-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Results of Achilles tendon rupture repair. Classical open approach versus percutaneous suture
Authors: Dávid Fekete; Martin Carda
Authors place of work: Traumatologické oddělení Nemocnice Pardubice, Nemocnice Pardubického kraje
Published in the journal: Úraz chir. 26., 2018, č.2
Summary
Goal: To compare the results of threatment of Achilles tendon rupture by open and percutaneous suture.
Method: Authors retrospectively evaluated a group of 73 pacients with acute Achilles tendon rupture threated in the years 2011–2013. 54 patient were threated by percutaneous tendon suture (CLOSE), 19 uderwent open tendon suture (OPEN). They compared the total threatment time, associated complications and subjective pacient’s rating according to questionnaire study - Rupp score.
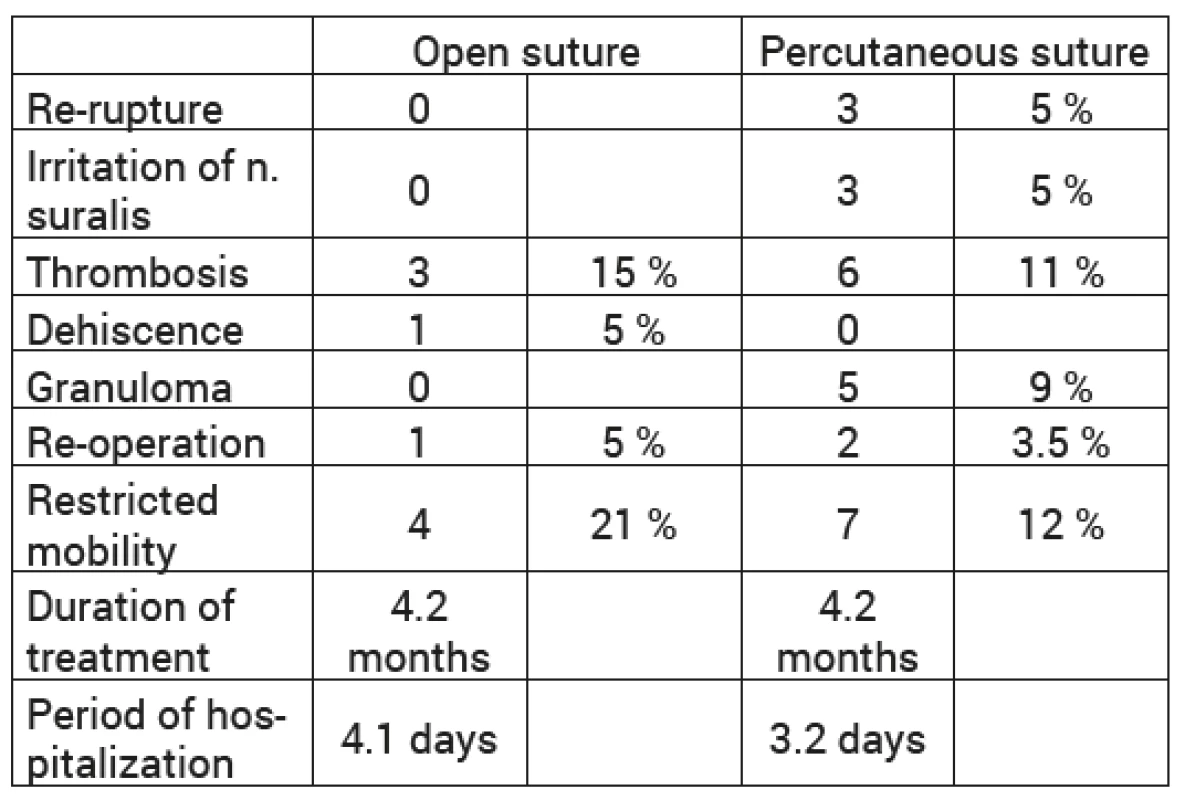
Results: Mean threatment time didn’t differ in both groups (4,2 months). Full range of motion wasn’t achieved in 4 patients (21 ) threated by open suture and in 7 patients (12 ) threated by percutaneous suture. There were 3 cases (5 ) of tendon rerupture and 3 cases (5 ) of n. suralis irritation in CLOSE group. Deep vein thrombosis occured in 3 patients (15 ) operated classicaly and in 6 patients (11 ) operated miniinvasively. There was 1 case of wound breakdown due to infection in the OPEN group. The formation of wound granuloma with fistula was whitnessed in 5 patients (9 ) of the CLOSE group. The results of threatment were evaluated by patients as excellent in 9 , good in 27 , fair in 18 and poor in 46 in the OPEN group. Pacients threated by percutaneous suture achieved excellent result in 15 , good in 30 , fair in 37 and poor in 18
Conclusion: Percutaneous Achilles tendon suture is a comparable method to the classical open suture. The miniinvasivity brings lower rate of wound infection and better physiotherapy results. Furthermore it’s generally better tolerated by patients.
Keywords:
Achilles tendon – rupture – surgical treatment – percutaneus suture – miniinvasive
Introduction
The Achilles tendon is the largest and strongest tendon in the human body. Injuries of the same occur relatively frequently and opinions on treatment are not uniform [11]. Rupture occurs in completely healthy tendons only exceptionally, more often as a result of tendon degeneration after repeated microtrauma [5]. For example, the use of corticoids, either locally in the form of puncture or systemically contribute to deteriorating of the condition [8,10,12]. The use of fluoroquinolones causes the formation of intra-tendon irregular calcifications that increase the risk of rupture [6,15]. Some systemic diseases also have been found to cause an increased incidence of Achilles tendon rupture - such as diabetes mellitus, renal disease, hyperuricemia, rheumatoid arthritis, asthma, TB, systemic lupus erythematosus [1, 2, 3]. The weakened tendon then tears after a single overload. The injury occurs during intense contraction of triceps during take-offs and starts during running, walking on stairs, etc. Strong pain with a bursting feeling, sometimes an acoustic phenomenon, is very conspicuous. This injury often occurs in recreational athletes, more often men aged 40–50, returning to former sporting activity after a longer period of rest [13]. The tendon is most often torn at 2–6 m proximal to the insertion of tuber calcanei [7, 14]. It is an area of relative hypovascularity of the tendon [4].
Aim of the thesis
The aim of this work was to evaluate the results of surgical treatment of Achilles tendon injury. We compared two surgical techniques: a suture technique from an open approach to a percutaneous suture from a mini-invasive approach. We were interested in which of these methods has lower risk of complications, requires a shorter rehabilitation period, leaves less permanent consequences and last but not least, which is better evaluated by patients.
Type of thesis
This is a retrospective, comparative, randomized study.
Material
In the period from 1/1/2011 to 31/12/2013 we treated 82 patients with Achilles tendon injury in our clinical facility. We selected 73 patients in the study. These patients met the study enrollment requirement, which is the recent tendon rupture with a defect 2–6 m from the calcaneus. 63 men (85 ) and 10 women (15 ) were included in the cohort to be monitored. The age range of patients was 24–81 years with an average of 48 years of age.
Methodology
The Achilles tendon rupture was diagnosed on the basis of a clinical examination. In all patients the tendon was painful, there was a palpable tendon defect and Thompson‘s test was positive. All patients were indicated for surgical therapy and surgery was performed in all patients using one of the following two methods. The first group of patients was operated by the conventional open method. Achilles tendon was accessed by longitudinal dorsal or paramedial approach. The tendon was visualized and its suture was performed using Bunnell method under visual inspection. 19 (26 ) patients were operated on by this method. The second group of patients was operated on minimally invasively. This method was first described by Ma and Griffith in 1977 [9], it was modified by Trč and Pacovský in 1996 [16]. We approached the tendon with 8 miniincisions along both ends of the broken tendon. Then, the Bunnell suture of the tendon was performed using these procedures. A total of 54 (74 ) patients were operated on by this method. A total of 10 physicians performed the surgery. 7 of them performed only the percutaneous tendon suture and 3 only the open suture. A specific operator was assigned randomly to the patient. Patients in whom the surgical method was chosen on the basis of the clinical picture (e.g. invetered rupture, avulsive calcaneus fractures, large defect not suitable for percutaneous suture, etc. were excluded from the study (9 patients).
In both surgical groups, the tendon was subsequently fixed with gypsum fixation for 3 weeks in extension and then for 3 weeks in physiological position. The second fixation option was the VacoAchil vacuum brace system. The selection of postoperative fixation was chosen randomly – according to the preferences of a particular patient. The ratio of gypsum fixations and vacuum brace fixation was 35 : 38. All patients applied low molecular weight heparin to prevent thromboembolic disease. The patients were completely weight and load free for the operated limb for a period of 3 weeks, after which the limb was gradually loaded. After the fixation was removed, rehabilitation – therapeutic physical education, diadynamic (DD) currents and hydrotherapy in a series of ten followed. We performed regular postoperative checkups at the traumatology clinic. Data collection for the study was performed retrospectively from the outpatient reports and then sent by questionnaire.
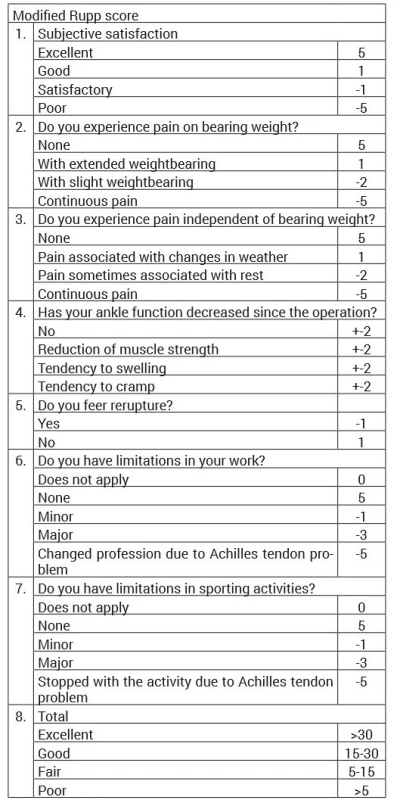
The results of the treatment were evaluated within 6–12 months after the surgery. We evaluated objective results such as mobility limitation, rerupture or thrombosis-type complications. We were also interested in subjective evaluation of patients, so the patients completed a questionnaire study to evaluate Rupp‘s score. The questionnaire contains 7 questions: Are you satisfied with the outcome of the surgery? Do you feel pain during exercise? Do you feel pain at rest? Has the ankle function impaired after surgery? Are you afraid of it breaking again? Are you limited by the injury at work? Are you limited in sports? For each of these questions, there are several answers in the questionnaire to which the corresponding score is assigned. After totaling the score we obtain the result – the so-called Rupp‘s score. According to the score established in patients, we could achieve an excellent result (more than 30 points), a good result (15–30 points), a decent result (5–15 points) or a bad result (below 5 points). 54 patients (73 ) completed the questionnaire.
Results
The average treatment period was the same in both surgical groups (4.2 months), although the average hospitalization period was 1 day longer (4.1d versus 3.2d) in patients operated using conventional procedure. In both groups, an average of 23 individual rehabilitations were needed to achieve functional recovery.
The full mobility could not be achieved in 4 patients (21 ) operated conventionally and 7 patients (12 ) operated in closed manner. In these patients, a certain degree of mobility limitation remained as a permanent consequence of the injury.
There was no re-ruptured tendon observed in any of the patients treated conventionally. In 3 patients (5 ) operated with minimally invasive procedure, the tendon re-ruptured. In all cases, this happened as a result of a severe stepping down in the early post-operative period and was therefore a result of a non-compliance with the therapeutic guidelines. In 2 patients (3.2 %), it was a partial rupture according to ultrasound with the selected conservative treatment, in 1 patient (1.8 ) the re-rupture required reoperation.
Symptoms of n. suralis irritation was observed in 3 patients (5 ) operated on with minimally invasive procedure. One case (1.8 ) requested a neurosurgical revision – there was evidence of nerve entrapment by stitching. In 2 cases, the complaints resolved spontaneously under conservative treatment. There was no nerve injury observed in the conventionally operated group.
Despite the pharmacological TEN prevention, deep venous thrombosis occurred in 3 patients (15 ) operated on conventionally and 6 patients (11 ) operated on percutaneously.
An infectious complication with wound dehiscence occurred in one patient operated on conventionally (5 %). This complication required several reoperations and subsequent plasty. We did not notice a similar complication in percutaneously operated patients. In 5 patients (9 ) operated on in closed procedure, granuloma and stitch fistulae occurred at the site of the stich. In all cases, the granuloma was in one of the distal wounds. The solution was the ambulatory excision of the nodule, which was healed in all cases (Tab. 1).
These objective results were supplemented by a questionnaire study in which the patients evaluated their satisfaction with the surgery. The patients operated conventionally rated the result as excellent (Rupp score above 30 point) in 9 as good (15–30 points) in 27 as decent (5–15 points) in 18 and bad (below 5 points) in 46 . In percutaneous suture we achieved an excellent result in 15 , a good result in 30 , a decent result in 37 and a bad one in 18 of patients (Tab. 2).
Tab. 2. Subjective assessment – Rupp score 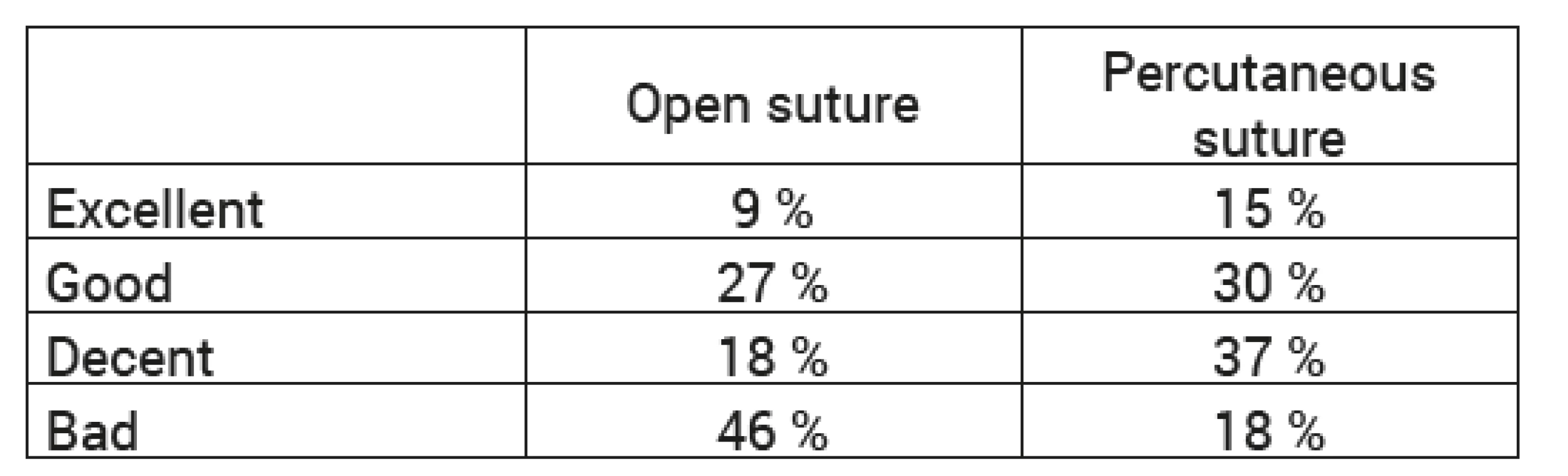
Discussion
The results show that both methods are comparable in terms of length of treatment and length of rehabilitation needed. If we use the mini-invasive method, we will reduce the hospital stay period by 1 day. Certain differences can also be traced in the incidence of complications.
Re-rupture occurred only in patients operated on percutaneously (5 %). This is explained by the nature of the suture itself. Percutaneously performed suture is only adaptive and certainly does not reach such strength as the open suture, therefore it is more prone to failure. As a result of using this method, it is important to adhere to post-operative relief.
The proven injury of n.suralis also occurred only in the patient operated on using minimally invasive method (1.8 %). The reason is the lack of visualization resulting from the minimal approach. This complication can be avoided by knowing the course of the nerve and adapting to the position of the access points.
An onset of granuloma was also found in percutaneously operated patients (9 %). In all cases, this was due to an incorrectly chosen stitching site - in the distal wound. However, this complication did not result in a prolonged treatment for the patient and was resolved by a simple outpatient procedure.
On the other hand, a wound infection with dehiscence was only observed in a patient operated on conventionally (5 %). In this case, 2 follow-up reoperations and a wound defect plasty were necessary. This complication significantly prolonged the patient‘s treatment period.
The risk of developing thrombosis was higher in conventionally operated patients (15 ) compared to the percutaneous group (9 ) despite the same type of fixation and adherence to the same TEN prevention procedure.
Permanent consequences in terms of restricted mobility are more likely to occur after using the conventional method (21 vs. 12 %).
Another significant difference was observed in the results of the questionnaire survey. The subjective evaluation of patients is better after using the percutaneous method. An excellent result was achieved in 15 of patients and a poor result in 18 , while using the conventional method an excellent result was achieved in 9 of patients and a poor result in 46 of patients.
Conclusion
The percutaneous suture of the Achilles tendon is a relatively recent procedure and, as such, still raises a number of unanswered questions. There has not yet been a clear consensus on how to use this method, and opinions on the same are changing from one facility to another. With our study, we wanted to share the experience that we have with using this procedure.
The results of the study are unexpectedly contradictory in some aspects, but highlight the benefits of this surgical procedure.
Percutaneous suture in our study had objectively more complications than the open one. Most of these complications have been explained by improper surgical techniques, or by the patient‘s failure to follow the treatment procedure (especially exercise). Here it was clear that it is a new method and more experience is needed to master it. However, these are avoidable complications and can be prevented by consistent erudition of surgeons and good communication with the patient. With this in mind, it could be said that this is a method comparable to the conventional open suture.
On the other hand, its mini-invasiveness brings us many advantages that are missing in the open method. The surgical access from miniature incisions ensures better healing with lower risk of infection. Less tissue scarring, in turn, improves rehabilitation results. These are the main reasons why it is also much better perceived by patients than the conventional approach. According to the questionnaire survey, percutaneous suture in patients causes much less subjective complaints and is therefore preferable by the patients over conventional suture.
MUDr. Dávid Fekete
Zdroje
1. Aydin, S. et al. A rare case of spontaneous, bilateral Achilles tendon rupture in systemic lupus erythematosus and review of the literature. Lupus. 2008, 17, 1051–1052. ISSN 1477-0962
2. Basic-Jukic, N. et al. Spontaneous tendon ruputres in patients with end-stage renal disease. Kidnesy Blood Press Res. 2009, 32, 32–36. ISSN 1420-4096
3. Benthien, JP, Delling, G., Ruther, W. Spontaneous Achilles tendon rupture in granulomatou vasculitis. Z Rheumatol. 2003, 62, 402–405. ISSN 0172-8172
4. Chen, TM. et al. The arterial anatomy of the Achilles tendon: anatomical study and clinical implications. Clin Anat. 2009, 22, 377–385. DOI: 10.1002/ca.23378
5. Davidsson, L., Salo M. Pathogenesis of subcutaneous tendon ruptures. Acta Chir Scand.1969, 13, 209–212. ISSN 0001-5482
6. De La Red, G. et al. Bilateral Achilles tendinitis with spontaneous rupture induced by levofloxacin in a patient with systemic sclerosis. Clin Rheumatol. 2003, 22, 367–368. ISSN 0172-8172
7. De Vos RJ, et al. The value of power Doppler ultrasonography in Achilles tendinopathy: a prospective study. Am J Sports Med. 2007, 35, 1696–1701. ISSN 0363-5465
8. Hamilton, B. et al. Achilles tendon rupture in an elite athlete following multiple injection therapies. J Sci Med Sport. 2008, 11, 566–568. ISSN 1440-2440
9. Ma, GW, Griffith, TG. Percutaneous repair of acute closed ruptured achilles tendon: a new technique. Clin Orthop Relat Res. 1977, 128, 247–255. ISSN 1528-1132
10. Magnussen, RA, Dunn, WR, Thompson, AB. Nonoperative treatment of midportion Achilles tendinopathy: a systemic review. Clin J Sport Med. 2009, 19, 54–65. ISSN 1050-642X
11. McGlamr, y. et al. Comprehensive textbook of foot and ankle surgery. 4. vyd. Philadelpha: Wolters Kluwer, 2013, 2078. ISBN 0781765803
12. McQuillan, R., Gregan, P. Tendon rupture as a complication of corticosteroid therapy. Palliat Med. 2005, 19, 352–353. ISSN 0269-2163
13. Pokorný, V. et al. Traumatologie. Praha : Triton, 2002. 307. ISBN 80-7254-277-X.
14. Saxena, A., Bareither, D. Magnetic resonance and cadaveric findings of the „watershed band“ of the Achilles tendon. J Foot Ankle Surg. 2001, 40, 132–136. ISSN 2405-4569
15. Sugimoto, T. et al. Levofloxacin-induced Achilles tendon rupture in a patient with systemic microscopic polyangiitis. Mod Rheumatol. 2005, 15, 217–219. ISSN 1439-7595
16. Trč, T., Pacovský, V. Perkutánní sutura Achillovy šlachy: předběžné sdělení a první zkušenosti. Acta chir Orthop Traum Čech. 1996, 63, 206–210. ISSN 0001-5415
Štítky
Chirurgie všeobecná Traumatologie Urgentní medicína
Článek vyšel v časopiseÚrazová chirurgie
Nejčtenější tento týden
2018 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
- Stillova choroba: vzácné a závažné systémové onemocnění
- Hojení análních fisur urychlí čípky a gel
- Jak souvisí postcovidový syndrom s poškozením mozku?
-
Všechny články tohoto čísla
- Abdominal trauma and wandering spleen - case report
- Addressing of trochanteric femoral fractures using a revision femoral stem with a cervicocapital prosthesis – coxofemoral by-pass
- Complex Response of the Organism to Trauma
- Results of Achilles tendon rupture repair. Classical open approach versus percutaneous suture
- Kelly MJ., Holton AE., Cassar-Gheiti AJ., Hanna SA., Quinlan JF., Molony DC.: The aetiology of posterior glenohumeral dislocation and occurrence of associated injuries. A systematic review.
- Úrazová chirurgie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Results of Achilles tendon rupture repair. Classical open approach versus percutaneous suture
- Complex Response of the Organism to Trauma
- Addressing of trochanteric femoral fractures using a revision femoral stem with a cervicocapital prosthesis – coxofemoral by-pass
- Abdominal trauma and wandering spleen - case report
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání