-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Computer-aided modeling and additive manufacturing fabrication of patient-specific mandibular implant
Authors: Mario Sokac; Igor Budak; Dajana Miljanovic; Zeljko Santosi; Djordje Vukelic
Authors place of work: Faculty of Technical Sciences, University of Novi Sad, Novi Sad, Serbia
Published in the journal: Lékař a technika - Clinician and Technology No. 4, 2018, 48, 113-117
Category: Original research
Summary
With the recent advances in computer-aided technologies and their breach into the medical field, there can be seen more and more successful outcomes, especially in the files of reconstructive prosthetic surgery. With the application of advanced tools for reconstruction of complex shape such as human anatomy, it allowed accurate and fast design of complex implants as a substitution for deformed or damaged regions in the field of maxillofacial surgery. Design, in compliance with application of additive manufacturing (AM) technologies, is starting to gain more recognition as a tool for fast and accurate delivery of patient-specific 3D implants. This paper present a case study where such 3D technologies are used to design and fabricate a patient-specific mandibular implant. Tools for design of complex anatomical surfaces, such as mandible are presented and demonstrated in this paper. As the verification stage, AM technologies are used for visual inspection and surgical procedure planning of the designed 3D model of the mandibular implant.
Keywords:
computer-aided modeling – design – mandibular implant – additive manufacturing (AM) technologies
Introduction
Different types of trauma concerning damaged or completely lost organs or tissues are mostly related to different types of diseased and benign or malignant tumors. As such, they present one of the biggest health problems in the world today and affect a large number of people [1]. In order to face those problems, and with the advancements of three-dimensional (3D) technol-ogies and their implementation in the medical field, a new era of computer-aided implants has emerged. Implants present medical devices designed to replace the missing biological structure, to play the role of the backbone of the damaged structure, or to improve the already existing biological structure. For many years, implants have been used in medicine, and thanks to the technologies of reverse engineering (RE) design and additive manufacturing (AM) technologies, their appli-cation has been raised to a higher level. In order to be able to use the medical implants up to their full capabilities, they are being made out of biocompatible materials, and thus are able to replicate the role of the missing structure inside the patient. Today, titanium alloys are commonly used as a material for fabrication of temporary or permanent implants [1]. Permanent implants are replacing parts of the body and should perform their function throughout the life of the patient [2].
Defects of the lower jaw (mandible), caused by tumors, injuries or infections, can lead to serious deformities or difficulties in chewing food. Such defects significantly affects the quality of life of patients where speech impairment and facial aesthetics are often severely compromised [3]. Mandibular reconstruction represents a major challenge, from both the engineering and medical aspect. From a medical aspect it poses a challenge for a number of reasons, such as compli-cated geometry of the mandible or muscles attached to the mandible which act in different directions, form and position [4]. Various materials and bone grafts have been used in surgery so far and had different outcomes [3]. However, using conventional methods, it is difficult to achieve satisfactory results, both aesthetically and in a functional sense. And with the fast growing implemen-tation of 3D tools in the medical field, such challenges are reduced and further improvements have been made [2, 4–6]. Many authors have dealt with design and fabrication of different types of implants over the years, where several factors were investigated and one of them is accuracy of such designed and fabricated implants and its impact on the manufactured implant [7]. Other authors based their design on mirror-based reconstruc-tion [8], or by application of engineering software for parametric modeling of implants [9].
Anatomical structures present a major challenge to replicate due to their complexity regarding their shape and role inside the human body. Given the geometric complexity of human anatomy, application of advanced 3D tools for RE design, represents a very important tool in the fields of medicine and dentistry, both for diagnostic and reparative, as well as for therapeutic purposes [10]. The 3D CAD (computer-aided design) model has become very important in biomedical engineering, and with the help of computer aided manufacturing (CAM)/AM technologies for production, it is possible to produce physical anatomical models that have diagnostic, therapeutic and rehabilitative medical applications [10]. Using patient or biomedical data to reconstruct 3D models of anatomical structures can contribute to the development of various medical devices, applications and biomedical research. The requirements for the accuracy of the RE design depends on the application of the object itself. For personalized cranio-maxillofacial implants, biomodels and training models, the accuracy does not have to be as high as it should be in industrial reverse engineering [11]. However, for surgical tools and functional implants such as spine, knee or knee implants, the requirements for accuracy are very high [10, 12]. AM has helped to achieve several significant achievements in the field of medicine, especially for fabrication of custom-made implants [4–7, 12–14]. The use of AM has enabled the use of 3D models for making operational plans and simulations, and these 3D models, with great accuracy, represent the anatomy of the patient [5, 7, 10, 12, 13]. Also, AM is used to produce patient-specific implants designed for individual patients in medical fields, such as cranio-maxillofacial surgery [12] or oral surgery for production of bone grafts [15]. Although these AM technologies have been in existence for several decades, they have been implemented more intensively over the last decade in the field of biomedical engineering [5, 7, 10, 12].
This paper presents a case study in which a design solution is proposed for the reconstruction of the mandibular defect.
Methods
The development of a patient-specific implant for the maxillofacial defect is based on 3D model reconstruc-tion in 3D-DOCTOR software from medical 3D image dataset, as well as parametric modeling of mandibular implant in Solidworks software. Using the Wanhao Duplicator i3 plus 3D printer, an implant prototype is provided, which will serve to analyze its functionality, but also to plan surgical procedure.
The first step in the development of mandibular implant is the 3D reconstruction of defect area, ie. the mandible. Computed tomography (CT) images in DICOM (Digital imaging and communications in medicine) images are obtained and 3D model was reconstructed. The most crucial step in this process is to accurately segment the mandible. The segmentation was performed only on predefined 2D slices (15–152), and the reason for this is that the mandible was located within this range of 2D slices. When all 250 slides were segmented, the generated 3D model would consist of large number of polygons that would prolong recon-struction time, but also make it more difficult for further work and manipulation with the 3D model. The segmentation parameters that were used for acquisition of surface 3D model were: minimum pixel intensity 1458, and the maximum 4096.
The reconstructed 3D model of the mandible is shown in Figure 1a, while extracted 3D model of the mandibular defect is shown in Figure 1b. After its reconstruction it was exported in binary STL format for the next step, which is design of the mandibular implant.
Fig. 1. Showing a) reconstructed surface 3D model of the mandible and b) extracted 3D model of the mandibular defect. 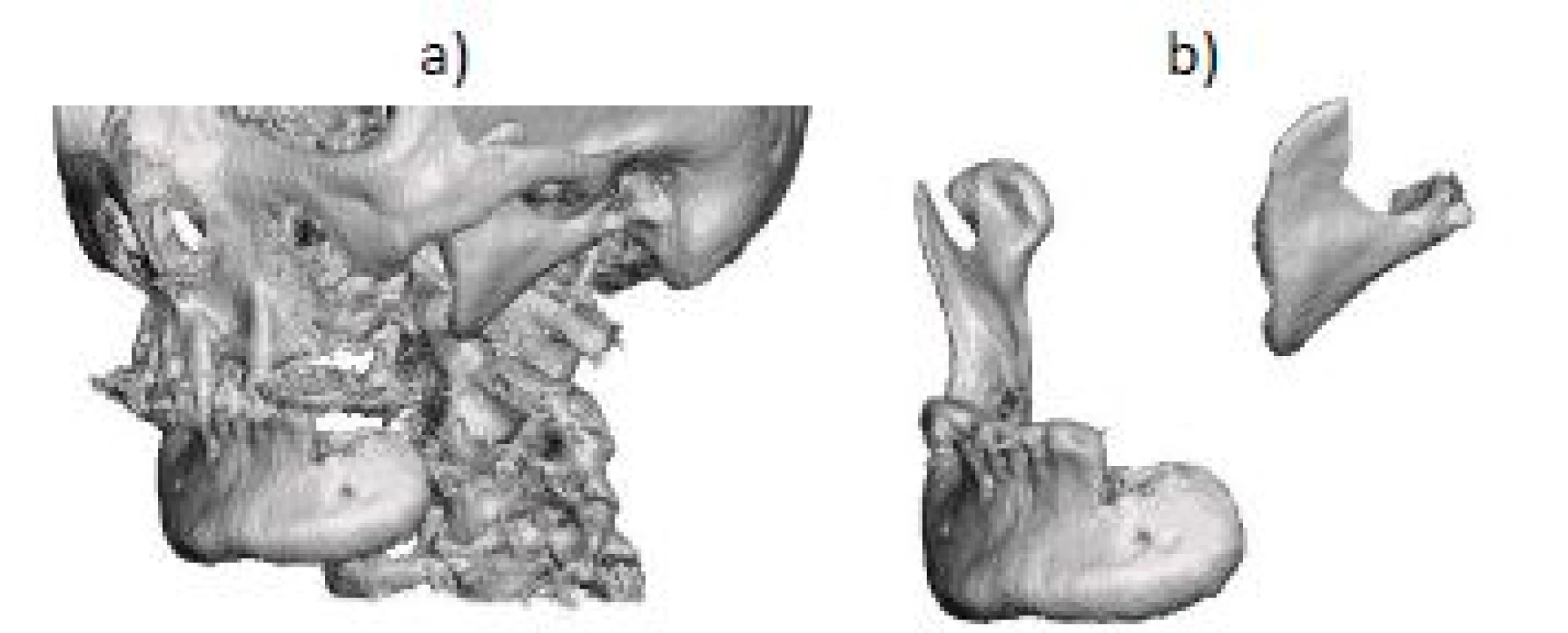
After reconstruction of the 3D model the next step presents the computer-aided modeling of the appropriate implant. Before the modeling first step was to copy the healthy part of the mandible to the defect side by using mirror-based reconstruction approach (Figure 2). This step enabled a guidance during modeling of the mandi-bular implant, in order to achieve high level of facial symmetry.
Fig. 2. Mirror-based reconstruction approach for the design of the mandibular implant. 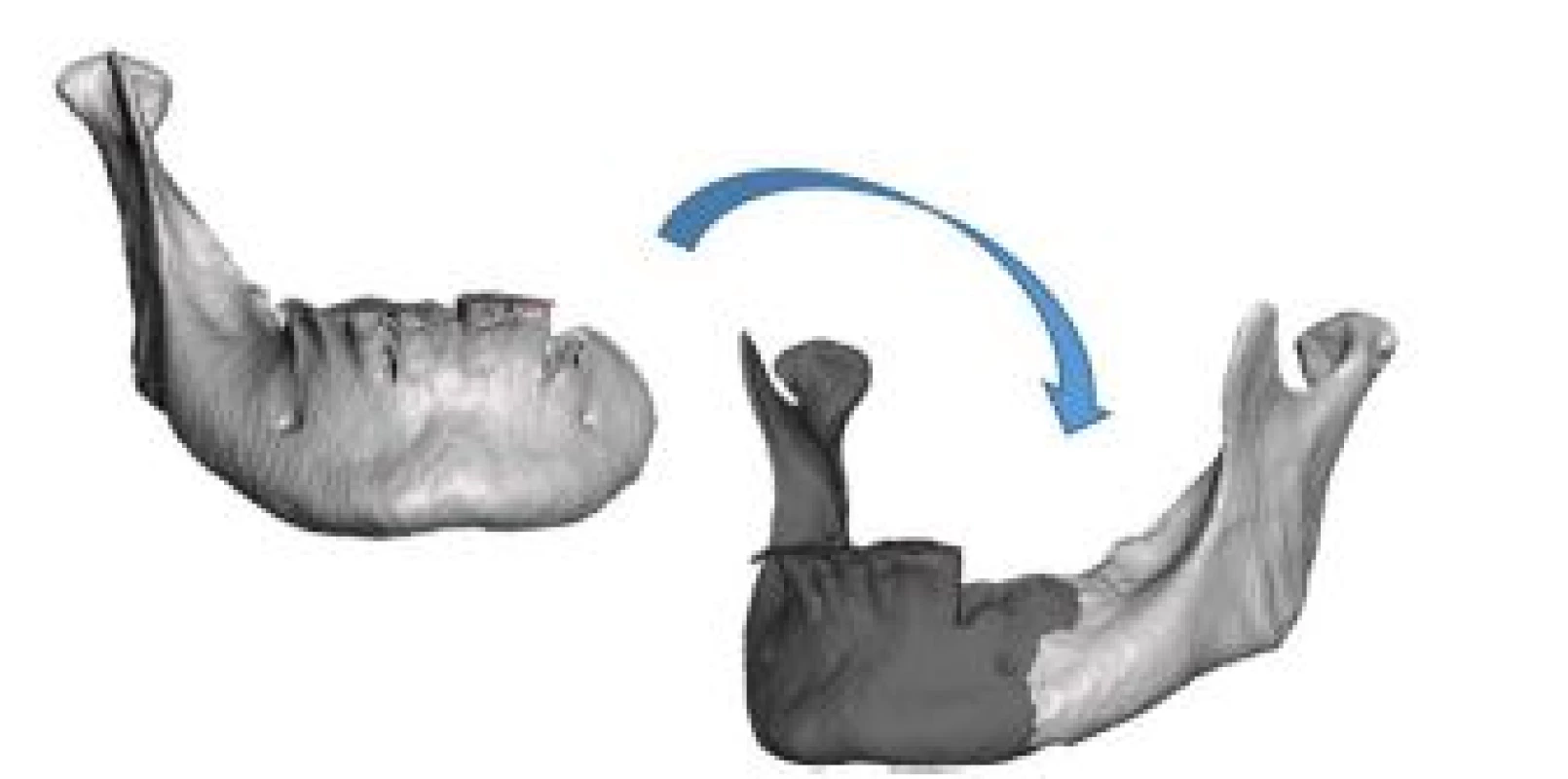
After the initial mirroring of the healthy side of the mandible that will be used for guidance, modeling of mandibular defect can start (Figure 3a). In order to model the outer bonds of the mandibular implants, 3D curves were used as a guidance for the newly designed implant (Figure 3b). These 3D curves enabled the initial contour (or shell) of the implant to be made. From there on the outer surface of the implant was created (Figure 3c). This enabled engineers to reconstruct the initial shape of the implant, which follows the original trace of the other mirrored side of the mandible. The surface was then extended on the lower side by 1 mm in order to fill in the gap present there, but also to align the outer surface with the initially mirrored half.
Fig. 3. Design process of the mandibular implant a) initial mirror, b) guidance 3D curves and c) outer surface of the mandibular implant. 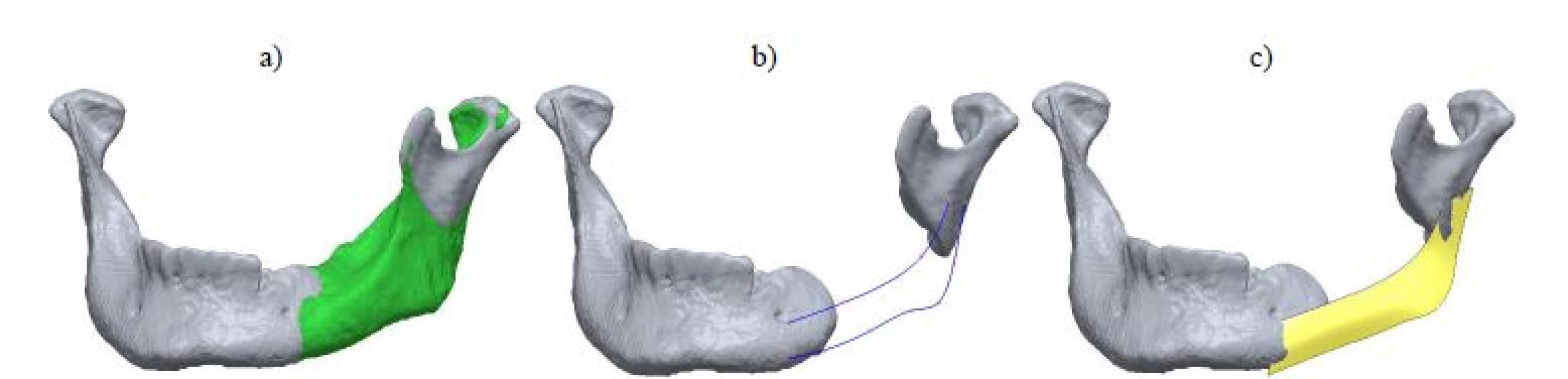
From here the initial surface was thickened to a value of 1 mm and then hollowed by a 1-mm thickness (Figure 4a) and the required extensions were made that will support fixation of the implant to the mandible, as well as to the temporomandibular joint (TMJ) (Figure 4b). From there on, in order to reduce the weight of the structure, fifteen perforated holes of 1 mm in diameter on the outside and six 1-mm holes on the top side of the implant were added (Figure 4c) along with some final improvements, especially to the edges of the implant, as they remained very sharp.
Fig. 4. Modeling procedure of the mandibular implant showing a) hollowed shell by 1mm thickness, b) fixation support, c) perforated mandibular implant and d) mounted implant on the reconstruction site, fixed with 4 titanium screws. 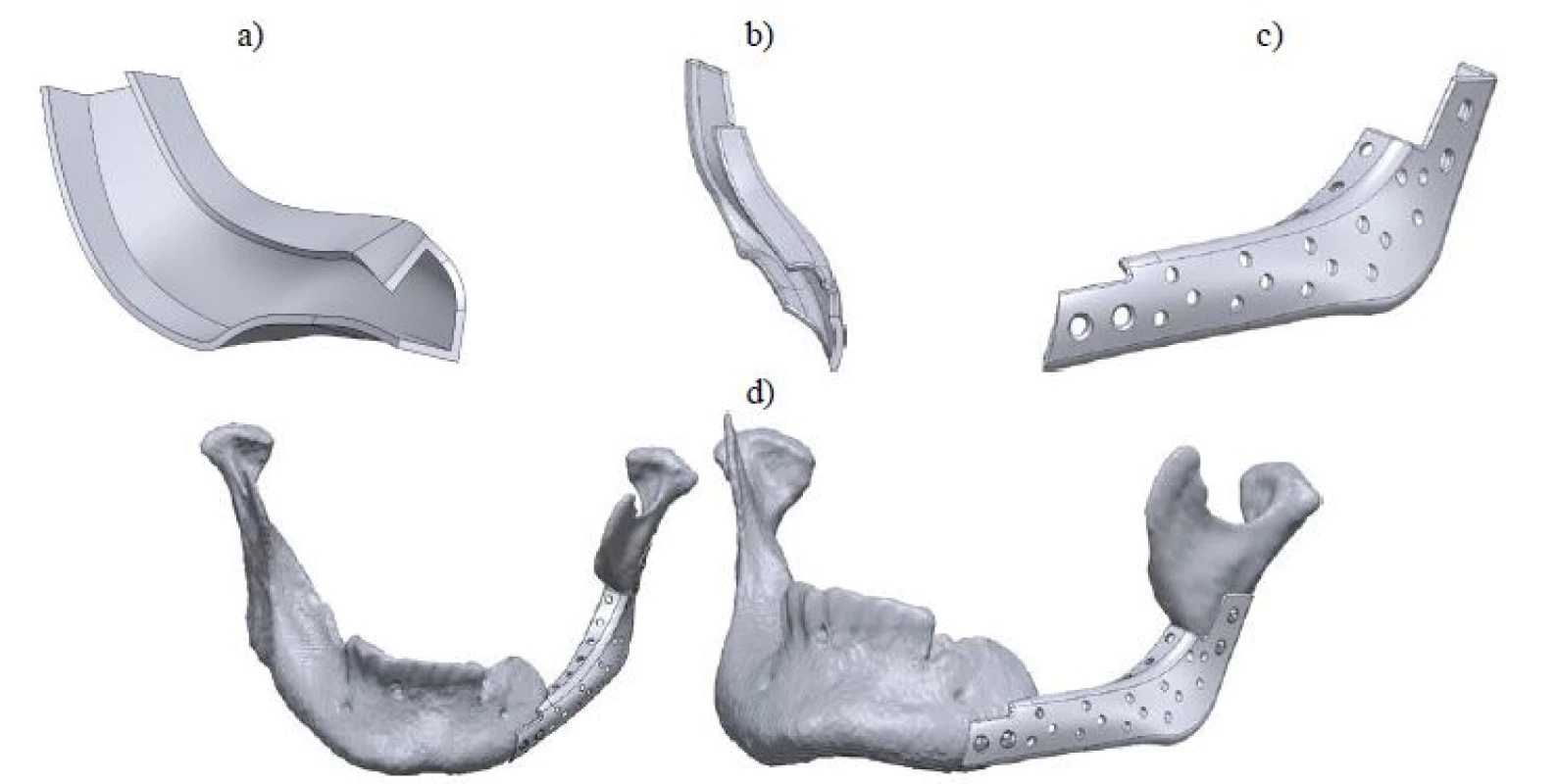
This initial version of the mandibular implant was also verified by the surgeon in order for it to comply with the required pre-conditions for successful surgical procedure.
Fabrication of mandibular implant
3D printing is a method that uses 3D CAD data to produce 3D physical models. The principle of 3D printing is the use of 3D computer models for the reconstruction of the 3D physical model by adding layers of materials. With the additive fabrication, the machine reads data from the CAD model and successively adds layers of material, and in this way forms the physical model. The layers created make the final shape of the physical model. The main advantage of the additive fabrication is the ability to create almost every complex form [12]. After the development of the implant, FDM 3D printer equipped with polylactic acid (PLA) filament was used. The specifications of the 3D printer are shown in Table 1.
Tab. 1. Technical characteristics of FDM printer. 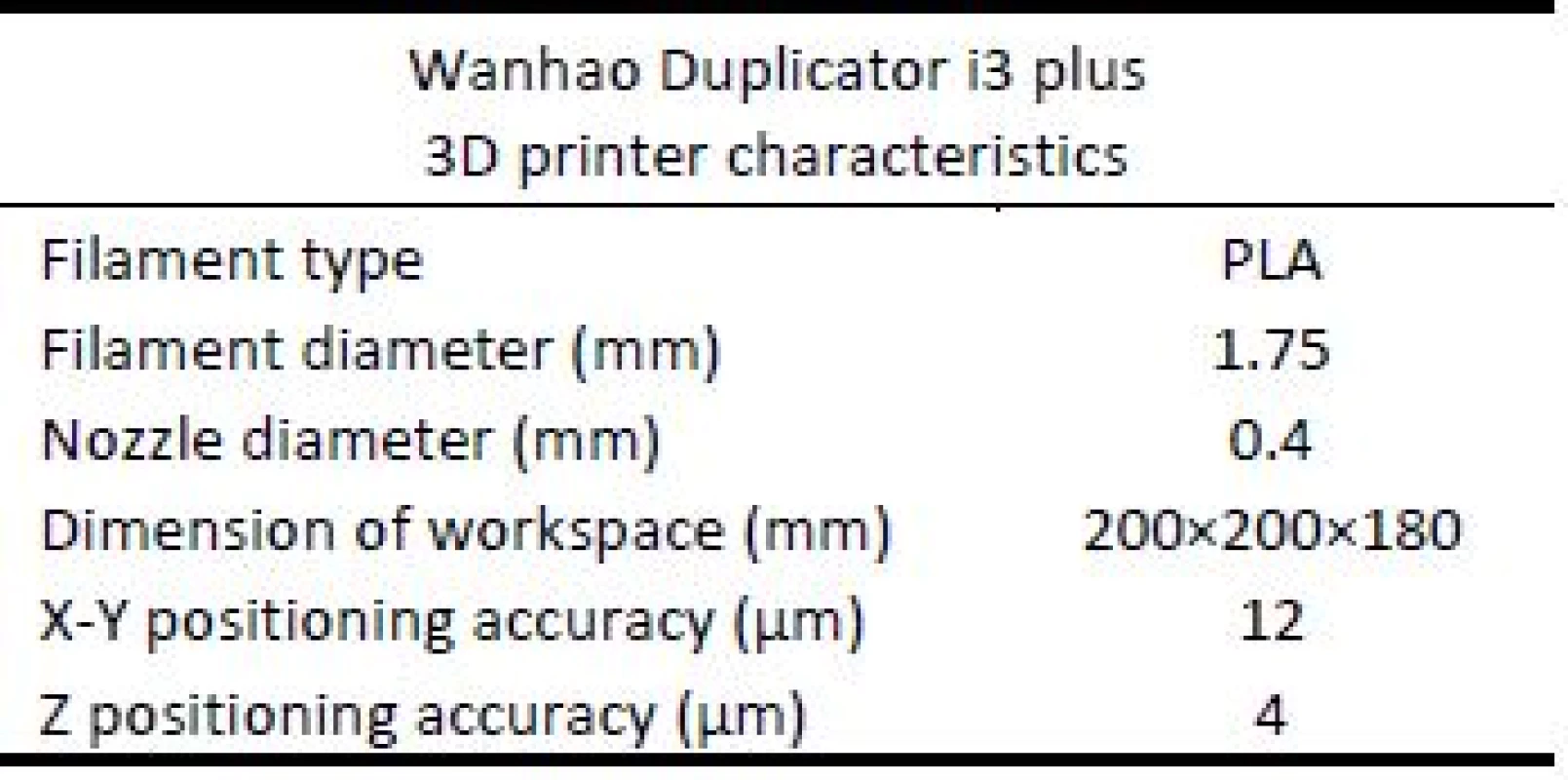
Results
Figure 5a shows the printed model of the mandibular implant on Wanhao duplicator i3 plus. After 3D printing, a mandibular implant was fixed on the patient’s mandible by total of 4 screws, two on the mandible, and two on the TMJ in order to position and fix the implant (Figure 5b).
Fig. 5. 3D Printed models of a) mandibular implant and b) mandibular implant positioned and fixed on the mandible and TMJ. 
Conclusion
This paper presents the application of RE design as well as AM technologies in the field of biomedical engineering. In this regard, a case study was realized in which the process of reconstruction of the 3D model of the mandible, as well as the design of the mandibular implant for reparation of defect was presented.
The presented results confirm that the application of RE and AM technologies are becoming indispensable in the field of biomedical engineering for development of modern medical implants. Obtained results indicate that 3D-DOCTOR and Solidworks present adequate tools that provide satisfactory results when modeling a 3D model of customized mandibular implant for 3D printing. Also, based on the printed 3D model of the mandible and the mandibular implant, it can be concluded that the presented approach provides a good way for the application of these 3D technologies, and that the applied 3D printer is adequate for this application and for further analysis of the mandibular reconstruction and surgical planning.
Acknowledgement
This paper presents the results achieved in the framework of the Project no. 114-451-2723/2016-03 funded by the Provincial Secretariat for Higher Education and Scientific Research, and within the project TR - 35020, funded by the Ministry of Education, Science and Technological Development of Republic of Serbia.
Mario Sokac, MSc
Department of Production Engineering
Faculty of Technical Sciences
University of Novi Sad
Trg Dositeja Obradovica 6, Novi Sad
E-mail: marios@uns.ac.rs
Phone: +381 21 485 2332
Zdroje
[1] Pacifici, L., De Angelis, F., Orefici, A., Cielo, A.: Metals used in maxillofacial surgery. Oral and Implantology, 2016, vol. 9, no. 2, pp. 107–111.
[2] Zhou, L., Shang, H., He, L., Bo, B., Liu, G. Liu, J., Zhao, J.: Accurate reconstruction of discontinuous mandible using a reverse engineering/computer-aided design/rapid prototyping technique: A pre-liminary clinical study. Journal of Oral and Maxillofacial Surgery, 2010, vol. 68, no. 9, pp. 2115–2121.
[3] Goh, B. T., Lee, S., Tideman, H., Stoelinga, P. J. W.: Mandibular reconstruction in adults: a review. International Journal of Oral and Maxillofacial Surgery, 2008, vol. 37, no. 7, pp. 597–605.
[4] Cohen, A., Laviv, A., Berman, P., Nashef, R., Abu-Tair, J.: Mandibular reconstruction using stereo-lithographic 3-dimensional printing modeling technology. Oral Surgery, Oral Medicine, Oral Pa-thology, Oral Radiology and Endodontology, 2009, vol. 108, no. 5, pp. 661–666.
[5] Stoor, P., Suomalainen, A., Mesimäki, K., Kontio, R.: Rapid prototyped patient specific guiding implants in critical mandibular reconstruction. Journal of Cranio-Maxillofacial Surgery, 2017, vol. 45, no. 1, pp. 63–70.
[6] Schwaiger, M., Wallner, J., Pau, M., Feichtinger, M., Zrnc, T., Zemann, W., Metzler, P.: Clinical experi-ence with a novel structure designed bridging plate system for segmental mandibular reconstruction: The TriLock bridging plate. Journal of Cranio-Maxillofacial Surgery, 2018, vol. 46, no. 9, pp. 1679–1690.
[7] Naros, A., Weise, H., Tilsen, F., Hoefert, S., Naros, G., Krimmel, M., Reinert, S., Polligkeit, J.: Three-dimensional accuracy of mandibular reconstruction by patient-specific pre-bent reconstruction plates using an ‘in-house’ 3D-printer. Journal of Cranio-Maxillofacial Surgery, 2018, vol. 46, no. 9, pp. 1645–1651.
[8] Singare, S., Lian, Q., Wang, W., Wang, J., Liu, Y., Li, D., Li, B.: Rapid prototyping assisted surgery planning and custom implant design. Rapid Prototyping Journal, 2009, vol. 15, no. 1, pp. 19–23.
[9] Nasr, E. A., Al-Ahmari, A., Kamrani, A., Moiduddin, K.: Digital design and fabrication of customized mandible implant. World Automation Congress Proceedings, 2014, pp. 1–6.
[10] Parthasarathy, J.: 3D modeling, custom implants and its future perspectives in craniofacial surgery. Annals of Maxillofacial Surgery, 2014, vol. 4, no. 1, pp. 9–18.
[11] Deeb, G., Allen, R., Hall, V., Whitley, D., Laskin, D., Bencharit, S.: How Accurate Are Implant Surgical Guides Produced With Desktop Stereo-lithographic 3-Dimentional Printers?. Journal of Oral and Maxillofacial Surgery, 2017, vol. 75, no. 12, p. 2559.e1-2559.e8.
[12] Salmi, M., Paloheimo, K., Tuomi, J., Wolff, J., Mäkitie, A.: Accuracy of medical models made by additive manufacturing (rapid manufacturing). Journal of Cranio-Maxillofacial Surgery, 2013, vol. 41, no. 7, pp. 603–609.
[13] Budak, I., Mirkovic, S., Sokac, M., Santosi, Z., Puskar, T., Vukelic, D.: An approach to modelling of personalized bone grafts based on advanced technologies. International Journal of Simulation Modelling, 2016, vol. 15, no. 4, pp. 637–648.
[14] Mirković, S., Budak, I., Puškar, T., Tadić, A., Šokac, M., Santoši, Ž., Djurdjević-Mirković, T.: Application of modern computer-aided technol-ogies in the production of individual bone graft: A case report. Vojnosanitetski Pregled, 2015, vol. 72, no. 12, pp. 1126–1131.
[15] Šokac, M., Budak, I., Mirković, S., Santoši, Ž., Movrin, D., Puškar, T.: The role of advanced 3D technologies and additive manufacturing in designing and manufacturing of customized bone grafts. Journal for Technology of Plasticity, 2017, vol. 42, no. 2, pp. 33–44
Štítky
Biomedicína
Článek Nanofiber scent carrier
Článek vyšel v časopiseLékař a technika

2018 Číslo 4-
Všechny články tohoto čísla
- Computer-aided modeling and additive manufacturing fabrication of patient-specific mandibular implant
- Immediate effect of physical on blood flow velocity in radial artery in young adults
- Nanofiber scent carrier
- NANOFIBERS FROM POLYVINYL ALCOHOL AND CAN ENLARGE THE SET OF TRAPPED ODOROLOGICAL TRACES
- GLOBAL CENTERS OF MEDICAL DEVICE TECHNOLOGY: UNITED STATES, EUROPE AND CHINA
- Lékař a technika
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- GLOBAL CENTERS OF MEDICAL DEVICE TECHNOLOGY: UNITED STATES, EUROPE AND CHINA
- Computer-aided modeling and additive manufacturing fabrication of patient-specific mandibular implant
- Nanofiber scent carrier
- Immediate effect of physical on blood flow velocity in radial artery in young adults
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání




