-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
proLékaře.cz / Odborné časopisy / Česká a slovenská neurologie a neurochirurgie / 2017 - Supplementum 1Possibilities of Evaluation of Psychometric Properties of Scales for Assessment of the Risk of Pressure Lesions at Selected Intensive Care Workplaces – a Pilot Study
Možnosti hodnocení psychometrických vlastností škál pro hodnocení rizika vzniku tlakových lézí na vybraných pracovištích v intenzivní péči – pilotní studie
Cíl:
Posouzení inter-rater reliability škál pro riziko vzniku dekubitů (Nortonové, modifikované Nortonové, Bradenové a Jackson/ Cubbin modifikované dle Maarit Ahtiala) u pacientů hospitalizovaných na pracovištích intenzivní péče.Soubor a metodika:
Pilotní fáze prospektivní, observačně deskriptivní studie probíhala v březnu 2017 na pěti odděleních intenzivní péče čtyř různých nemocnic v České republice. U každého pacienta byla realizována tři pravidelná hodnocení rizika vzniku dekubitů dvěma nezávislými hodnotiteli daného pracoviště, a to za pomocí čtyř standardizovaných škál. Do pilotní studie bylo zařazeno 26 probandů z celkového počtu 173 hospitalizovaných pacientů, 61,5 % (n = 16) mužů a 38,5 % (n = 10) žen.Výsledky:
Při všech hodnocení pacientů vykazovali první hodnotitelé nižší bodové hodnocení, které souvisí s vyšším rizikem vzniku dekubitů. Průměry skóre hodnotících škál se od prvního hodnocení v průběhu hospitalizace na jednotce intenzivní péče zvyšují.Závěr:
Významnou roli v inter-rater reliabilitě a využitelnosti hodnotících škál sehrává zkušenost s jejich využitím a důsledná edukace hodnotitelů. S ohledem na celkový počet probandů v pilotní studii nelze vyvodit jednoznačný závěr s doporučením pro konkrétní škálu k hodnocení rizika pro pacienty v intenzivní péči. Jako účelná se hodnotitelům v klinické praxi jevila škála Jackson/ Cubbin modifikovaná dle Maarit Ahtiala.Klíčová slova:
dekubitus – intenzivní péče – ošetřovatelství – škála rizika
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors: S. Saibertová; A. Pokorná
Authors place of work: Medicine, Masaryk university, Brno ; Czech Republic ; Department of Nursing, Faculty of
Published in the journal: Cesk Slov Neurol N 2017; 80(Supplementum 1): 36-40
Category: Původní práce
doi: https://doi.org/10.14735/amcsnn2017S36Summary
Aim:
Assessment of the inter-rater reliability of scales for the pressure ulcer development risk (Norton, modified Norton, Braden and Jackson/ Cubbin modified by Maarit Ahtiala) in patients hospitalized at intensive care units.Material and methods:
The pilot stage for the prospective, observational and descriptive study took place in March 2017 at five intensive care units of four different hospitals in the Czech Republic. For each patient, three regular evaluations of pressure ulcer risk were performed by two independent raters at the given workplace using four standardised scales. The pilot study comprised 26 probands of the total number of 173 hospitalized patients, 61.5% (n = 16) men and 38.5% (n = 10) women.Results:
For each evaluation of patients, the first raters provided lower score, which is associated with a higher risk of pressure ulcer development. The average scores at rating scales increase from the first evaluation in the course of hospitalization at intensive care units.Conclusion:
An important role in the inter-rater reliability and usability of the rating scales consists in the experience with their use and in thorough education of raters. With regard to the total number of probands in the pilot study (n = 26), it is not possible to draw a definite conclusion with the recommendation for a specific scale for rating the pressure ulcers risks in intensive care unit patients. The evaluators in clinical practice found the Jackson/ Cubbin scale modified by Maarit Ahtiala as the most practical.Key words:
pressure ulcer – intensive care – nursing – risk scaleIntroduction
The evaluation of pressure ulcer risk is one of the priority issues in nursing [1]. The incidence of chronic/ non-healing wounds, which include pressure ulcer among the most frequent ones, is connected with the overall aging of the population. The incidence of non-healing wounds in intensive care is also associated with the frequent use of invasive inputs and equipment, which may cause such complications, along with the fact that the care of the skin of the patients may be neglected, in particular in relation to priority given to life saving procedures [1].
Aim
Assessment of the inter-rater reliability of scales for the pressure ulcer development risk (Norton, modified Norton, Braden and Jackson/ Cubbin modified by Maarit Ahtiala) in patients hospitalized at selected intensive care units.
Methods
The pilot stage for the prospective, observational and descriptive study took place in March 2017 at five intensive care units (ICU) of four different hospitals in the Czech Republic, which agreed with the performed study. The study sample included only those patients who were hospitalized at the ICU for five or more days. The patients were evaluated for pressure ulcer risk and the emergence of pressure ulcers during hospitalization. The risk of pressure ulcer development was always evaluated by two raters/ evaluators working on the site. The first evaluator was always instructed in the use of rating scales and trained as part of the engagement in project activities involved in the identification of risk of pressure ulcer development at intensive care departments and also within the scope of their studies at the Faculty of Medicine of the Masaryk University. The other evaluator was instructed informally on the use of scales for the evaluation of the risks directly at each workplace. For each patient, evaluation of pressure ulcer risk was performed using four standardised rating scales according to Norton [2], modified Norton [3], Braden [4] and Jackson/ Cubbin modified by Maarit Ahtiala [5]. At admission, GCS (Glasgow Coma Scale), artificial pulmonary ventilation and the occurrence of pressure ulcers were monitored for each patient; see further. The evaluation was conducted always at the same time: within 24 hours after the admission of the patient to the ICU, the second evaluation took place on the 5th day of hospitalization and the last evaluation was performed at the end of hospitalization at the ICU. The evaluators had to assess the patient independently of each other, without knowing the total score at the rating scale given by the other evaluator. The final scores at the rating scales were entered in the original recording sheet. When monitoring pressure ulcers during hospitalization, not only the positioning and the day of the onset of the lesion were monitored, but in particular the evaluation of category rating of the pressure ulcer according to the EPUAP recommendation [6]. Also, reporting the L89 diagnosis code – decubitus ulcer according to ICD-10 (International Statistical Classification of Diseases and Related Health Problems) [7] by the doctor in the medical documentation was observed.
Sample
The pilot study included 26 patients from the total number of 173 patients hospitalized at selected intensive care units in the study period (March 2017). The sample of respondents comprised 61.5% (n = 16) men and 38.5% (n = 10) woman. The average age of respondents was 64 years. Basic information about the patients is summarised in Tab. 1.
Tab. 1. Patient Basic demographic data (n = 26). 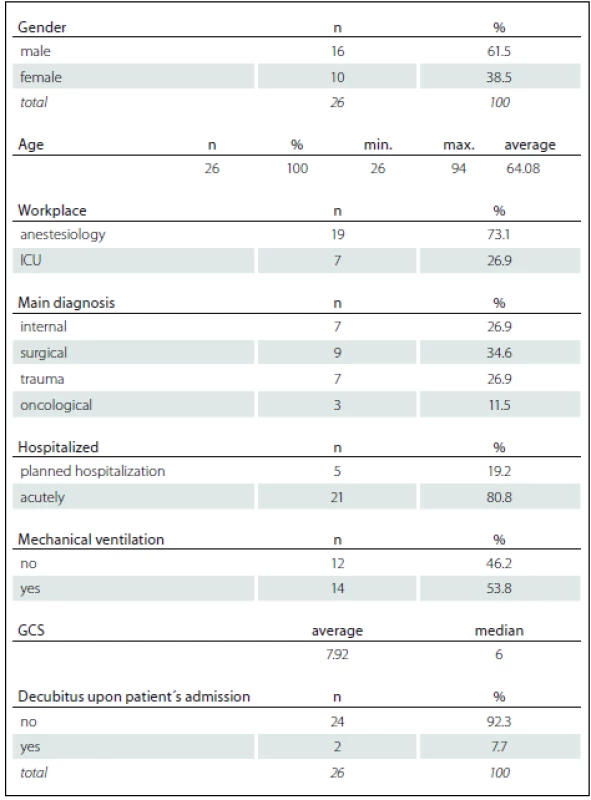
Results and discussion
For an appropriate identification of risks of pressure ulcer lesions and preventive measures, the implementing strategy of preventive interventions should be comprehensive and also properly prepared for the existing needs of the specific department [8]. The selection of the correct standardised rating scale for the identification of pressure ulcer risk at the intensive care unit is essential for the quality of care. The assessment of the inter-rater reliability in the prediction of pressure ulcer risk employed four internationally used standardised scales, two of them most frequently used in the Czech Republic, namely the scale according to Norton and the modified Norton scale, the latter being still recommended in the methodology of pressure ulcer examination for publishing in the Bulletin of the Ministry of Health No. 6/ 2009. Further, the Braden scale was included, which is the most frequently used scale in Anglo-Saxon countries. The fourth scale selected for the purpose of the study is one of the newest scales created for intensive care workplaces, the scale of Jackson/ Cubbin modified by Maarit Ahtiala, which was translated with the consent of the author and based on a well-defined methodology (translated into Czech by Pokorná, translation of the full version of the scale is available from the author). This scale always predicts the particular risk of pressure ulcer development in the context of the serious condition of the patient hospitalized at the intensive care unit.
In order to compare the evaluation of the first and the second evaluators/ raters, the scores at each scale were averaged (Tab. 2 – 4). In the evaluation of patients both at the admission and in the other instances, the first evaluators/ raters provided a lower score, which is associated with a higher risk of development of pressure ulcers. It can be noted that effective instruction in the work with the evaluation instruments and the readiness of the workplace are very important part of the implementation not only of the new rating scales into clinical practice, as the data we obtained confirm. However, the generalization of conclusions is significantly limited based on the total number of patients included in the study (n = 26). The number of probands was influenced by the fact that the average length of stay at intensive care units is reduced and majority of patients spent less than five days at the studied workplaces, thus, a relatively small sample of probands was included in the study; still, the methodology of the study was verified and it is possible to implement the next stage of data collection.
Tab. 2. Assessment of the risk of decubitus formation upon patient´s admission. 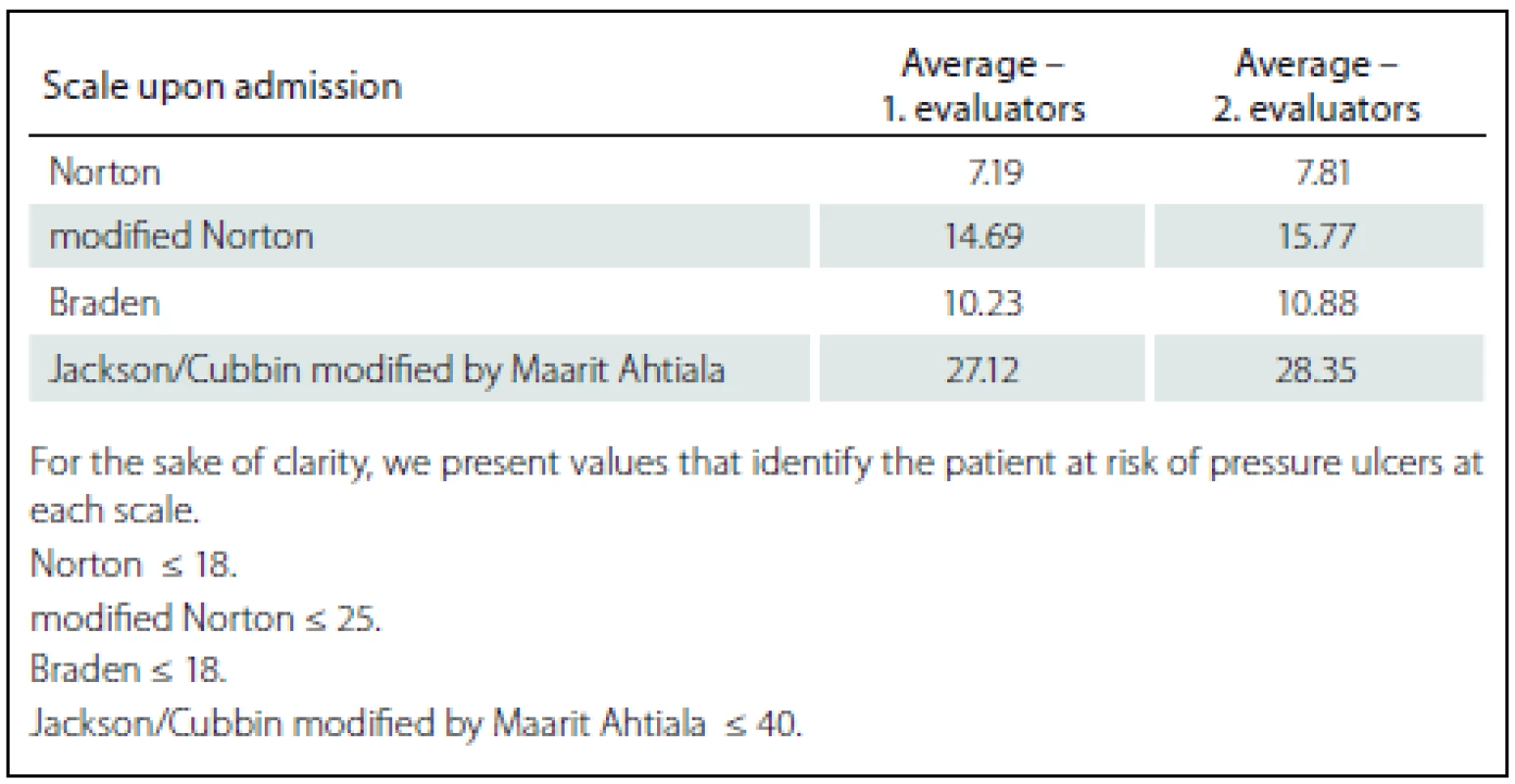
Tab. 3. Assessment of the risk of decubitus formation on the 5<sup>th</sup> day of hospitalization. 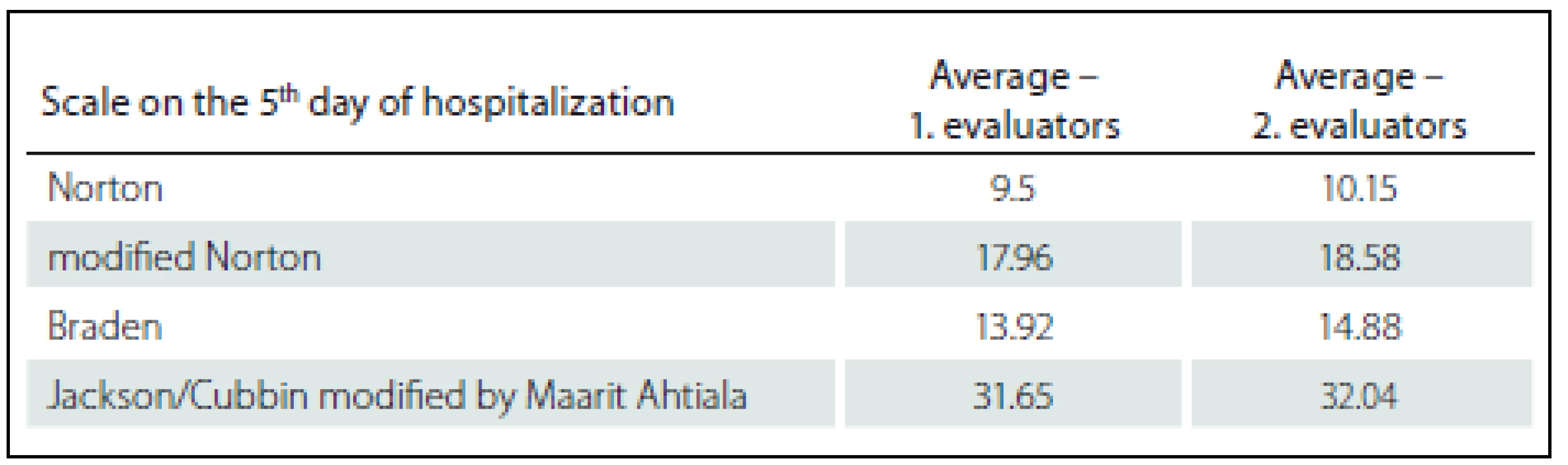
Tab. 4. Assessment of the risk of decubitus formation at the end of hospitalization in intensive care unit (ICU). 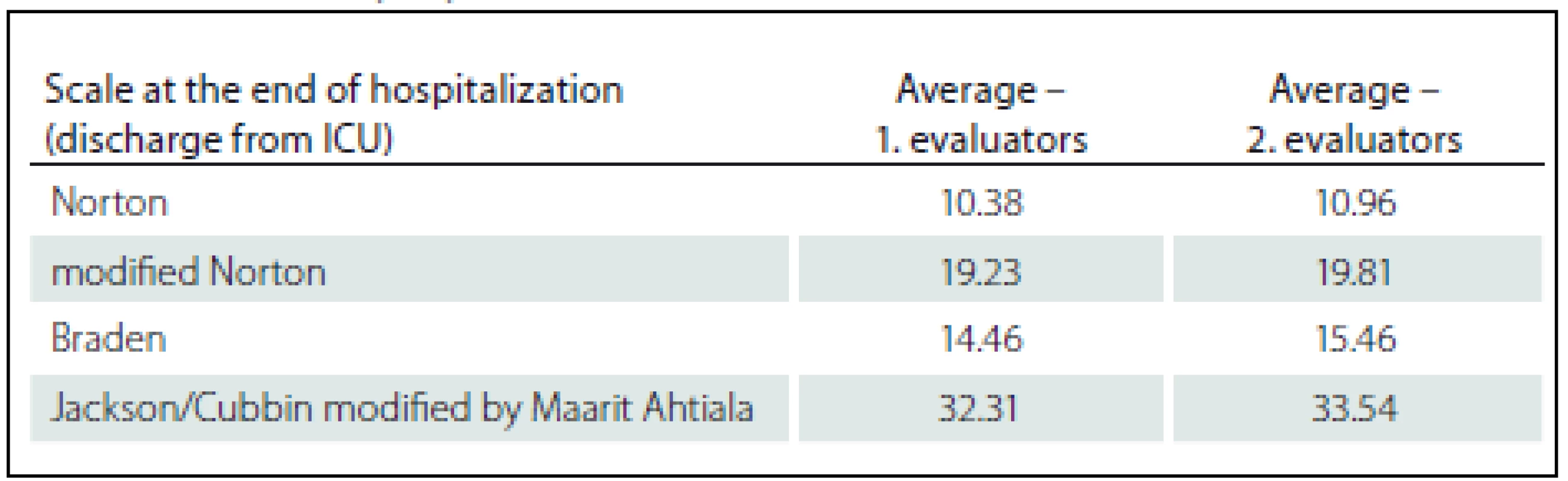
Further analysis of the data found that the average scores at the rating scales increase from the first evaluation during hospitalization at the intensive care unit; thus, it can be assumed that the rated risk of pressure ulcer development decreases along with the length of hospitalization, which is probably connected with the improvement of the health condition of the patient.
The presumed gradual reduction of the identified risk of the emergence of pressure ulcers can be confirmed also in Tab. 5, 6 with the analysis of resulting scores at individual scales showing the patients with the risk of development of pressure ulcers and with-out the risk of pressure ulcers. Also, the differences between the first and the second evaluators/ raters were assessed using the modified Norton and Braden scales. While in the case of the first evaluators/ raters all patients were identified as in the risk of pressure ulcer development at admission, the second raters identified one patient without the risk of pressure ulcers. In the second and third assessments, again, the second evaluators/ raters considered more patients without the risk of pressure ulcer development than the first nes. In consideration of the main limit of a limited sample of probands, there are differences in the risk assessment between the systematically and formally instructed and “uneducated” evaluators/ raters, which, in practice, may lead to inadequate identification of patients at risk, and thus higher incidence of pressure ulcer lesions, if the patient at risk is not administered adequate care and appropriate preventive intervention (Graph 1).
Tab. 5. Patients at risk and without risk of pressure ulcer according to used standardized scales – judged by 1<sup>st</sup> evaluator. 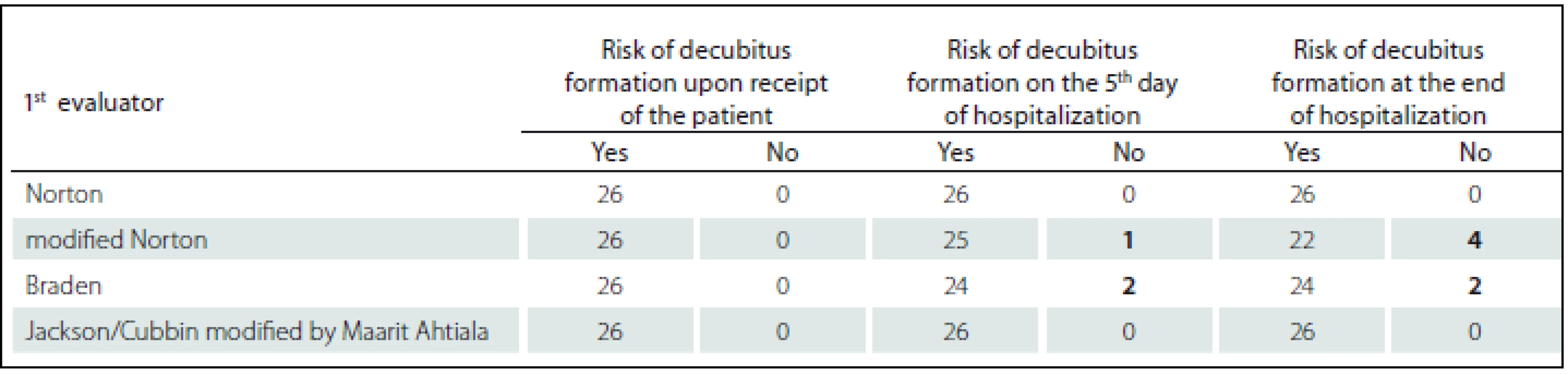
Tab. 6. Patients at risk and without risk of pressure ulcers according to used standardized scales – judged by 2<sup>nd</sup> evaluator. 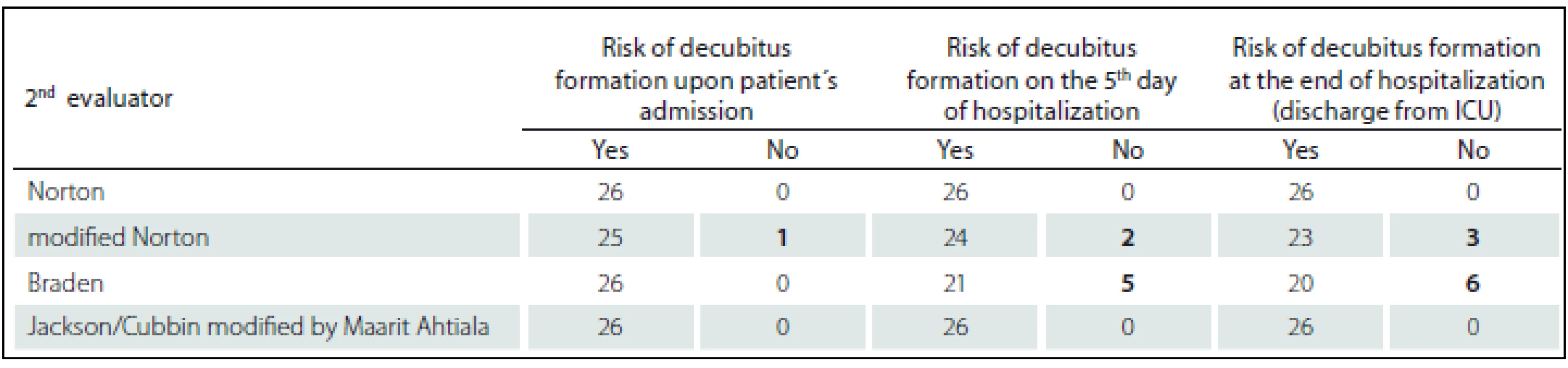
Graph 1. The difference in the assessment of the risk of decubitus formation between 1<sup>st</sup> and 2<sup>nd</sup> evaluators in individual scales. 
As Graph 1 shows, there are significant differences between individual evaluators/ raters in the number of points, the most significant ones occurring with the most commonly used modified Norton scale. The use of the traditional Norton scale without modification also shows differences, although not so significant; still, at the last evaluation at the time of release or transfer of the patient from the intensive care unit, there are evident outliers, both in positive and negative direction of evaluation of the risk for patients. Out of the analysed data from the pilot study, the results of the risk evaluation using the Braden scale appear as the most consistent. The Jackson/ Cubbin scale modified by Maarit Ahtiala was evaluated as the most user friendly as well as the most practical (providing the most detail for the intensive care unit patients).
In the course of the pilot study, hospitalised patients in the study sample were evaluated for the incidence of pressure ulcers (Hospital Acquired Pressure Ulcers; HAPU), because it is the only way to identify the sensitivity of the scale for the risk assessment. In the reference period, pressure ulcers developed in four patients out of the total of 26 probands. Three pressure ulcers were found in the sacrum area, out of which two were rated as stage 1 and one as stage 3. The fourth pressure ulcer was identified in the area of the labial commissure, in causal relationship with the use of endotracheal cannula, and it was rated as stage 2. It is one of the most frequent localization of medical technology and instruments related pressure lesions [9]. In neither case the doctors reported the code L89 according to the ICD-10, i.e., the care could not be covered, because it was not reported. The fact that pressure ulcers are not reported by doctors was also confirmed by other studies [1,9,10].
Conclusion
From the pilot analysis of the study aimed at evaluating the inter-rater reliability and usability of scales for the assessment of risk of pressure ulcer development, it was found that an important role consists in the experience with the use of the scale and thorough education of the evaluators/ raters. Based on the total number of probands in the pilot study, it is not possible to draw a definite conclusion with the recommendation for a specific scale for risk evaluation in intensive care patients, but the evaluators/ raters in clinical practice found the Jackson/ Cubbin scale modified by Maarit Ahtiala as the most practical. Another significant finding was that pressure ulcer was identified in 15% (n = 4) of patients monitored in the pilot study. There is a positive finding that in most cases, stage 1 of pressure ulcer was identified and recorded in the nursing documentation.
This study was supported by the Specific UniversityResearch provided by Ministry of Education, Youth and Sports (MEYS, MŠMT in Czech), grant no. 0922/ 2016 with the title “Identification of the risk of pressure lesions in intensive care – evaluation of the psychometric properties of pressure ulcer risk scale (IRTL)”. All rights reserved.
Authors would like to thank to colleagues who collected data at clinical settings: BSc. Vendula Zdrálková, BSc. Hana Hrabovská, BSc. Monika Maxnerová, BSc. Květa Kozlová, BSc. Michal Pelc a BSc. Michal Nový.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 15. 6. 2017
Accepted for print: 3. 7. 2017
PhDr. Simona Saibertová
Department of Nursing
Faculty of Medicine
Masaryk university
Kamenice 5
625 00 Brno
e-mail: saibert@med.muni.cz
Zdroje
1. Pokorná A, Saibertová S, Velichová R, et al. Sorrorigenní rány, jejich identifikace a průběh péče. Cesk Slov Neurol N 2016;79/ 112(Suppl 1):S31 – 6. doi: 10.14735/ amcsnn2016S31.
2. Norton D, McLaren R, Exton-Smith AN. An Investigation of Geriatric Nursing Problems in Hospital, London: ©National Corporation for the Care of Old People (now Centre for Policy on Ageing 1962.
3. Věstník MZ ČR. Částka 6. Metodické doporučení. Metodika prevalenčního sledování dekubitů na národní úrovni). Ministerstvo zdravotnictví 2009. [online]. Dostupné z URL: https:/ / www.kancelarzp.cz/ images/ cmu_documents/ dekubity/ Vestnik_MZCR.pdf.
4. Mandysová P, Ehler E, Trejablová L. Česká verze ŠkályBradenové: metodika překladu a shoda mezi posuzovateli. Ošetrovateľstvo 2012;2(4):137 – 42.
5. Ahtiala MH, Soppi E, Kivimäki R. Critical Evaluation of the Jackson/ Cubbin Pressure Ulcer Risk Scale – a Secondary Analysis of a Retrospective Cohort Study Population of Intensive Care Patients. Ostomy Wound Manage 2016;62(2):24 – 33.
6. Haesler E, ed. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific. Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Osborne Park, Australia: Cambridge Media 2014. [online]. Available from URL: https:/ / www.npuap.org/ wp-content/ uploads/ 2014/ 08/ Updated-10-16-14-Quick-Reference-Guide-DIGITAL-NPUAP-EPUAP-PPPIA-16Oct2014.pdf.
7. Mezinárodní statistická klasifikace nemocí a přidružených zdravotních problémů: MKN-10: desátá revize: aktualizovaná druhá verze k 1. 1. 2014. 2. vyd. [online]. Dostupné z URL: http:/ / www.uzis.cz/ zpravy/ aktualni-verze-mkn-10-cr.
8. Black J. Implementation of Pressure Ulcer Prevention Guidelines – Where to Start? Cesk Slov Neurol N 2016;79/ 112(Suppl 1):S45 – 6 doi: 10.14735/ amcsnn2016S45.
9. Pokorná A, Benešová K, Mužík J, et al. Sledování dekubitálních lézí u pacientů s neurologickým onemocněním – analýza Národního registru hospitalizovaných. Cesk Slov Neurol N 2016;79/ 112(Suppl 1):S8 – 14 doi: 10.14735/ amcsnn2016S8.
10. Pokorná A, Benešová K, Jarkovský J, et al. Pressure Injuries in Inpatient Care Facilities in the Czech Republic: Analysis of a National Electronic Database. J Wound Ostomy Continence Nurs 2017;44(4):331 – 5. doi: 10.1097/ WON.0000000000000344.
Štítky
Dětská neurologie Neurochirurgie Neurologie
Článek Editorial
Článek vyšel v časopiseČeská a slovenská neurologie a neurochirurgie
Nejčtenější tento týden
2017 Číslo Supplementum 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Magnosolv a jeho využití v neurologii
- Zolpidem může mít širší spektrum účinků, než jsme se doposud domnívali, a mnohdy i překvapivé
- Nejčastější nežádoucí účinky venlafaxinu během terapie odeznívají
-
Všechny články tohoto čísla
- Wound Healing – Cost-effectiveness Data from the Providers and Payers Viewpoint
- Deformation is a Cell “Killer” – Implications for Protecting Persons with a Spinal Cord Injury from Pressure Ulcers
- The Relationship between Risk Factors, Risk Assessment, and the Pathology of Pressure Ulcer Development
- Differential Diagnosis in Pressure Ulcers and Medical Devices
- Possibilities of Evaluation of Psychometric Properties of Scales for Assessment of the Risk of Pressure Lesions at Selected Intensive Care Workplaces – a Pilot Study
- Employment of Flap Surgery in Pressure Ulcers Surgical Treatment
- The Pressure Ulcers Evidence in Patients with Spinal Cord Injury at Spinal Unit of Department of Traumatology at University Hospital Brno 2013– 2016
- The Skin Lesions as a Complications of Parkinson’s Disease
- Validaton of Nursing Diagnosis of Acute and Chronic Pain According to NANDA International in the Patients with Wound
- Pressure Ulcers Represents a Constant Nightmare for Me
- Editorial
- Data Sources for Monitoring of Non-healing Wounds in a National Health Information System – Epidemiology of Non-healing Wounds – Analysis of the National Register of Hospitalized Patients in 2007– 2015
- Česká a slovenská neurologie a neurochirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Validaton of Nursing Diagnosis of Acute and Chronic Pain According to NANDA International in the Patients with Wound
- Employment of Flap Surgery in Pressure Ulcers Surgical Treatment
- Differential Diagnosis in Pressure Ulcers and Medical Devices
- Pressure Ulcers Represents a Constant Nightmare for Me
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



