-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
Authors: J. Halička 1,2; E. Sahatqija 2; M. Krasňanský 2; K. Kapitánová 1,2; M. Fedorová 2; P. Žiak 1,2
Authors place of work: Očná klinika, Jesseniova Lekárska fakulta v Martine, Univerzita Komenského v Bratislave, SR, Prednosta MUDr. Peter Žiak, Ph. D 1; UVEA Mediklinik, Martin, SR, Primár MUDr. Rastislav Vida 2
Published in the journal: Čes. a slov. Oftal., 76, 2020, No. 1, p. 24-28
Category: Původní práce
doi: https://doi.org/10.31348/2020/3Summary
Purpose: Amblyopia is one of the most common childhood disease. The average prevalence of amblyopia in children is estimated at 2-5 %. It arises during the child development until the age of six, if not treated then, it persist throught adulthood. The aim of our work is to retrospectively analyze the results of treatment of anisometropic amblyopia using dichoptical training in virtual reality in adult amblyopic patients.
Materials and Methods: Our group consisted of 84 amblyopic patients with anisometropic amblyopia with an average age of 33.8 ± 9.4 years. Patients played a video game twice a week in the Oculus Rift 3D virtual reality. Together they completed 8 visual trainings, with one training lasting 60 minutes. Before and after the training we evaluated the best corrected visual acuity (BCVA).
Discussion: Throughout the group, we observed an improvement of 0.1 BCVA from 0.48 to 0.58 Sloan table (p <0.05). 17% of patients before training and 31% after visual training reached BCVA better or equal to 0.9. The overall response rate was 56% in adult patients (n = 47).
Conclusion: Our results suggest that a certain degree of residual neuro-plasticity in the visual cortex can be revealed in the adult brain, thereby improve visual acuity in adult amblyopic patients.
Keywords:
anisometropic amblyopia – visual training – virtual reality – Video games – adult patient – pleoptics
INTRODUCTION
Amblyopia, also known as “lazy eye”, is among the most common childhood diseases. It is a functional disorder defined as: “a developmental defect of spatial-visual processing, which appears in the central visual pathway” [1]. The most pronounced effect is loss of central visual acuity in one or, in rare cases, both eyes. Colour sense, adaptation to darkness and acuity of peripheral vision is generally within the norm [2]. The disorder occurs during the child’s development, in the critical period up to the age of 6 years. Morphologically and functionally both eyes are mostly in order, but there is generally a problem in the central interpretation of the image in the brain, because the eye was not sufficiently stimulated during development in early childhood age. The reason for reduced stimulation is most often division of refraction of the eyes, strabismus and deprivation of stimulus [3].
The average prevalence of amblyopia in children is estimated at 2-5 % [4]. The prevalence of amblyopia in adulthood depends on the geographical location and on the degree of prevalence of the disease. Elflein et al. state the prevalence of amblyopia at 5.6 % in the German population aged 35 – 74 years [5]. There are no current studies in either Slovakia or the Czech Republic on the prevalence of amblyopia in adult patients. A French school asserts that amblyopia in adult age is merely the result of poor treatment at a young age. Timely treatment of amblyopia in childhood age is of decisive importance.
Reduced central visual acuity does not reach the level of the dominant eye even after complete correction of refractive error or surgery for cataract or strabismus. For a further improvement of visual acuity we most frequently use penalisation of the dominant eye and pleoptic exercises. The “plastic period”, or the borderline of maximum neuroplasticity of the visual cortex, is between the ages of 6 and 8 years. Subsequent training of the amblyopic eye proceeds more slowly.
As in child patients, the first step in the treatment of amblyopia in adult patients is precise correction of the refractive error. Many of them wore correction in childhood age, and subsequently ceased to wear it during the course of puberty. If the patients wear correction, they rarely wear full anisometric correction. Precise correction leads to an improvement of visual acuity also in adult patients [6]. In children the gold standard in the treatment of amblyopia is penalisation, aimed at forcing the use of the amblyopic eye [7]. Penalisation works not only in childhood, but also in adult patients. The problem of occlusion therapy is non-compliance on the part of the patients, or their inability to wear occlusion [8]. Playing video games for adult patients is a further advance in the treatment of amblyopia, evidence of which is provided by positive results of both monocular and binocular training [9,10]. Motivation in the form of playing video games is of key importance in the “compliance” of patients [11]. The most recent advance in the development of new pleoptic methods is the use of virtual reality, which enables full dichoptic imaging – both eyes in part have a different image, concerning especially small details which are necessary in order to manage the game in question – and fundamentally better 3D imaging. To date this method has not been sufficiently described in adult patients.
Current research on animals and humans who demonstrate residual plasticity, in which patients have lost their vision in the dominant eye also at a more advanced age, provide examples of this [12,13]. This may be a consequence of demasking or determination of higher regions of the brain, which learn to analyse previously inhibited signals from the amblyopic eye [14]. On the basis of current knowledge, we therefore consider the “plastic period” to refer only to the time of maximal neurological plasticity, and with regard to regular cases of patients whose central visual acuity in the blunt-sighted eye has improved after the loss of the dominant eye, we consider neurological plasticity to be perhaps unlimited [15]. In a post-mortem analysis of the visual cortex in adult patients, this region appears to be plastic up to the age of 40 years on the basis of the presence of activation transmitters. At the same time, the authors document a discrepancy between the structural and functional properties of this part of the visual cortex [16].
The purpose of the submitted study is to present a retrospective analysis of the results of treatment of amblyopia with the aid of dichoptic training in virtual reality in adults with anisometric amblyopia.
METHOD OF STUDY
The cohort comprised 84 amblyopic patients with anisometric amblyopia, with an average age of 33.8 ± 9.4 years, of whom 60 were men and 24 were women. The youngest patients were aged 18 years and the oldest patients were aged 53 years. The average spherical equivalent in the amblyopic eye was +3.04 ± 0.3 DSph and in the non-amblyopic eye +1.37 ± 0.23 DSph (p < 0.05, Student t-test). The patients played a video game (Vivid Vision, USA) twice per week for a period of 60 minutes in 3D virtual reality Oculus Rift DK2 and HD (Oculus VR, USA).
We included in the study patients with anisometropic amblyopia aged 18 years and over, who were willing to undergo visual training. All the patients financed the training themselves. The exclusion criteria were strabismus, previous eye operation, corneal irregularities, opacification of ocular media including cataract, and active ocular pathology. All the patients were informed of the course of the clinical trial, and provided their informed consent in writing in accordance with the principles of the Helsinki declaration. The research study was approved by the Ethical Commission of the Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava.
All the patients underwent a basic ophthalmological examination, covering manifest and cycloplegic refraction, cover test, Worth test, examination of the anterior segment with a slit lamp, topographic examination of the cornea in patients with high astigmatism, and examination of the ocular fundus. We measured best corrected visual acuity (BCVA) with the aid of a calibrated optotype with a liquid crystal display (LCD CC-X10, Topcon, Japan). We measured BCVA both before and after the end of training in virtual reality.
We conducted dichoptic visual training with the use of the computer game Diplopia Game (Vivid Vision, USA), which was run in a virtual reality helmet Oculus Rift DK2 (Oculus VR, USA). Oculus Rift DK2 was equipped with an AMOLED display (5.7” in diagonal, resolution 960 x 1080 pixels per eye) with a visual field of 100°, with an added accelerometer, gyroscope and magnetometer for the system of monitoring head position (Fig. 1). The VR Oculus Rift helmet was attached to a computer system (Intel i5 3-4 GHz, 8 GB RAM, Nvidia GeForce 970GT 4 GB; MSi, USA). We had four games at our disposal – basketball (Fig. 2A), a block game (Fig. 2B), vegetable picking (Fig. 2C) and cosmic flight (Fig. 2D). All the games had a dichoptic setting, in which the part of the displayed image was different in both eyes.
Fig. 1. Virtual reality system (Oculus Rift, USA) 
Fig. 2. What does the patient see in virtual reality? The left and right eyes have their own display. The principle of dichoptic vision consists in the division of the image or part of the image between the eyes. In the above examples of games – basketball (fig. 2A), block game (fig. 2B), vegetable picking (fig. 2C) and cosmic flight (fig. 2D) – we see what is seen by the the dominant eye on the right, amblyopic eye on the left. 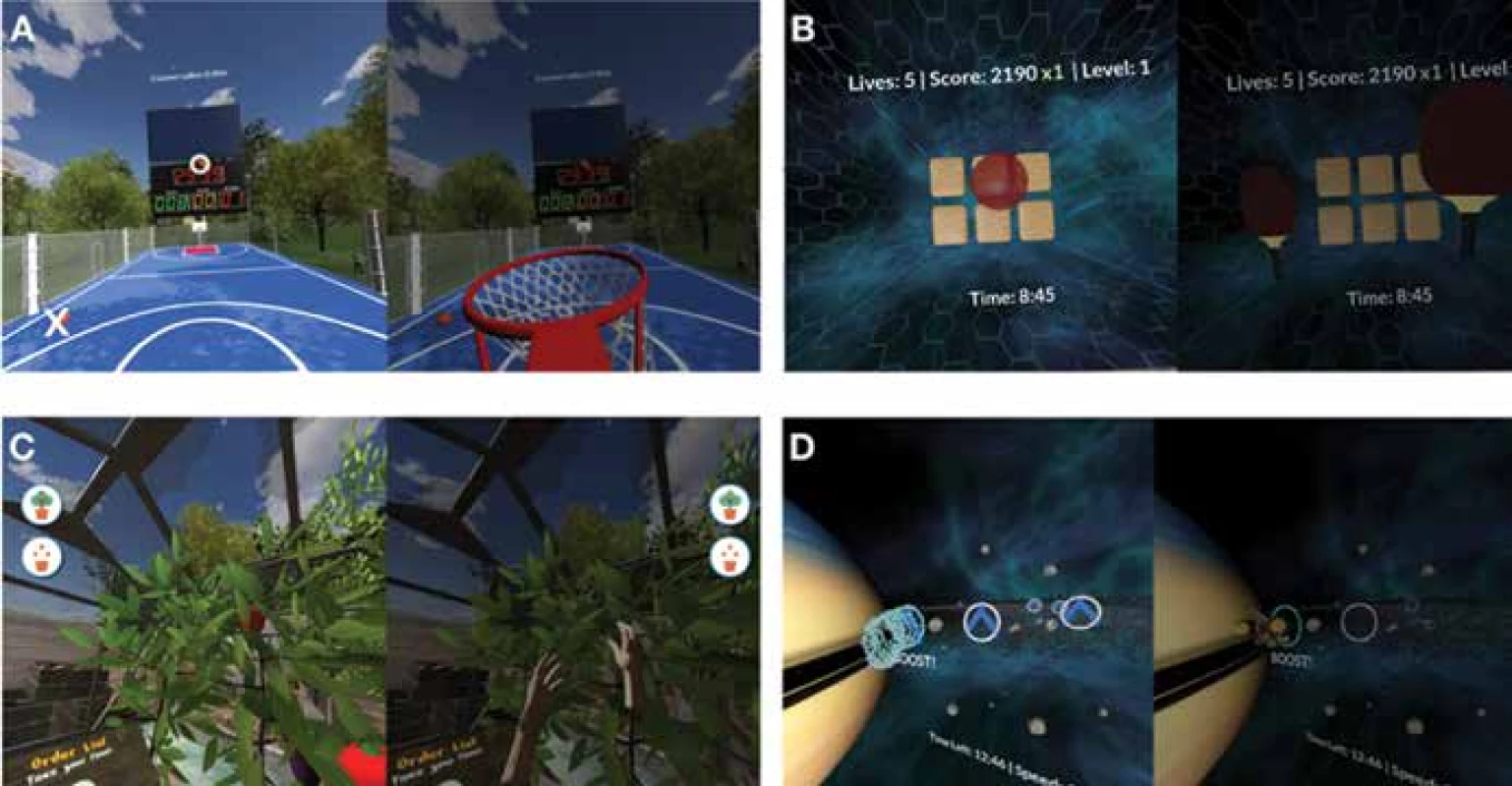
One cycle of the exercise contained 8 hours of training, performed twice per week. Each session covered 60 minutes of training with different games (15-20 minutes per game). BCVA was tested before the first session and after the last training session. Pleoptic exercises in the home environment were not limited.
An analysis of the data was performed with the aid of SPSS software version 19.0 for Windows (IBM, Armonk, USA). The normality of distribution of the selection data was evaluated with the use of a Shapiro-Wilk test. The data was not normally distributed, and for this reason a Wilcoxon test was used for evaluating the difference in BCVA before and after the training. For correlation of the change of visual acuity to the calculated BCVA, we used a Spearman’s rank correlation coefficient. A p-value lower than 0.05 was considered statistically significant for all tests.
RESULTS
In the entire group we observed an improvement of BCVA by 0.1, from a value of 0.48 to a value of 0.58 on a Sloan table (p < 0.05, graph 1). We did not record a statistically significant difference upon a comparison of the change of BCVA in comparison with the age of the patients. In total, before training 17 % and after training 31 % of amblyopic eyes attained BCVA of equal to or more than 0.9 (Graph 2), in which 56 % (n = 47) of adult patients responded to treatment by increase of BCVA. In 37 cases we did not record any change of BCVA after training. We did not find any correlation between change of BCVA and initial BCVA, the Spearman’s rank correlation coefficient rho = -0.015, P = 0.892. In patients who responded to treatment, the average improvement of BCVA was by 0.16.
Graph 1. Improvement of best corrected visual acuity in entire cohort before and after 8 hours of training (p < 0.05) 
Graph 2. Representation of vision in individual groups according to best corrected visual acuity (n = 84) 
DISCUSSION
Amblyopia is a disease with a prevalence of approximately 4 % in children and 2 % in adults. It is mostly unilateral, both legislatively and formally people with one eye function normally. Only a few professions exist for which individuals require two healthy eyes. However, in the case of trauma there is an up to three times higher risk of loss of the good eye if the other eye is amblyopic [17]. Why, therefore, should we treat amblyopia? The main advantage is an improvement of best corrected visual acuity and stereoscopic vision. Also interesting is incidental realignment of the strabismal eye, attaining better visual acuity. For adult patients who are accustomed to functioning with one eye, all we can promise is to create a kind of “spare tyre”, with better capacity of vision in the case of trauma or disease of the healthy eye.
In the case of small children with anisometropic amblyopia, a period of 16 to 22 weeks of treatment by optic correction alone is sufficient in most cases to overcome the suppression of the amblyopic eye and lead to an improvement of visual acuity by 2 or more rows. In almost one third of child patients, optical correction alone is sufficient for the complete resolution of amblyopia [18]. The gold standard in treatment is penalisation of the dominant eye. Older children require approximately 120 hours of treatment for an improvement by 1 row. The disadvantage of this treatment is its limitation by the critical period, which means that it is effective maximally up to the age of 8 years. Adult patients with amblyopia also show an interest in the solution or at least an improvement of their existing condition. This interest is also confirmed by the number of patients participating in our study.
In adults, scientific evidence of effective treatment of amblyopia is insufficient. In the practical part we processed data on 84 amblyopic patients, who underwent 8 dichoptic training sessions with the aid of Oculus Rift. In the entire cohort of patients we recorded an improvement of BCVA by one row. In similar studies with young patients, it is stated that 10 hours of binocular playing of a dichoptic video game leads to an improvement by 1.6 rows [19]. The use of anti-suppressive binocular pleoptic training may be more effective than monocular pleoptic training of amblyopia, because suppression is physiologically manifested only under binocular conditions [20]. It is necessary to take into consideration the fact that our study presents the results after 8 dichoptic training sessions, and some patients require a longer duration of treatment before attaining an improvement of vision.
In a contemporary retrospective study we encountered inconsistent use of various tests for the comparison of 3D vision (RanDot, Lang, Titmus), which cannot be compared mutually. As a result, we present the results of our previous study, in which the average capacity of 3D vision was improved following visual training from 263.3 ± 135.1 before training to 176.7 ± 152.4 angular seconds after 8 hours of training. This change was statistically significant (p < 0.01) [21].
The results of our study point to the possibility of using visual virtual reality training in the treatment of amblyopia in adulthood. Our results indicate that it is possible to “detect” a certain degree of neural plasticity in the visual cortex of the adult brain. From the results we obtained, the most effective exercise appears to be in the case of a medium-severe decrease of BCVA (Graph 2), although the correlation analysis did not demonstrate a significant relationship. From clinical experiences to date with patients with anisometric amblyopia who have not improved after training, we assume the effect of microstrabismus as a negative prognostic factor. Pleoptic training in a certain proportion of adult patients with amblyopia represents a possibility for improving quality of life. In future it shall be necessary to conduct a controlled clinical trial and compare pleoptic training virtual reality with conventional pleoptic exercises.
A limitation of the presented study is the lack of long-term observation which could demonstrate the stability of the obtained result.
Zdroje
1. Diamond, GR., Eggers, HM.: Textbook of ophthalmology. Vol. 5, Strabismus and pediatric ophthalmology. London, Mosby, 1993, 70 p.
2. Divišová, G.: Strabizmus. 2. vyd. Praha, Avicenum, 1990, 312 s..
3. Williams, C., Northstone, K., Harrad, RA. et al.: Amblyopia treatment outcomes after preschool screening v school entry screening: observational data from a prospective cohort study. Br J Ophthalmol, 87 (8); 2003 : 988–993.
4. Wu, C., Hunter, DG.: Amblyopia: diagnostic and therapeutic options. Am J Ophthalmol, 141 (1); 2006 : 175–184.
5. Elflein, HM., Fresenius, S., Lamparter, J. et al.: The prevalence of amblyopia in Germany: data from the prospective, population-based Gutenberg Health Study. Deutsches Arzteblatt international, 112(19); 2015 : 338–344.
6. Gao, TY., Anstice, N., Babu, RJ. et al.: Optical treatment of amblyopia in older children and adults is essential prior to enrolment in a clinical trial. Ophthalmic Physiol Opt., 38(2); 2018 : 129-143.
7. Loudon, SE., Simonsz, HJ.: The history of the treatment of amblyopia. Strabismus, 13 (2); 2005 : 93–106.
8. Simonsz-Tóth, B., Joosse, MV., Besch, D.: Refractive adaptation and efficacy of occlusion therapy in untreated amblyopic patients aged 12 to 40 years. Graefes Arch Clin Exp Ophthalmol., 257(2); 2019 : 379-389.
9. Li, J., Thompson, B., Deng, D. et al.: Dichoptic training enables the adult amblyopic brain to learn. Curr Biol, 23 (8); 2013 : 308–309.
10. Hess, RF., Babu, RJ., Clavagnier, S. et al.: The iPod binocular home-based treatment for amblyopia in adults: efficacy and compliance. Clin Exp Optom., 97(5); 2014 : 389-98.
11. Gao, TY., Guo, CX., Babu, RJ. et al.: Effectiveness of a Binocular Video Game vs Placebo Video Game for Improving Visual Functions in Older Children, Teenagers, and Adults With Amblyopia: A Randomized Clinical Trial. JAMA Ophthalmol., 136(2); 2018 : 172-181.
12. Rahi, JS., Logan, S., Cortina-Borja, M. et al.: Prediction of improved vision in the amblyopic eye after visual loss in the non-amblyopic eye. Lancet, 360 (9333); 2002 : 621–622.
13. El Mallah, MK., Chakravartz U., Hart, PM.: Amblyopia: is visual loss permanent? Br J Ophthalmol, 84 (9); 2000 : 952–956.
14. Restani, L., Cerri, C., Pietrasanta, M. et al.: Functional masking of deprived eye responses by callosal input during ocular dominance plasticity. Neuron, 64 (5); 2009 : 707-18.
15. Proscialloy, P., Proscialloy E.: The accuracy of binocular fixation preference for the diagnosis of strabismic amblyopia. J Pediatr Ophthalmol Strabismus, 14; 2010 : 205–10.
16. Siu, CR., Beshara, SP., Jones, DG. et al.: Development of Glutamatergic Proteins in Human Visual Cortex across the Lifespan. J Neurosci., 37(25); 2017 : 6031-6042.
17. Tommila, V., Tarkkanen, A.: Incidence of loss of vision in the healthy eye in amblyopia. Br J Ophthalmol, 65 (8); 1981 : 575-7.
18. Cotter, SA., Edwards, AR., Wallace, DK. et al.: Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology, 113 (6); 2006 : 895-903.
19. Li, SL., Reynaud, A., Hess, RF. et al.: Dichoptic movie viewing treats childhood amblyopia. J AAPOS, 19 (5); 2015 : 401–405.
20. Hess, RF., Thompson, B.: Amblyopia and the binocular approach to its therapy. Vision Res., 114; 2015 : 4-16.
21. Žiak, P., Holm, A., Halička, J. et al.: Amblyopia treatment of adults with dichoptic training using the virtual reality oculus rift head mounted display: preliminary results. BMC Ophthalmol, 17 (1); 2017 : 105.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2020 Číslo 1- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Konjunktivitida a původce Corynebacterium macginleyi – kazuistika
-
Všechny články tohoto čísla
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Current use of the automatic retinal oximetry. Review
- Importance of PET/CT examination in patients with malignant uveal melanoma
- Enucleation after Stereotactic Radiosurgery in Patients with Uveal Melanoma
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Importance of PET/CT examination in patients with malignant uveal melanoma
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



