-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Inverted Meckel´s diverticulum: a rare cause of ileo-ileal intussusceptions and lower gastrointestinal bleeding
Invertovaný Meckelův divertikl: raritní příčina ileo-ileální invaginace a krvácení do dolní části zažívacího traktu
Invaginace je u dospělých vzácná. V naší kazuistice se věnujeme případu 28letého muže s invertovaným Meckelovým divertiklem, který se stal příčinou střevní neprůchodnosti v oblasti ilea. Pacient byl přijat do nemocnice s ileem na tenkém střevu, výraznou bolestí břicha a krvácením z konečníku. Předoperačně provedený ultrazvuk břicha odhalil nehomogenní terčovitý útvar v oblasti pravého dolního kvadrantu břicha s intraluminálním útvarem jako příčinou suspektní invaginace. Následoval akutní chirurgický zákrok, který invaginaci potvrdil, a postižený úsek tenkého střeva (cca 70 cm) byl resekován. Resekát obsahoval polypoidní útvar velikosti cca 8x3x2 cm. Histologické vyšetření odhalilo invertovaný Meckelův divertikl. V diskuzi se zabýváme problematikou Meckelova divertiklu z hlediska možností diagnostiky a terapie.
Klíčová slova:
Meckelův divertikl − invaginace − krvácení do trávicího traktu − náhlá příhoda břišní
Authors: J. Matek; J. Ptacnik; Z. Krska
Authors place of work: 1. st. Department of Surgery of Charles University Teaching Hospital in Prague
Published in the journal: Rozhl. Chir., 2018, roč. 97, č. 8, s. 399-401.
Category: Původní práce
Summary
Intussusception due to an inverted Meckel’s diverticulum in adults is rare. We present a case report of a 28-year-old man with Meckel’s diverticulum as a cause of ileo-ileal intussusceptions and lower gastrointestinal bleeding. The patient was admitted to the hospital with incomplete small bowel obstruction, abdominal pain and massive rectal bleeding. Surprisingly, pre-operative abdominal USG revealed inhomogeneous target-like mass in the right lower abdominal quadrant as intussusception with an intraluminal polypoid lesion. The patient underwent urgent laparotomy which confirmed ileo-ileal intussusception. The involved segment of small intestine (70 cm) was resected. The surgical specimen contained an elongated polypoid lesion of 8×2.5×2 cm within the ileal lumen. Histopathological examination ascertained an inverted Meckel’s diverticulum. In the discussion, we deal with diagnosis and treatment issues of Meckel’s diverticulum.
Key words:
inverted Meckel’s diverticulum − intussusceptions − gastrointestinal bleeding − acute abdomen
Introduction
Meckel’s diverticulum is the most common congenital abnormality of the gastrointestinal tract. According to autoptic studies, prevalence in the population is 2−3% (1). We deal with the remnants of incompletely closed omphaloenteric duct connecting fetal yolk sac with primitive gut during 7th and 8th week of gestation. In the early 19th century, Johan Friedrich Meckel thoroughly described and documented this structure in his works, thus the diverticulum was named after him, although it had already been described by a German surgeon Wilhelm F. Hildan in 1598 [2]. As the diverticulum contains all layers of the intestinal wall, it is a true diverticulum. Approximately 50% of diverticula contain heterotopic tissue, mostly gastric mucosa or pancreatic tissue. However, there are also reports of diverticulum containing duodenal Brunner’s glands, hepatobiliary tissue, endometrium, or combinations of the previously mentioned tissues. Usually, it is located within a 100 cm distance from the ileocaecal valve, mostly on the antimesenteric side of ileum, rarely on the mesenteric side. Most diverticula size varies from 1 to 10 cm [1,2]. Meckel’s diverticulum is usually asymptomatic, only about 2% of carriers develop complications during their lives [1,2]. In our case report, we describe an unique case of inverted Meckel’s diverticulum presenting with ileo-ileal invagination and massive intestinal bleeding.
Case report
A twenty-eight-year-old man was admitted to the 1st Department of Surgery of Charles University Teaching Hospital in Prague, due to small intestine ileus and massive rectal bleeding (enterorrhagia). For approximately one month prior to admission, the patient had a medical history of recurrent abdominal colic pain and unspecified digestive problems accompanied by nausea and episodic vomiting, diarrhea with occurrence of fresh blood in the stool, and suffered from loss of appetite. Over this period, he lost about 7 pounds (3.5 kg). On admission to hospital, he had enterorrhagia with clinical signs of commencing hypovolemic shock. Laboratory tests showed anemia (Hb 87 g/L), leukocytosis (21x109/L), elevated CRP (250 mg/L), hypoproteinemia (45 g/L) and hypokalemia (2.9 mmol/L). Plain abdominal radiograph showed numerous, up to 4 cm wide, air-fluid levels in the small intestine. Bedside sonographic examination revealed invagination of the small intestine as a possible cause of ileus and bleeding (Fig. 1). According to sonography, a stalk intraluminal structure was stated as the cause of invagination. We introduced a nasogastric tube, initiated parenteral rehydration and indicated urgent surgical intervention. After median laparotomy, we found dilatation of the ileum and jejunum corresponding to chronic incomplete ileal obstruction. The obstruction was caused by invagination located approximately 70 cm away from the Bauhin’s valve. We also found reactive mesenteric lymphadenopathy (nodules of up to 4 cm) that were not malignant macroscopically and rather corresponded with activated nodules due to bowel content infection. There was a palpable elongated elastic polypoid body within the ileal lumen. As disinvagination was impossible and we could not exclude intraluminal tumour, we decided to perform resection of the affected part of the small intestine with side-to-side anastomosis. We removed about 70 cm of the small intestine (the invaginated portion was about 25 cm long). An intraluminal polypoid structure (size 8×2.5×2 cm, Fig. 2) was identified as the main cause of invagination and, histologically, as the inverted Meckel’s diverticulum with multiple hemorrhages and gangrenes in the wall. After the surgery, we recorded a rapid normalization of blood counts and serum biochemical parameters. The patient recovered without complications and was discharged on the 9th postoperative day.
Fig. 1. Abdominal USG with a target-like mass – intussusception (transverse section, axis A= 4.2 cm, axis B=7.2 cm), hyperechogenic polypoid structure intraluminally 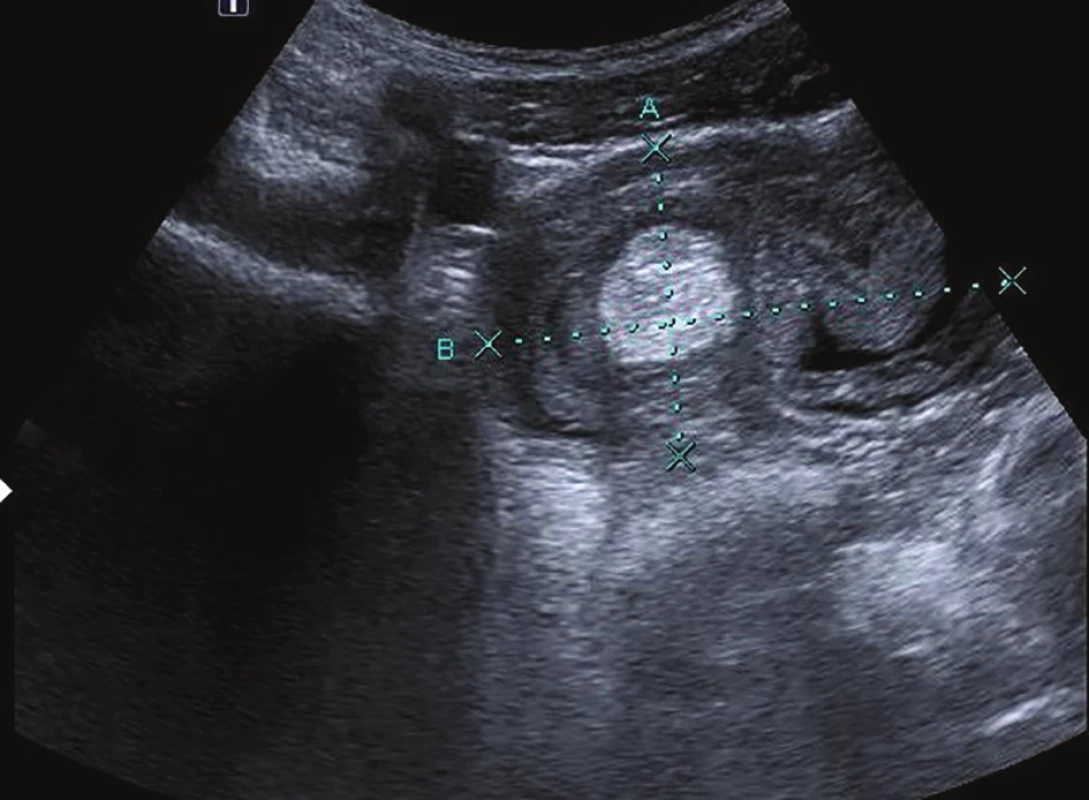
Fig. 2. Specimen of the small intestine Hemorrhagic infarcted invagination (green arrow) with inverted Meckel’s diverticulum (red arrow). 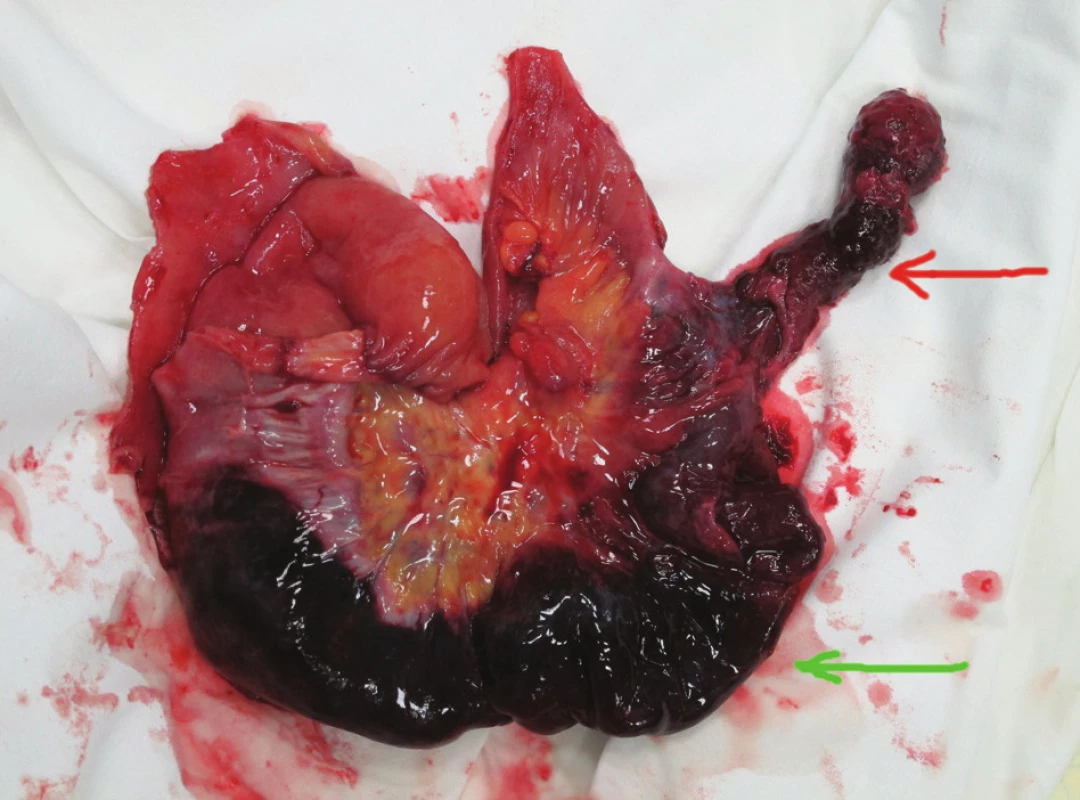
Discussion
The most common cause of intestinal obstruction in the small intestine is adhesion (up to 70%), commonly after previous surgery in the abdominal cavity. Invagination in adulthood is a rare phenomenon and represents only about 1% of small and large bowel obstructions, usually occurring on the basis of an intraluminal polypoid structure. As in our case, the intraluminal obstruction remains only partial for a relatively long time. This often causes only vague abdominal complaints, anemia and weight loss due to gradually decreasing food intake. These nonspecific manifestations explain why it is so difficult to establish the correct diagnosis preoperatively and why intussusception often goes undetected until surgery is performed. Although Meckel’s diverticulum is the most common congenital gastrointestinal anomaly, it often remains clinically silent. The largest proportion of symptomatic diverticula occurs in the first decade of life, decreasing with age significantly in the next decades. Complications in adults occur only in 2% of patients with diverticulum [1,2]. The most common complications of Meckel’s diverticulum are bleeding, intestinal obstruction, tumors, inflammation or perforation. Individual complications may overlap (e.g. inflammation – bleeding, tumor – obstruction, obstruction – bleeding). Frequency of complications in children and adults is different. While in childhood bleeding is often described, the most frequent complication in adulthood is intestinal obstruction [2,3]. Perforation occurs due to ulcer, incarceration, tumor or inflammation. Some cases have been reported with the occurrence of Crohn’s disease in the diverticulum. Tumors represent less frequent complications. Meckel’s diverticulum may be the source of histopathologically heterogeneous types of neoplasms, carcinoids especially, sarcomas, gastrointestinal stromal tumors (GIST), rarely adenocarcinomas or lymphomas. Intussusception with inverted Meckel’s diverticulum as a leading point is a rare phenomenon generally. There are only a few similar case reports in the literature describing inverted Meckel’s diverticulum as a cause of ileo-ileal invagination [4−9] and two similar cases with concomitant bleeding [10,11]. In other cases, the inverted diverticulum caused anemisation or massive bleeding alone [12,13], mimicked polypoid intraluminal tumor of the small intestine [14] or Crohn’s disease symptoms [15]. In Czech literature, a similar case report has not been published to date. Diagnosis of Meckel’s diverticulum and its complications is quite difficult; therefore, in cases of otherwise unexplained abdominal disorder, acute or chronic gastrointestinal bleeding or vague gastrointestinal symptoms (anorexia, nausea, vomiting, weight loss), the first diagnostic step should be to consider the possible presence of diverticulum. Complicated diverticulum can easily imitate simple gastroenteritis or ulcer disease. Plain radiography of the abdomen with small bowel obstruction usually shows no specific signs, however it may reveal enteroliths or calcified wall of Meckel’s diverticulum in some cases. Contrast examination of the small intestine may not be beneficial either, since the narrow or obturated diverticulum may not fill at all; nonetheless, enteroclysis may detect the inverted diverticulum as a filling defect in the small intestine extending along the longitudinal axis of the small intestine. Arteriography may be beneficial in acute hemorrhage when the diverticulum is bleeding from the nourishing artery. Contrast CT can also be helpful, although it produces a greater proportion of false-negative results due to the fact that the diverticulum may not be filled with contrast. The same applies to magnetic resonance imaging. Ultrasonography in Meckel’s diverticulum diagnosis is usually not too beneficial, for the unfavourable patient’s habitus, diverticulum size or its location between distended intestines during obstruction. Despite these facts, it was just ultrasound alone that brought fundamental diagnostic findings in our case (Fig.1). Endoscopic methods add further diagnostic options
capsule endoscopy and mainly double-balloon enteroscopy. One of the most reliable diagnostic methods is also a pertechnetate scan; however, the success of this screening depends on the presence of ectopic gastric mucosa where the technetium is accumulated. In adults, the sensitivity of this test is up to 50−60%. Scan sensitivity can be influenced by pentagastrin administration. Due to the fact that none of the abovementioned methods has a 100% diagnostic sensitivity in detecting Meckel’s diverticulum, the most valuable investigative modality is laparoscopic inspection of the abdominal cavity of small intestine. Complicated Meckel’s diverticulum always requires surgical resection. The extent of the resection required depends on the size of the diverticulum and associated complication. Minimum possible surgery is a simple wedge excision and suture of the intestine or laparoscopic stapled resection. Invagination may require bowel resection, as it was in our case. In malignant findings, it is necessary to proceed in accordance with the principles of oncological radicality. Surgical treatment of asymptomatic diverticulum might be a little controversial, yet the majority of surgeons choose resection as prevention of possible late complications.
Conclusion
Meckel’s diverticulum is the most common congenital anomaly of the gastrointestinal tract. The majority of diverticula do not cause any health problems. Complicated diverticulum displays no specific symptoms and mostly causes bleeding or obstruction of the digestive tract. Preoperative diagnosis, even if considered, is very difficult and detection of the diverticulum at this stage is rather a matter of coincidence than a rule. The most reliable diagnostic method in symptomatic and asymptomatic diverticula is laparoscopy, usually as part of definitive surgical treatment. In symptomatic diverticula, resection is the treatment of choice; in cases of asymptomatic diverticula, preventive removal is generally preferred.
This work has been supported by Grant RVO 64164.
Conflict of Interests The authors declare that they have not conflict of interest in connection with the emergence of and that the article was not published in any other journal.
MUDr. Jan Matek 1st
Department of Surgery of Charles University
Teaching Hospital in Prague
U nemocnice 2
128 00 Prague 2
e-mail: jan.matek@vfn.cz
Zdroje
- Yahchouchy EK, Marano AF, Etienne JC, el al. Meckel’s diverticulum. J Am Coll Surg 2001;192 : 658−62.
- Martin JP et al. Meckel‘s diverticulum. Amer Family Phys 2002;61 : 1037−41.
- Keller AA, Movson J, Shah SA. Meckel Diverticulum. Arch Intern Med 2003;163 : 2093−6.
- Ito T, Sato K, Maekawa H, et al. Adult intussusception caused by an inverted Meckel diverticulum. Case Rep Gastroenterol 2011;5 : 320−4.
- Banli O, Karakoyun R, Altun H. Ileo-ileal intussusception due to inverted Meckel’s diverticulum. Acta Chir Belg 2009;109 : 516−8.
- Steinwald PM, Trachiotis GD, Tannebaum IR. Intussusception in an adult secondary to an inverted Meckel’s diverticulum. Am Surg 1996;62 : 889−94.
- Saitoh O, Matsumoto H, Masaki K, et al. Intussusception of inverted Meckel’s diverticulum: a case report. Rinsho Hoshasen 1987;32 : 143−6.
- Ishida H, Sakata T, Yamasaki K, et al. A case of intussusception due to inverted Meckel’s diverticulum Rinsho Hoshasen 1978;23 : 1489−92.
- Dujardin M, de Beeck BO, Osteaux M. Inverted Meckel’s diverticulum as a leading point for ileoileal intussusception in an adult: case report. Abdom Imaging 2002;27 : 563−5.
- Andrabi SI, Spence GM, Clements WB. Inversion of Meckel’s diverticulum causing gastrointestinal bleeding and small bowel obstruction. Br J Hosp Med (London) 2007;68 : 442−3
- Kelley HG, Jr. Intussusception and bleeding caused by inverted Meckel’s diverticulum. Am J Surg 1962;104 : 108−10.
- Heider R, Warshauer DM, Behrns KE. Inverted Meckel’s diverticulum as a source of chronic gastrointestinal blood loss. Surgery 2000;128 : 107−8.
- Kopacová M, Vykouril L, Vacek Z, et al. Inverted Meckel’s diverticulum with ectopic pancreatic tissue as a source of severe gastrointestinal bleeding. J Gastrointest Surg 2010;14 : 578−81.
- Blakeborough A, McWilliams RG, Raja U, et al. Pseudolipoma of inverted Meckel’s diverticulum: clinical, radiological and pathological correlation. Eur Radiol 1997;7 : 900−4.
- Henneberg Holmboe C, Thorlacius-Ussing O, Teglbjaerg PS, et al. Inverted Meckel’s diverticulum masquerading Crohn disease in the small intestine. Scand J Gastroenterol 2003;38 : 225−7.
Štítky
Chirurgie všeobecná Ortopedie Urgentní medicína
Článek vyšel v časopiseRozhledy v chirurgii
Nejčtenější tento týden
2018 Číslo 8- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Hojení análních fisur urychlí čípky a gel
- Stillova choroba: vzácné a závažné systémové onemocnění
-
Všechny články tohoto čísla
- Ohlédnutí za letošním kongresem sekce mladých chirurgů
- Radicality of proximal gastrectomy – a rewiev
- Quality of life after proximal gastrectomy − a review
- Can the One-Step Nucleic Acid Amplification method of lymph nodes examination make the staging of pulmonary tumours more precise?
- Pleural empyema – single center experience
- Risk factors and post-operative complications after gastrectomy for cancer
- Liver Tuberculosis − a case report
- Inverted Meckel´s diverticulum: a rare cause of ileo-ileal intussusceptions and lower gastrointestinal bleeding
- XVIII. Dny mladých chirurgů profesora Stanislava Čárského
- Rozhledy v chirurgii
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Risk factors and post-operative complications after gastrectomy for cancer
- Radicality of proximal gastrectomy – a rewiev
- Quality of life after proximal gastrectomy − a review
- Liver Tuberculosis − a case report
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



