-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Fractures of the surgical neck of the scapula with separation of the coracoid base
Zlomeniny chirurgického krčku lopatky spojené s odlomením baze korakoideu
Zlomeniny krčku lopatky kombinované se zlomeninou korakoideu představují vzácný a specifický typ poranění. Dislokované případy patří mezi komplikované, plně nestabilní typy zlomenin chirurgického krčku lopatky a vyžadují přesnou CT diagnostiku a stabilní osteosyntézu krčku lopatky prováděnou z Judetova přístupu. Cílem této studie je popis našich 4 případů a dalších 3 kazuistik popsaných v odborné literatuře.
Klíčová slova:
lopatka – zlomeniny lopatky – korakoid – krček lopatky – Judetův přístup
Authors: M. Tucek 1; T. Strnad 1; P. Obruba 2; J. Bartonicek 1
Authors place of work: Department of Orthopaedics, 1st Faculty of Medicine, Charles University and Military University Hospital Prague 1; Department of Trauma of Masaryk Hospital, Jan Evengelista Purkyně University, Ústí nad Labem 2
Published in the journal: Rozhl. Chir., 2020, roč. 99, č. 8, s. 368-372.
Category: Kazuistika
doi: https://doi.org/10.33699/PIS.2020.99.8.368–372Summary
Fractures of the surgical neck of the scapula combined with a fracture of the coracoid base constitute a specific and rare type of a fracture pattern. When displaced, they present a severe, completely unstable type of surgical neck fracture, requiring a precise CT diagnosis, open reduction and stable internal fixation of the fracture via the Judet approach. The aim of this study is to describe our four cases and discuss three others reported to date.
Keywords:
scapular fractures – scapula – coracoid process – scapular neck – Judet approach
Introduction
Fractures of the surgical neck of the scapula (SN fractures) are widely debated in the literature, primarily in connection with so-called floating shoulder [1–4]. SN fractures are classified, according to the integrity of the coracoclavicular and coracoacromial ligaments, as stable, rotationally unstable, or completely unstable [2]. A special and rare type of a completely unstable injury is a fracture of the surgical neck combined with a fracture of the coracoid base (SN+C fractures).
Probably the oldest report of a fracture of the surgical neck and the coracoid was published by Badouin [5] in 1909. It was a scapula of a man found in the Neolithic grave.
This type of fracture was described in the orthopedic literature for the first time by Goss [6] in 1996, although only in general. The first to detail a particular case on the basis of 3D CT reconstructions were Limb and Mc Murray in 2005 [7]. Another two cases were mentioned by Bartoníček [2] in 2014, but only marginally. The rare incidence and the minimal number of recorded cases is the reason why this fracture pattern has often been neglected and the standard of its treatment has not yet been established.
The aim of our study is to detail our four cases and analyze the cases found in the literature.
Case reports
The authors of this study treated a total of four cases of SN+C fractures between 2002 and 2018. The first two cases have already been written about in 2014 [2].
Case report 1
A 26-year-old woman sustained fractures of the pelvis and the left scapula, as a result of a parachuting accident. After initial management and stabilization in a regional hospital, she was referred to our department for definitive treatment. In view of only minimal displacement, the pelvic fracture was treated nonoperatively. CT scans of the scapula and 3D reconstructions confirmed a displaced fracture of the surgical neck of the left scapula and separation of the coracoid base. The glenoid fragment was displaced distally and into valgus and the glenopolar angle (GPA) was 66 degrees. The patient was operated on 14 days after the injury, via a Judet approach, with full mobilization of the infraspinatus. Entrapment of the suprascapular nerve in the fracture line was detected intraoperatively. The nerve was released and the fracture fixed with two 3.5mm plates. The coracoid fracture was left unfixed. The surgical wound healed without complications. The postoperative radiograph showed close contact between the coracoid base and the superior surface of the scapular neck. Passive motion exercises, with the use of CPM, were started on the second postoperative day, active motion exercises from six weeks postoperatively. At one-year follow-up, the patient reported no subjective symptoms and had a full range of motion in the shoulder joint, although atrophy of the infraspinatus due to suprascapular nerve lession was observed. The radiograph showed healing in an anatomical position, including union of the coracoid (Fig. 1). In the follow-up telephone interview, 10 years after the injury, no changes were reported by the patient.
Fig. 1. A – preoperative radiograph; B – preoperative 3D CT reconstruction; C – radiograph one year after the surgery 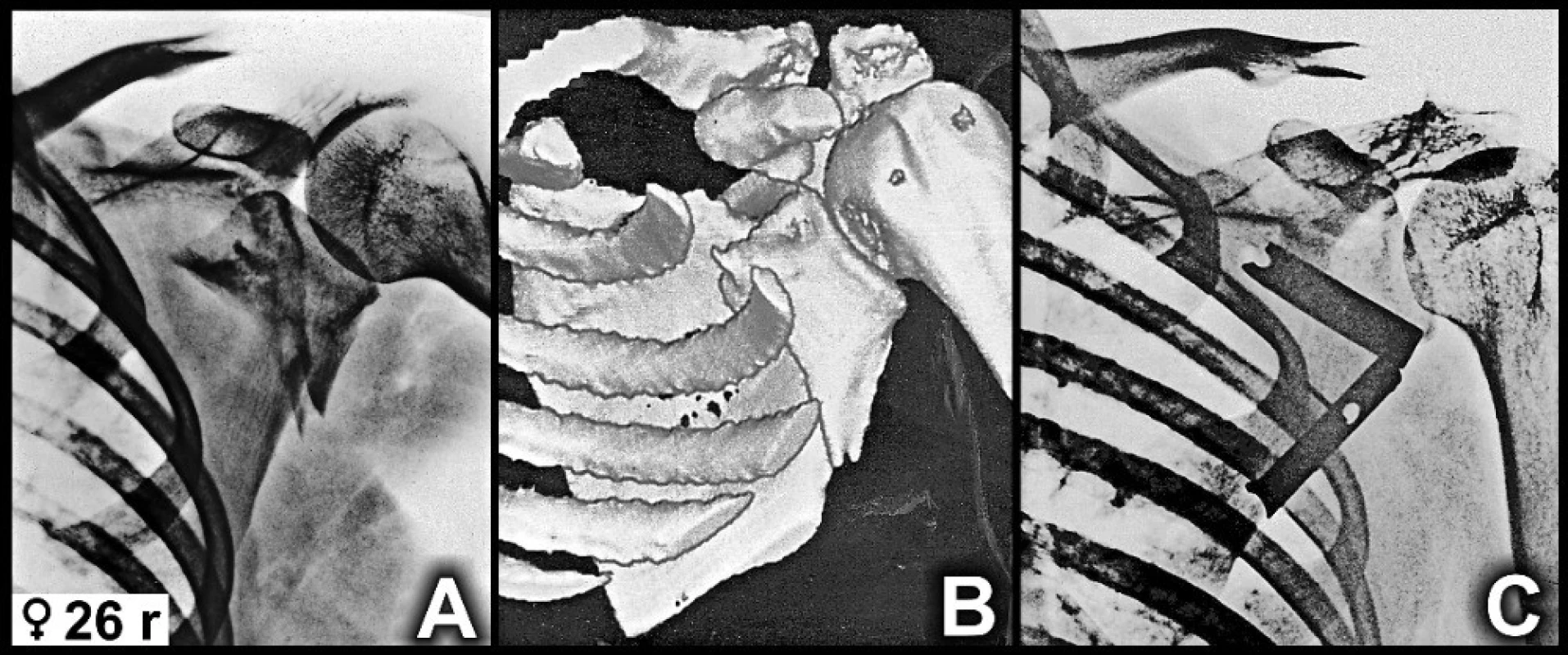
Case report 2
A 34-year-old man sustained an isolated fracture of the scapula after falling from a bicycle. The radiograph and the CT scans, including 3D CT reconstructions, revealed a complete undisplaced SN fracture and a minimally displaced fracture of the coracoid base, extending as far as the superior border of the scapular body (Fig. 2). The GPA was 40 degrees. The fracture was treated nonoperatively by immobilization for four weeks, followed by passive exercises and by active rehabilitation after another two weeks. Normal function of the shoulder joint was restored within three months. Follow-up at two years after the injury showed radiographic union of the fractures and full function of the shoulder joint, without limitation of activity.
Fig. 2. A+B – 3D CT reconstructions, anterior and lateral views. The 3D CT reconstruction showed the fracture line only partially, while it was well seen on 2D CT reconstructions 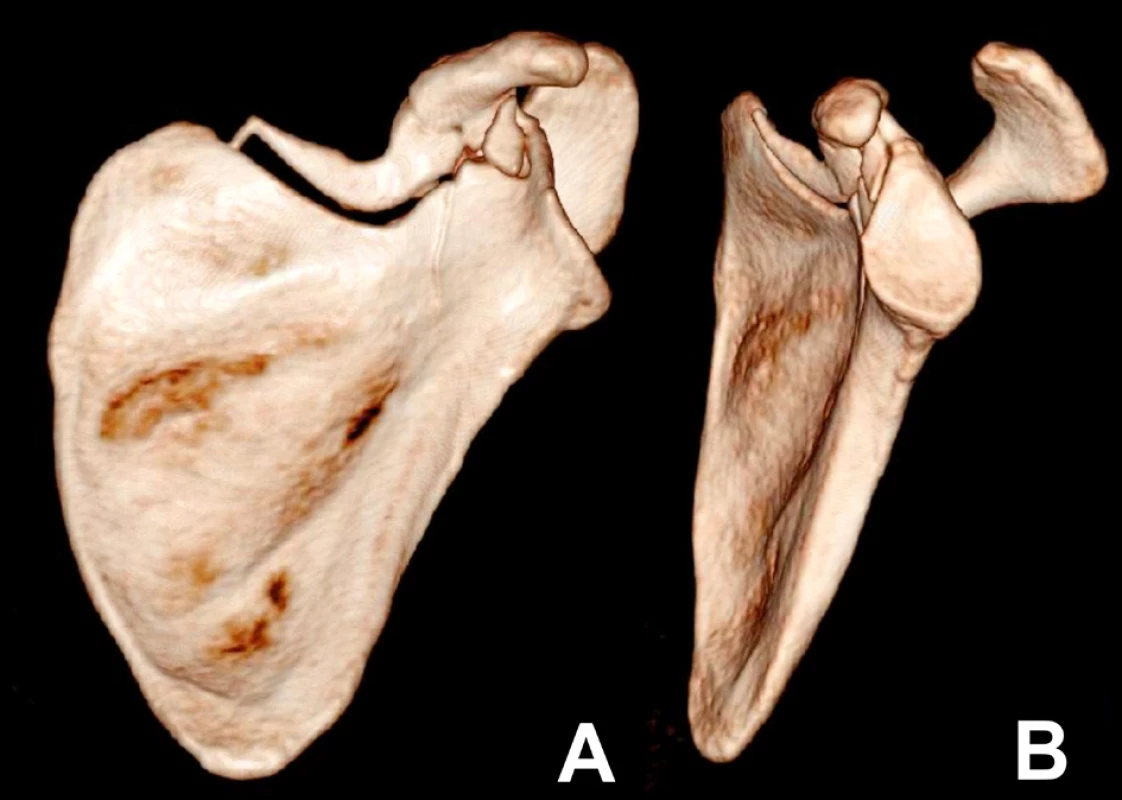
Case report 3
A 24-year-old man sustained a scapular fracture and splenic rupture after falling from a motorcycle. After urgent splenectomy, the patient was referred to our department on the 11th day after the injury. Radiographs and subsequent 3D CT reconstructions showed displaced SN+C fractures. The GPA was 50 degrees. Operation was performed on the 13th day post injury, via a Judet approach, with partial mobilization of the infraspinatus. The fracture was reduced and stabilized using four 2.7mm T - and L-plates. The surgical wound healed uneventfully. Passive motion exercises using CPM were started on the second postoperative day, active motion exercises six weeks postoperatively. At one-year follow-up the patient reported no subjective symptoms and had a full range of motion in the shoulder joint, without atrophy of the infraspinatus. Radiograph demonstrated healing of both the SN and the coracoid fractures in an anatomical position (Fig. 3).
Fig. 3. A – preoperative radiograph; B+C – 3D CT reconstructions, anterior and lateral views; D – radiograph one year after surgery 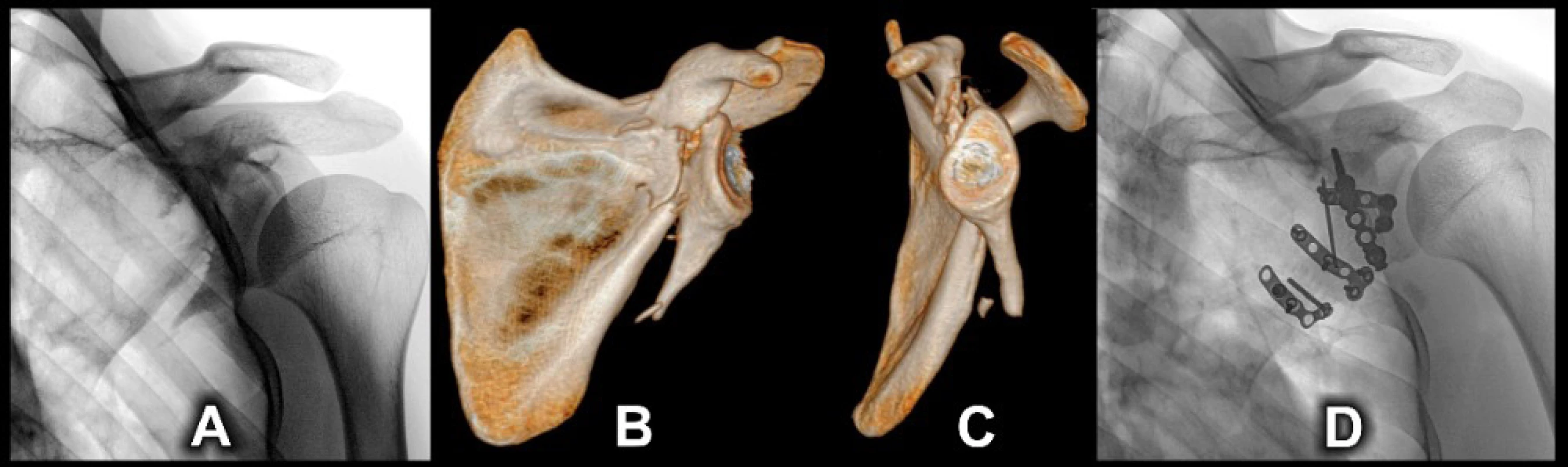
Case report 4
A 44-year-old man sustained an injury to the left shoulder joint and a mild lung contusion after falling four meters from a ladder whilst under the influence of alcohol. Radiography showed a displaced fracture of the surgical neck of the scapula and a slightly displaced fracture of the coracoid base (Fig. 4). The GPA was 52 degrees. The patient refused CT examination, accepted only immobilization of the shoulder joint in a brace and never attended follow-up evaluation.
Fig. 4. A+B postinjury radiographs 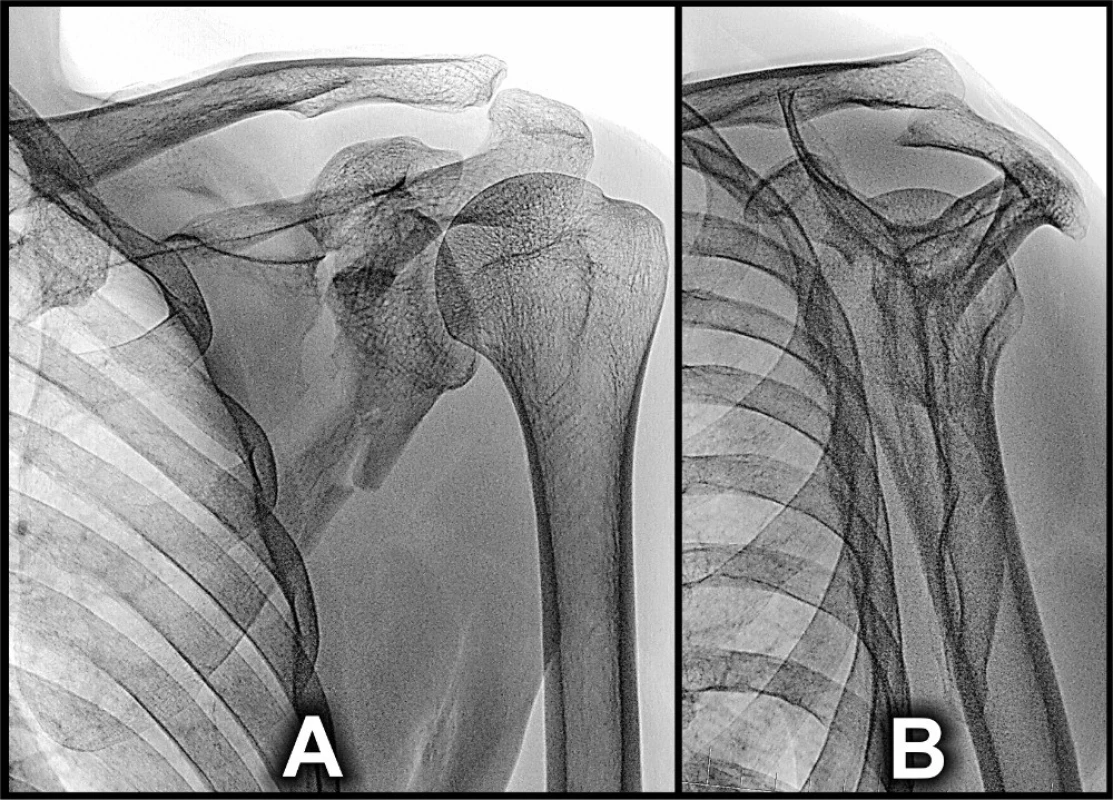
Discussion
In addition to the case reported by Limb and Mc Murray [7], we have found only two other cases that could be interpreted as SN+C fractures in current literature [8–9].
Wyrch et al. [9] described in 1995 a somewhat questionable case of scapular neck fracture diagnosed solely by radiographs and MRI. Unfortunately, the fracture pattern could not be reliably verified. Its detailed pathoanatomy was assessed in the absence of 3D CT reconstruction, which we consider to be an essential part of assessment that should be performed in all suspected SN fractures.
Another case was reported by Ogawa et al. [8] in 2018, who classified it as a fracture of the anatomical neck of the scapula, but 3D CT reconstructions showed also a fracture of the coracoid and the lateral part of the scapular spine. Correctness of interpretation of these fractures is questionable.
In 2014, Bartoníček et al. [2] briefly mentioned two cases in their series of 17 fractures of the scapular neck, both detailed in this study (cases 1 and 2).
The small number of cases of SN+C fractures may be explained by the fact that, although extensively debated in the literature, surgical neck fractures are quite infrequent and account for approximately 3% of all scapular fractures [10]. Noticeably, a fracture with an associated separation of the coracoid base is one of the four variants of this injury [11].
In terms of displacement, SN+C fractures occurred in two forms. A complete but undisplaced fracture was recorded only by us (case 2). The remaining three fractures and the fracture described by Limb and Mc Murray [7] were displaced. Radiographs and 3D CT reconstructions showed a typical displacement pattern.
The glenoid fragment is displaced distally and into valgus. This can be well-seen in our first case (Fig. 1) and the case reported by Limb and Mc Murray [7], both documented by similar 3D CT reconstructions. Part of the displacement is also rotation of the superior pole of the glenoid anteriorly and of the inferior part of the fragment posteriorly, as demonstrated in our case 3 (Fig. 3). A marked valgus displacement of the glenoid fragment (our case 1 and the case described by Limb and Murray) showed a wide gap between the coracoid base and the glenoid fragment.
The type of displacement was reflected also in the values of the glenopolar angle (GPA). The standard GPA value ranges from 35 to 51 degrees [12]. In displaced fractures of the scapular body and neck, the GPA value decreases, with only two exceptions, i.e. in displaced fractures of the anatomical neck of the scapula and SN+C fractures (Fig. 5). In our three displaced cases, the GPA value increased up to 68 degrees (Table 1) and it was also increased in the case reported by Limb and Mc Murray [7].
Tab. 1. Overview of all cases 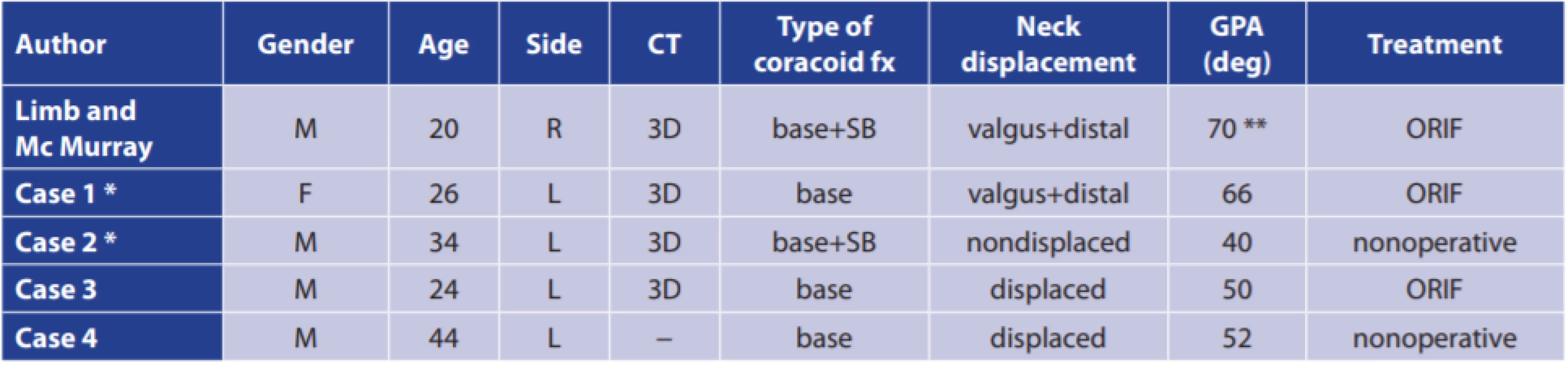
Legend: M − male, F − female, R − right, L − left, SB − superior border of scapular body, ORIF − open reduction, internal fixation, * − a case mentioned briefly before, **− measured by authors using CT scans presented in the publications. Fig. 5. Comparison of the degree of displacement of the glenoid fragment, showing an increasing valgosity and widening of a gap between the coracoid and the glenoid fragment. A – case 2; B – case 3; C – case 4, D – case 1 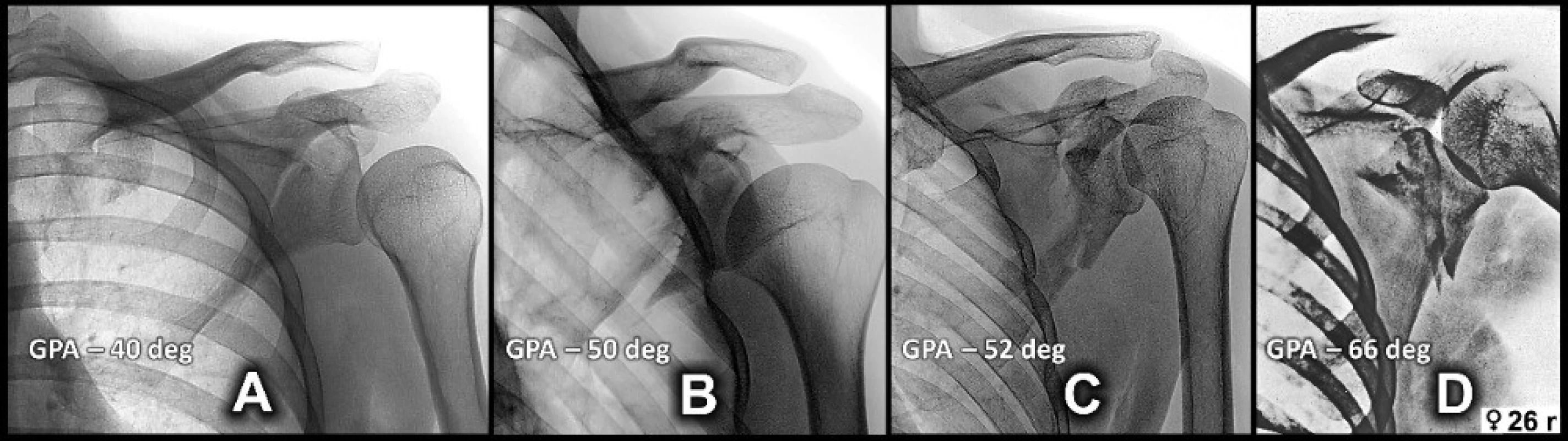
This type of displacement is quite different from a totally unstable fracture of the surgical neck with rupture of the coracoacromial and coracoclavicular ligaments [9,10,13], where the coracoid is part of the glenoid fragment and the coracoid muscles pull the glenoid fragment distomedially and at the same time rotate it anteriorly (Fig. 6).
Fig. 6. Typical displacement of a totally unstable (rupture of coracoacromial and coracoclavicular ligaments) fracture of surgical neck 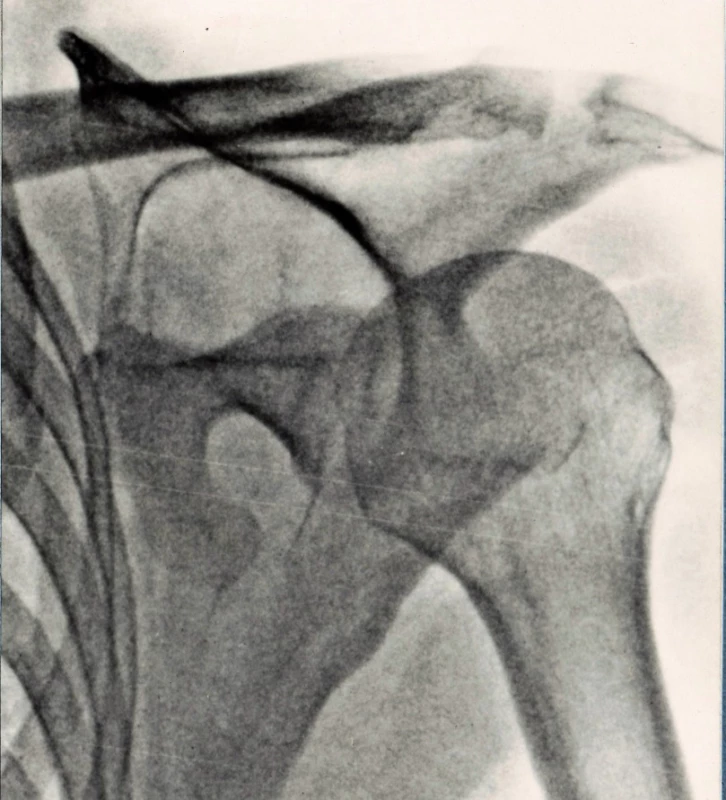
A displaced SN fracture with separation of the coracoid base is one of the variants of the floating shoulder [14], due to the total loss of the osseoligamentous connection between the glenoid fragment and both the scapular body and the axial skeleton [3]. The same applies to a displaced fracture of the anatomical neck which behaves identically [2,14].
A displaced SN+Co fracture requires operative treatment. We prefer the Judet approach, allowing a safe exposure of fracture site and revision of the fracture line in the spinoglenoid notch, as entrapment of the suprascapular nerve has been described in several fractures of the surgical neck [15–17]. Limb and Mc Murray [7] used the lateral approach in the interval between the infraspinatus and the teres minor. In our view, this approach does not always provide an adequate exposure and its extension is difficult. The fracture is not easy to reduce because the fracture line is long and the contact surface between the two fragments is only several millimeters broad, and thereby unstable. It is beneficial to insert a longer screw into the glenoid fragment to use as a joy-stick [2,7]. We preferably use two plates for internal fixation, as one plate on the lateral pillar does not always guarantee sufficient stability.
Fixation of the coracoid is not necessary [2,6]. After reduction of two cases treated operatively, close contact between the coracoid base and the superior surface of the glenoid fragment was restored and this fracture healed. A similar case was recorded by Limb et al. All three operatively treated cases, i.e. our two cases and that of Limb and Mc Murray [7] healed completely without complications and with exceptional functional results.
Conclusion
Fractures of the surgical neck of the scapula with separation of the coracoid base are rare, but when displaced, they represent a severe scapular fracture pattern. Precise diagnosis requires CT examination, including 3D CT reconstructions. The typical feature is displacement of the glenoid fragment distally and into valgus, and increase of the GPA value. The method of choice for treatment of displaced fractures is open reduction and stable internal fixation via the Judet approach.
Ethical approval: “All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
Informed consent: Informed consent was obtained from all individual participants included in our scapular research.
Acknowledgments: The authors wish to thank Chris Colton Prof MD FRCS and Ludmila Bébarová PhD for their assistance in the editing of the manuscript.
Supported by IP DZRVO MO1012.
Conflict of interests
The authors declare that they have no conflict of interest in connection with this paper and that the article has not been published in any other journal, except congress abstracts and clinical guidelines.
Michal Tuček MD PhD
Department of Orthopaedics,
1st Faculty of Medicine,
Charles University and Military University Hospital Prague
U Vojenské nemocnice 1200
169 02 Prague 6
e-mail: tucekmic@gmail.com
Zdroje
- Bartoníček J, Cronier P. History of the treatment of scapular fractures. Arch Orthop Trauma Surg. 2010;130 : 83–92. doi: 10.1007/s00402-009-0884-y.
- Bartoníček J, Tuček M, Frič V, et al. Fractures of the scapular neck: diagnosis, classification and treatment. Int Orthop. 2014;38 : 2163–2173. doi: 10.1007/s00264-014-2434-7.
- Bartoníček J, Tuček M, Naňka O. Floating shoulder – myths or reality? J Bone Joint Surg Rew. 2018;6:e5(1–10). doi: 10.2106/JBJS.RVW.17.00198.
- Goss TP. Scapula fractures and dislocations: Diagnosis and treatment. J Am Acad Orthop Surg. 1995;3 : 22–33.
- Baudouin M. Un cas de fracture du col chirurgical de l’omoplate d’origine préhistorique. Arch Provinc Chir. 1909;16 : 575–583.
- Goss TP. The scapula: coracoid, acromial and avulsion fractures. Am J Orthop. 1996;25 : 106–115.
- Limb D, Mc Murray D. Dislocation of the glenoid fossa. J Shoulder Elbow Surg. 2005;14 : 338–339.
- Ogawa K, Inokuchi W, Matsumura N. Delayed surgery for displaced fracture of the anatomic neck and spine of the scapula: a case report and literature review. JSES Open Access. 2018;14 : 169–173. doi: 10.1016/j.jses.2018.06.001.
- Wyrsch RB, Soindler KP, Stricker PR. Scapular fracture in professional boxer. J Shoulder Elbow Surg. 1995;4 : 395–398.
- Bartoníček J. Scapular fractures. In: Tornetta P, Ricci WM, Ostrum RF, et al. McQueen M, Court-Brown CH, eds. Rockwood and Green´s Fractures in Adults. 9th edition. Philadelphia, PA: Wolters Kluwer 2020 : 976–1008.
- Magerl F. Osteosynthesen im Bereich der Schulter. Helv Chir Acta. 1974;41 : 225–232.
- Tuček M, Naňka O, Malík J, et al. The scapular glenopolar angle: standard values and side differences. Skeletal Radiol. 2014;43 : 1583–1587. doi: 10.1007/s00256-014-1977-4.
- Goss TP. Fractures of glenoid neck. J Shoulder Elbow Surg. 1994;3 : 42–52.
- Arts V, Louette L. Scapular neck fractures; an update of the concept of floating shoulder. Injury. 1999;30 : 146–148.
- Boerger TO, Limb D. Suprascapular nerve injury at the spinoglenoid notch after glenoid neck fracture. J Shoulder Elbow Surg. 2000;9 : 236–237.
- Edeland HG, Zachrisson BE. Fracture of the scapular notch associated with lesion of the suprascapular nerve. Acta Orthop Scand. 1975;46 : 758–763.
- Solheim LF, Roaas A. Compression of the scapular nerve after fracture of the scapular notch. Acta Orthop Scand. 1978;49 : 338–340.
Štítky
Chirurgie všeobecná Ortopedie Urgentní medicína
Článek vyšel v časopiseRozhledy v chirurgii
Nejčtenější tento týden
2020 Číslo 8- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Hojení análních fisur urychlí čípky a gel
- Stillova choroba: vzácné a závažné systémové onemocnění
-
Všechny články tohoto čísla
- Covid-19: fakta a mýty
- Thyroid tumors at the limit of operability
- Surgical treatment of fractures of the distal radius – ORIF vs external fixation with ligamentotaxis
- Pilonidal sinus disease: Karydakis flap procedure in our patients
- How to proceed with a patent popliteal artery aneurysm below the chronic superficial femoral artery occlusion?
- Secondary appendicitis in an adult patient with an ascended testicle – case report
- EUS-guided jejunoduodenostomy: another option for the management of stenosis in hepaticojejunoanastomosis
- Fractures of the surgical neck of the scapula with separation of the coracoid base
- K editorialu J. Párala: Technický rozvoj robotické chirurgie
- Rozhledy v chirurgii
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Pilonidal sinus disease: Karydakis flap procedure in our patients
- Surgical treatment of fractures of the distal radius – ORIF vs external fixation with ligamentotaxis
- Thyroid tumors at the limit of operability
- How to proceed with a patent popliteal artery aneurysm below the chronic superficial femoral artery occlusion?
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



