-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
An autopsy case of heatstroke under the influence of psychotropic drugs
Případ úpalu pod vlivem psychotropních látek
V článku prezentujeme fatální případ úpalu po požití olanzapinu a levomepromazinu. V polovině srpna byl ve své skladištní místnosti v Japonsku nalezen muž bez známek života. V době ohledání, přibližně sedm hodin po jeho smrti, měl rektální teplotu 40,1°C. Teplota okolního prostředí byla 30,2°C, nejvyšší teplota v místnosti v průběhu dne dosahovala 36°C. Histopatologické nálezy prokázaly hyperkontrahovaná vlákna v kosterních svalech. Kvantitativní toxikologická analýza pomocí tandemové hmotnostní spektrometrie s kapalinovou chromatografií (LC-MS/MS) odhalila koncentrace olanzapinu, levomepromazinu, 7-aminonitrazepamu (metabolit nitrazepamu) a 7-aminoflunitrazepamu (metabolit flunitrazepamu) ve vzorku femorální krve 0,433 µg/ml, 0,177 ug/ml, 0,604 ug/ml, respektive 0,041 ug / ml. Ze vzorku post mortem odebrané krve nebyly detekovány žádné další léky ani ethanol. Koncentrace myoglobinu v moči byla 3000 ng/ml. Koncentrace olanzapinu překročila toxické hladiny; hladina levomepromazinu však byla v terapeutickém rozmezí. Protože jak olanzapin, tak levomepromazin působí blokováním muskarinových receptorů, mohou potlačit pocení a narušit odvod tepla. Na základě makroskopických pitevních nálezů, histologických nálezů svědčících o rozpadu svalů, výsledcích toxikologických vyšetření a vyšetřování úřadů jsme dospěli k závěru, že příčinou úmrtí byl úpal způsobený olanzapinem a levomepromazinem.
Klíčová slova:
olanzapine – levomepromazine – úpal
Authors: Kinoshita Hiroshi 1; Tanaka Naoko 1; Kumihashi Mitsuru 2; Jamal Mostofa 1; Ito Asuka 1; Nagata Ken 1; Tsutsui Kunihiko 3; Kimura Shoji 1
Authors place of work: Department of Forensic Medicine, Faculty of Medicine, Kagawa University, Kagawa, Japan 1; Forensic Science Laboratory, Kagawa Prefectural Police Headquarters, Kagawa, Japan 2; Health Sciences, Faculty of Medicine, Kagawa University, Kagawa, Japan 3
Published in the journal: Soud Lék., 65, 2020, No. 4, p. 76-78
Category: Original article
Summary
We present here a fatal case of heatstroke, involving olanzapine and levomepromazine medications. A male in his sixties was found dead in his storage room in the middle of August, with a high rectal temperature. Autopsy revealed congestion of the lungs without any specific findings. Quantitative toxicological analysis demonstrated concentrations of olanzapine, levomepromazine, 7-aminonitrazepam, and 7-aminoflunitrazepam in a femoral blood sample of 0.433 µg/mL, 0.177 µg/mL, 0.604 µg/mL, and 0.041 µg/mL, respectively. The concentration of olanzapine exceeded toxic levels; however, levomepromazine level was within the therapeutic range. Due to the blocking mechanism of both olanzapine and levomepromazine against muscarinic receptors, they might depress sweating and impair heat dissipation. Based on autopsy findings, results of toxicological examination, and investigation by the authorities, we concluded that the cause of death was heatstroke under the influence of olanzapine and levomepromazine.
Keywords:
olanzapine – levomepromazine – heatstroke
Olanzapine is an atypical antipsychotic drug with both dopamine D2 and serotonin 5-HT2 receptor antagonistic actions (1-3) as well as muscarinic receptor-blocking properties (2,3). Levomepromazine (methotrimeprazine) is phenothiazine derivative, a first-generation antipsychotics, used in the treatment of psychosis (4,5). It also has a pronounced sedative effect (4). Moreover, both olanzapine and levomepromazine have anticholinergic effects. These pharmacological actions presenting as dryness of the mouth and depression of sweating (5-7). In this study, we report a case of fatal heatstroke under the influence of olanzapine and levomepromazine.
CASE REPORT
A Japanese man in his sixties (height, 178 cm; weight, 79 kg) was found dead in his storage room in the middle of August. The ambient temperature was 30.2 °C, when he was found. And the maximum air temperature of that day was 36 °C, at daytime. He had been receiving therapy for schizophrenia and prescribed olanzapine, levomepromazine, nitrazepam, and flunitrazepam. His rectal temperature was 40.1 °C at the time of police inspection, which was approximately seven hours after his death. The medicolegal autopsy revealed a slight contusion on his head. However, these were not considered contributory to the cause of death.
His heart weighed 465 g and contained 40 mL of blood without coagulum. The brain weighed 1255 g and with no injuries observed. The left and right lungs weighed 477 g and 515 g, respectively, and were moderately congested. The stomach contained 40 mL of brownish liquid. Signs other than congestion were not evident in other organs. Histopathological findings revealed hypercontracted fibers in skeletal muscles, appearing as “opaque fibers” (Figure. 1). Furthermore, internal examination revealed no diseases. A drug screening test using an Instant-view TM panel (ALFA Scientific Designs, Poway, CA) yielded negative results. The myoglobin concentration in the urine was 3000 ng/ml (normal postmortem urinary myoglobin level, <50 ng/ml (8)). Postmortem blood samples were obtained for toxicological investigation.
Fig. 1. Hypercontracted fi ber in the skeletal muscle. (diaphragm, hematoxylin and eosin staining, objective lens ; 10). 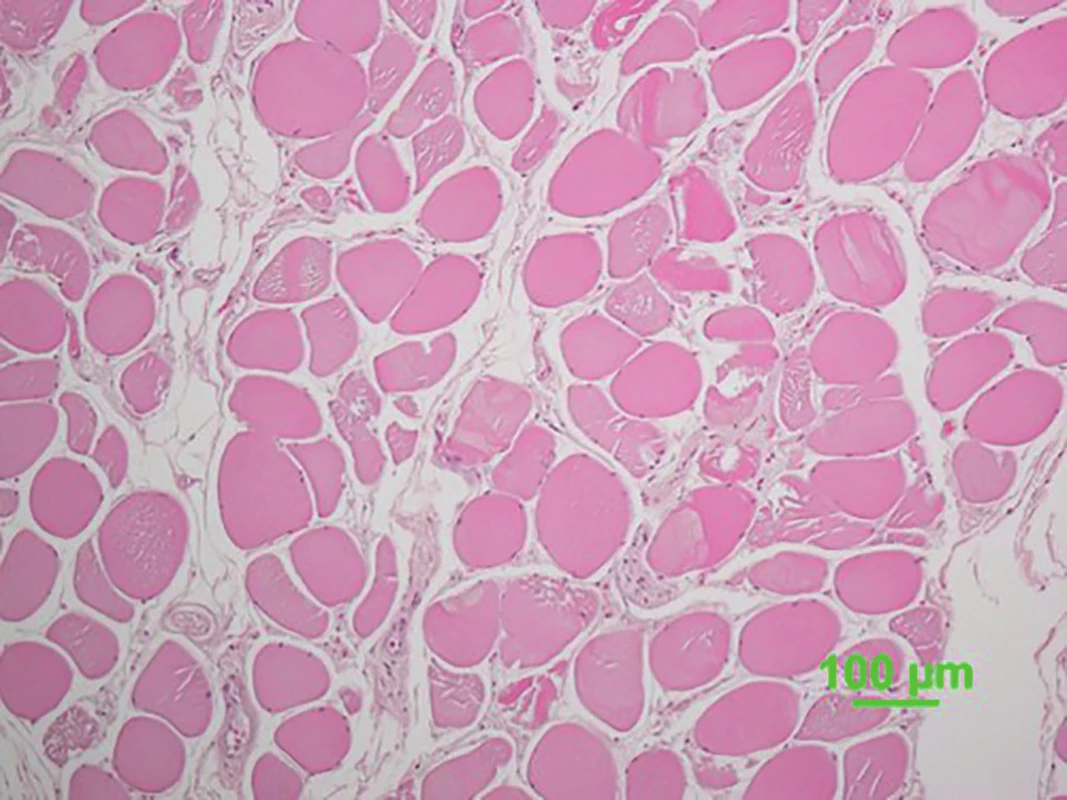
Toxicological analysis using liquid chromatography tandem mass spectrometry (LC-MS/MS) was performed as previously described (9). In brief, the liquid chromatography separations were carried out using EkspertTM UltraLC 100-XL (Eksigent part of Sciex, Framingham, MA, USA). An L-column2 ODS (1.5 mm × 150 mm, 5.0 µm particle size, Chemicals Evaluation and Research Institutes, Tokyo, Japan) was used with the mobile phase consisting of solvent A (5% methanol containing 10 mM ammonium formate) and solvent B (95% methanol containing 10 mM ammonium formate) with a flow rate of 0.1 mL/min. The mass spectra was obtained by a QTrap® 4500 tandem mass spectrometer (Sciex, Framingham, MA, USA). Quantitation of ethanol was performed using headspace gas chromatography.
RESULTS AND DISCUSSION
Since the morphological findings of heatstroke are usually non-specific such as the congestion of the lungs and brain edema, forensic diagnosis of heatstroke is usually based on an exclusion of other causes of death (10). In the present case, disease and trauma were excluded by the autopsy findings. The histological findings of “opaque fibers” in skeletal muscles and extremely high concentration of urinary myoglobin were attributed to muscle breakdown due to high temperature (11).
Olanzapine, levomepromazine, 7-aminonitrazepam, and 7-aminoflunitrazepam were quantitated by the toxicological examination. Table 1 shows concentrations of these substances, along with the lethal, toxic and therapeutic ranges (12-14). No other drugs or ethanol were detected.
Tab. 1. Concentration of each drug and metabolites in the postmortem blood sample and their lethal, toxic, and therapeutic ranges (μg/ml). 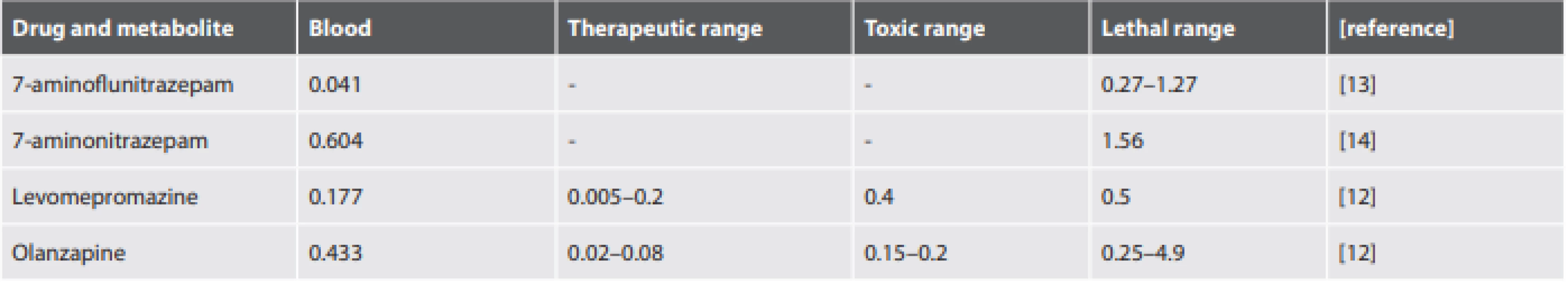
The 7-aminonitrazepam and 7-aminoflunitrazepam are metabolites of nitrazepam and flunitrazepam, respectively. However, we could not detect both nitrazepam and flunitrazepam in the present case. Since nitrazepam and flunitrazepam are converted to 7-amino metabolites after death (15), the pharmacological properties of these drugs were evaluated as the sum of the concentration of each parent drug and its metabolites. In the present case, as postmortem blood concentrations of 7-aminonitrazepam and 7-aminoflunitrazepam were below lethal range (13,14), both these drugs were not likely to have significantly contributed to his death.
The diagnosis of fatal heatstroke is based not only on autopsy findings, but also with the consideration of the circumstances of the victim (10). Drugs, such as anticholinergics and phenothiazines, are predisposing factors for heatstroke (16). It has been reported that patients with schizophrenia have higher risk for heat-related illness (17). First-generation antipsychotics, such as levomepromazine and chlorpromazine, are risk factors of heatstroke (17,18), and second-generation antipsychotic olanzapine is also implicated to drug-induced fever in the absence of neuroleptic malignant syndrome (19). Since the present case occurred in the middle of summer, the pharmacological effect of antipsychotic drugs with anticholinergic properties that he was receiving might have potentiated heat accumulation and impairment of heat dissipation.
Blood levels of olanzapine was over the therapeutic range (0.433 µg/ml). Olanzapine has a potent antagonistic action to dopamine D2 receptor (2,3), and it may impair thermoregulation and decrease heat tolerance (18,20). As both olanzapine and levomepromazine have an anticholinergic property within the range of clinical dose (7), pharmacological actions via muscarinic receptor may decrease sweating and cause impairment of heat dissipation (18,20). Although the concentration of levomepromazine is within the therapeutic range, it has a pronounced sedative effect (4). This would have decreased his ability to move away from the hot environment.
Based on the macroscopic autopsy findings, histological findings suggestive of muscle breakdown, results of toxicological examination, and investigation by the authorities, we concluded that the cause of death was heatstroke under the influence of antipsychotic drugs. Our case highlighted the fact that we need to consider the effects of prescribed drugs for forensic diagnosis.
CONFLICTS OF INTEREST
The authors declare that there is no conflict of interest with regard to the publication of this paper.
ACKNOWLEDGEMENTS
The authors would like to thank Enago (www.enago.jp) for the English language review.
∗ Correspondence address:
Hiroshi Kinoshita
Department of Forensic Medicine, Faculty of Medicine, Kagawa University,
1750-1, Miki, Kita, Kagawa 761-0793, Japan
tel.: +81-87-891-2140
fax: +81-87-891-2141
e-mail: kinochin@med.kagawa-u.ac.jp
Received: June 6, 2020
Accepted: July 14, 2020
Zdroje
Baselt RC. Olanzapine. In: Disposition of toxicdrugs and chemicals in man (8th ed). Foster City: Biomedical Publications; 2008 : 1140-1143.
Richelson ER. Receptor pharmacology of neuroleptics: relation to clinical effects. J Clin Psychiatry 1999; 60 (supple 10): 5-14.
Baldessarini RJ, Tarazi FI. Pharmacotherapy of psychosis and mania. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman & Gilman’s The pharmacological basis of therapeutics (11th ed). New York, Chicago: McGraw-Hill; 2006 : 461-500.
Baselt RC. Methotrimeprazine. In: Disposition of toxic drugs and chemicals in man (8th ed). Foster City: Biomedical Publications; 2008 : 971-973.
Muench J, Hamer AM. Adverse effects of antipsychotic medications. Am Fam Physician 2010; 81 : 617-622.
Brown JH, Taylor P. Muscarinic receptor agonist and antagonist. In: Brunton LL, Lazo JS, Parker KL, eds. Goodman & Gilman’s The pharmacological basis of therapeutics (11th ed). New York, Chicago: McGraw-Hill; 2006 : 183-200.
Obara K, Horiguchi S, Shimada T, et al. Characterization of binding of antipsychotics to muscarinic receptors using mouse cerebral cortex. J Pharmacol Sci 2019; 140 : 197-200.
Zhu BL, Ishida K, Quan L, et al. Post-mortem urinary myoglobin levels with reference to the causes of death. Forensic Sci Int 2001; 115 : 183-188.
Kinoshita H, Tanaka N, Takakura A, et al. Flunitrazepam in stomach contents may be a good indicator of its massive ingestion. Rom J Legal Med 2017; 25 : 193-195.
Madea B. Injuries due to heat. In: Handbook of forensic medicine. Madea B, ed. West Sussex: Wiley Blackwell; 2014 : 451-467.
Kinoshita H, Kubota A, Nishiguchi M, et al. Three autopsy cases of heat illness. Res Pract Forens Med 2005; 48 : 173-177.
Schulz M, Iwersen-Bergmann S, Andresen H, Schmoldt A. Therapeutic and toxic blood concentrations of nearly 1000 drugs and other xenobiotics. Crit Care 2012; 16: R136.
Kinoshita H, Tanaka N, Takakura A, et al. Medicologal implications of an autopsy case of hypothermia under the influence of flunitrazepam and quetiapine. Rom J Legal Med 2018; 26 : 67-69.
Moriya F, Hashimoto Y. Tissue distribution of nitrazepam and 7-aminonitrazepam in a case of nitrazepam intoxication. Forensic Sci Int 2003; 28 : 108-112.
Drummer OH, Odell M. Monographs of selected drugs. Benzodiazepine. In: The forensic pharmacology of drugs of abuse. London: Arnold; 2001 : 382-405.
Grogan H, Hopkins PM. Heat stroke: implications for critical care and anesthesia. Br J Anesth 2002; 88 : 700-707.
- Bark N. Deaths of psychiatric patients during heat waves. Psychiatr Serv 1998; 49 : 1088-1090.
- Lee C-P, Chen P-J, Chang C-M. Heat stroke during treatment with olanzapine, trihexyphenidyl and trazodone in a patient with schizophrenia. Acta Neuropsychiatr 2015; 27 : 380-385.
- Yang C-H, Chen Y-Y. A case of olanzapine-induced fever. Psychopharmacol Bull 2017; 47 : 45-47.
- Bhanushali M, Tuite P. The evaluation and management of patients with neuroleptic malignant syndrome. Neurol Clin 2004; 22 : 389-411.
Štítky
Patologie Soudní lékařství Toxikologie
Článek vyšel v časopiseSoudní lékařství

2020 Číslo 4
Nejčtenější v tomto čísle- Autoerotic deaths: report of two unusual cases
- An autopsy case of heatstroke under the influence of psychotropic drugs
- The reasons for reoperations after surgery for acute subdural hematoma and the implications of suspected injury mechanisms
- MUDr. Jaromír Hrubecký osmdesátiletý
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



