-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
BILATERAL CHEEK-TO-NOSE ADVANCEMENT FLAP: AN ALTERNATIVE TO THE PARAMEDIAN FOREHEAD FLAP FOR RECONSTRUCTION OF THE NOSE
Autoři: M. Sand 1; P. Boorboor 2; D. Sand 3; P. Altmeyer 4; B. Mann 1; F. G. Bechara 4
Působiště autorů: Department of General and Visceral Surgery, Augusta Kranken Anstalt, Academic Teaching Hospital of the Ruhr-University Bochum, Germany 1; Department of Plastic and Reconstructive Surgery, Hannover Medical School, Hannover, Germany 2; Department of Physiological Science, University of California Los Angeles (UCLA), Los Angeles California, USA, and 3; Department of Dermatology and Allergology, Ruhr-University Bochum, Germany 4
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 3, 2007, pp. 67-70
BACKGROUND
Skin cancer requiring micrographic-controlled surgery is one of the most common human malignancies (1). The dorsal aspect of the nose is quite a common location for this type of cancer. When the defect is sizeable and incorporates both sides of the nose, reconstruction is difficult. The specific anatomy of the nose with multiple topographic subunits and functional considerations demand detailed operational planning by the surgeon. Based on the underlying bone and cartilaginous framework, the nose can be subdivided into several topographic subunits. The nasal sidewall, the dorsum, alar nostril, columella and tip can be distinguished (2). Specific characteristics of the skin must also be considered when planning reconstruction. The skin of the nasal sidewall and the dorsum is thin, smooth, and mobile whereas the skin of the alar nostril and tip is thick and pitted with sebaceous glands (3, 4).
Defects on the nasal sidewall can be closed with a variety of approaches. The commonly used paramedian forehead flap (PFF) is one of the most important nasal reconstructive procedures for medium to large sized defects (5). It has been called the workhorse of nasal reconstruction and used for centuries in different modifications. It is ideally used for unilateral defects exceeding 1.5 cm in diameter. The area vascularised by the supratrochlear vessel is considerable, which enables larger defects to be covered with this type of repair (6). Even larger defects covering one or more subunits or which are bilateral require a combination of different approaches. Convex subunits of the nose (nasal dorsum and tip) are frequently closed with the PFF. Concave or planar subunits such as the nasal sidewall are also sometimes – but not necessarily – reconstructed with skin grafts (7). Differential sculpting of the undersurface of the flap to match the contours of the defect allows great flexibility, hence the use of the PFF almost anywhere on the nose. In large defects, the PFF transposes thick sebaceous skin of the forehead to the nasal dorsum and lateral sidewall of the nose. The skin of the forehead is thicker than the thin skin on the nasal dorsum. This often results in excessively bulky flaps with a hump-like appearance on the nasal dorsum which require additional procedures (8). We present a feasible, single stage alternative to the median forehead flap for a selective group of patients with very prominent nasolabial folds and tissue laxity lateral to the resection borders. All patients required reconstruction of defects after skin cancer resection for lesions which were spread onto both sides of the nose, including the nasal sidewall and dorsum. Skin-laxity adjacent to the nasolabial fold is used in a bilateral V-Y shaped advancement flap to close bilateral defects on the lateral and frontal dorsum of the nose. We describe our experience using the latter flap design in a case series of 12 patients.
METHODS
Over a 3-year period all patients who had MOHS surgery defects repaired using the bilateral cheek-to-nose advancement flap were identified. The localization of the defect was the nasal dorsum, alone or in combination with the lateral sidewall of the nose (Fig. 1a). The defects were assessed by clinical inspection, photographs and notes regarding the site, extension, size, cartilage involvement and the topographic subunit involved. Two topographic subunits were differentiated into the nasal dorsum and sidewall. The main outcomes were assessed by the acceptability of the procedure by the patient, complications, and appearance by evaluating photographic records. Patients were asked to judge their overall satisfaction of surgery six months after reconstruction. Satisfaction survey consisted of a number scale (1 = completely satisfied, 2 = satisfied, 3 = moderate satisfaction, 4 = not satisfied, 5 = not satisfied at all). Additionally, an identical scale was used later for the surgeons’ evaluation of the reconstruction achieved. Patients were assessed by two board certified MOHS surgeons. All patients were evaluated after two weeks and six months. Complications during the postoperative period were also recorded.
Surgical Technique
All patients are operated with local anesthesia and Monitored Anaesthesia Care (MAC). One hour before surgery patients receive a single injection of antibiotic prophylaxis with 500 mg levofloxacin. The nose is prepped and draped in routine fashion. Local anesthesia is achieved with lidocaine with 1 : 100 000 epinephrine (adrenaline). The flap is designed in a bilateral airplane-wing fashion, ideally along relaxed skin tension lines (RSTLs), with an inferior-lateral V-Y tip (Fig. 1b). We use an aluminum foil pattern of the defect to approximate its extension/margins. If necessary the defects were extended to fit a topographic subunit. The inferior aspect of the flap lies within the nasolabial fold. The flap is dissected and mobilized to provide medial advancement. The myocutaneous pedicle of the flap lies within its lateral half. It is advisable that the flap is prepared rather thin at its medial aspect to prevent unnecessary bulging on the thin skinned nasal dorsum and lateral sidewall. After the flap and its pedicle are prepared they are advanced by gently easing the flap with a skin hook towards the median line of the nasal dorsum. The flap thickness must be revised to match the defect. Additional trimming may be necessary to get a thin subdermal layer in the medial parts which are covering the initial defect. Before closure gentle undermining around the defect minimizes tension and reduces scarring along the incisions. Dermal (subcutaneous) and epidermal (superficial) closure is performed separately. Flap inset begins with one central absorbable undyed monofilament suture (suture size UPS 5-0, Monocryl, Ethicon GmbH, Norderstedt, Germany) on the nasal dorsum for subcutaneous closure of the two medial sites of the flap. The rest of the flap is sutured with epidermal non-absorbable nylon sutures (suture size UPS 4-0, Ethilon, Ethicon GmbH, Norderstedt, Germany) in a half-buried vertical mattress stitch technique to evert wound edges. The secondary defect is closed, resulting in a Y configuration suture line. Sutures were removed after 7 days (Fig. 1c).
Fig. 1a. Pre-operative view on a large BCC involving the nasal dorsum and right nasal sidewall Fig. 1b. Planned operative repair delineating bilateral cheek-to-nose advancement flap for a defect involving the nasal dorsum and the right nasal sidewall Fig. 1c. Postoperative result after 7 days Fig. 1d. Postoperative follow-up at 6 months 
RESULTS
Between 2003 and 2006 twelve patients (n = 12) with defects after MOHS surgery on the upper and mid third of the nose with involvement of the nasal dorsum and the lateral sidewall were treated by closure with a bilateral cheek-to-nose advancement flap. All the repaired defects were limited to the skin without any cartilage involvement. The mean age of the patients was 67 years (range 42–81), 5 female and 7 male. Defect size varied between 1.1 x 2.3 cm and 2.8 x 3.5 cm. The mean size of the defects’ diameter was 2.9 cm (range 2.1–3.7 cm). All the defects were reconstructed in a single procedure with a bilateral cheek-to-nose advancement flapafter histological confirmation of tumor-free margins. The etiology of the defect was basal cell carcinoma (BCC) in ten patients. One patient had a BCC relapse and another patient was suffering from trichoepithelioma. The reconstructed defects were on the nasal dorsum and on one nasal sidewall in five cases. Five cases included the nasal dorsum and both nasal sidewalls, one patient’s defect was limited to the nasal sidewall and another patient’s defect to the nasal dorsum (Table 1). Patients’ mean satisfaction rate was 1.3 after 6 months with all patients being either completely satisfied or satisfied with the reconstruction achieved. The surgeons’ satisfaction rate was 1.75 after 6 months. The complete satisfaction rates are compiled in Table 1. All donor sites healed without any complications. Reviewing all twelve repairs no adverse effects were observed. No repair required a secondary procedure and to date no tumor recurrences have occurred.
Tab. 1. Table 1. Complete satisfaction rates (all cases in detail) 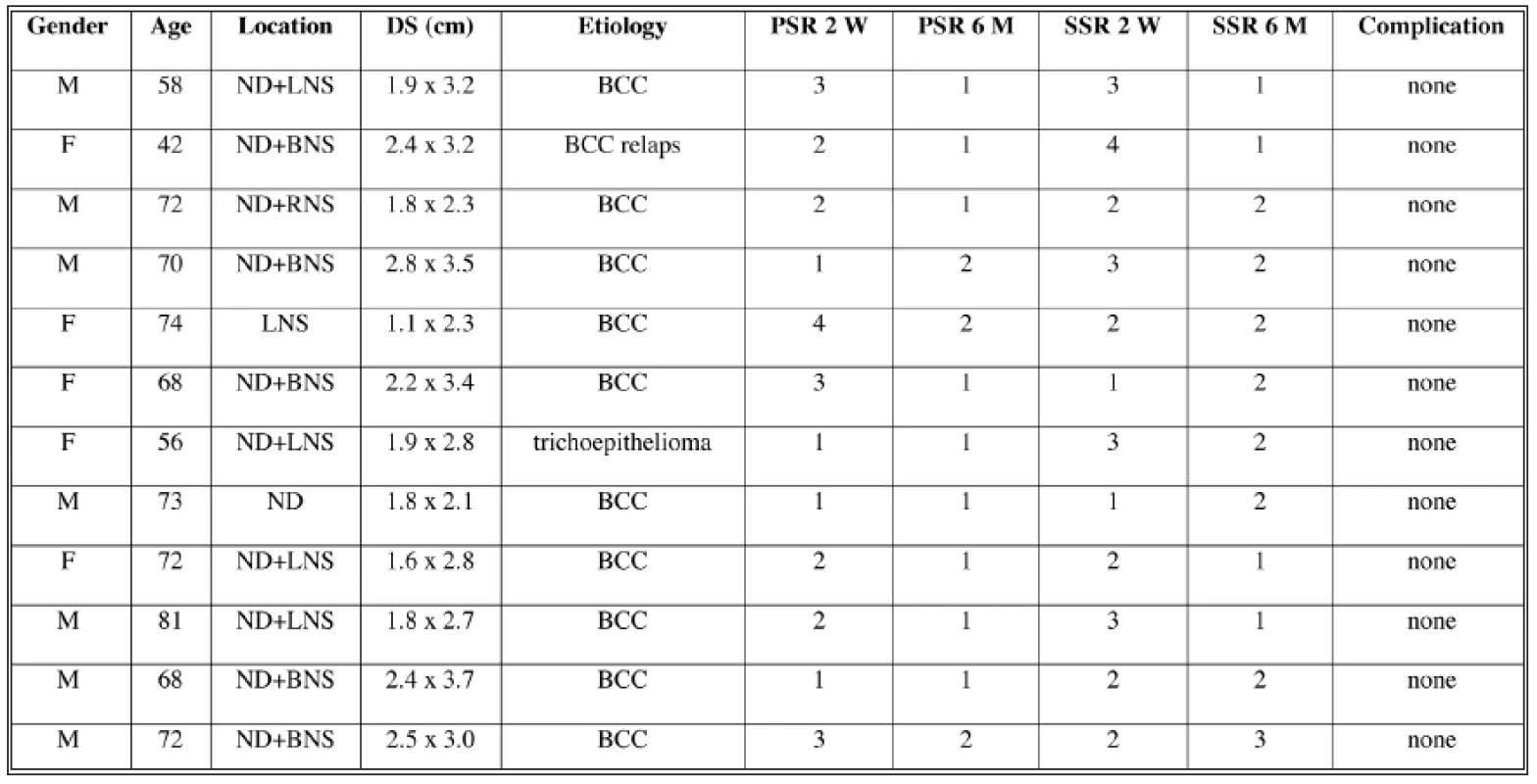
(M = male, F = female, ND = nasal dorsum, LNS = left nasal sidewall, RNS = right nasal sidewall, BNS = both nasal sidewalls, BCC = basal cell carcinoma, DS = defect size in cm, PSR = patients satisfaction rate, SSR = surgeons satisfaction rate, W = weeks, M = months) DISCUSSION
The reconstruction of cutaneous defects involving the superior two-thirds of the nose (nasal dorsum and paired lateral sidewalls) is demanding. Located prominently in the center of the face, the nose is one of the most noticed facial areas (9, 10). Expectations towards a cosmetic and unobtrusive repair are high and represent a challenging task for the reconstructive surgeon. Depending on the size and location of the defect several reconstructive procedures are available. For smaller skin defects, primary closure or healing by second intention is appropriate (11). For larger defects skin grafts can provide satisfactory results and are the easiest means for reconstruction (12). In contrast to the lower third of the nose with high density of sebaceous glands, the skin of the superior two-thirds has fewer sebaceous glands. It is thin, smooth, mobile and easier to match. The preauricular skin has been reported to be a good donor site for full-thickness skin grafts (13, 14). However in large defects which involve both the nasal dorsum and the lateral sidewall, skin grafts appear less than ideal (15). A patched-like appearance cannot always be prevented because of textural and color differences which disregard the topographical nasal subunits and their borders. Large defects however often require a regional flap, most commonly a paramedian forehead flap (PFF) based on the supratrochlear artery. The most common flap is either the single-stage forehead flap which has a deepithelialized pedicle or the two-stage PFF (16, 17). A downside of the latter flap design is that the pedicle must be divided and inset at a second stage after neovascularization occurs – mostly two or three weeks after the first procedure. Additionally a third procedure is often necessary because bulkiness is a common postoperative effect which must be thinned out in a subsequent intervention. Moreover the skin of the PFF is thicker than the regular skin of the nasal dorsum. When the flap is applied to the nasal dorsum, the nose acquires a hump it did not originally possess. An additional disadvantage of the PFF is the vertically oriented forehead scar and the limited length in non-hair-bearing forehead skin.
The bilateral cheek-to-nose advancement flap that we describe is a reasonable alternative for the PFF in a highly selective group of patients who are subject to closure of defects on the nasal dorsum and lateral sidewall and have prominent nasolabial folds. It is essential that strong tissue laxity above the nasolabial fold with excessive tissue is available for utilizing this flap technique. Patients with normal nasolabial folds and regular tissue laxity are unsuitable and should be considered for other reconstructive options. However patients with skin cancer are mostly older and often meet the requirement of adjacent reservoirs of tissue for this bilateral flap, which should therefore be taken into consideration when planning reconstruction (18). Our case series demonstrates that short - and long-term results achieved with the bilateral cheek-to-nose advancement flap are excellent. It is a single stage repair without any functional and moderate esthetic sacrifices with the condition that patients are appropriately screened and the indication is strictly applied. It transposes matching skin lateral and above the nasolabial fold towards the nose, which lies adjacent to the donor site. It is a random vascular flap which receives good blood supply from subcutaneous branches of the facial and angular artery. We observed no vascular impairment. The closure of the secondary defect is a suture line with a Y configuration hidden in the nasolabial fold which promotes unobtrusive appearance after MOHS surgery defect on the nose. The six-month function and cosmetic results were rated subjectively by the patient and objectively by two board certified MOHS surgeon as excellent (Fig. 1d).
CONCLUSIONS
The bilateral cheek-to-nose advancement flap is a reliable tool in the interventional portfolio of the reconstructive surgeon. It is suitable for a highly selective group of patients with deep nasolabial folds and pronounced laxity of the adjacent buccal skin. It is capable of restoring function and cosmesis of large bilateral MOHS surgery defects on the nasal dorsum and lateral sidewall in a satisfactory manner.
Acknowledgements
Written consent was obtained from the patient.
Address for correspondence:
Michael Sand, M.D.
Department of General and Visceral Surgery,
Augusta Kranken Anstalt, Academic Teaching Hospital
of the Ruhr-University Bochum, Germany
Bergstrasse 26
44791 Bochum, Germany
E-mail: michael.sand@ruhr-uni-bochum.de
Zdroje
1. Padgett JK.. Cutaneous lesions: benign and malignant. Facial Plast. Surg. Clin. North. Am., 13, 2005, p. 195–202.
2. Burget GC., Menick FJ. The subunit principle in nasal reconstruction. Plast. Reconstr. Surg., 76, 1985, p. 239–247.
3. Tardy ME. Tardy ME. Surgical anatomy of the nose. New York: Raven, 1990, p.25.
4. Dzubow LM. Repair of defects on nasal sebaceous skin. Dermatol. Surg., 31, 2005, p. 1053–1054.
5. Rohrich RJ., Griffin JR., Ansari M., Beran SJ., Potter JK. Nasal reconstruction – beyond aesthetic subunits: a 15-year review of 1334 cases. Plast. Reconstr. Surg., 114, 2004, p. 1405–1416.
6. Potparic Z., Fukuta K., Colen LB., Jackson IT., Carraway JH. Galeo-pericranial flaps in the forehead: a study of blood supply and volumes. Br. J. Plast. Surg., 49, 1996, p. 519–528.
7. Yoon T., Benito-Ruiz J., Garcia-Diez E., Serra-Renom JM. Our algorithm for nasal reconstruction. J. Plast. Reconstr. Aesthet. Surg., 59, 2006, p. 239–247.
8. Arden RL., Nawroz-Danish M., Yoo GH., Meleca RJ., Burgio DL. Nasal alar reconstruction: a critical analysis using melolabial island and paramedian forehead flaps. Laryngoscope, 109, 1999, p. 376–382.
9. Nguyen TH. Staged cheek-to-nose and auricular interpolation flaps. Dermatol. Surg., 31, 2005, p. 1034–1045.
10. Singh DJ., Bartlett SP. Aesthetic considerations in nasal reconstruction and the role of modified nasal subunits. Plast. Reconstr. Surg., 111, 2003, p. 639–648.
11. Mott KJ., Clark DP., Stelljes LS. Regional variation in wound contraction of mohs surgery defects allowed to heal by second intention. Dermatol. Surg., 29, 2003, p. 712–722.
12. Gurunluoglu R., Shafighi M., Gardetto A., Piza-Katzer H. Composite skin grafts for basal cell carcinoma defects of the nose. Aesthetic Plast. Surg., 27, 2003, p. 286–292.
13. Breach NM. Pre-auricular full-thickness skin grafts. Br. J. Plast. Surg., 31, 1978, p. 124–126.
14. Corwin TR., Klein AW., Habal MB. The aesthetics of the preauricular graft in facial reconstruction. Ann. Plast. Surg., 9, 1982, p. 312–315.
15. Silapunt S., Peterson SR., Alam M., Goldberg LH. Clinical appearance of full-thickness skin grafts of the nose. Dermatol. Surg., 31, 2005, p. 177–183.
16. Lee JJ., Zimbler MS. Paramedian forehead flap for the reconstruction of large nasal defects. Ear Nose Throat J., 83, 2004, p. 322.
17. Park SS. The single-stage forehead flap in nasal reconstruction: an alternative with advantages. Arch. Facial Plast. Surg., 4, 2002, p. 32–36.
18. Diepgen TL., Mahler V. The epidemiology of skin cancer. Br. J. Dermatol., 146, 2002, Suppl. 61, p. 1–6.
Štítky
Chirurgie plastická Ortopedie Popáleninová medicína Traumatologie
Článek ČESKÉ SOUHRNY
Článek vyšel v časopiseActa chirurgiae plasticae
Nejčtenější tento týden
2007 Číslo 3- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Metamizol v léčbě různých bolestivých stavů – kazuistiky
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Léčba akutní pooperační bolesti z pohledu ortopeda
-
Všechny články tohoto čísla
- COMMEMORATING THE 125th ANNIVERSARY OF THE BIRTHOF PROFESSOR FRANTIŠEK BURIAN
- GRAFTING POSTERIOR TIBIAL NERVE WITH IPSILATERAL SURAL NERVE CABLES IN LEG REPLANTATION – A COMMON SENSE APPROACH
- BILATERAL CHEEK-TO-NOSE ADVANCEMENT FLAP: AN ALTERNATIVE TO THE PARAMEDIAN FOREHEAD FLAP FOR RECONSTRUCTION OF THE NOSE
- CASE SERIES: VARIATIONS IN THE EMBRYOLOGY OF CONGENITAL MIDLINE CERVICAL CLEFTS
- VACUUM-ASSISTED CLOSURE (VAC) THERAPY IN THE MANAGEMENT OF DIGITAL PULP DEFECTS
- UNEXPECTED ULNAR NERVE SCHWANNOMA. THE REASONABLE RISK OF MISDIAGNOSIS
- ČESKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- VACUUM-ASSISTED CLOSURE (VAC) THERAPY IN THE MANAGEMENT OF DIGITAL PULP DEFECTS
- GRAFTING POSTERIOR TIBIAL NERVE WITH IPSILATERAL SURAL NERVE CABLES IN LEG REPLANTATION – A COMMON SENSE APPROACH
- BILATERAL CHEEK-TO-NOSE ADVANCEMENT FLAP: AN ALTERNATIVE TO THE PARAMEDIAN FOREHEAD FLAP FOR RECONSTRUCTION OF THE NOSE
- UNEXPECTED ULNAR NERVE SCHWANNOMA. THE REASONABLE RISK OF MISDIAGNOSIS
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



