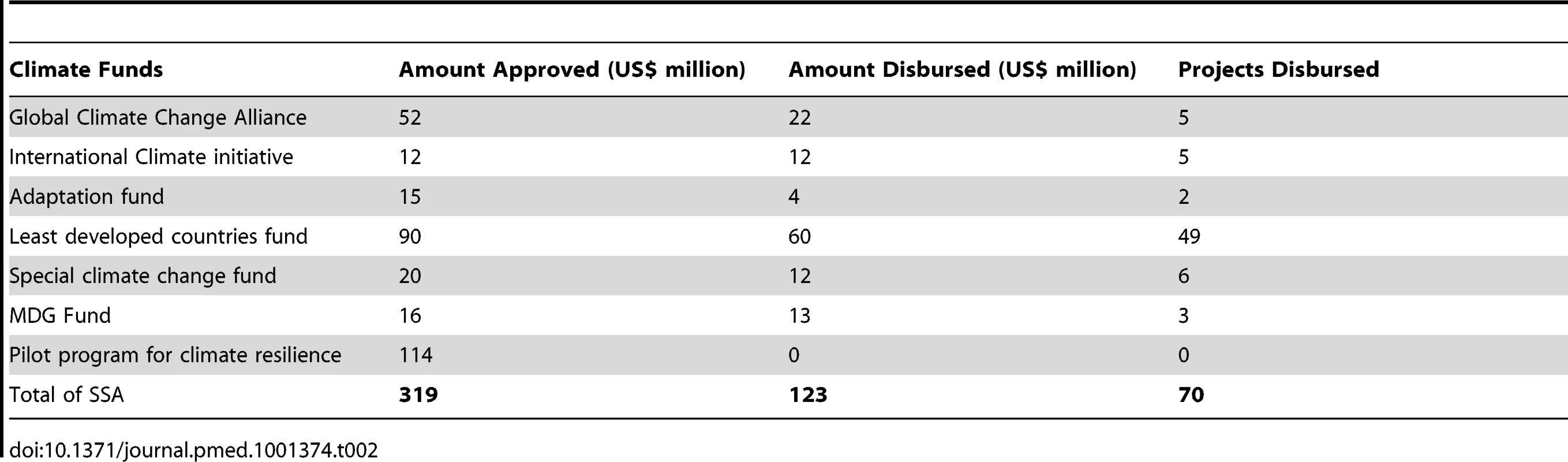
Contributions of dedicated climate funds monitored by CFU to adaptation in sub-Saharan Africa <em class="ref">[16]</em>. Tab. 3. 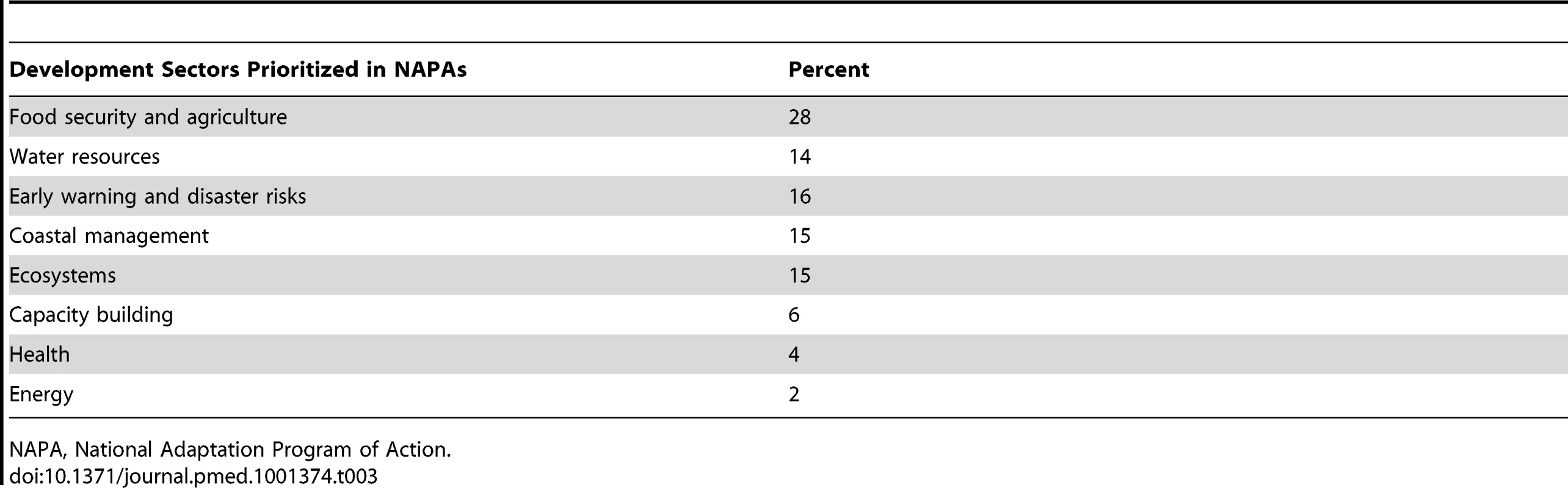
Prioritization of funding in least developed countries <em class="ref">[23]</em>. More Urgent Action Is Required To Build Capacity To Respond To Climate Change And Variability
Building An Evidence Base
A review of health sector policy options for health adaptation [18] lists a range of specific actions that the health sector should undertake to reduce cases of disease and deaths attributable to climate change (Box 1). For example, SSA countries need to establish the vulnerability of existing populations to climate-sensitive health risks [12] and plan adaptation on the basis of detailed assessments of national vulnerabilities to specific health risks [19]. Research infrastructure in many African settings needs to be improved and investments need to be made to strengthen networks of institutions to conduct cross-disciplinary work between meteorology/climatology, other relevant sectors and health, building on what has already started [20]. Research is required to enhance understanding of the health effects of climate change in different settings within SSA and to generate and disseminate knowledge on appropriate local adaptation measures.
Box 1. Examples Of Health Sector Policy Options For Adaptation To Climate Change [17]
-
Improving, modifying, or expanding health protection systems including surveillance systems for vector - and water-borne diseases and, seasonal forecasting and early warning systems for infectious diseases (e.g., epidemic malaria).
-
Developing and implementing health forecasting and early warning systems (including emergency incident response plans) for extreme events such as heat - and flood-health warning measures.
-
Maintaining and improving current environmental health regulatory standards (e.g., water and air quality standards).
-
Improving or modifying health systems infrastructure by adapting hospitals and clinics to increased frequency of extreme weather events such as heat waves and floods.
-
Increasing the capacity of health care services and human resources to cope with additional disease burden associated with extreme weather events.
-
Preventing or treating the additional cases of diseases due to failure in adaptation upstream.
-
Improving the provision of medication to reduce the impact of potential increases in infectious disease transmission.
Keeping A Focus On Health And Health Systems
A range of empirical studies demonstrate that advancing broader development goals is a crucial pre-requisite for an effective climate change response [21]. WHO suggests that health-system actions that can also protect populations from the impacts of climate change should encompass public health interventions, such as control of neglected tropical diseases and provision of primary health care, and actions to address the environmental and social determinants of health [19]. There is a strong case for prioritising these factors that determine how well the health system will respond to impacts of climate on health. For example it will be important to consider how health facilities and supply chains may be affected by climate extremes—floods, storms, droughts, and heat waves—and how they can be made more resilient.
Promoting The Health Benefits Of Low Carbon Strategies
“Health co-benefits” is the term used to describe the ancillary benefits to health as a result of climate change mitigation strategies [22]. There are significant win-win options that can reduce greenhouse gas emissions as well as contribute to better health. Many measures to reduce greenhouse gas emissions in household energy, transport, food, and agriculture and electricity generation have substantial health benefits [23]. To achieve mitigation with a health dividend, policy makers will need to prioritize increased active transport (walking and cycling) public transport systems and reduced private-car use in urban settings, increased uptake of improved cooking stoves in low-income countries, reduced consumption of animal products in high-consumption settings, and generation of electricity from affordable, clean, “low-carbon” sources, as well as avoidance of highly polluting biomass [24]. These strategies can address major health problems such as child mortality from acute respiratory infections, ischaemic heart disease in adults, and other non-communicable diseases such as obesity, diabetes, and depression.
Increase Funding For Work On Climate Change And Health
With less than 4% of funds currently allocated to health protection, and given the region's vulnerability, there is a compelling case for SSA to receive significant funding for additional health adaptation. This should be targeted at building a stronger evidence base for future policy makers and documenting specific actions that will enhance adaptation to climate change together with low carbon strategies that will also benefit health.
Conclusions
There is a need to rapidly build the adaptive capacity in existing health institutions in SSA, and to develop a stronger evidence base for local adaptation strategies in vulnerable sectors such as health. Such action will also assist the region to successfully access additional adaptation funding that may be available. The health sector needs to engage in partnerships with other organizations and sectors to ensure that health concerns are adequately integrated into the work of national climate change adaptation committees, National Adaptation Programmes of Action, and regional and international adaptation and mitigation strategies. This collaboration should include more recognition of the potential ancillary benefits to health from low carbon development.
Zdroje
1. Nakhooda S, Caravani A, Neil Bird, Schalatek L (2011) Climate finance fundamentals: regional briefing for Sub Saharan Africa. Heinrich Böll Stiftung North America and the Overseas Development Institute (ODI). Available: http://www.odi.org.uk/resources/docs/7474.pdf. Accessed 4 December 2012.
2. African Development Bank (2011) The cost of adaptation to climate change in Africa. Available: http://www.afdb.org/fileadmin/uploads/afdb/Documents/Project-and-Operations/Cost%20of%20Adaptation%20in%20Africa.pdf. Accessed 4 December 2012.
3. WHO (2008) Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: WHO.
4. ByassP (2009) Climate change and population health in Africa: where are the scientists? Glob Health Action 2 doi:10.3402/gha.v2i0.2065
5. HaySI, RogersDJ, RandolphSE, SternDI, CoxJ, et al. (2002) Hot topic or hot air? Climate change and malaria resurgence in East African highlands. Trends Parasitol 18 : 530–534.
6. OmumboJA, WaweruSM, OmumboJA, LyonB, ThomsonMC, et al. (2011) Raised temperatures over the Kericho tea estates: revisiting the climate in the East African highlands malaria debate. Malar J 10 : 12.
7. United Nations Economic Commission for Africa (UNECA) (2011) African Climate Policy Centre. Climate change and health across Africa: issues and options. Working paper 20 November 2011. New York: UNECA.
8. GethingPW, SmithDL, PatilAP, TatemAJ, SnowRW, et al. (2010) Climate change and the global malaria recession. Nature 465 : 342–345.
9. Nerlander L (2009) Commission on Climate and Development. Climate change and health. Available: http://www.ccdcomission.org. Accessed 4 December 2012.
10. FunkC, DettingerMD, MichaelsenJC, VerdinJP, BrownME, et al. (2008) Warming of the Indian Ocean threatens eastern and southern African food security but could be mitigated by agricultural development. Proc Natl Acad Sci U S A 105 : 11081–11086.
11. Economic Report on Africa (2008) Africa and the Monterrey Consensus: tracking performance and progress. Development challenges for Africa in 2007. Chapter 3: New York: UNECA.
12. WHO Regional Committee for Africa (2011) Framework for public health adaptation to climate change in the Africa Region. Sixty-first session; Yamoussoukro, Côte d'Ivoire, 29 August–2 September 2011.
13. WHO UNEP (2011) Adaptation to climate change in Africa, plan of action for the health sector 2012–2016. Geneva: WHO.
14. Manga L, Bagayoko M, Meredith T, Neira M (2010) Overview of health considerations within National Adaptation programmes of Action for climate change in least developed countries and small island states. Available: http://www.who.int/phe/Health_in_NAPAs_final.pdf. Accessed 4 December 2012.
15. Adaptation partnership (2011) Review of current and planned adaptation action: Southern Africa. Available: http://www.adaptationpartnership.org/…/Southern_Africa_Adaptation. Accessed 4 December 2012.
16. Climate Funds Update (2012) Climate Funds Update website. Available: http://www.climatefundsupdate.org/. Accessed 4 December 2012.
17. Global Environmental Facility (2012) Least developed countries fund (LDCF). Available: http://www.thegef.org/gef/LDCF. Accessed 4 December 2012.
18. Chalabi Z, Kovats S (2011) MCA4climate: a practical framework for planning pro-development climate policies adaptation theme report: reducing human health impacts and risks. UNEP, 2011 Available: http://www.mca4climate.info. Accessed 4 December 2012.
19. WHO (2012) WHO work plan for climate change and human health. Available: http://www.who.int/globalchange/health_policy/who_workplan/en/index.html on 28 May 2012. Accessed 4 December 2012.
20. WHO and World Meteorological Organisation (2012) Atlas of health and climate. Geneva: WHO
21. HessJJ, McDowellJZ, LuberG (2012) Integrating climate change adaptation into public health practice: using adaptive management to increase adaptive capacity and build resilience. Environ Health Perspect 120 : 171–179.
22. Intergovernmental Panel on Climate Change. Climate Change 2007: Working Group III: Mitigation of Climate Change. Available: http://www.ipcc.ch/publications_and_data/ar4/wg3/en/ch7s7-10.html. Accessed 4 December 2012.
23. HainesA, McMichaelAJ, SmithKR, RobertsI, WoodcockJ, et al. (2009) Public health benefits of strategies to reduce greenhouse-gas emissions: overview and implications for policy makers. Lancet 374 : 2104–2114.
24. HainesA, WilkinsonP, TonneC, RobertsI (2009) Aligning climate change and public health policies. Lancet 374 : 2035–2038.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 1- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Magnosolv a jeho využití v neurologii
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- More Data and Appropriate Statistical Methods Needed to Fully Measure the Displacement Effects of Development Assistance for Health
- Preventing Antiretroviral Treatment Interruptions among HIV/AIDS Patients in Africa
- Translating Coverage Gains into Health Gains for All Women and Children: The Quality Care Opportunity
- Implementation of a Mental Health Care Package for Children in Areas of Armed Conflict: A Case Study from Burundi, Indonesia, Nepal, Sri Lanka, and Sudan
- Toward an Understanding of Disengagement from HIV Treatment and Care in Sub-Saharan Africa: A Qualitative Study
- Tackling Non-Communicable Diseases In Low- and Middle-Income Countries: Is the Evidence from High-Income Countries All We Need?
- Change in the Body Mass Index Distribution for Women: Analysis of Surveys from 37 Low- and Middle-Income Countries
- Getting More Generous with the Truth: Clinical Trial Reporting in 2013 and Beyond
- Reducing Vulnerability to Climate Change in Sub-Saharan Africa: The Need for Better Evidence
- Erectile Dysfunction Severity as a Risk Marker for Cardiovascular Disease Hospitalisation and All-Cause Mortality: A Prospective Cohort Study
- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
- Considerations in Assessing the Evidence and Implications of Aid Displacement from the Health Sector
- Prioritizing Congenital Syphilis Control in South China: A Decision Analytic Model to Inform Policy Implementation
- Balancing Community and Hospital Care: A Case Study of Reforming Mental Health Services in Georgia
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



