-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
The use of micropulse laser in patients with diabetic macular edema at the Department of Ophthalmology, Faculty Hospital Hradec Králové
Authors: Š. Veselá; L. Hejsek; A. Stepanov; J. Dusová; J. Marak; N. Jirásková; J. Studnička
Authors place of work: Oční klinika Fakultní nemocnice Hradec Králové
Published in the journal: Čes. a slov. Oftal., 74, 2018, No. 2, p. 53-58
Category: Původní práce
doi: https://doi.org/10.31348/2018/1/2-2-2018Summary
Introduction:
Diabetic macular edema (DME) is the most frequent cause of decreased vision in patiens with diabetes type 2. DME is caused by increased permeability of macular capillaries. The aim of our study was to retrospectively evaluate the results of micropulse laser treatment, 577 nm wavelength, in pacients with DME with follow-up three months and one year.
Methods:
The retrospective trial with one year follow-up includes 63 eyes of 37 patients with diabetic macular edema treated from September 2015 to January 2017. Most patients had diabetes type 2 (34 patients), 3 patients had diabetes type 1. Diffuse DME was diagnosed in 54 eyes, focal DME in 9 eyes. Most of the patients (42 eyes) suffered from non proliferative diabetic retinopathy, 21 eyes showed signs of proliferative retinopathy. DME lasted on average for 29 months before initiating with micropulse laser (median 21 months).
On average 1,56 laser visits were needed for the treatment of 1 eye, usually in 3 months interval. Photocoagulation of macula was performed in all patients by micropulse laser, 577 nm wavelenght/IQ 577TM IRIDEX). We used 5 % duty cycle. The average glycated hemoglobin in the group was 66,8 mmol/mol, maximal 100 mmol/mol. Estimated data were statistically evaluated by Friedman and Dunn´s test.
Results:
At the end of 1 year period we found out improvement in BCVA (increase of at least 5 letters of ETDRS charts) in 20 eyes, 25 eyes showed stabilisation of BCVA (alltogether 71 % of the group), in 18 eyes we found out decrease of BCVA of more than 5 letters of ETDRS charts. On average we estimated decrease of visual acuity from 62 to 61,1 letters (p > 0,05). After one year we estimated 63 μm CRT decrease on average, from 442 μm to 379 μm (p= 0,0124).
Conclusion:
In our group of DME patiens treated by micropulse laser we have estimated BCVA stabilisation and signifiant improvement of macular edema in ¾ eyes, confirmed by OCT. We have estimated clinically significant decrease of macular edema in the whole group with one-year follow-up.
Keywords:
micropulse laser, diabetic macular edema, optical coherence tomography, central retinal thickness, laser retinal photocoagulation
INTRODUCTION
Diabetic macular edema (DME) is the most common cause of loss of sight in persons aged younger than 60 years in developed countries (6). The incidence and prevalence of diabetes mellitus (DM) is increasing worldwide (5). Chronic hyperglycaemia leads to the creation and accumulation of advanced end products of glycation, the formation of microaneurysms, alteration of the blood-retinal barrier, loss of pericytes and obstruction of the flow of blood through capillaries. This all causes ischaemia of the retina and an increase in the generation of angiogenic factors, e.g. vascular endothelial growth factor (VEGF), which among other factors increases the permeability of capillaries. An important role is also played by inflammation; as a result of the action of prostaglandins and inflammatory mediators, leukostasis occurs in capillaries and there is a further increase in the permeability of the vascular wall (1).
Laser treatment of the retina in the case of DME has been the gold standard of treatment in the last 30 years. The importance of laser treatment of the retina consists rather in the stabilisation of retinopathy and avoidance of blindness. Improvement of central visual acuity following photocoagulation treatment is not the rule, and in the case of diffuse edema it is rather a rare occurrence (2). At present procedures are known which more effectively improve central visual acuity (application of corticosteroids and anti-VEGF preparations intravitreally), but these are not available to all patients due to the indication restrictions on payment valid for the Czech Republic. Treatment with VEGF blockers is paid for in the case that the current value of glycated haemoglobin is no older than 3 months and is lower than 70.0 mmol/mol. The recommended level of total cholesterol is lower than 4.8 mmol/l. The exclusion criteria for the commencement of treatment are condition following ictus, blood pressure higher than 140/90 mmHg, level of serum creatinine higher than 180 µmol/l and advanced complications of the proliferative form of diabetic retinopathy. Treatment is restricted to one eye and may be commenced in patients who suffer from DME that is a cause of deterioration of vision within the range of 6/12 – 6/30 in the case of affliction of the worse seeing eye. In the case of affliction of the only seeing eye it is possible to commence treatment in the case of visual acuity of 6/12 – 6/48. The period of duration of DME should be maximally two years, and central retinal thickness (CRT) 300 µm or more according to OCT.
The therapeutic effect of laser photocoagulation on DME was first documented in the Early Treatment of Diabetic Retinopathy Study (ETDRS) in 1979. This study incorporated 754 eyes with DME and mild to medium diabetic retinopathy. The treatment was most effective in eyes with clinically significant macular edema (CSME) (3).
The micropulse laser represents a new modality in the treatment of retinal vascular pathologies. It acts as a photo-stimulating agent on the chromophores in the layer of the retinal pigment epithelium. Instead of photo-destruction the cells are stimulated, iatrogenic collateral damage to the retina does not occur and there is no formation of cicatricial changes, it does not damage the photoreceptors or the choroid (9). Micropulse laser treatment can be repeated in areas of the retina that have already been treated. The continual laser beam is divided into several short, repeating low-energy pulses, separated by pauses, which enables cooling of the tissue between the laser pulses and enables the use of lower energy per one pulse. The micropulse laser can also be used as supplementary treatment together with other therapeutic options (9). The clinical results are similar in comparison with conventional laser coagulation of the retina (10).
Aim: The aim of our observation was to evaluate the effectiveness of treatment with micropulse laser in patients with DME.
METHOD AND PATIENTS
The retrospective study with an observation period of 1 year following treatment incorporates 63 eyes of 37 patients with DME, treated in the period from September 2015 to January 2017. Patients with type 2 DM predominated within the cohort (34 patients), type 1 DM was represented in 3 patients. Diffuse DME was diagnosed in 54 eyes, focal DME in 9 eyes. Prior treatment was as follows: conventional laser coagulation of the retina (60 eyes, 95%), which was terminated at the latest 3 months before the commencement of treatment with micropulse laser. Before treatment with micropulse laser some patients (34 eyes) had been treated with other modalities, namely intravitreal applications of anti-VEGF preparations (7 eyes), applications of triamcinolone (2 eyes) and pars plana vitrectomy (PPV) in 25 eyes. The majority (42 eyes) had non-proliferative form of diabetic retinopathy, 21 eyes manifested signs of proliferative diabetic retinopathy. The average length of duration of DME in the entire cohort was 29 months (median 21 months). The cohort includes patients who had not responded to other therapy (treatment with anti-VEGF preparations, treatment with triamcinolone, PPV), as well as patients who did not meet the indication criteria for payment of treatment of DME with anti-VEGF preparations valid for the Czech Republic.
Within the cohort, BCVA was evaluated on ETDRS optotypes, and CRT on OCT (Cirrus HD OCT, Zeiss) both before laser treatment, as well as 3 and 12 months afterwards. At each visit an examination of intraocular tension was performed with the aid of noncontact tonometry, and an examination of the anterior segment of the eye was conducted on a slit lamp. The posterior ocular segment was examined biomicroscopically, and photography of the ocular fundus was performed on a fundus camera (FF 450 + IR, Zeiss) at each visit.
On average 1.56 laser sessions were required for the treatment of 1 eye, as a rule the patients were monitored at 3 monthly intervals. In all patients photocoagulation of the macula was performed using a micropulse laser with a wavelength of 577 nm (IQ 577TM IRIDEX). A 5% micropulse duty cycle mode of the laser beam was used. This means that upon a total exposure of 200 ms, the active dose of the laser was divided into 100 micropulses, with a total length of 5%, therefore 10 ms. Each micropulse lasted 2.0 ms, in which the laser was switched on for 0.1 ms and off for 1,9 ms. The titration of energy was performed in the healthy retina close to the edematous retina. The energy was progressively increased up to the level where the beam was visible on the retina. Then micropulse mode was set, exposure of 200 ms and energy of 30-50% titrated energy. Beams with a size of 160 µm were applied confluently. Micropulse treatment was always applied according to the OCT map.
During observation, laser photocoagulation of the central periphery or in supplementing panretinal photocoagulation continued in 18 eyes, in 3 eyes application of anti-VEGF preparation was performed, and 3 eyes underwent PPV.
The obtained data in the cohort was statistically processed with the aid of a Friedman and Dunn's test. During the course of observation of the patients we also determined any applicable adverse effects of laser treatment.
RESULTS
In the entire cohort of 63 eyes, initial average BCVA was 62 letters, in 14 eyes (22%) BCVA was worse than 50 letters and in 5 eyes (8%) BCVA was worse than 40 letters. Average initial CRT was 442 µm and in 18 eyes (29%) we measured initial CRT of more than 500 µm. In 4 eyes high DME was determined at the beginning of observation, with CRT of more than 800 µm (6.4%) of cohort.
The development of BCVA and CRT in the entire cohort is illustrated in table 1. At the follow-up after three months we documented an improvement of BCVA (gain of at least 5 letters of ETDRS optotypes) in 12 eyes (19% of cohort), stabilisation of BCVA (gain of ± 4 letters of ETDRS optotypes) in 26 eyes (41%) and in 25 eyes (40%) there was a decrease of BCVA (decrease by more than 5 letters of ETDRS optotypes). There was a reduction of CRT in 38 eyes (60%), in 25 eyes (40%) macular edema was not reduced.
Tab. 1. BCVA and CRT parameters in the whole group of patients treated by micropulse laser 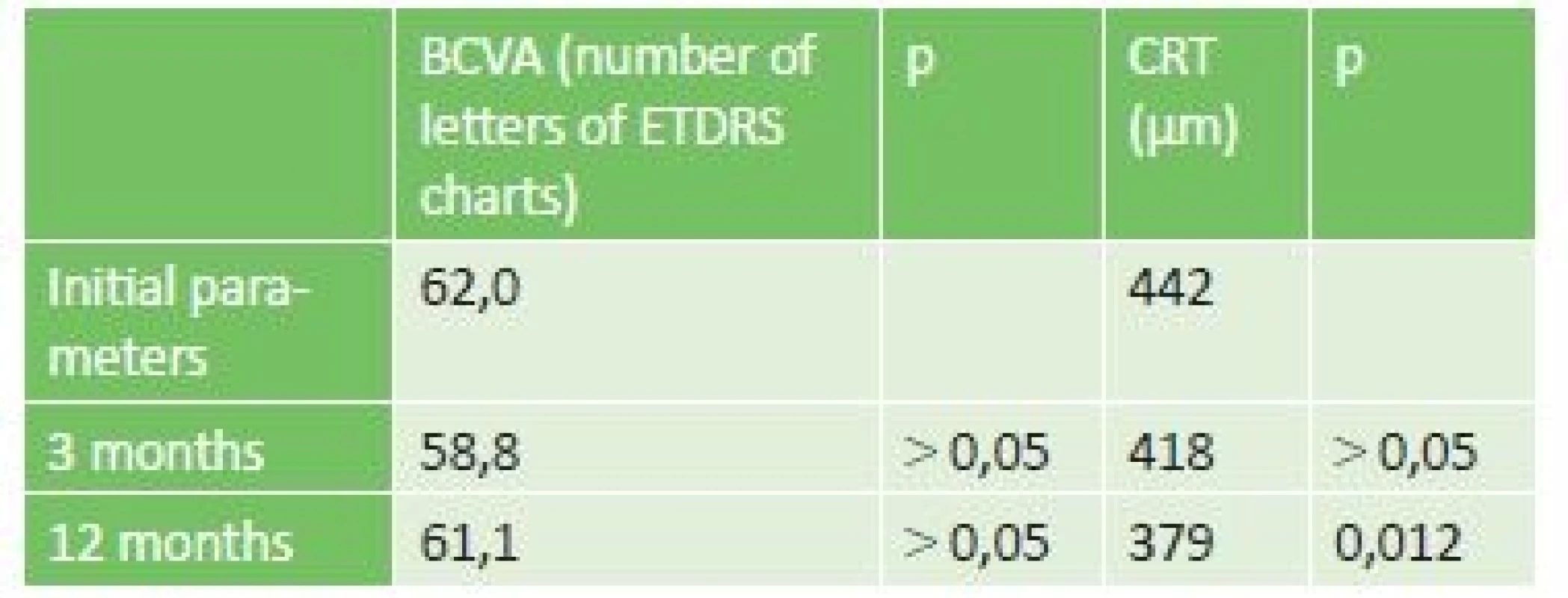
At the end of the one-year observation period we determined an improvement of BCVA by at least 5 letters of ETDRS optotypes in 20 eyes and stabilisation in 25 eyes (45 eyes, 71% of cohort), in 18 eyes (29% of cohort) there was a decrease of BCVA by more than 5 letters of ETDRS optotypes. We documented a reduction of CRT in 44 eyes (70%), in 19 eyes (30%) macular edema was not reduced.
The average value of glycated haemoglobin (HbA1c) in the cohort was 66.8 mmol/mol, max. value 100 mmol/mol. According to requirement the laser was supplemented, on average during the course of one year 1.56 sessions were applied for the treatment of one eye, as a rule at an interval of 3 months.
The development of BCVA and CRT in the subgroup of eyes which before treatment with micropulse laser had been treated only with conventional laser coagulation of the retina (21 eyes, 33% of cohort) is illustrated in table 2. At the end of the three-month observation period we documented a gain of at least 5 letters of ETDRS optotypes in 3 eyes (14.3% of cohort), stabilisation of BCVA in 11 eyes (52.4%) and in 7 eyes (33.3%) there was a deterioration of vision by more than 5 letters of ETDRS optotypes. We determined a reduction of CRT in 11 eyes (52%), in 10 eyes edema was not reduced (48%). At the end of the one-year observation period we recorded an improvement of BCVA by at least 5 letters of ETDRS optotypes in 6 eyes (29%), in 10 eyes stabilisation of vision was achieved (48%) and in 5 eyes BCVA deteriorated by more than 5 letters (23%). We determined a reduction of CRT in 16 eyes (76%), in 5 eyes (24%) macular edema was not reduced. The average value of HbA1c in this group was 66.4 mmol/mol, and the average duration of DME was 24.1 months (median 12 months). In this group an average of 1.65 laser treatments of the retina were applied per 1 eye.
Tab. 2. BCVA and CRT parameters in the subgroup of eyes treated only by conventional laser photocoagulation before micropulse laser treatment 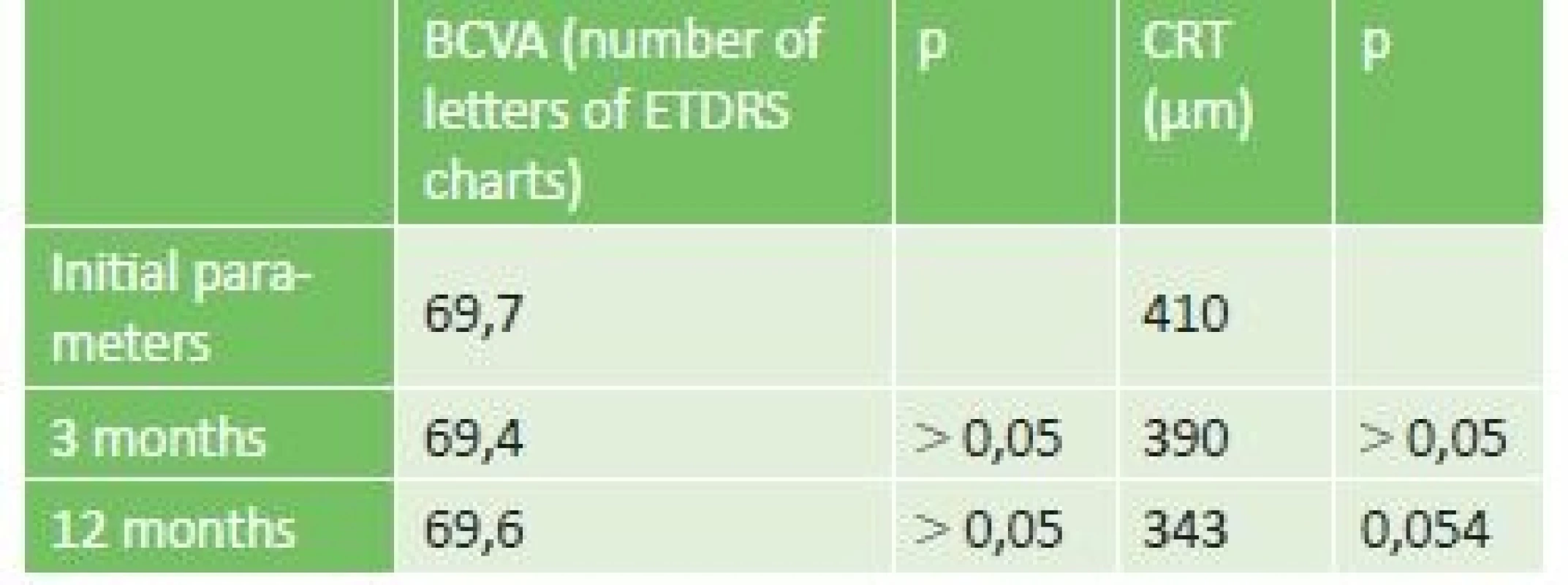
Case report
The patient was a 52 year old man with type 2 diabetes on insulin therapy since 1998, after amputation of the right lower limb due to chronic extensive defects in diabetic neuropathy, on dialysis due to terminal stage of diabetic nephropathy with massive proteinuria. In 2009 he had suffered myocardial infarction. The patient was observed for ischaemic heart disease, ischaemic disease of the lower limbs, arterial hypertension and congestive heart failure. In 2009 he had suffered from sepsis following an extensive abscess in the gluteal region and phlegmona of the thigh. At the beginning of 2016 glycated haemoglobin was 84 mmol/mol.
DME was diagnosed in both eyes in 2007, in both eyes there were signs of medium advanced non-proliferative diabetic retinopathy (fig. 1, 2). The patient attended examinations regularly, panretinal photocoagulation and photocoagulation of the centre of the retina were progressively performed in both eyes. In the right eye we determined progression of a cataract during the course of our observation. In this eye the patient underwent uncomplicated phacoemulsification with implantation of an IOL. Treatment of the centre of the retina by micropulse laser was performed twice in both eyes. Initial BCVA in the right eye was 20/63 and CRT 495 µm (fig. 3), after 6 months 20/40 and CRT 266 µm (fig. 4). In the left eye initial BCVA was 20/40 and CRT 395 µm (fig. 5), after 6 months BCVA remained at 20/40 and CRT was reduced to 284 µm (fig. 6). There was a substantial reduction of macular edema and a disappearance of the majority of the neuroretinal cyst in the macular landscape of both eyes. Following repeated laser treatment of the central landscape of the retina by micropulse laser we demonstrated an anatomical and functional improvement in a polymorbid, poorly compensated diabetic patient who did not meet the indication restrictions for payment of application of anti-VEGF (DME diagnosed in 2007). However, after one year in February 2017 we again observed a growth of cystoid macular edema in both eyes. BCVA in the right eye was 20/63 and CRT 384 µm, in the left eye BCVA was 20/40 and CRT 484 µm. We shall continue to treat the patient further with micropulse laser.
Fig. 1. Initial fundus photography of right eye: stable retinal periphery after panretinal laser photocoagulation, with macular edema. 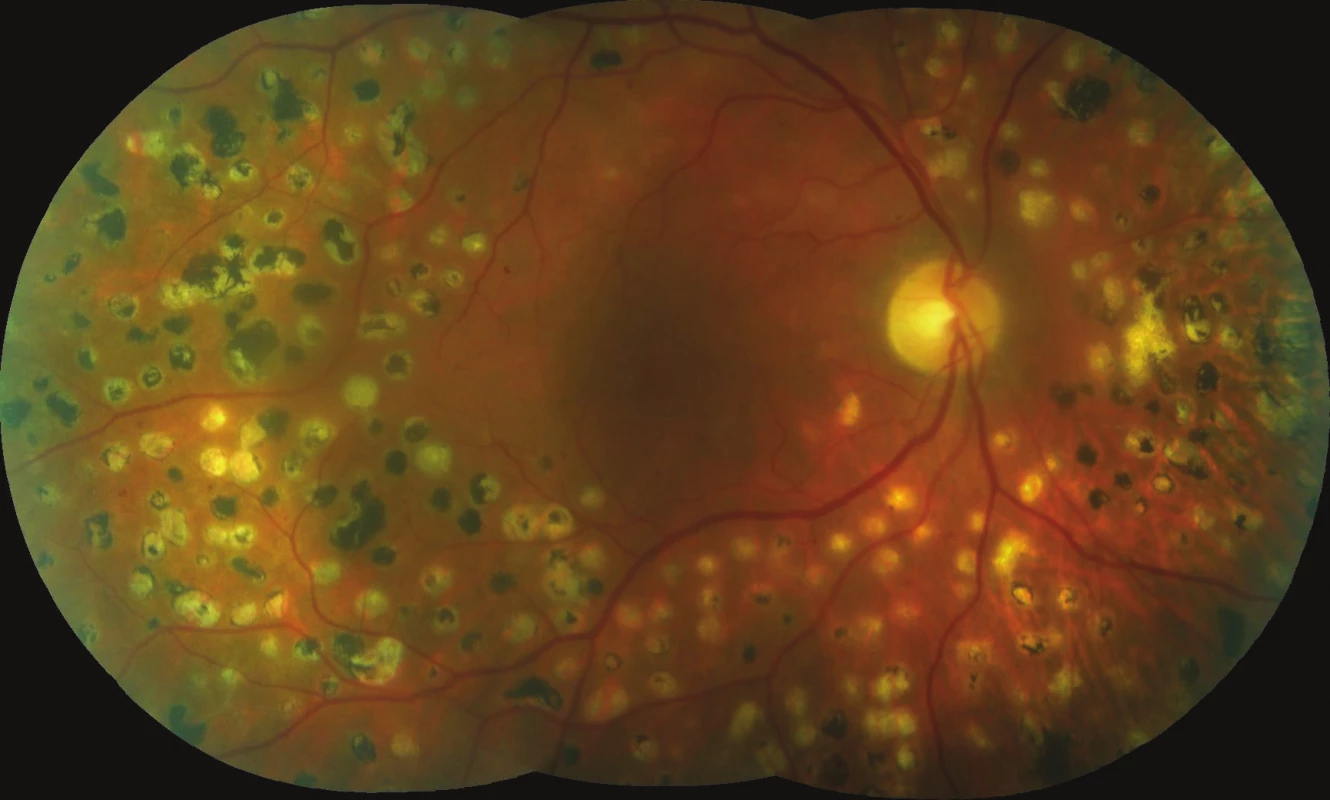
Fig. 2. Initial fundus photography of left eye: edema in the central area, several microaneurysms and intraretinal haemorrhages, spots after partial panretinal photocoagulation. 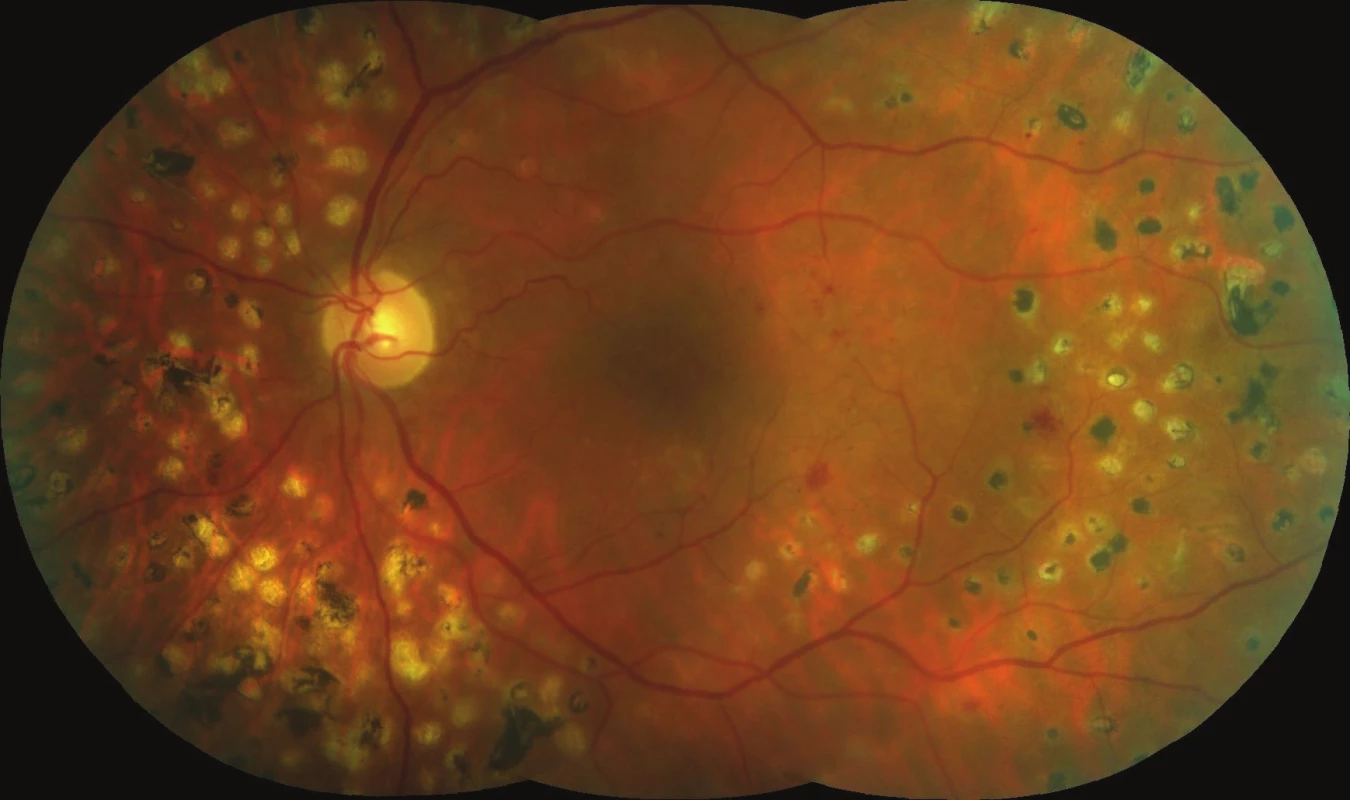
Fig. 3. OCT image of right eye before micropulse laser treatment: cystoid macular edema, CRT 495 μm. 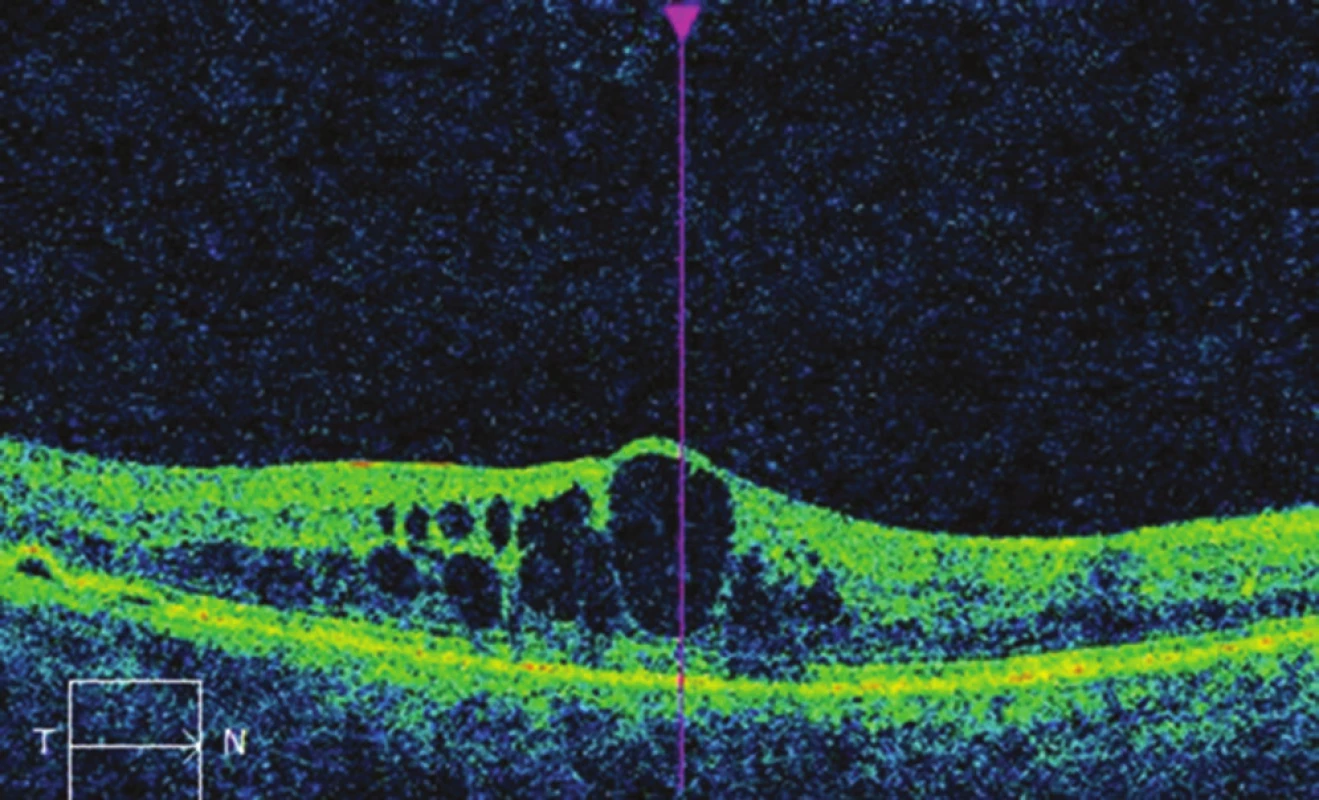
Fig. 4. OCT image of right eye after micropulse laser treatment of the central area: decrease of ocular edema, CRT 266 μm. 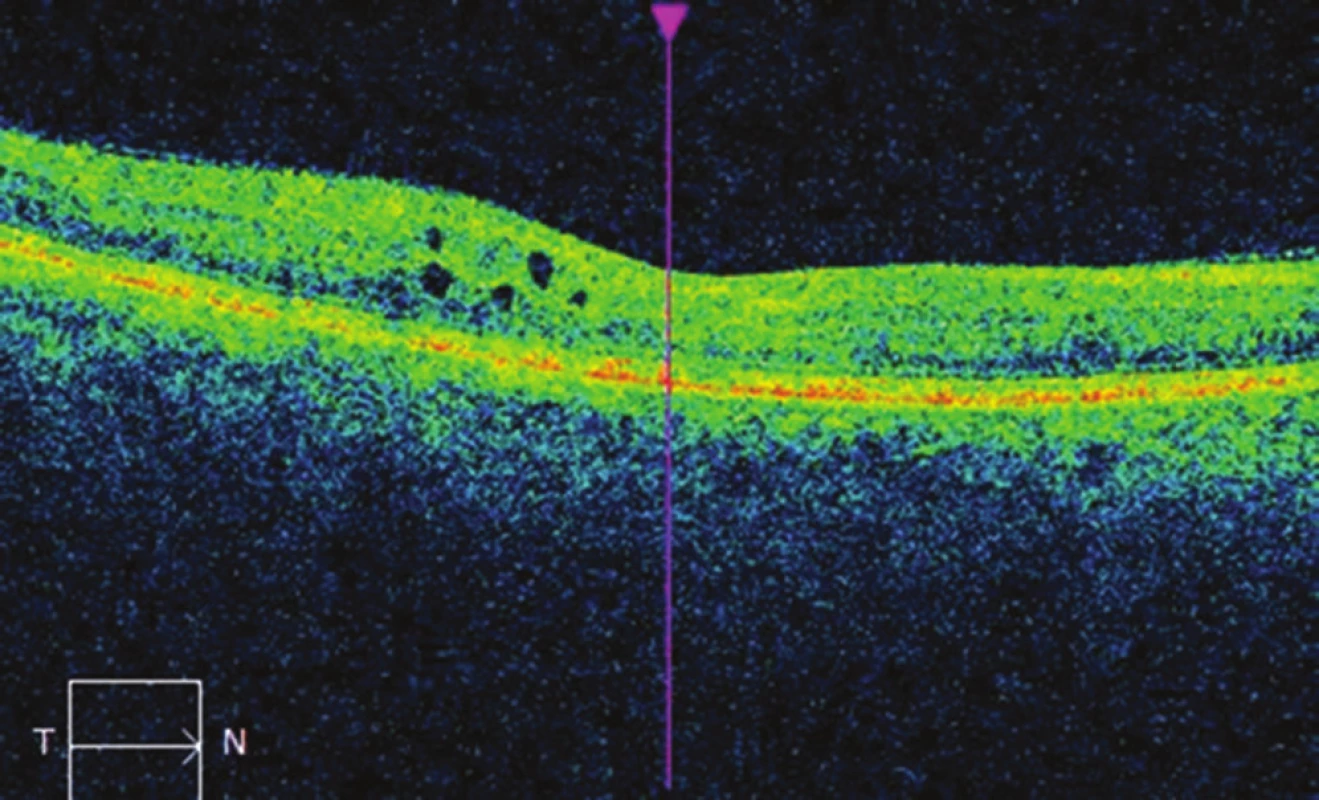
Fig. 5. OCT image of left eye before micropulse laser treatment: cystoid macular edema, CRT 395 μm. 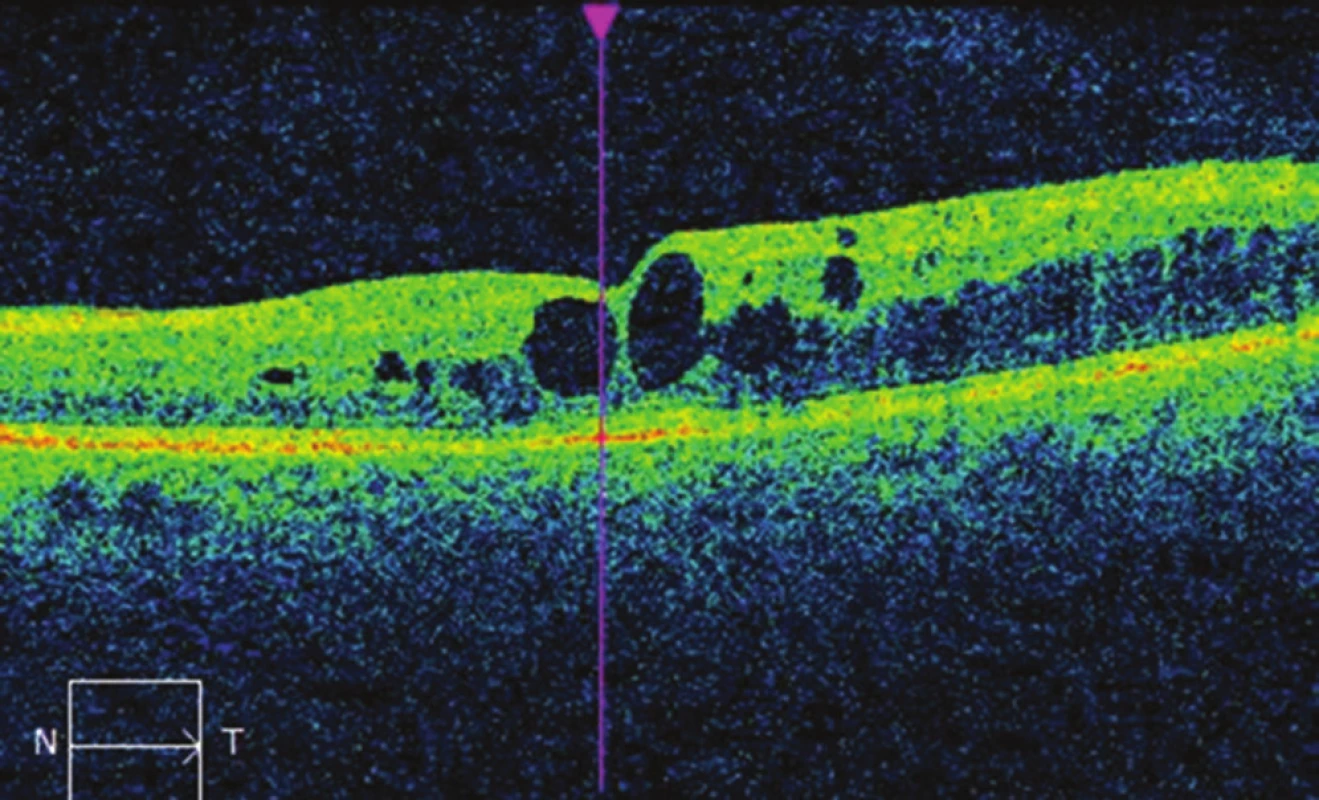
Fig. 6. OCT image of left eye after micropulse laser treatment: decrease of macular edema, CRT 284 μm. 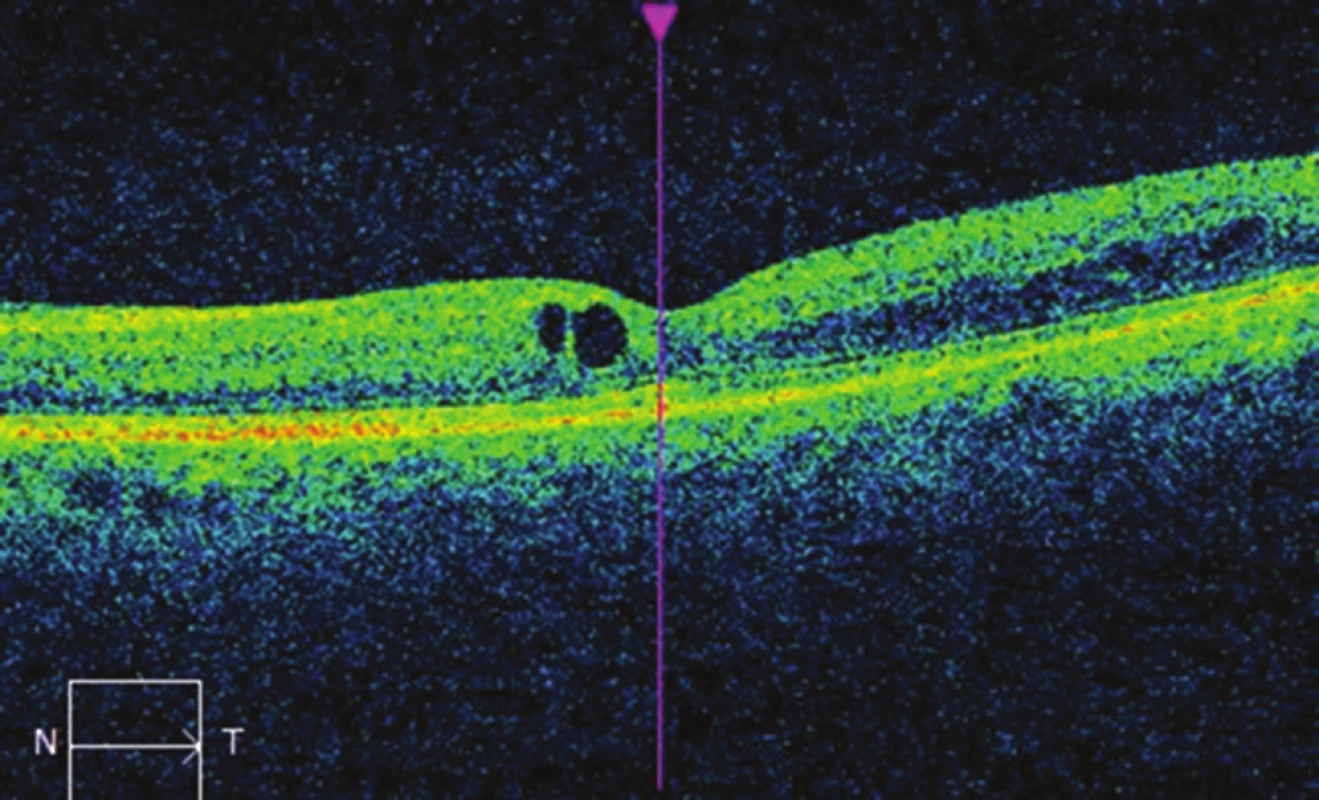
DISCUSSION
In this study we are focusing on the results of the use of a micropulse laser with a wavelength of 577 nm on patients with DME. Some studies that have evaluated the effect of a micropulse laser on DME have pointed to the fact that diode and conventional argon lasers are equally effective (9, 11). Yellow light with a wavelength of 577 nm is suitable for use in the treatment of macular pathologies, because it is well absorbed by melanin and haemoglobin, but only minimally by macular xanthophylls. Although no study has documented a clinically significant difference in the results in relation to the used wavelength of the laser, a yellow laser has certain advantages. It is better absorbed by melanin than a laser with a wavelength of 810 nm. Therefore, the micropulse laser has a better effect on the cells of the RPE. A further advantage is that it causes smaller dispersion than a laser with a wavelength of 532 nm. As a result, energy can be concentrated into a small volume, which enables the reduction of energy and a shortening of the pulse duration (11).
Lavinsky et al. in their study, which in the characteristics of the patients corresponds to our cohort of patients, treated only with conventional laser photocoagulation, compared treatment of the centre of the retina by beams with a normal density and treatment of the retina by confluent beams, and in both groups documented the best results in patients with one-year observation. They were of the opinion that healing and renewal of the retina takes place progressively, and that improvement of BCVA may in fact precede the reduction of CRT (7). In our study we documented an improvement or stabilisation of BCVA in 76% of eyes and a reduction of CRT in 76% of cases in the subgroup of eyes treated only by conventional laser coagulation before micropulse therapy. It shall be appropriate to continue in the observation in order to obtain further results.
Our results are consistent with the results of Korean authors, who documented the results of treatment of DME with micropulse laser with the same wavelength and evaluated a cohort over an average observation period of 7.9 months. We determined a similar effect on the reduction of CRT, but in our cohort we documented stabilisation of BCVA at 61.1 letters (deterioration of vision by 0.9 letters) unlike their cohort, in which an average gain of 5 letters was documented at the end of the observation period. We explain these differences primarily with reference to the fact that in our patients an average of 1.56 laser sessions were performed per 1 eye, while an average of 3 laser treatments were applied in the cohort of Korean patients. Further reasons may be due to the different configuration of the parameters of the laser (use of laser with 15% duty cycle, beam of 100 µm).
The results of our study are similar to the study by Závorková et al., which also demonstrated a reduction of CRT at follow-up examinations after 6 and 12 months, with stabilisation of BCVA (12). In the compared cohort, in the majority of patients the technique of laser treatment of the macula according to the ETDRS study was used, whereas in our cohort we used the technique of confluent beams. An average of 1.56 sessions was required for the attained results in our cohort, whereas in the previous cohort an average of 3 sessions was used.
According to the recommendation of the laser manufacturer, use of a micropulse laser on DME is particularly effective in patients with mild DME and with good initial BCVA (4). In 22% of eyes from the entire cohort, BCVA was worse than 50 letters, and in 8% of eyes BCVA was worse than 40 letters. In almost one third (29%) of eyes, the initial measurement of CRT was more than 500 µm, and in 6.4% of the cohort high DME was determined at the beginning of observation, with CRT of more than 800 µm. This may explain why an improvement of BCVA was not attained throughout the entire cohort and why there was not a more substantial reduction of CRT.
A prospective study by Nakamura et al., focusing on the results of treatment by micropulse laser and the functional and morphological changes only 3 months after laser treatment of the centre of the retina, published a statistically significant anatomical and functional improvement after 3 months. In our cohort we observed a statistically significant reduction of DME and stabilisation of BCVA after one year of treatment. A possible reason is the stricter exclusion criteria of this study, namely PPV and LPC of the retina 6 months or less before the commencement of micropulse treatment. In addition a 15% duty cycle mode was used (8).
A further study by Yoon Hyung Kwon et al. focused on the risk of unexpected chorioretinal damage following treatment by micropulse laser. It was recommended to set the duration of one pulse at 20 ms, the number of laser beams at maximum 2000, titration of energy in the place of non-edemous retina and use of 50-70% of this energy. It is also appropriate to use pattern mode, in which several beams are applied simultaneously, which is more comfortable for the patient and reduces the risk of non-co-operation on the part of the patient (11).
CONCLUSION
In our cohort we demonstrated an improvement and stabilisation of BCVA in patients with DME treated with micropulse laser after one-year evaluation in almost ¾ of the total number of eyes. We achieved a statistically significant reduction of macular edema in all eyes in the observed cohort.
Our cohort represents patients whom we encounter in regular clinical practice. Before treatment with micropulse laser a total of 95% of eyes had been treated by another therapeutic modality (PPV, application of anti-VEGF preparation, triamcinolone, treatment of retina by conventional laser). Without subsequent treatment by micropulse laser, a further deterioration may have occurred as a result of the progressive character of the pathology.
Treatment by micropulse laser is an effective method, which is safe upon the correct configuration of the parameters of the laser and suitably selected energy of the laser. Its main advantage is that no scars form on the retina, thereby preventing the possible occurrence of scotomas in the visual field. Another advantage of treatment by micropulse laser is that in the case of insufficient effect we can repeat the treatment or combine it with other methods of treatment, e.g. with anti-VEGF therapy.
This study was published in the form of a lecture at the 18th Vejdovský Olomouc Science Day in 2017.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Department of Ophthalmology, University Hospital Hradec Králové
Sokolská 581
500 05 Hradec Králové
Zdroje
1. Das et al.: Diabetic macular edema: Pathophysiology and novel therapeutictargets. Ophthalmology 2015;122 : 1375-94.
2. Diabetic Retinopathy Clinical Research Network: A randomized trial comparing intravitreal trimacinolon eacetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology 115 : 1447-1459.
3. Early Treatment DiabeticRetinopathy Study Research Group: Photocoagulation for diabetic macular edema. Early Treatment DiabeticRetinopathy Study report number 1. Arch Ophthalmol 1985 Dec; 103(12):1796-806.
4. Feistmann, JA., Rosenthal, JL.:.Making the Jump to Micro Pulse Laser Therapy for Treating theMacule, An effective first-line therapy adjunct to current ttreatments. Micro Pulse safely treats areas of the retina including the fovea. Iridex [online]: http://www.iridex.com/Portals/0/pdf/Rosenthal_Feistmann_webinar_writeup.pdf.
5. Kahn, HA., Bradley, RF.: Prevalence of diabetic retinopathy. Age, sex, and duration of diabetes. Br J Ophthalmol 1975;59 : 345–9
6. Kahn, HA., Hiller, R.: Blindness caused by diabetic retinopathy. Am J Ophthalmol 1974; 78 : 58–67.
7. Lavinsky, D., Cardillo, JA., Melo, LA. et al.: Randomized clinical trial evaluating ETDRS versus normalorhigh-density micropulse photocoagulation for diabetic macular edema. Invest Ophthalmol Vis Sci.; 2011 : 52 : 4314–4323.
8. Nakamuram, Y., Mitamura, Y., Ogata, K. et al.: Functional and morphological ganges of macula after subthreshold micropulse diode laser photocoagulation for diabetic macular oedema. Eye (London); 2010 : 24 : 784–788.
9. Sipravasad, S., Elagouz, M., McHugh, D. et al.: Micropulsed diode laser therapy:Evolution and clinical applications, Survey Ophthalmol, November–December; 2010 : 55 (6): 516–530.
10. Stanga, PE., Reck, AC., Hamilton, AMP. et al.: Micropulse laser in thetreatment of diabetic macular edema, Semin Ophthamol; 1999 : 14(4): 210-213.
11. Yoon, HK., Dong, KL., Oh, W K., et al.: The Short-term Efficacy of Subtreshold MicropulseYellow (577-nm) Laser Photocoagulation for Diabetic MacularEdema, Korean J Ophthalmol.; 2014 : 28(5): 379–385.
12. Závorková, M., Procházková, L.: Léčba diabetického makulárního edému mikropulzním laserem – první zkušenosti. Ces Slov Oftalmol; 2015 : 71(5):223-228.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2018 Číslo 2- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Možnosti využití přípravku Desodrop v terapii a prevenci oftalmologických onemocnění
- Selektivní laserová trabekuloplastika nesnižuje nitroční tlak více než argonová laserová trabekuloplastika
-
Všechny články tohoto čísla
- ONE-YEAR FOLLOW-UP OUTCOMES OF TREATMENT OF WET AGE-RELATED MACULAR DEGENERATION WITH AFLIBERCEPT
- The use of micropulse laser in patients with diabetic macular edema at the Department of Ophthalmology, Faculty Hospital Hradec Králové
- Results of the first 12 months treatment of macular edema complicating BRVO in patients treated with ranibizumab
- ACUTE MYOPIA WITH ELEVATION OF INTRAOCULAR TENSION AS AN ADVERSE SIDE EFFECT OF ANTIDEPRESSANT MEDICATION
- CHANGE OF CENTRAL AND PERIPHERAL VISION IN PATIENT WITH SYMPTOMATIC CYST OF RATHKE'S CLEFT FOLLOWING TRANSSPHENOIDAL RESECTION.
- Patnáct let Lionského oftalmologického edukačního centra oční kliniky Fakultní nemocnice Královské Vinohrady v Praze
- 19. Vejdovského olomoucký vědecký den
- Zemřela Jaroslava Vladyková
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- CHANGE OF CENTRAL AND PERIPHERAL VISION IN PATIENT WITH SYMPTOMATIC CYST OF RATHKE'S CLEFT FOLLOWING TRANSSPHENOIDAL RESECTION.
- The use of micropulse laser in patients with diabetic macular edema at the Department of Ophthalmology, Faculty Hospital Hradec Králové
- Results of the first 12 months treatment of macular edema complicating BRVO in patients treated with ranibizumab
- ACUTE MYOPIA WITH ELEVATION OF INTRAOCULAR TENSION AS AN ADVERSE SIDE EFFECT OF ANTIDEPRESSANT MEDICATION
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



