-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
Autoři: J. Velemínská 1; Z. Šmahel 1; S. Katina 2
Působiště autorů: Department of Anthropology and Human Genetics, Faculty of Science, Charles University, Prague, Czech Republic, and 1; Department of Applied Mathematics and Statistics, Faculty of Mathematics, Physics and CS, Comenius University, Bratislava, Slovakia 2
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 2, 2007, pp. 41-46
INTRODUCTION
The objective of this study is to find a predictive model for jaw development in patients with complete unilateral cleft lip and palate in the period of pubertal growth spurt. Puberty is crucial for jaw growth and development in facial clefts, and also for orthodontic treatment. Anterior upper jaw growth deficiency may enhance the disproportion in the anteroposterior position of both jaws within a very short time period. This actually leads very often to impaired sagittal intermaxillary relations as well as profile configuration and occlusion of incisors. It may be supposed that as a result of the use of a predicting model in clinical practice, attention would be drawn in time to patients needing intensive orthodontic care. A reduction in the rate of most serious patients requiring maxillofacial surgery should result as well.
LITERARY REVIEW
Many models predicting face growth and development in the healthy population or in patients with less serious growth disorders can be found in the literature (e.g. 2, 3, 7, 11, 17). Prediction of the direction and extension of mandibular growth rotation based on morphological features has been often studied (1, 9, 10, 14). However, the possibilities of predicting facial growth in patients with clefts are very limited, and prediction models are rare so far. A simple system for the prediction of both jaws development was established (4). This method uses individual cephalometric assessment based on specific morphological and morphogenetic face patterns. The procedure consists of two main parts: shape analysis using face growth patterns and sizes of craniofacial structures. This method was applied to clefts by Gnoinska (5) and was conceived as a study of anterior jaw growth as well as the possibility of detection of the first signs of adverse development. The sooner these signs occur, the more disadvantageous is their development. The morphology of the facial skeleton in patients with clefts depended mainly on the following factors: the baseline condition, the surgical intervention and its timing. We consider the poor reliability regarding the location of certain applied points as a disadvantage of this method. Also, the inclination of occlusion plane, representing a substantial part of the system, may undergo quick and significant change as a result of treatment during the mixed dentition period. Schwarz et al. (13) studied options for the utilization of 11 dental arch dimensions in patients with clefts measured prior to surgery for the prediction of subsequently developed lateral cross bite. None of the dimensions used, taken alone, predicted the future development of this pathological deviation. The data were used to calculate multiple predictive equations to accurately forecast cross bite presence or absence in 88% of cases with deciduous, and in 91% of subjects with mixed dentition. Kramer et al. (8) developed a model predicting palatal width and depth in patients with clefts at 4 years of age. The relation between these parameters at 4 years of age and the early growth rate and palate development in the period from birth until 1.5 years of age was submitted to analysis using multi-levelled modelling of longitudinal data. Patients were divided into three groups according to their surgical therapy (without palatal surgery, with repair of the soft palate only, and with surgery of both the soft and the hard palate). Individual predictions were tested and appeared to be possible and purposeful.
A nomogram for the estimation of the failure risk regarding attempts to restore a positive overjet in patients with clefts based on roentgencephalometric assessment of one parameter (interalveolar relations) was developed (15). The system defines critical limits not to be exceeded if the requirements for therapeutic success are to be complied with. However, this system does not involve the development of the jaws and is also unable to predict this development.
In order to establish facial growth prognosis in patients with clefts, Sheuer et al. (12) applied the method of multi-dimensional regression analysis. Equations with correlation coefficients exceeding 0.92 were evolved separately for the estimation of development of the upper and lower jaw protrusion/retrusion (SNA and SNB angles); however, the sagittal intermaxillary relations were not predicted, and prediction was not tested on another patient group.
MATERIAL AND METHOD
The investigation involved 73 boys with complete unilateralcleft lip and palate without other associated malformations,treated at the Clinic of Plastic Surgery inPrague. The patients were monitored during puberty andassessed at the onset and end of this period, i.e. at theages of 10 and 15. The mean age was 10 years and2 months and 15 years and 1 month. 48 patients wereborn between 1972 and 1978, and 25 boys were bornbetween 1985 and 1988.
Primary cheiloplasty performed according to Tennison’s method at an average age of 9 months was associated with periosteoplasty using a 5–7 mm wide and 15–20 mm long periostal flap obtained from the lateral maxillary segment. All patients underwent palatoplasty at a mean age of 5 years, always by the method of pushback with pharyngeal flap surgery. In addition, 25 patients born during the 1980s had primary repositioning of the nasal septum. In about one-third of the patients a tonsillectomy was performed or, in exceptional cases, adenotomy.
Secondary corrective procedures were implemented in patients with persisting soft tissue deformities (64.6%). Corrections of the lip and nose were made in 33.3% of the subjects, correction of the lip in 23% and correction of the nose alone in 8.3%. Fifty patients of the group were treated using fixed appliances, while twenty-three were treated with removable appliances only in order to align the teeth properly in the dental arch and to achieve proclination of the upper incisors and maxillary overjet. The study was based on a craniometric analysis of X-ray films of the patients’ heads made under standard conditions (focus-object distance = 370 cm, object-film = 30 cm, enlargement 8.1%). Cephalometric points and reference lines mentioned in the study are indicated in Fig. 1. In the case of double contours the centre between the right and left side has been marked.
Fig. 1. Cephalometric points and reference lines used in this study: Cd (condylion) – most superior point on the condylar head; Go (gonion) – point on the angle of the mandible determined by the axis of ML/RL angle; Pgn (prognathion) – point on the mandibular symphysis furthest from Cd; Pg (pogonion) – most anterior point on the bony chin; Sm (supramentale) – deepest point on the anterior contour of the mandibular symphysis; Id (infradentale) – point of the gingival contact with the lower central incisor; Ii (incision inferius) – incisal tip of the lower central incisor; Is (incision superius) – incisal tip of the upper central incisor; Pr (prosthion) – point of gingival contact with the upper central incisor; Ss (subspinale) – deepest point of the subspinal concavity; Sp (spinale) – tip of the anterior nasal spine; S (sella) – centre of sella turcica; N (nasion) – most anterior point on the frontonasal suture; NSL – line through N and S; OL – line passing though the midpoint between incisal tip of the upper and lower central incisors and posterior cuspid of the first lower molar; +1 – axis of the upper incisor; –1 – axis of the lower incisor; ML – tangent to the mandibular body through Gn 
Seventy-one variables were assessed by means of a digitizer: 22 linear, 40 characteristics of position and shape, and 9 dental or special parameters. Measurement of characteristics N-Ss-Pg, Ss-N-Sm and Pr-N-Id is illustrated in Fig. 2, variables Pr+Id and +1/-1 are explained in Fig. 3. Pr+Id is the distance between points Pr and Id after their perpendicular projection to the occlusion plane passing through the midpoint between the cusps of the upper and lower central incisors and molare point (if Pr is posterior in relation to Id, the value is negative). Interincisal angle +1/–1 is the angle between the axis of the upper and lower first incisors.
Fig. 2. The illustration of measurement of three important angle variables used in this study (N-Ss-Pg, Ss-N-Sm, Pr, N-Id) 
Fig. 3. Pr+Id is the distance between points Pr and Id after their perpendicular projection to the occlusion plane passing through the midpoint between the cusps of the upper and lower central incisors and molar point (if Pr is posterior in relation to Id, the value is negative). Measurement of interincisal angle +1/–1 between axis of the first upper and lower incisors 
For statistical processing of the assembled data, the statistical system S-plus 6.2 was used.
The prediction was made on the base of multiple linear regression models and regression partitioning trees (18). Tree-based models provide an alternative to linear and additive models for regression problems, and to linear and additive logistic models for classification problems. Compared to linear and additive models, tree-based models have the following advantages in relation to the analysed data: they allow more general (that is, other than of a particular multiplicative form) interactions between predictor variables, and they also search for deeper relationships between variables based on the tree branches. Prediction was compared with real measurements using paired Wilcoxon rank-sum test and paired t-test at significance level α = 0.05.
RESULTS
The group of 73 long-term follow-up patients made itpossible to propose 2 types of predictive models regardingjaw development in patients with clefts. On the basisof 6 variables at 10 years of age, an equation (Table 1)was created to predict the sagittal intermaxillary relationsat 15 years of age with high reliability (determinationcoefficient R2 = 0.822). In order to test the model itwas calculated 73 times, each time excluding one differentpatient. The parameters of this patient were insertedinto the equation, and in this way we successively establisheda set of 73 predicted values of sagittal intermaxillaryrelations, one for each patient. The real and predictedvalues for each patient were compared with the pairedt-test (t = –0.578, p-value = 0.565) and the Wilcoxon test(z = –0.561, p-value = 0.575), and no difference wasshown using either method (Table 2).
Tab. 1. Results of linear regression model Ss-N-Sm15 = 24.736 + 0.245*Cd-Go10 - 0.327 *N-S-Pgn10 + 0.249*S-N-Sp10 + 0.8*S-N-Pr10 - 1.383*S-N-Sm10 + 0.163*ML/NSL10, (adjusted R2 = 0.822) 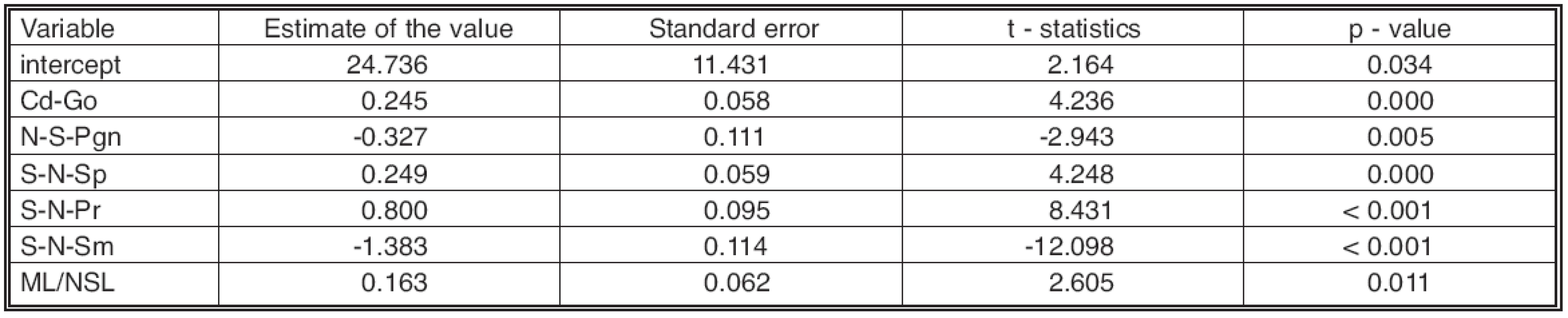
Even though the results obtained indicate the extreme reliability of the model, there is high interindividual variability among the tested patients. The results of our former study (20) proved that groups of similarly developing patients exist, endowed with a similar compensatory adaptation mechanism. Therefore we chose another method, regression partitioning trees. On the basis of a least-square (LS) algorithm, similarly developing patients were grouped into the same clusters with the same predicted values, in our case the ANB angle at 15 years of age. The trees consist of branches defined by intervals of regressor values, which are most connected with the predicted variable. The final model splits our set of 73 patients into six groups that correspond to a certain value of the predicted variable (i.e. ANB). These groups are characterized by one to four variables at 10 years of age (N-Ss-Pg, Pr+Id, +1/–1 and Pr-N-Id), where the tree branches with regard to their size intervals (see Fig. 2).
Six groups of our patients to which the values of the ANB angle at 15 years of age were attributed are as follows: –6.021 (n = 9), –2.529 (n = 12), –0.978 (n = 11), 0.639 (n = 21), 2.078 (n = 13) and 4.300 (n = 7). The final model is based on 4 variables at 10 years of age. The predicted model depends most heavily on face convexity (N-Ss-Pg). A concave face characterized by an angle N-Ss-Pg ≥180.800 degrees predicts in itself the patients with most affected sagittal intermaxillary relations (values of –6.021 and –2.529 degrees). More precisely, an extreme concave face, with convexity angle above 187.800 degrees at 10 years of age, develops during puberty into the model ANB (Ss-N-Sm) angle value –6.021. The ANB angle value of –2.53 degrees is allocated to the face convexity angle in the interval of 187.8–180.8 degrees.
Fig. 4. Regression partitioning tree. The presented critical values do not express accuracy of measurement but only exact statistical figure (see text) 
The remaining patient groups may be analyzed in a similar way. Here, other variables at 10 years of age also play a role, namely the sagittal interalveolar relations Pr+Id and the inter-incisal angle +1/–1. For patients with face convexity below 180.800 degrees the borderline value of interalveolar relations (Pr+Id) of 2.550 mm is crucial. If it is above or at this level, sagittal intermaxillary relations develop successfully (model values 2.078 and 4.300 degrees of ANB).
However, from the point of view of orthodontic practice, it is most difficult to make predictions for the last two groups in whom at the age of 15 the ANB angle assumes model values of about zero. If the interincisal angle +1/–1 is greater or equal to 150.300 degrees at 10 years of age, the sagittal intermaxillary relations develop until negative values are reached (–0.978). If it attains values below 150.300 degrees, the ANB angle at 15 years of age reaches the more favourable predicted value of 0.639 degrees.
As with the former model, we compared the actual (measured) and predicted variables by means of the paired t-test (t = –0.002, p-value = 0.999) and the Wilcoxon test (z = –0.380, p-value = 0.648). Neither of the methods yielded any significant difference between predicted and actual values (see Table 2).
Tab. 2. Table 2. Real and predicted values of ANB (Ss-N-Sm) in 15 yrs counted on the base of both models, with means, difference, t-statistics, zW- statistics and p-values 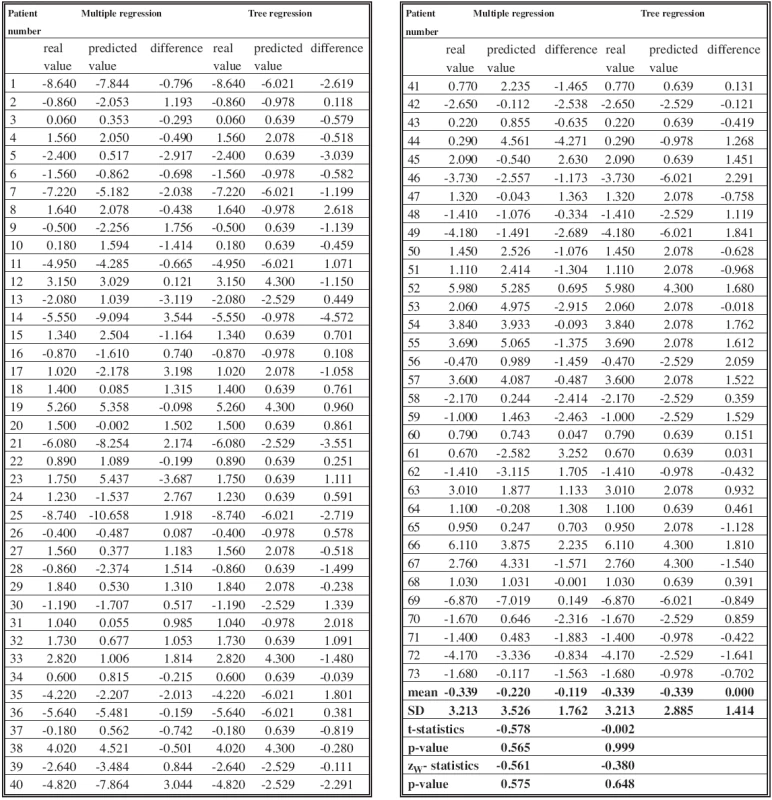
DISCUSSION AND CONCLUSION
Facial clefts produce a high degree of developmental variability of both jaws, making prognosis and therapeutic outlooks very difficult. They represent a specific malformation which is among the most serious skeletal and orthodontic anomalies linked with facial developmental disorders. Therefore predictive systems derived on the basis of findings in subjects free of such malformation cannot be used for patients with clefts. An inherent component in the development of a successful method of prediction is a detailed multivariate analysis of craniometric signs of the patients. We therefore firstmonitored how the single parameters are linked at 10 years of age. The mutual intracranial relations using cluster and factor analysis were investigated (19). Then we concentrated on the longitudinal cephalometric monitoring of facial growth and development between 10 and 15 years of age assessed both according to average statistical characteristics and in individual patients (20). On the basis of these studies a series of trinominal predictive equations was calculated, verified in practice on 12 more patients (21) and published (22).
Models which possess the strongest predictive abilities (R2 of about 0.80) are based on prediction of the ANB angle at 15 years of age. This angle gives good information on therapeutic possibilities and also shows less variability (SD = 1.77) than other characteristics of sagittal jaw relations (Pr-N-Id SD = 1.91, Ss+Sm SD = 2.92, Pr+Id SD = 2.77) (18, 19). The borderline value of the determination coefficient, which is useful for prediction, as verified in orthodontic practice, amounts to about 0.64 (6). Paradoxically, and as confirmed by our present conclusions, the angle ANB at 10 years of age itself is not the strongest regressor in trinomial equations that we proposed. Linear facial dimensions, or more precisely the maxillary height dimensions prior to the pubertal growth spurt, have proved to be among the other important predictive variables (22).
However, the use of the calculated regression tree appears to be a much better and simplex option for practical purposes than trinomial equations. The measurements of only 1 to 4 parameters in a patient at 10 years of age are sufficient for estimation of the ANB angle at 15 years. From the diagram (see Fig. 2) the following conclusions explicitly result:
1. In patients exhibiting facial convexity angle above 180.80 degrees at 10 years of age, the ANB angle below –2.529 degrees at 15 years of age was predicted.
2. In patients with facial convexity angle below 180.80 degrees at 10 years of age and sagittal interalveolar relations (Pr+Id) above 2.55 mm, an ANB angle of at least 2.078 degrees was predicted.
3. In the remaining patients with facial convexity angle below 180.80 degrees and a Pr+Id distance below 2.55 mm, the following predictions may be made using the interincisal angle (+1/–1):
- 3a. An angle below 150.30 degrees predicts an ANB angle of –0.978 degrees.
- 3b. An angle above 150.30 degrees predicts an ANB angle of 0.639 degrees.
These predictive values present sufficient base information on jaw interrelations at 15 years of age and make prediction simpler from the practical point of view.
The series of patients was homogeneous (complete UCLP) and treated with the same primary operations. Some inevitable variations in later treatment, such as in the use of secondary soft tissue procedures or tonsilectomy, do not influence the ANB angle used for prediction, and the same applies to primary repositioning of the nasal septum (16). The impact of the use of fixed appliances on prediction of the ANB angle was also followed up, and no substantial differences as compared to patients with the use of removable appliances alone were found (20).
Our study shows some possible approaches to the still unsolved problem and may contribute to the achievement of better therapeutic results in patients with facial clefts. However, it is necessary to verify the results on patients treated with different procedures and under different conditions.
Acknowledgement: This study was supported by Grant Agency of Charles University 270/2004/B-BIO/PrF and Research plan MSM 0021620843.
Address for correspondence:
Jana Velemínská
Department of Anthropology and Human Genetics
Faculty of Science, Charles University
128 44 Viničná 7, Prague 2
Czech Republic
E-mail: velemins@natur.cuni.cz
Zdroje
1. Baumrind S., Korn EL., West EE. Prediction of mandibular rotation: An empirical test of clinician performance. Am. J. Orthod., 86, 1984, p. 371–385.
2. Björk A., Skieller V. Facial development and tooth eruption. Am. J. Orthod., 62, 1972, p. 339–382.
3. Eales EA., Jones ML., Newton C., Sugar AW. Astudy of the accuracy of predicted soft tissue changes produced by a computer software package (COG 3.4) in a series of patients treated by the Le Fort I osteotomy. Brit. J. Oral Maxillofac. Surg., 33, 1995, p. 362–369.
4. Enlow DH., Moyers RE., Hunter WS., McNamara JA. A procedure for the analysis of intrinsic facial form and growth. Am. J. Orthod., 56, 1968, p. 6–23.
5. Gnoinski WM. Early maxillary orthopaedics as a supplement to conventional primary surgery in complete cleft lip and palate cases – Long-term results. J. Oral. Maxillofac. Surg., 10, 1982, p. 165–172.
6. Hixon EH. Prediction of facial growth. Trans. Europ. Orthod. Soc., 44, 1968, p. 127–139.
7. Hultgren BW., Isaacson RJ., Erdman AG., Worms FW. Mechanics, growth and Class II corrections. Am. J. Orthod., 74, 1978, p. 388–395.
8. Kramer GJ., Hoeksma JB., Prahl-Andersen B. Prediction of early palatal growth and development in children with cleft lip and palate. Cleft Palate Craniofac. J., 33, 1996, p. 112–117.
9. Lee RS., Daniel FJ., Swartz M., Baumrind S., Korn EL. Assessment of a method for the prediction of mandibular rotation. Am. J. Orthod. Dentofac. Orthop., 91, 1987, p. 395–402.
10. Leslie LR., Southard TE. Prediction of mandibular growth rotation: assessment of the Skieller, Björk, and Linde-Hansen method. Am. J. Orthod. Dentofac. Orthop., 114, 1998, p. 659–667.
11. Rudolph DJ., White SE., Sinclair PM. Multivariate prediction of skeletal Class II growth. Am. J. Orthod. Dentofac. Orthop., 114, 1998, p. 283–291.
12. Scheuer HA., Höltje WJ., Nasune A., Pfeifer G. Prognosis of facial growth in patients with unilateral complete clefts of the lip, alveolus and palate. J. Oral. Maxillofac. Surg., 29, 2001, p. 198–204.
13. Schwartz BH., Long RE., Smith RJ., Gipe DP. Early prediction of posterior crossbite in the complete unilateral cleft lip and palate. Cleft Palate Craniofac. J., 21, 1984, p. 76–81.
14. Skieller V., Björk A., Linde-Hansen T. Prediction of mandibular growth rotation evaluated from a longitudinal implant sample.
Am. J. Orthod., 86, 1984, p. 359–370.
15. Šmahel Z. Nomogram for assessment of restoration of a positive overjet in unilateral cleft lip and palate. Acta Chir. Plast., 39, 1997, p. 117–120.
16. Šmahel Z., Müllerová Ž., Nejedlý A. Effect of primary repositioning of the nasal septum on facial growth in unilateral cleft lip and palate. Cleft Palate Craniofac. J., 36, 1999, p. 310–313.
17. Thames TL., Sinclair PM., Alexander RG. The accuracy of computerized growth prediction in Class II high-angle cases. Am. J. Orthod., 87, 1985, p. 398–405.
18. Vanables WN., Ripley BD. Modern Applied Statistics with S-PLUS. New York: Springer, 2002.
19. Velemínská J., Müllerová Ž. Development of intracranial relations in patients aged 10 to 18 years with clefts of the lip and palate using cluster analysis. Acta Chir. Plast., 43, 2001, p. 137–142.
20. Velemínská J., Šmahel Z., Müllerová Ž. Facial growth and development during the pubertal period in patients with complete unilateral cleft of lip and palate. Acta Chir. Plast., 45, 2003, p. 22–31.
21. Velemínská J., Müllerová Ž. Prediction of the development of jaws in patients with complete unilateral cleft of the lip and palate. Am. J. Phys. Anthropol., Suppl., 36, 2003, p. 214.
22. Velemínská J., Šmahel Z., Müllerová Ž. Predicting the development of jaws in patients with complete unilateral cleft of the lip and palate. Acta Chir. Plast., 47, 2005, p. 81–84.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ/SLOVENSKÉ SOUHRNY
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2007 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- S doc. Janou Hirmerovou o tromboprofylaxi v břišní či onkologické chirurgii a jak k ní správně přistupovat
- Incidence asymptomatické hluboké žilní trombózy po totální endoprotéze kyčle a účinnost enoxaparinu v tromboprofylaxi
- INTERAKTIVNÍ KAZUISTIKA: Žilní trombóza v graviditě
-
Všechny články tohoto čísla
- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- UTILIZATION OF INTENSE PULSED LIGHT IN THE TREATMENT OF FACE AND NECK ERYTHROSIS
- ČESKÉ/SLOVENSKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



