-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaPrioritizing Congenital Syphilis Control in South China: A Decision Analytic Model to Inform Policy Implementation
Background:
Syphilis is a major public health problem in many regions of China, with increases in congenital syphilis (CS) cases causing concern. The Chinese Ministry of Health recently announced a comprehensive 10-y national syphilis control plan focusing on averting CS. The decision analytic model presented here quantifies the impact of the planned strategies to determine whether they are likely to meet the goals laid out in the control plan.Methods and Findings:
Our model incorporated data on age-stratified fertility, female adult syphilis cases, and empirical syphilis transmission rates to estimate the number of CS cases associated with prenatal syphilis infection on a yearly basis. Guangdong Province was the focus of this analysis because of the availability of high-quality demographic and public health data. Each model outcome was simulated 1,000 times to incorporate uncertainty in model inputs. The model was validated using data from a CS intervention program among 477,656 women in China. Sensitivity analyses were performed to identify which variables are likely to be most influential in achieving Chinese and international policy goals. Increasing prenatal screening coverage was the single most effective strategy for reducing CS cases. An incremental increase in prenatal screening from the base case of 57% coverage to 95% coverage was associated with 106 (95% CI: 101, 111) CS cases averted per 100,000 live births (58% decrease). The policy strategies laid out in the national plan led to an outcome that fell short of the target, while a four-pronged comprehensive syphilis control strategy consisting of increased prenatal screening coverage, increased treatment completion, earlier prenatal screening, and improved syphilis test characteristics was associated with 157 (95% CI: 154, 160) CS cases averted per 100,000 live births (85% decrease).Conclusions:
The Chinese national plan provides a strong foundation for syphilis control, but more comprehensive measures that include earlier and more extensive screening are necessary for reaching policy goals.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(1): e32767. doi:10.1371/journal.pmed.1001375
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001375Summary
Background:
Syphilis is a major public health problem in many regions of China, with increases in congenital syphilis (CS) cases causing concern. The Chinese Ministry of Health recently announced a comprehensive 10-y national syphilis control plan focusing on averting CS. The decision analytic model presented here quantifies the impact of the planned strategies to determine whether they are likely to meet the goals laid out in the control plan.Methods and Findings:
Our model incorporated data on age-stratified fertility, female adult syphilis cases, and empirical syphilis transmission rates to estimate the number of CS cases associated with prenatal syphilis infection on a yearly basis. Guangdong Province was the focus of this analysis because of the availability of high-quality demographic and public health data. Each model outcome was simulated 1,000 times to incorporate uncertainty in model inputs. The model was validated using data from a CS intervention program among 477,656 women in China. Sensitivity analyses were performed to identify which variables are likely to be most influential in achieving Chinese and international policy goals. Increasing prenatal screening coverage was the single most effective strategy for reducing CS cases. An incremental increase in prenatal screening from the base case of 57% coverage to 95% coverage was associated with 106 (95% CI: 101, 111) CS cases averted per 100,000 live births (58% decrease). The policy strategies laid out in the national plan led to an outcome that fell short of the target, while a four-pronged comprehensive syphilis control strategy consisting of increased prenatal screening coverage, increased treatment completion, earlier prenatal screening, and improved syphilis test characteristics was associated with 157 (95% CI: 154, 160) CS cases averted per 100,000 live births (85% decrease).Conclusions:
The Chinese national plan provides a strong foundation for syphilis control, but more comprehensive measures that include earlier and more extensive screening are necessary for reaching policy goals.
Please see later in the article for the Editors' SummaryIntroduction
Congenital syphilis (CS) has reemerged in China as a common, preventable cause of stillbirth, neonatal death, low birth weight, and irreversible congenital malformations [1]–[4]. In response to the resurgent syphilis epidemic, the Chinese Ministry of Health recently announced a comprehensive 10-y National Syphilis Prevention and Control Plan (NSCP). Averting CS cases stands at the center of this mandate, with explicit strategies that focus on improving prenatal syphilis screening coverage (target of 80% coverage in urban areas and 60% coverage in rural areas), increasing treatment rates in infected pregnant woman (target of 90% coverage in urban areas and 70% coverage in rural areas), and increasing syphilis awareness among adults [5]. The NSCP aims to reduce the number of newly reported CS cases to less than 30 cases per 100,000 live births by 2015 and to less than 15 cases per 100,000 live births by 2020. In 2009, there were 139 reported CS cases per 100,000 live births. The 2015 goal represents a 78.4% reduction from the 2009 reported caseload. The 2015 goal is consistent with recommendations from a working group led by the World Health Organization (WHO) and critical to achieving the 2020 objective of fewer than 15 CS cases per 100,000 live births [6]. Prioritizing policy strategies and understanding the key drivers of adverse outcomes associated with syphilis in pregnancy are essential for meeting these policy goals.
The lack of population-based data on adverse outcomes associated with syphilis infection during pregnancy in China has generated ambiguity about the extent of this public health problem and the organization of optimal control strategies. Although syphilis is associated with other adverse outcomes (neonatal death, premature birth, and low birth weight), this study focused on measuring CS cases because of the availability of robust data and a direct connection to NSCP goals [1]–[4]. Decision analytic methods provide a quantitative foundation for understanding the scope of CS in China and have been widely used to explore syphilis burden in other contexts [7],[8]. Drawing on empirical Chinese studies, adult syphilis case rates, and age-stratified fertility data, we estimate the reduction in CS burden among pregnant women with syphilis in Guangdong Province, China, with the expectation of achieving NSCP goals.
Methods
Analytic Overview
Based on published literature and Guangdong surveillance data, a decision analytical tree approach was used to model the acquisition and natural history of syphilis from infection to pregnancy to congenital birth outcomes. The Chinese case definition of CS was used, requiring positive treponemal and non-treponemal serologies in addition to a consistent clinical history. The decision analytical model consists of sequences of possible health states that simulate the pathways leading to CS within a population (Figure 1). Each health transition state is separated from other states by a transition state probability (Table 1). The decision analytical model consists of four main health events: syphilis acquisition, pregnancy, prenatal screening, and birth outcome.
Fig. 1. Decision analytic model. 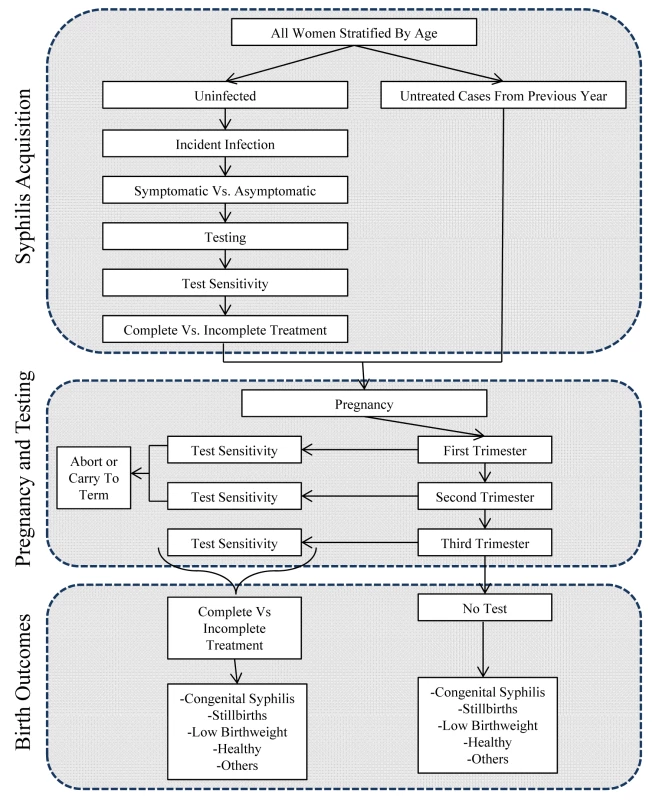
The figure illustrates the series of transition states leading to various adverse birth outcomes attributable to CS. Tab. 1. Transition state probabilities with uncertainty. 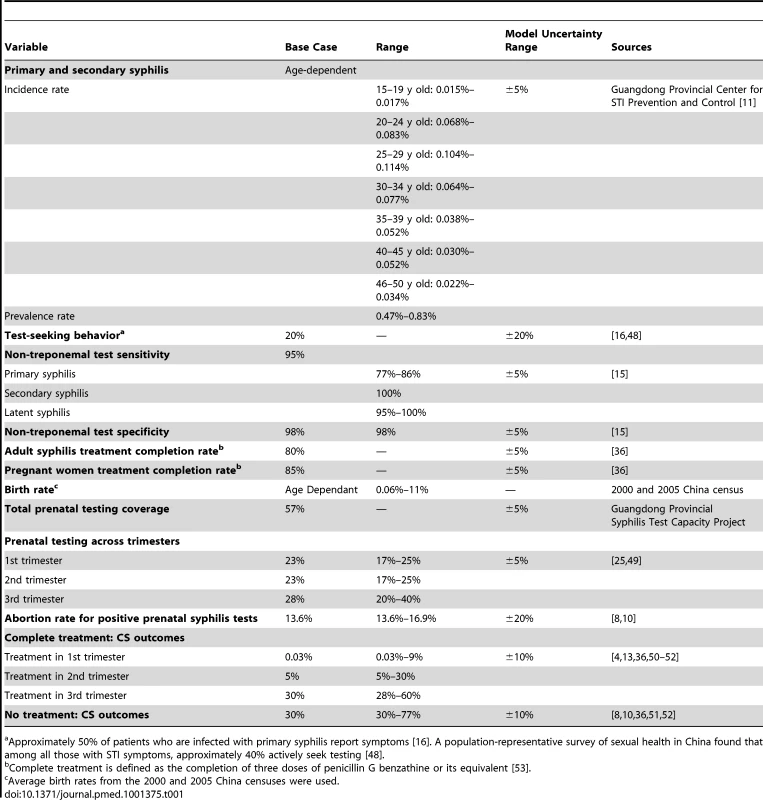
Approximately 50% of patients who are infected with primary syphilis report symptoms [16]. A population-representative survey of sexual health in China found that among all those with STI symptoms, approximately 40% actively seek testing [48]. The cycle length for the model simulation was 1 y. Within each year, the female population was stratified into seven age groups: 15–19 y old, 20–24 y old, 25–29 y old, 30–34 y old, 35–39 y old, 40–44 y old, and 45–49 y old. The total estimated CS burden was the sum of infants with CS born to pregnant women across all seven age groups.
The model was validated both internally and externally according to International Society for Pharmacoeconomics and Outcomes Research modeling guidelines [9], using, respectively, Guangdong syphilis surveillance data from years 2005 to 2008 and empirical data from a CS intervention program in Guangdong Province that screened 477,656 pregnant women citywide from 2002 to 2005 [10]. For both validation exercises, the set of the data used for validation purposes was separate from data used for later input parameter estimates.
Model
The decision analytic model was built and programmed using TreeAge Pro 2011 (TreeAge Software). Women entered the model through one of two possible starting states—uninfected or infected. The proportion of women in each starting state was determined by syphilis prevalence, represented by provincial data on syphilis burden per 100,000 people.
For uninfected women, the probability of acquiring syphilis was represented by the primary and secondary syphilis incidence rates. All sexually transmitted infection (STI) data for syphilis were obtained from the province-wide mandatory reporting system organized by the Guangdong Provincial Center for STI Prevention and Control [11].
Data
Table 1 lists the transition state probabilities used in the decision analytic model and respective data ranges. The base case was based on disease and demographic data from 2009. Conservative parameter estimates were used for base case values but were varied across the upper and lower ranges of reported values and values from sensitivity analyses to ensure that the results were robust. Syphilis prevalence rates refer to primary and secondary syphilis cases. Latent and tertiary syphilis cases were excluded because mother–child transmission rates are very low for these stages. Treatment completion was defined as three doses of penicillin G benzathine or its equivalent. Whenever possible, we used data from randomized controlled trials and epidemiologic studies specific to the population under evaluation. In addition, model inputs were drawn from Chinese studies. We drew from a large body of literature pertaining to the natural history and epidemiology of syphilis in pregnancy, using data from large and high-quality studies. Incidence and prevalence rates utilized as model inputs were predominantly from urban clinics, where there is a greater burden of syphilis and better infrastructure to respond to diagnosed cases. In instances where data specific to the analysis population were limited, relevant applicable data from the literature for populations that most closely approximated our study population characteristics, while providing the best available parameter estimate, were used.
Sensitivity analyses
We performed 1,000 simulations using parameter values randomly sampled from uniform distributions between the upper and lower ranges of all health state variables to ensure that the model was stable and robust (ranges used are shown in Table 1). For model parameters obtained from strong, geographically relevant, empirical sources (e.g., syphilis incidence rates, test sensitivity and specificity, treatment completion, testing coverage, and time of testing), a ±5% uncertainty interval was applied. For the CS outcome probability, a ±10% uncertainty interval was applied because there was some variation from study to study, although all studies considered were Chinese studies. For behavioral measures that lacked reliable and accurate data (e.g., test-seeking behavior and abortion rate), a ±20% uncertainty interval was applied. For each individual policy strategy (see “Strategies” below), the percent reduction was computed; the point estimate was the mean of these percent reduction estimates. The confidence interval was taken from the 2.5th and 97.5th percentiles. Policy strategy, CS outcome probability, and prevalence rate were the only health state variables that resulted in more than a 4% change in the number CS cases.
In addition, sensitivity analyses were performed on all variables that corresponded to each policy strategy. The individual policy strategies that were associated with the largest number of CS cases averted were identified. Multivariate sensitivity analyses were then performed to identify the combinations of individual strategies associated with the greatest decreases in CS cases.
Validation exercises
Two exercises were used to validate the model, involving 2005–2008 CS incidence in Guangdong Province and a CS intervention program in Shenzhen City.
Internal Validation: Historical Guangdong Province Reported CS Cases
After model testing and debugging, an internal validation was performed with data for a 4-y period (2005–2008) from the Guangdong Provincial Center for STI Prevention and Control. This constitutes an internal validation because data exist on both model inputs (demographic data and adult syphilis incidence and prevalence rates) and model outputs (incident annual CS cases) over the same time period [9]. This time period was chosen because there were major administrative changes in reporting from 2003 to 2004 [12]. Demographic data, adult syphilis incidence rates, and adult syphilis prevalence rates for each respective year were used. Demographic data consisted of birth rates and female population sizes for each age-stratified group obtained from the 2000 and 2005 China censuses. Adult syphilis incidence and adult syphilis prevalence rates were obtained from the Guangdong Provincial Center for STI Prevention and Control [11]. The number of reported CS cases was divided by the number of estimated CS cases to calculate reporting rates. The validation exercise showed similar trends for model estimates and reported CS cases across all 4 y, with reporting rates of 54%, 69%, 78%, and 82% for 2005, 2006, 2007, and 2008, respectively. Reporting rates from 2005 to 2008 were stable, with an average reporting rate of 71% (95% CI: 59%, 83%).
External Validation: Shenzhen CS Intervention Program
The model was validated against published data from a CS intervention among 477,656 pregnant women in Shenzhen. This external validation tested the model outcomes against a pilot study conducted in a Guangdong city. Model inputs were obtained from Cheng et al. [10] and did not include inputs used to make base case model assumptions. From 2002 to 2005, the Shenzhen government initiated a citywide syphilis prevention program for pregnant women to curb the sharp rise in CS cases [10]. The program provided free syphilis screening, treatment, and follow-up for all pregnant women. Demographic data, prenatal screening coverage, syphilis prevalence and incidence rates, and treatment completion rates that were specific to Shenzhen were inputted into the decision analytic model [8],[10],[13],[14]. Data used for validation of the model consisted of a subset of the original data that was not used for producing policy parameter estimates. Shenzhen demographic data were obtained from the 2000 and 2005 China censuses. Shenzhen adult syphilis incidence rates were obtained from the Guangdong Provincial Center for STI Prevention and Control. The adult syphilis prevalence in Shenzhen was obtained from a published study that investigated syphilis in many populations [14]. The intervention program increased prenatal screening coverage to 94% and the treatment completion rate to 92%. Based on all of the above inputs, the model estimated 29 (95% CI: 28, 30) CS cases per 100,000 live births over the course of the entire Guangdong CS intervention program, compared to the 27 (95% CI: 24, 30) cases per 100,000 reported in the empirical data, after accounting for loss to follow-up. This represents a difference of 7% between the model and the empirical Shenzhen data.
Strategies
The NSCP approach focuses on four main strategies [5]: running educational campaigns aimed at educating the public on safer sex practices to decrease syphilis incidence rates, increasing prenatal screening coverage, increasing treatment completion rates in rural and urban places, and improving the medical knowledge and skills of health professionals. In addition to these four strategies, we investigated three strategies that have been successful in other countries and settings [4]: increasing the percentage of pregnant women who receive syphilis testing early, i.e., in the first and second trimester; introducing new testing technologies that might improve test sensitivity and specificity; and running educational campaigns aimed at reducing the social stigma associated with STIs and promoting recognition of syphilis symptoms among the general adult population, to increase test-seeking rates.
The number of CS cases expected with the isolated implementation of each policy strategy was estimated. Single policy strategies were combined into combination strategies, and all possible combinations were explored. Analyzing the CS case reductions from combined strategies is crucial because the overall outcome from combination strategies depends on the interaction between individual strategies. The reduction in the number of CS cases that would result from the successful implementation of the NSCP was computed and compared against NSCP and WHO targets, and against the combination policies that resulted in the highest CS case reductions. This analysis enables the advocacy of effective strategies outside of the scope of the NSCP.
Results
Base Case Results
The base case year 2009 had a model estimate of 2,079 new CS cases, corresponding to 184 (95% CI: 172, 196) CS cases per 100,000 live births. Given the 1,567 CS cases reported by the Guangdong Provincial Center for STI Prevention and Control surveillance system, this represents an estimated reporting rate of 75.5% if the model estimate is correct. Table 1 includes all base case model inputs used in this analysis. Conservative inputs within the respective input ranges were used to avoid the possibility of overestimating CS cases.
One-Way Sensitivity Analyses: Single CS Policy Strategies
Total prenatal screening coverage
Increasing prenatal screening coverage to 95% was the most influential individual strategy in reducing CS burden (Table 2). In 2009, the estimated coverage for screening of pregnant women was 57%, with an estimated 184 (95% CI: 172, 196) CS cases per 100,000 live births. Increasing prenatal screening coverage to 95% while leaving all other aspects of the 2009 model inputs constant resulted in an estimated 78 (95% CI: 73, 83) CS cases per 100,000 live births. This policy strategy alone averted 58% (95% CI: 55, 60) of CS cases compared to the base case. Figure S1 shows the linear relationship between increasing prenatal screening coverage and total CS cases over a range of values.
Tab. 2. Summary of estimated outcomes with parameters from the base case scenario, single CS policy strategies, and combination strategies. 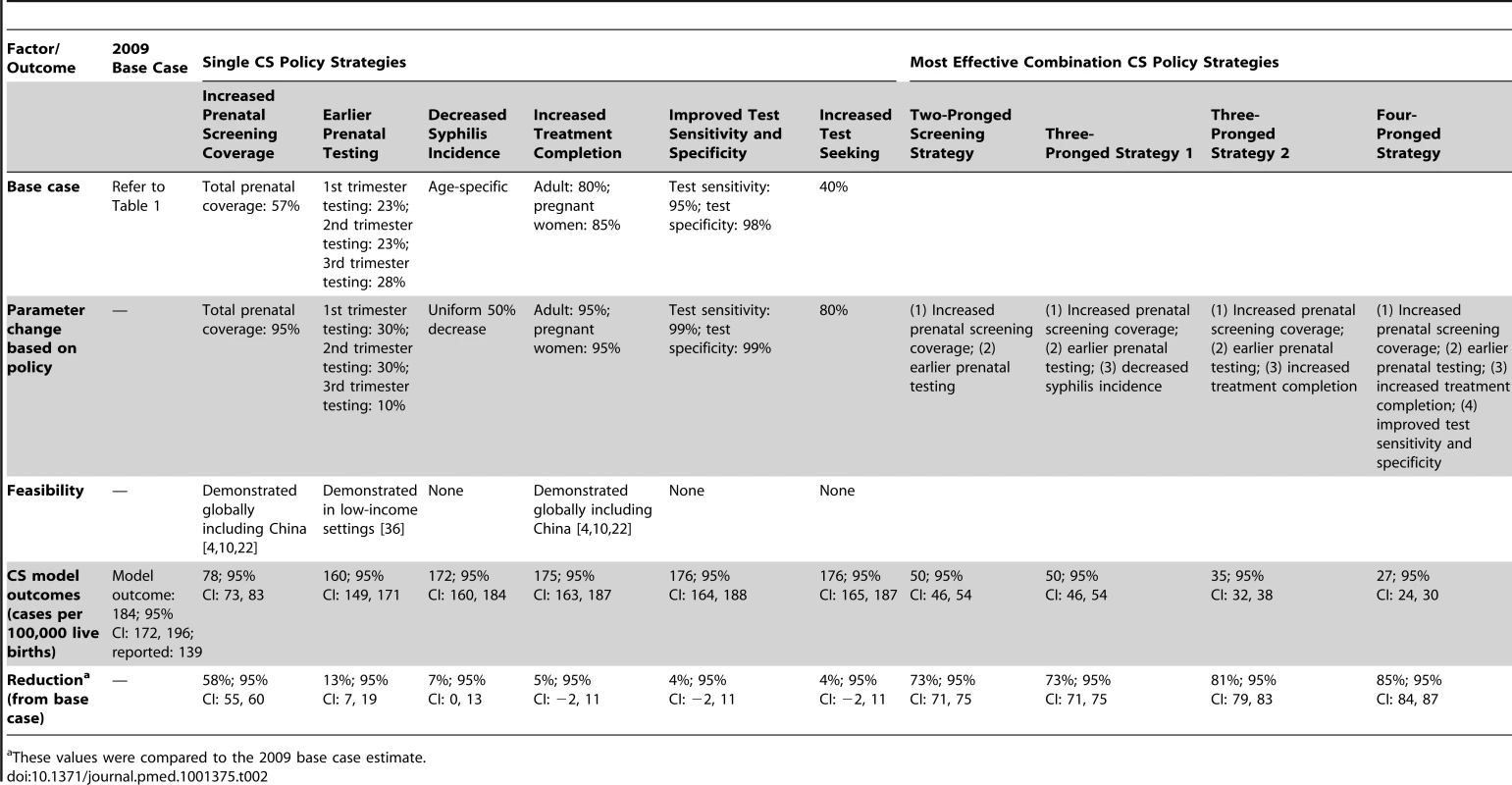
These values were compared to the 2009 base case estimate. Earlier prenatal screening
The second most influential individual strategy was earlier prenatal screening. The proportion of women screened during their first trimester and second trimester was increased from 23% to 30% while holding total prenatal coverage constant at the base case value of 57%. Third trimester screening was reallocated to the first and second trimesters to keep the total prenatal screening coverage constant. Hence, this measure isolates the effect of reaching out to already accessible women earlier in their pregnancy without increasing testing coverage or affecting other variables. This strategy was associated with 160 (95% CI: 149, 171) CS cases per 100,000 births and a 13% (95% CI: 7, 19) reduction compared to the base case (Table 2).
Syphilis incidence
The third most influential individual strategy was decreasing adult syphilis incidence, a strategy in which the NSCP has substantially invested. Syphilis incidence was decreased by 100% to 0% in the model, and it was found that after the 50% point, CS case reductions were negligible. Hence a 50% decrease was used as the maximum policy parameter target. This strategy was associated with 172 (95% CI: 160, 184) CS cases per 100,000 births and a 7% (95% CI: 0, 13) reduction compared to the base case (Table 2).
Treatment completion
The fourth most influential individual strategy was increasing treatment completion rates. Treatment completion rate is defined as the portion of pregnant women with syphilis overall who receive three doses of penicillin G benzathine or its equivalent. The treatment completion rate for pregnant women was increased in the model from 85% to 95%, while the treatment completion rate for all non-pregnant adults was increased from 80% to 95%. This strategy was associated with 175 (95% CI: 163, 187) CS cases per 100,000 births and a 5% (95% CI: −2, 11) reduction compared to the base case (Table 2).
Test sensitivity and specificity
The fifth most influential individual strategy was improving test sensitivity and specificity. Current non-treponemal test sensitivity and specificity are 95% and 98%, respectively [15]. This policy parameter aims to increase both test sensitivity and specificity to 99%, which is the upper limit demonstrated in US Centers for Disease Control and Prevention studies [15]. This strategy was associated with 176 (95% CI: 164, 188) CS cases per 100,000 births and a 4% (95% CI: −2, 11) reduction compared to the base case (Table 2).
Test-seeking behavior among adult population
The least influential policy strategy was increasing test-seeking behavior. Test-seeking behavior is limited by biological symptoms, with only 50% of patients infected with primary and secondary syphilis reporting symptoms [16]. Test-seeking behavior was increased from 40% to 100%. When test seeking reached 80%, it resulted in the greatest CS case reductions, but above that point, increases in test seeking resulted in negligible CS case reductions.
Multi-Way Sensitivity Analyses: Combination CS Policy Strategies
We performed multi-way sensitivity analyses to identify the combinations of strategies that averted the most CS cases for multi-pronged policy strategies. Feasibility was also taken into account when developing combination CS policy strategies. All combinations of two-pronged, three-pronged, four-pronged, and five-pronged strategies were tested. The most effective combinations are reported (Table 2). No five-pronged policy strategy reduced more CS cases than the most effective four-pronged combination.
Two-pronged strategy
The two-pronged strategy that averted the most CS cases consisted of increased prenatal screening coverage and earlier prenatal testing, which were also the two most influential individual strategies. Prenatal screening coverage was increased from 57% to 95% and prenatal screening was performed 75% of the time in the first and second trimester. This screening strategy was associated with 50 (95% CI: 46, 54) CS cases per 100,000 births and a 73% (95% CI: 71, 75) reduction compared to the base case (Table 2; Figure 2).
Fig. 2. National syphilis control plan and combination strategy estimated outcomes with 95% CIs. 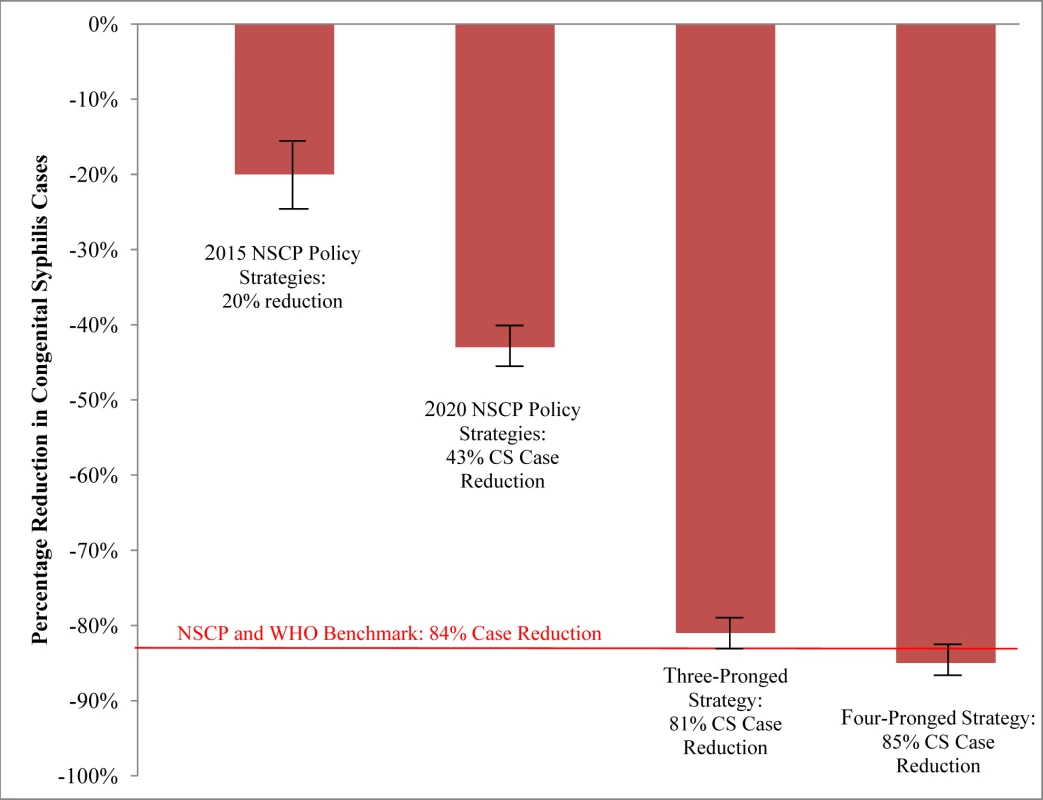
The three-pronged strategy consists of increased prenatal screening coverage, earlier prenatal testing, and increased treatment completion rate. The four-pronged strategy consists of increased prenatal screening coverage, earlier prenatal testing, increased treatment completion rate, and increased test sensitivity and specificity. These values were compared to the 2009 base case estimate. Three-pronged strategy
The three-pronged strategy that averted the most CS cases consisted of increased prenatal screening coverage, earlier prenatal testing, and increased treatment completion. Total prenatal screening coverage was increased from 57% to 95%, prenatal screening was performed 75% of the time in the first and second trimester, and treatment completion rates were 95%. This three-pronged strategy was associated with 35 (95% CI: 32, 38) CS cases per 100,000 births and an 81% (95% CI: 79, 83) reduction compared to the base case (Table 2; Figure 2).
The three-pronged strategy that averted the second most CS cases consisted of increased prenatal screening coverage, earlier prenatal testing, and decreased adult syphilis incidence. Prenatal screening coverage metrics were similar to the above, and syphilis incidence was decreased by 50%. This three-pronged strategy was associated with 50 (95% CI: 46, 54) CS cases per 100,000 births and a 73% (95% CI: 71, 75) reduction compared to the base case (Table 2; Figure 2).
Four-pronged strategy
The four-pronged strategy that averted the most CS cases consisted of increased prenatal screening coverage, earlier prenatal testing, increased treatment completion, and improved test sensitivity and specificity. Total prenatal screening coverage was increased from 57% to 95%, prenatal screening was performed 75% of the time in the first and second trimester, treatment completion rates were 95%, and test sensitivity and specificity were 99%. This four-pronged strategy was associated with 27 (95% CI: 24, 30) CS cases per 100,000 live births and an 85% reduction (95% CI: 84, 87) compared to the base case. This was the only strategy that met the WHO and NSCP target of less than 30 CS cases per 100,000 live births.
Comparison to national syphilis control plan combination strategies
Based on the 2015 and 2020 NSCP strategies laid out by the Chinese Ministry of Health, parameter values were extracted and input into the decision analytic model (Table 2). These parameter changes include incrementally increasing prenatal screening coverage to 86%, incrementally increasing treatment completion rates to 92%, and decreasing incidence rates. The NSCP policies were effective in reducing the number of CS cases to 148 and 105 CS cases per 100,000 live births for the years 2015 and 2020, respectively (Figure 2). Implementing the 2015 policy strategies in the model reduced the CS caseload by 20%, while implementing the 2020 policy strategies reduced the CS caseload by an additional 23%. Figure 2 compares the estimated reduction expected from implementing NSCP strategies with their goals, and illustrates that NSCP strategies alone are insufficient to achieve the desired goals. The four-pronged approach that consisted of increased prenatal syphilis testing, earlier screening, higher treatment completion rate, and increased test specificity and sensitivity was able to achieve the WHO benchmark of <30 CS cases per 100,000 live births.
Discussion
Our model suggests that prenatal syphilis screening coverage is the single most important component of CS control, but several other strategies, including earlier screening and improved treatment completion, are needed to achieve targets established by the Chinese government. Increasing prenatal screening coverage to 95% resulted in an estimated 78 (95% CI: 73, 83) CS cases per 100,000 live births, compared to the estimated 184 (95% CI: 172, 196) CS cases per 100,000 live births with current screening coverage (57%). Catalyzed by momentum from the NSCP and subsequent increased local resources for syphilis control, China is uniquely positioned to implement far-reaching CS control programs that could have a major impact on maternal and child health [17]. While previous studies have analyzed the relationship between screening coverage and CS cases [10],[18], to our knowledge this is the first study to analyze the relative contribution of individual and comprehensive strategies to overall syphilis control, and the first syphilis control model with empirical validation datasets available, representing a substantial improvement on earlier studies.
Our analysis suggests that improving prenatal syphilis screening is the most important individual component of CS control. This is likely related to suboptimal baseline screening and the critical position of screening in downstream control efforts [19],[20]. Although there have been reports of duplicate reporting of cases and misdiagnosis in China [12], our findings are consistent with net underreporting, with an estimated reporting rate of 75.5%. Some reasons for underreporting include misdiagnosis, lack of CS testing, and non-hospital deliveries. Our model input parameters were conservative and did not account for the underreporting of adult syphilis cases or birth rates [21], and hence CS case outcomes are likely to be an underestimation. While other studies have modeled syphilis screening as part of a comprehensive strategy [4], the relative contribution of screening has not been investigated to date. Achieving 95% screening coverage rates in prenatal settings exceeds the Chinese policy goals of 60% screening coverage in rural areas and 80% screening coverage in urban areas. The 95% screening coverage target is not only necessary but feasible, and has been implemented in similar rural and urban settings. The pilot study in urban Shenzhen City achieved 94% prenatal screening coverage, while another study conducted in rural Guangdong achieved 96% prenatal screening coverage [10],[22]. Globally, greater than 90% prenatal screening coverage rates have been implemented in pilot programs in several low - and middle-income countries [4],[22]. A simple, inexpensive, rapid on-site syphilis test has been rolled out in China and could help realize the universal syphilis screening required at hygiene stations and other low-level prenatal clinics that may not be able to implement non-treponemal syphilis screening [23], but improvement in point-of-care test sensitivity is needed. A United Nations report in 2010 estimated that there is 92% antenatal care coverage across China and suggested the feasibility of expanding syphilis screening coverage across China [24].
Next, earlier syphilis treatment is a critical variable for averting CS burden. Previous models of syphilis control have not explicitly targeted first and second trimester syphilis screening [4],[7],[8]. Many pregnant women in China initiate prenatal care late in pregnancy [25]. Earlier prenatal care would be useful not only for syphilis screening, but also for routine prenatal care [26]–[28]. Treatment in the third trimester is minimally effective in reducing CS transmission to the infant [29]–[32] because much of vertical syphilis transmission occurs prior to the third trimester [33]. At the same time, there are benefits to third trimester screening that include detection of reinfection and prevention of subsequent transmission, in addition to early treatment of infected infants. Early syphilis screening has been proven feasible in resource-constrained settings. A Zambian study successfully implemented earlier prenatal screening through educational campaigns, increasing prenatal syphilis screening before the first 16 wk of gestation from 9.4% to 42.5% [34]. Earlier prenatal screening in Mongolia also resulted in reduced CS cases [35]. Delayed prenatal care is a particular problem among migrant women in China, many of whom have an increased risk of syphilis [36]. The WHO Global Strategy for the Elimination of Congenital Syphilis also calls for early, high-quality prenatal care to increase the impact of syphilis screening [37]. More operational research is needed in order to implement earlier routine prenatal care, especially among migrant women in China.
Treatment completion was also found to reduce CS cases, and previous studies in global settings have demonstrated the potential feasibility of attaining high treatment completion rates in low-income settings [22],[38]–[40]. In the Shenzhen intervention trial, the treatment completion rate was 92% [10]. Increasing treatment completion rates will require the strengthening of local health systems in order to enhance health professional training and identify sustainable financing. Mistrust of syphilis test results, physicians, and clinics has been observed in China, and may contribute to incomplete treatment [41]. In addition, suboptimal test kits were problematic in the past in Guangdong Province. Newly available point-of-care testing provides a higher sensitivity and specificity than many existing test technologies [4].
There are limitations as to how effective small pilot studies can be applied on a larger scale in China and across diverse populations around the world. The presence of existing infrastructure and political will, as well as public acceptance of health outreach programs are critical components for attaining high screening coverage and completion of treatment. Widespread scale-up of successful prenatal syphilis screening pilot programs and clinical services that are trusted among pregnant women within most-at-risk populations are needed in order to overcome these challenges [10]. The NSCP consists of policies targeted at decreasing adult syphilis rates and educational campaigns aimed at increasing test-seeking probabilities. These interventions may decrease adult syphilis cases, but appear to have a limited effect on reducing CS rates, as one-way sensitivity analysis results demonstrated that they avert no more than 7% of the estimated CS case burden, and two-way sensitivity analysis with increased screening coverage demonstrated that they avert no more than 3% of estimated CS case burden. Nonetheless, the additional benefits of reducing the incidence of syphilis among the adult population should not be overlooked—improved sexual health and possibly reduced HIV transmission risk.
The most effective three-pronged strategy fell slightly short of the Chinese Ministry of Health target of <30 cases per 100,000 births, but the four-pronged strategy consisting of increased prenatal syphilis screening coverage, earlier prenatal testing, increased treatment completion rates, and increased test specificity and sensitivity managed to surpass that target, with a model-estimated CS outcome of 27 cases per 100,000 live births. This particular four-pronged strategy was also the most successful of all the combinations: no five-pronged strategy resulted in more CS case aversions. The model suggests that this combination strategy is the strategy that would most likely be associated with achieving the Chinese Ministry of Health goals.
This study has several important limitations. First, as with any model-based analysis, there are inherent uncertainties associated with the structure and necessary simplifying assumptions used for model analysis of a complex problem. In particular, pregnant women and non-pregnant women may have different clinical presentations or test-seeking behaviors. No model can simulate all aspects of real-world interactions. However, simplified models provide a useful tool for understanding the dynamics of relationships between interacting components, which facilitates greater understanding of complex phenomena. Based on current understanding and data from the literature, we included key aspects of syphilis natural history and treatment as well as critical features of intervention strategies, both those laid out in the NSCP and other proven intervention strategies. Confidence intervals for each model estimate were calculated, and the resulting uncertainty in the model did not affect the results. Second, this study generated estimates only for Guangdong Province in China and so may not be applicable to other regions with different syphilis epidemiology, health-seeking behaviors, or other health systems issues. At the same time, our estimates could potentially be applied to similar Chinese urban settings where , as in Guangdong Province, there is a substantial burden of syphilis. Third, our model addresses the impact of syphilis control strategies on the number of CS cases averted, but it does not include other adverse outcomes avoided and all the benefits associated with syphilis control policies in pregnancy. There was a lack of data from Chinese studies that described other adverse outcomes associated with syphilis such as stillbirths and prematurity. Fourth, this study did not collect or evaluate costing data, but other Guangdong research has shown that prenatal syphilis screening is highly cost-effective [8]. Prenatal syphilis testing has also been found to be cost-effective in a variety of settings from Europe to Africa and across a range of syphilis prevalence settings [4],[7],[42]–[45]. Lastly, this study could not quantify the health systems strengthening and improved case management that are also likely to play an important role in syphilis control programs [4]. Health systems strengthening would be useful for CS prevention as well as stemming the syphilis epidemic among pregnant women.
While our analysis specifically focuses on Guangdong Province, these results have broader implications within China and for other middle-income nations. Our analysis illustrates the importance of using multi-pronged approaches to address the complex problem of syphilis control and to reduce the number of CS cases. Reducing the burden of CS would also help achieve child and maternal health goals established by the United Nations [46] and the Asian Development Bank [47].
CS control is a solvable public health problem, but critical details about metrics and screening strategies are required for successful implementation. China's high level of commitment to syphilis control and extensive public health infrastructure create unparalleled opportunities for progress. The targets in the NSCP are consistent with WHO recommendations and represent useful goals. However, our model suggests that achieving these goals may require broadening and further refining of public health strategies for syphilis control.
Supporting Information
Zdroje
1. TuckerJD, ChenXS, PeelingRW (2010) Syphilis and social upheaval in china. N Engl J Med 362 : 1658–1661.
2. TemmermanM, GichangiP, FonckK, ApersL, ClaeysP, et al. (2000) Effect of a syphilis control programme on pregnancy outcome in Nairobi, Kenya. Sex Transm Infect 76 : 117–121.
3. Watson-JonesD, ChangaluchaJ, GumodokaB, WeissH, RusizokaM, et al. (2002) Syphilis in pregnancy in tanzania. I. Impact of maternal syphilis on outcome of pregnancy. J Infect Dis 186 : 940–947.
4. HawkesS, MatinN, BroutetN, LowN (2011) Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis. Lancet Infect Dis 11 : 684–691.
5. TuckerJD, CohenMS (2011) China's syphilis epidemic: epidemiology, proximate determinants of spread, and control responses. Curr Opin Infect Dis 24 : 50–55.
6. KambML, NewmanLM, RileyPL, MarkJ, HawkesSJ, et al. (2010) A road map for the global elimination of congenital syphilis. Obstet Gynecol Int 2010 : 312798.
7. RydzakCE, GoldieSJ (2008) Cost-effectiveness of rapid point-of-care prenatal syphilis screening in sub-Saharan Africa. Sex Transm Dis 35 : 775–784.
8. HongFC, LiuJB, FengTJ, LiuXL, PanP, et al. (2010) Congenital syphilis: an economic evaluation of a prevention program in China. Sex Transm Dis 37 : 26–31.
9. WeinsteinMC, O'BrienB, HornbergerJ, JacksonJ, JohannessonM, et al. (2003) Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR task force on good research practices—modeling studies. Value Health 6 : 9–17.
10. ChengJQ, ZhouH, HongFC, ZhangD, ZhangYJ, et al. (2007) Syphilis screening and intervention in 500,000 pregnant women in Shenzhen, the People's Republic of China. Sex Transm Infect 83 : 347–350.
11. YangLG, TuckerJD, YangB, ShenSY, SunXF, et al. (2010) Primary syphilis cases in Guangdong Province 1995–2008: opportunities for linking syphilis control and regional development. BMC Public Health 10 : 793.
12. WuZY, ZhouPY (2010) Syphilis and social upheaval in china. N Engl J Med 363 : 1088–1089.
13. WuDD, HongFC, FengTJ, LiuXL, LinLJ, et al. (2010) Congenital syphilis: refining newborn evaluation and management in Shenzhen, southern China. Sex Transm Infect 86 : 280–284.
14. HongFC, FengTJ, CaiYM, WenLZ, PanP, et al. (2009) Burden of syphilis infections in Shenzhen, China: a preliminary estimation. Int J STD AIDS 20 : 115–118.
15. LarsenSA, SteinerBM, RudolphAH (1995) Laboratory diagnosis and interpretation of tests for syphilis. Clin Microbiol Rev 8 : 1–21.
16. ChapelTA (1980) The signs and symptoms of secondary syphilis. Sex Transm Dis 7 : 161–164.
17. ChenZQ, ZhangGC, GongXD, LinC, GaoX, et al. (2007) Syphilis in China: results of a national surveillance programme. Lancet 369 : 132–138.
18. DeperthesBD, MeheusA, O'ReillyK, BroutetN (2004) Maternal and congenital syphilis programmes: case studies in Bolivia, Kenya and South Africa. Bull World Health Organ 82 : 410–416.
19. US Centers for Disease Control and Prevention (2010) 2010 STD treatment guidelines. Atlanta: US Centers for Disease Control and Prevention.
20. World Health Organization (2010) Elimination of congenital syphilis. Geneva: World Health Organization.
21. LinCC, GaoX, ChenXS, ChenQ, CohenMS (2006) China's syphilis epidemic: a systematic review of seroprevalence studies. Sex Transm Dis 33 : 726–736.
22. MabeyDC, SollisKA, KellyHA, BenzakenAS, BitarakwateE, et al. (2012) Point-of-care tests to strengthen health systems and save newborn lives: the case of syphilis. PLoS Med 9: e1001233 doi:10.1371/journal.pmed.1001233.
23. TuckerJD, HawkesSJ, YinYP, PeelingRW, CohenMS, et al. (2010) Scaling up syphilis testing in China: implementation beyond the clinic. Bull World Health Organ 88 : 452–457.
24. United Nations Statistics Division (2010) Antenatal care coverage (ANC) [database]. Available: http://data.un.org/Data.aspx?d=SOWC&f=inID%3A77. Accessed 1 July 2012.
25. CuiY, YangL, LuMT (2009) [Analysis on the status of antenatal checkup program in certain areas of China, 2005]. Zhonghua Liu Xing Bing Xue Za Zhi 30 : 887–890.
26. LiCG, LiCF, LiQ, LiM (2009) Thalassemia incidence and treatment in China with special reference to Shenzhen City and Guangdong province. Hemoglobin 33 : 296–303.
27. YanpingW, LeiM, LiD, ChunhuaH, XiaohongL, et al. (2010) A study on rural-urban differences in neonatal mortality rate in china, 1996–2006. J Epidemiol Community Health 64 : 935–936.
28. TangJ, LiNX (2008) [Use of maternal health care services in poor regions in Sichuan.]. Sichuan Da Xue Xue Bao Yi Xue Ban 39 : 1004–1006.
29. WendelGDJr, SheffieldJS, HollierLM, HillJB, RamseyPS, et al. (2002) Treatment of syphilis in pregnancy and prevention of congenital syphilis. Clin Infect Dis 35 (Suppl 2)
S200–S209.
30. LiuJB, HongFC, PanP, ZhouH, YangF, et al. (2010) A risk model for congenital syphilis in infants born to mothers with syphilis treated in gestation: a prospective cohort study. Sex Transm Infect 86 : 292–296.
31. AlexanderJM, SheffieldJS, SanchezPJ, MayfieldJ, WendelGDJr (1999) Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol 93 : 5–8.
32. SheffieldJS, SanchezPJ, MorrisG, MaberryM, ZerayF, et al. (2002) Congenital syphilis after maternal treatment for syphilis during pregnancy. Am J Obstet Gynecol 186 : 569–573.
33. WalkerDG, WalkerGJ (2002) Forgotten but not gone: the continuing scourge of congenital syphilis. Lancet Infect Dis 2 : 432–436.
34. HiraSK, BhatGJ, ChikamataDM, NkowaneB, TemboG, et al. (1990) Syphilis intervention in pregnancy: Zambian demonstration project. Genitourin Med 66 : 159–164.
35. MunkhuuB, LiabsuetrakulT, ChongsuvivatwongV, McNeilE, JanchivR (2009) One-stop service for antenatal syphilis screening and prevention of congenital syphilis in Ulaanbaatar, Mongolia: a cluster randomized trial. Sex Transm Dis 36 : 714–720.
36. ZhuL, QinM, DuL, XieRH, WongT, et al. (2010) Maternal and congenital syphilis in Shanghai, China, 2002 to 2006. Int J Infect Dis 14 (Suppl 3)
e45–e48.
37. World Health Organization (2007) The global elimination of congenital syphilis: rationale and strategy for action. Geneva: World Health Organization.
38. WilkinsonD, SachM (1998) Improved treatment of syphilis among pregnant women through on-site testing: an intervention study in rural South Africa. Trans R Soc Trop Med Hyg 92 : 348.
39. FitzgeraldDW, BehetsF, PrevalJ, SchulwolfL, BommiV, et al. (2003) Decreased congenital syphilis incidence in Haiti's rural Artibonite region following decentralized prenatal screening. Am J Public Health 93 : 444–446.
40. BronzanRN, Mwesigwa-KayongoDC, NarkunasD, SchmidGP, NeilsenGA, et al. (2007) On-site rapid antenatal syphilis screening with an immunochromatographic strip improves case detection and treatment in rural South African clinics. Sex Transm Dis 34 (Suppl 7)
S55–S60.
41. TuckerJD, YangLG, YangB, YoungD, HendersonGE, et al. (2011) Prior HIV testing among STD patients in Guangdong Province, China: opportunities for expanding detection of sexually transmitted HIV infection. Sex Transm Dis 39 : 182–187.
42. SchmidG (2004) Economic and programmatic aspects of congenital syphilis prevention. Bull World Health Organ 82 : 402–409.
43. BlandfordJM, GiftTL, VasaikarS, Mwesigwa-KayongoD, DlaliP, et al. (2007) Cost-effectiveness of on-site antenatal screening to prevent congenital syphilis in rural eastern Cape Province, Republic of South Africa. Sex Transm Dis 34 (Suppl 7)
S61–S66.
44. SchackmanBR, NeukermansCP, FontainSN, NolteC, JosephP, et al. (2007) Cost-effectiveness of rapid syphilis screening in prenatal HIV testing programs in Haiti. PLoS Med 4: e183 doi:10.1371/journal.pmed.0040183.
45. VickermanP, PeelingRW, Terris-PrestholtF, ChangaluchaJ, MabeyD, et al. (2006) Modelling the cost-effectiveness of introducing rapid syphilis tests into an antenatal syphilis screening programme in Mwanza, Tanzania. Sex Transm Infect 82 (Suppl 5)v38–v43.
46. United Nations (2011) What they are [Millennium Development Goals]. Available: http://www.unmillenniumproject.org/goals/index.htm. Accessed 1 July 2012.
47. Asian Development Bank (2012) Health. Available: http://www.adb.org/sectors/health/main. Accessed 1 July 2012.
48. ParishWL, LaumannEO, CohenMS, PanS, ZhengH, et al. (2003) Population-based study of chlamydial infection in China: a hidden epidemic. JAMA 289 : 1265–1273.
49. ZhaoF, GuoSF, LiBH, CuiY, WuKS (2005) [Survey on the situation of antenatal care in different regions of China in 1971–2003]. Zhonghua Liu Xing Bing Xue Za Zhi 26 : 172–176.
50. JiaoT, XuX, HanCY, LiuL, ZhouY, et al. (2010) [Perinatal outcomes of pregnant women with syphilis treated by procaine penicillin at different gestations]. Chin J Derm Venereol 24 : 934.
51. ZhangXM, ZhangRN, LinSQ, ChenSX, ZhengLY (2004) [Clinical analysis of 192 pregnant women infected by syphilis.]. Zhonghua Fu Chan Ke Za Zhi 39 : 682–686.
52. LiL, LiuM, WangF (2009) [Clinical analysis on 121 pregnant women infected by syphilis.]. Matern Child Health Care China 24 : 4087.
53. China National STD Control Center (2010) [2010 national STD control and prevention national treatment guidelines]. Nanjing: China National STD Control Center.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 1- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- Magnosolv a jeho využití v neurologii
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- More Data and Appropriate Statistical Methods Needed to Fully Measure the Displacement Effects of Development Assistance for Health
- Preventing Antiretroviral Treatment Interruptions among HIV/AIDS Patients in Africa
- Translating Coverage Gains into Health Gains for All Women and Children: The Quality Care Opportunity
- Implementation of a Mental Health Care Package for Children in Areas of Armed Conflict: A Case Study from Burundi, Indonesia, Nepal, Sri Lanka, and Sudan
- Toward an Understanding of Disengagement from HIV Treatment and Care in Sub-Saharan Africa: A Qualitative Study
- Tackling Non-Communicable Diseases In Low- and Middle-Income Countries: Is the Evidence from High-Income Countries All We Need?
- Change in the Body Mass Index Distribution for Women: Analysis of Surveys from 37 Low- and Middle-Income Countries
- Getting More Generous with the Truth: Clinical Trial Reporting in 2013 and Beyond
- Reducing Vulnerability to Climate Change in Sub-Saharan Africa: The Need for Better Evidence
- Erectile Dysfunction Severity as a Risk Marker for Cardiovascular Disease Hospitalisation and All-Cause Mortality: A Prospective Cohort Study
- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
- Considerations in Assessing the Evidence and Implications of Aid Displacement from the Health Sector
- Prioritizing Congenital Syphilis Control in South China: A Decision Analytic Model to Inform Policy Implementation
- Balancing Community and Hospital Care: A Case Study of Reforming Mental Health Services in Georgia
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Differences in Reporting of Analyses in Internal Company Documents Versus Published Trial Reports: Comparisons in Industry-Sponsored Trials in Off-Label Uses of Gabapentin
- The Effectiveness of Mobile-Health Technologies to Improve Health Care Service Delivery Processes: A Systematic Review and Meta-Analysis
- The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review
- Why Do Women Not Use Antenatal Services in Low- and Middle-Income Countries? A Meta-Synthesis of Qualitative Studies
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



