-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaUTILIZATION OF INTENSE PULSED LIGHT IN THE TREATMENT OF FACE AND NECK ERYTHROSIS
Autoři: Madonna Terracina F. S.; G. Curinga; M. Mazzocchi; M. G. Onesti; N. Scuderi
Působiště autorů: Department of Dermatology and Plastic Reconstructive Surgery, University of Rome “La Sapienza”, Italy
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 2, 2007, pp. 51-54
INTRODUCTION
Erythrosis is a clinical manifestation characterized by parossistic vasodilatations followed by fixed superficial venular dilatations localized at the face, neck, décolleté and pinnas. This topography is due to the vascularization of these areas, in particular to the microcirculation of the face, correlated to the body and brain thermoregulation. In fact the concentration of the dermal capillaries of the face is the highest of all the other cutaneous districts.
It is known that erythrosis is the clinical manifestation of different dermatological diseases such as rosacea, Civatte’s poikiloderma, though in some cases its etiology is still unknown.
Vascular fragility is at the basis of erythrosis. Vessel walls are influenced and eventually altered by the release of histamine-like cytokines due to emotional, endocrine, neurovegetative and ambiental factors, as well as vasodilatatory refluxes that cause hyperthermia.
Neurovegetative alterations such as excitability and emotivity, alcohol abuse and constipation are examples of events that can promote inflammation and, when chronic, the presence of a persistent erythema.
Microcirculation is also influenced by environmental and climatic factors: unexpected temperature alterations, high temperatures, solar radiation (sun exposure or UV radiation), excessive humidity and the wind, all make the couperose worse.
Erythrosis and couperose are frequent in external workers or those exposed to high temperature (farmers, athletes, sailors, chefs).
Alterations of the microcirculation and the correlated cutaneous manifestations may also be a sign of internal diseases such as hepatic or endocrine pathologies.
The treatment of erythrosis with laser therapy results in cutaneous clinical benefits, which may be of a transitory nature. The efficacy of vascular laser (500–1064 nm) as pulsed-dye laser, KTP pulse laser, diode laser, cuprum vapour and the long impulse Nd-YAG laser is well described in the literature; as a result the authors wish to focus on the utilization of IPL for face and neck erythrosis (3, 9, 11).
The IPL is a white, filtered, non-selective, incoherent, not collimed light of wide spectrum (wavelength between 400–1200 nm). The IPL may release “long” impulses during the thermal relaxation time (TRT) of the vessel, so it is also useful for the treatment of deep ectasic vessels of medium diameter (4, 8).
The protocol adopted points out the benefits of the pulsed light vs. conventional laser, with particular attention to the efficacy and the minimal collateral effects.
MATERIAL AND METHOD
The authors propose a study of the previous year which involved 34 patients with erythrosis of the face and of the neck of unknown etiology. 22 of them are female and 12 are men, aged between 19 and 65 years and phototype ranging from 2 to 4 on the Fitzpatrick scale. From anamnestic results particular conditions such as pregnancy, assumption of photosensibilization and anticoagulant drugs, diabetes, hemorrhagic diseases, predisposition to cheloids, and those who were recently exposed or shortly will be exposed to the sun are excluded.
Two patients were affected by Civatte’s poikiloderma, eighteen by face rosacea and fourteen by erythrosis and face teleangiectasia of unknown origin.
Each patient received an explanation regarding the benefits, the risks and limits of the method before signing the informed consent for participation in the IPL study. For every patient we took a series of pictures pre-treatment and after 5 cycles of IPL.
None of the patients had undergone laser treatment in the past, and only four of them had started medical therapy with topic fluconazol some months before.
The technique is based on a pulsed light of high intensity obtained with a vascular filter of 560 nm.
In the previous two weeks patients applied topical antioxidants, nutrients and depigmentants.
Only five patients applied topical anesthetic prilocaine (EMLA®) immediately before each treatment. All patients applied a cooling gel on the area to be treated and used protective glasses. They underwent five treatments of twenty minutes each, at intervals of twenty-one days, with a variable fluency between 9–12 J/cm² and impulse time of 10–20 ms. The sheaf used is a rectangular spot of 2 cm x 5 cm.
Immediately after the treatment we applied topical cooling systems (cool head of the apparatus) for 10–15 minutes and subsequently topical lenitive anti-inflammatory non steroid creams, for use over the next 2–3 days if necessary.
During the treatment period the patients were required to apply sunscreens and to limit sun-exposure. The follow-up from the end of the protocol is at 5 months. After five treatments we evaluated objectively the grade of improvement by a standard system for computerized color image analysis of skin erythrosis modification after IPL treatments (6).
RESULTS
In the two patients affected by Civatte’s poikiloderma of the neck we obtained differing results: In the first case, an evident positive response of the clinical picture was perceived after only two applications of the IPL with regression of the erythema and satisfaction of the patient at the end of the treatment; in the second case the benefits were evident after 3–4 applications of IPL at a higher fluency of up to 14 J/ cm².
In twenty-four patients we obtained a total regression of the cutaneous manifestation after 5 applications, whilst another two patients showed only an attenuation of the erythema – possibly due to the fact that they exposed themselves to the sun frequently during the protocol and they did not apply topical sunscreens as recommended by the authors.
In five cases with erythrosis the erythema persisted after the end of the treatment, although the patients were satisfied with the evident benefits.
One patient affected by face rosacea and in treatment with oral antibiotics showed good results from the first application with regression of the erythema up to its disappearance.
Skin erythrosis evaluation by digital images permits us to evaluate objectively the grade of improvement of the erythrosis after IPL therapy (Table 1).
Tab. 1. Quantitative evaluation of the efficacy of IPL treatment by digital images according to Mezzana (6) 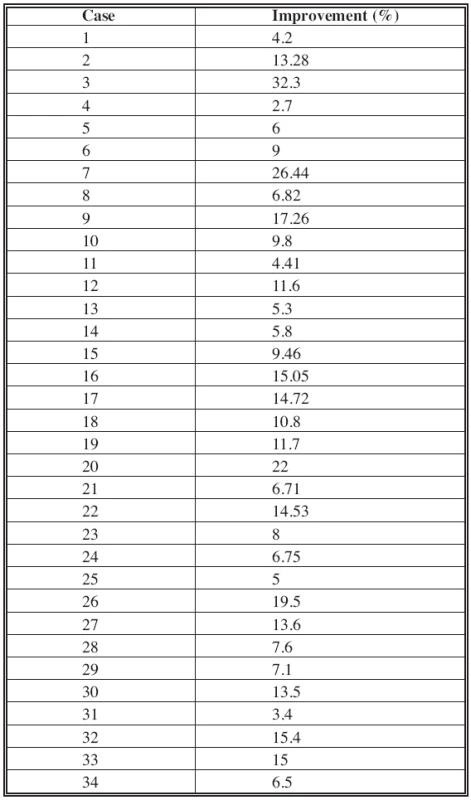
Collateral effects are not reported, despite a long-standing (more than 48 hours) post-treatment erythema in only one case.
During the follow-up period (every two months from the last application) the clinical results proved to be stable: in one case the patient showed a positive benefit from the constant application of sunscreens at the fifth month of follow-up. In contrast, the patient with face rosacea suffered from a return of erythrosis at the time of antibiotic therapy suspension (2).
Fig. 1. Pre and post five IPL treatments (lateral view) 
Fig. 2. Pre and post four treatments 
Fig. 3. Pre and post two IPL applications 
DISCUSSION AND CONCLUSION
The new generation of laser and non-laser light devices (e.g. intense pulsed light, IPL) offers excellent results in the management of clinical and cosmetic conditions, including significant changes in improvement in vascular conditions such as erythrosis, without significant injury to the epidermis (1, 7, 5, 10).
Despite the low number of patients, the reported results demonstrate the efficacy of the IPL technique.
The benefits of IPL vs. traditional lasers are:
- The possibility to treat wide areas in a shorter time;
- The absence of significant collateral effects such as porpora (with pulsed-dye laser) or post-treatment edema;
- A good response from the patient in terms of the security of the method and the constant presentability days after treatment.
The disadvantages encountered are:
- Possible light absorption from the epidermis with appearance of hypo - and hyperpigmented areas;
- Variability of results due to operator experience.
In any case, we can affirm that the IPL technique should be considered as the treatment of first choice for erythrosis of the face and neck.
Address for correspondence:
Giuseppe Curinga, MD.
Via Benedetta 24
00153 Rome
Italy
E-mail: giuseppecuringa@libero.it
Zdroje
1. Angermeier MC. Treatment of facial vascular lesions with intense pulsed light. J. Cutan. Laser Ther., 1(2), 1999, p. 95–100.
2. Ceilley RI. Advances in the topical treatment of acne and rosacea. J. Drugs Dermatol., 3(5 Suppl), 2004, p. S12–22.
3. Clark C., Cameron H., Moseley H., Ferguson J., Ibbotson SH. Treatment of superficial cutaneous vascular lesions: experience with the KTP 532 nm laser. Lasers Med. Sci., 19(1), 2004, p. 1–5.
4. Clementoni MT., Gilardino P., Muti GF., Signorini M., Pistorale A., Morselli PG., Cavina C. Facial teleangectasias: our experience in treatment with IPL. Lasers Surg. Med., 37(1), 2005, p. 9–13.
5. Loo WJ., Lanigan SW. Recent advances in laser therapy for the treatment of cutaneous vascular disorders. Lasers Med. Sci., 17(1), 2002, p. 9–12.
6. Mezzana P., Anniboletti T., Curinga G., Onesti MG. A new method of skin erythrosis evaluation in digital images. Acta. Chir. Plast., 49, 2007, p. 21–26.
7. Nestor MS. Combination therapy in clinical and cosmetic dermatology: the marriage of device and drug. J. Drugs Dermatol., 3(5 Suppl), 2004, p. S4–11.
8. Schroeter CA., Haaf-von Below S., Neumann HA. Effective treatment of rosacea using intense pulsed light systems. Dermatol. Surg., 31(10), 2005, p. 1285–1289.
9. Smit JM., Bauland CG., Wijnberg DS., Spauwen PH. Pulsed dye laser treatment, a review of indications and outcome based on published trials. Br. J. Plast. Surg., 58(7), 2005, p. 981–987.
10. Sperber BR., Walling HW., Arpey CJ., Whitaker DC. Vesiculobullous eruption from intense pulsed light treatment. Dermatol. Surg., 31(3), 2005, p. 345–348; discussion p. 348–349.
11. Woo SH., Ahn HH., Kim SN., Kye YC. Treatment of vascular skin lesions with the variable-pulse 595 nm pulsed dye laser. Dermatol. Surg., 32(1), 2006, p. 41–48.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ/SLOVENSKÉ SOUHRNY
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2007 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- S doc. Janou Hirmerovou o tromboprofylaxi v břišní či onkologické chirurgii a jak k ní správně přistupovat
- Incidence asymptomatické hluboké žilní trombózy po totální endoprotéze kyčle a účinnost enoxaparinu v tromboprofylaxi
- INTERAKTIVNÍ KAZUISTIKA: Žilní trombóza v graviditě
-
Všechny články tohoto čísla
- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- UTILIZATION OF INTENSE PULSED LIGHT IN THE TREATMENT OF FACE AND NECK ERYTHROSIS
- ČESKÉ/SLOVENSKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



