-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaProgression of diabetes, heart disease, and stroke multimorbidity in middle-aged women: A 20-year cohort study
Using data from the Australian Longitudinal Study on Women’s Health, Xiaolin Xu and colleagues examine the progression of diabetes, heart disease, and stroke co - and multimorbidity in middle-aged women over 20 years.
Published in the journal: . PLoS Med 15(3): e32767. doi:10.1371/journal.pmed.1002516
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1002516Summary
Using data from the Australian Longitudinal Study on Women’s Health, Xiaolin Xu and colleagues examine the progression of diabetes, heart disease, and stroke co - and multimorbidity in middle-aged women over 20 years.
Introduction
The prevalence of diabetes, heart disease, and stroke multimorbidity (co-occurrence of two or three from these conditions) has increased rapidly over the past few decades [1–3], potentially translating to excess morbidity and mortality [4,5]. As the three conditions may interact with each other and be driven by common risk factors through the life course [6,7], the relationships among them are complex.
Diabetes is a well-established risk factor for heart disease and stroke, with a stronger effect in women than in men [8,9]. Although limited, there is evidence that patients with heart disease or stroke may progress to diabetes [10]. However, much less is known about how the three conditions progress from one to another sequentially through the life course [10]. The relationship between common risk factors (e.g., high blood pressure, obesity) and individual conditions has been researched intensively [6,7], but far less is known about the roles of these risk factors in the accumulation of diabetes, heart disease, and stroke multimorbidity from a longitudinal perspective [11].
Understanding the course of diabetes, heart disease, and stroke multimorbidity and related risk factors is essential for developing medical strategies to interrupt the progression from one condition to additional conditions. Considerable evidence has already shown that early intervention with diabetes or common risk factors might have the potential to ameliorate the course or even prevent the onset of cardiovascular disease (CVD) [12–14].
The aims of this article were (a) to investigate the progression of diabetes, heart disease, and stroke multimorbidity in middle-aged women over 20 years of follow-up and (b) to determine the roles of common risk factors in the accumulation of these conditions.
Methods
The Australian Longitudinal Study on Women’s Health (ALSWH) is an ongoing population-based cohort study that aims to investigate factors associated with health and well-being over time. The women were randomly selected from the national database of the Health Insurance Commission, the universal health insurance scheme that includes all citizens and permanent residents of Australia. Details of the study design, recruitment methods, and response rates have been described elsewhere [15,16]. The data analyses for the present study were performed following a prespecified analysis plan (S1 Text). Changes in the analysis plan were also described in S1 Text. This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (S1 Checklist).
Ethics statement
The study was approved by the Human Research Ethics Committees of the Universities of Queensland and Newcastle. All participants signed informed consent, and all data used in the analyses were de-identified.
Participants
This study includes data from women born between 1946 and 1951, also known as the 1946–1951 cohort in ALSWH. A total of 13,714 women aged 45–50 years responded to the first survey in 1996. Response rates to the first mailed survey (baseline) cannot be exactly specified, as some women selected for the sample may not have received the invitation (e.g., if they had died or had changed their address without notifying the Health Insurance Commission). It is estimated that 53%–56% responded to the initial invitation to participate [16]. Self-administered questionnaires were sent to the women every 3 years (apart from a 2-year interval between the first and second surveys) until 2016.
Women who participated in at least two consecutive surveys with relevant information on exposures and outcomes of interest were included in the analysis (see Fig 1). Attrition rates and reasons for dropout at each survey are shown in S1 Table.
Fig. 1. Flow diagram showing the selection of participants. 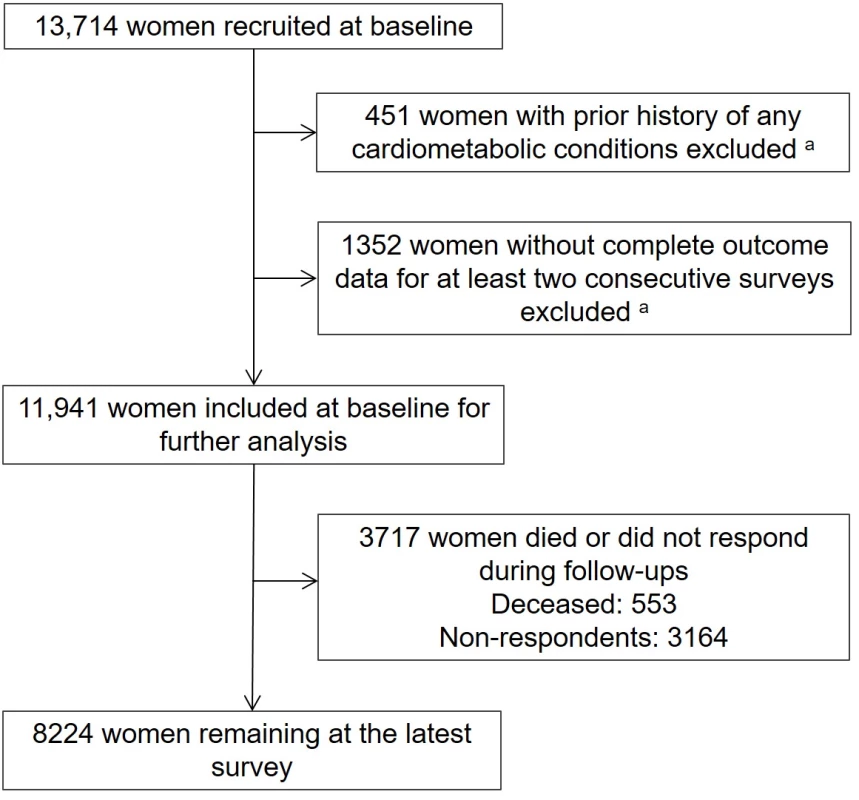
aData for these women in the two boxes may overlap. Outcomes
The main outcomes were the cumulative incidence of diabetes, heart disease, and stroke and accumulation of multimorbidity from these conditions. At each survey, women were asked “Have you ever been told by a doctor that you have diabetes (high blood sugar), heart disease (including heart attack, angina), and stroke over the past 3 years?” The three self-reported conditions were validated with hospital discharge data in a subset of the cohort (women living in New South Wales, Australia). The following International Statistical Classification of Diseases and Related Health Problems-Tenth Revision-Australian Modification (ICD-10-AM) diagnosis codes were used for the validation: diabetes mellitus (E10, E11, E13, and E14), ischemic heart diseases (I20–I25), and stroke (I60–I64). The prevalence and bias-adjusted kappa statistics for the three conditions were 0.93, 0.91, and 0.98, respectively [17].
The incidence of each of the conditions was based on the first report of that condition. Accumulation of multimorbidity was based on the first report of two or three of these conditions and the progression from two to three conditions.
Additionally, we decomposed multimorbidity into 4 unique outcomes that had developed over the 20-year follow-up: diabetes only, CVD only, CVD followed by diabetes, and diabetes followed by CVD [11]. CVD followed by diabetes refers to women with heart disease or stroke who subsequently developed comorbid diabetes. Diabetes followed by CVD refers to women with diabetes who subsequently developed comorbid heart disease or stroke.
Covariates
There were four groups of covariates used in the analysis, and these covariates were collected at each survey unless indicated otherwise. Covariates included are study design variables: age in single years at 1996 (baseline), time period (Surveys 1–8); sociodemographic factors: country of birth, marital status, area of residence, education (at baseline), and ability to manage on income; lifestyle factors: body mass index (BMI), hypertension, physical activity, and smoking; and other chronic conditions: depression/anxiety, cancer, asthma, arthritis, osteoporosis, and chronic obstructive pulmonary disease (COPD). All covariates were time-varying except for country of birth and level of education.
BMI was calculated as weight in kilograms divided by height in meters squared and categorized as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), or obese (≥30 kg/m2), according to the World Health Organization classification [18]. Physical activity was categorized as sedentary (0–39 metabolic equivalent [MET] min/week), low (40–599 MET min/week), moderate (600–1,199 MET min/week), and high (≥1,200 MET min/week) [19].
Statistical analysis
Baseline characteristics were described by the number of conditions from diabetes, heart disease, and stroke developed during the 20-year follow-up. Differences among the groups were examined using analysis of variance (ANOVA) or chi-squared tests. A proportional Venn diagram was drawn to display the number of women with single or overlapping conditions. A Sankey diagram was constructed to characterize the dynamic changes of different combinations of these conditions over time. We estimated the association among the three conditions using repeated measures logistic regression of existing conditions on the incidence of each of the other two conditions, adjusted for age at baseline and time period.
To investigate the longitudinal odds of developing these conditions, we used a repeated measures logistic regression model fitted using generalized estimating equations. We calculated odds ratios (ORs) and 95% confidence intervals (CIs) for incidence one of the three conditions or two or three over each 3-year period, compared to a reference group of women who did not develop any new conditions. We also calculated cumulative incidence of the other two conditions after the first onset of each single condition.
To estimate the associations between predictors (sociodemographic factors, lifestyle factors, and other prior chronic conditions) in the progression of diabetes, heart disease, and stroke multimorbidity, we used a generalized linear mixed model for the multinomial outcome of cumulative incidence of 0, 1, or ≥2 conditions (≥2, including the transition from 2 to 3). We calculated ORs with 95% CIs for the association between the three outcomes at each survey and the risk factors (including time-varying covariates except for education and country of birth) at the previous survey; women with 0 conditions were the reference group. For example, the cumulative incidence of 1 or ≥2 conditions from Surveys 6–7 were modelled using predictors from Survey 6. We also used multinomial logistic regression to investigate the association between the three outcomes and the predictors at baseline (rather than time-varying).
We also used multinomial logistic regression to investigate the association between the predictors at baseline and four unique outcomes that had developed over the 20-year follow-up: diabetes only, CVD only, CVD followed by diabetes, and diabetes followed by CVD [11].
Sensitivity analyses
We conducted sensitivity analyses to check the robustness of our findings. All analyses were rerun using complete case data (i.e., only data from those women who responded to all 8 surveys).
All analyses were performed using SAS (version 9.4, SAS Institute Inc.). All statistical tests were two-sided, and P < 0.05 was considered to be statistically significant.
Results
Characteristics of participants
Of 13,714 women aged 45–50 years at baseline, 3.3% (n = 451) reported a history of any of the three conditions and were excluded. The final analytic sample comprised 11,941 women who provided information at two or more consecutive surveys from 1996 to 2016 (Fig 1).
Descriptive statistics for women at baseline, categorized according to the number of conditions developed during follow-up, are shown in Table 1. Over a follow-up period of 20 years, women who developed multimorbidity were more likely to be separated, divorced, or widowed; to have difficulty in managing on their available income; to be overweight or obese; to have hypertension; to have low levels of physical activity; to be smokers; and to have other chronic conditions (depression/anxiety, asthma, cancer, and arthritis) at baseline.
Tab. 1. Baseline characteristics of women by number of conditions from diabetes, heart disease, and stroke developed during follow-up (N = 11,914). 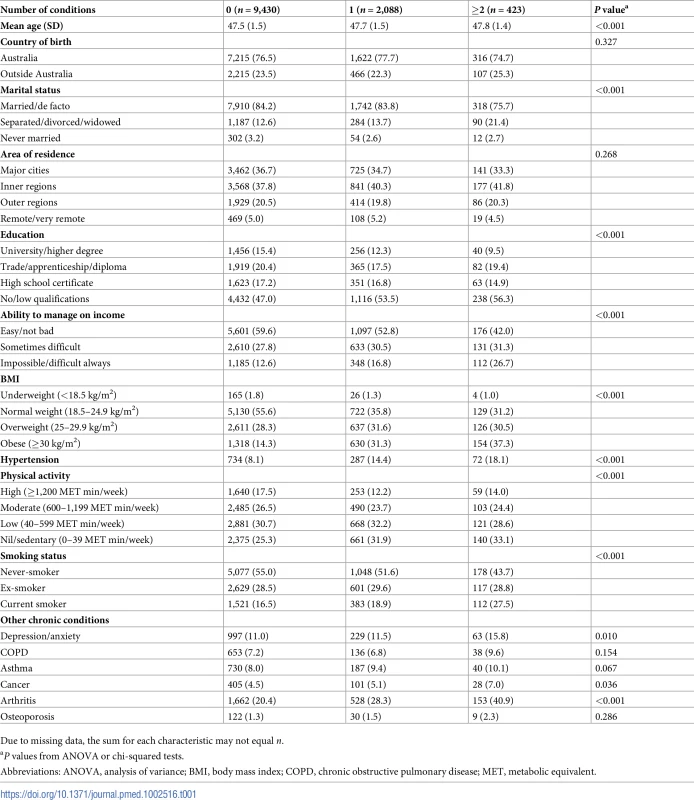
Due to missing data, the sum for each characteristic may not equal n. Longitudinal progression of diabetes, heart disease, stroke, and multimorbidity
During the 20 years of follow-up, 2,511 (18.3%) of the women progressed to at least one condition, of whom 1,420 (56.6%) had diabetes, 1,277 (50.9%) had heart disease, and 308 (12.3%) had stroke; 423 (16.8%) had 2 or 3 of these conditions (Fig 2). As expected, there was an increase in the proportion of women with one or more conditions over time, culminating in 19.2% with 1 condition and 3.9% with multimorbidity at Survey 8. Proportions of women with each combination of these conditions at each survey are presented in S2 Table.
Fig. 2. Venn diagram displaying the overlapping combinations of diabetes, heart disease, and stroke in women who developed any condition over the 20 years (N = 2,511). 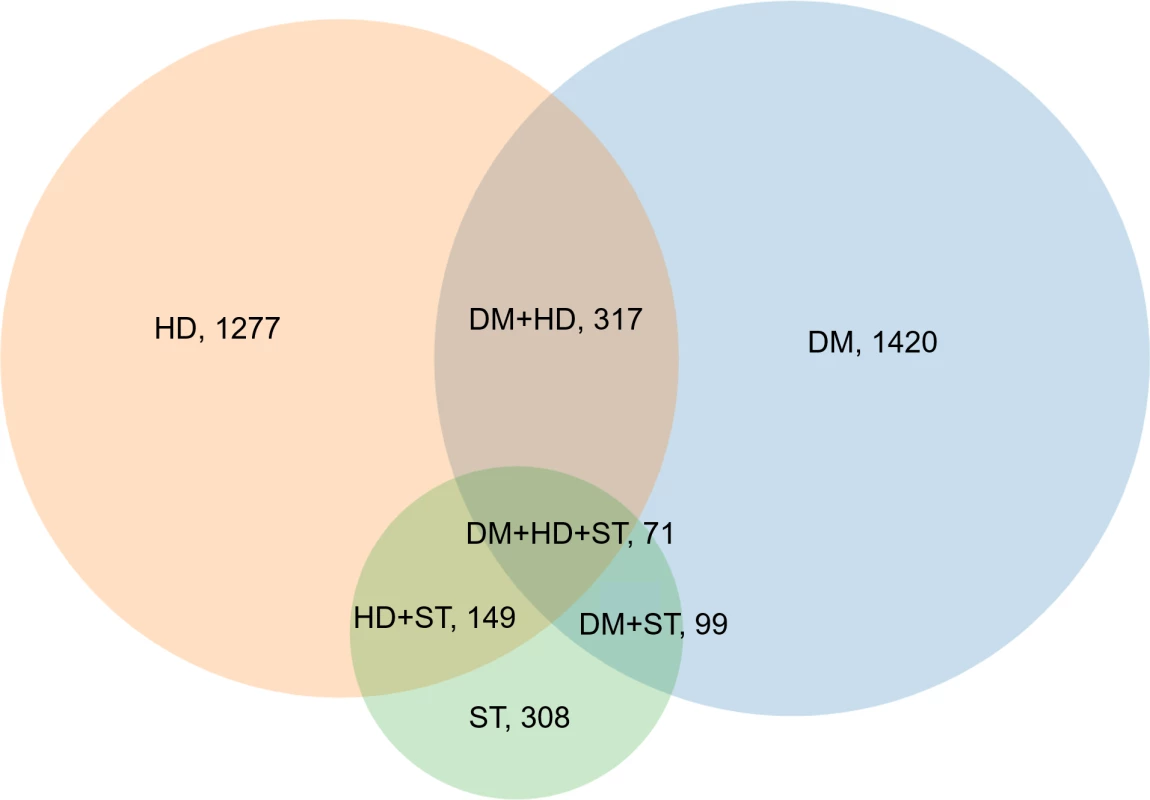
DM, diabetes; HD, heart disease; ST, stroke. The cumulative incidence of the three individual conditions is presented in Fig 3, with 12.9%, 12.0%, and 2.7% of women progressing to diabetes, heart disease, and stroke by Survey 8, respectively. The three conditions were associated with each other (Fig 4). For example, compared with women without stroke, the OR for progressing to diabetes was 2.29 (95% CI, 1.49–3.52) and to heart disease was 3.84 (95% CI, 2.58–5.72) in women with stroke.
Fig. 3. Cumulative incidence of diabetes, heart disease, and stroke in middle-aged Australian women (1996–2016). 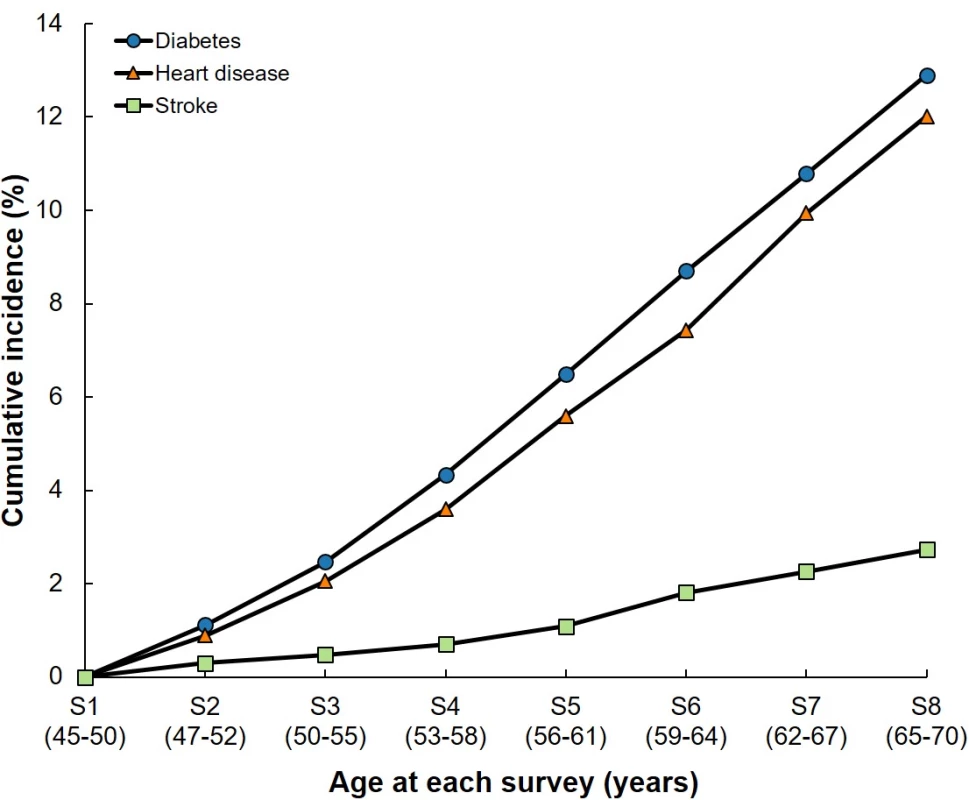
S, survey number. Fig. 4. Associations among diabetes, heart disease, and stroke. 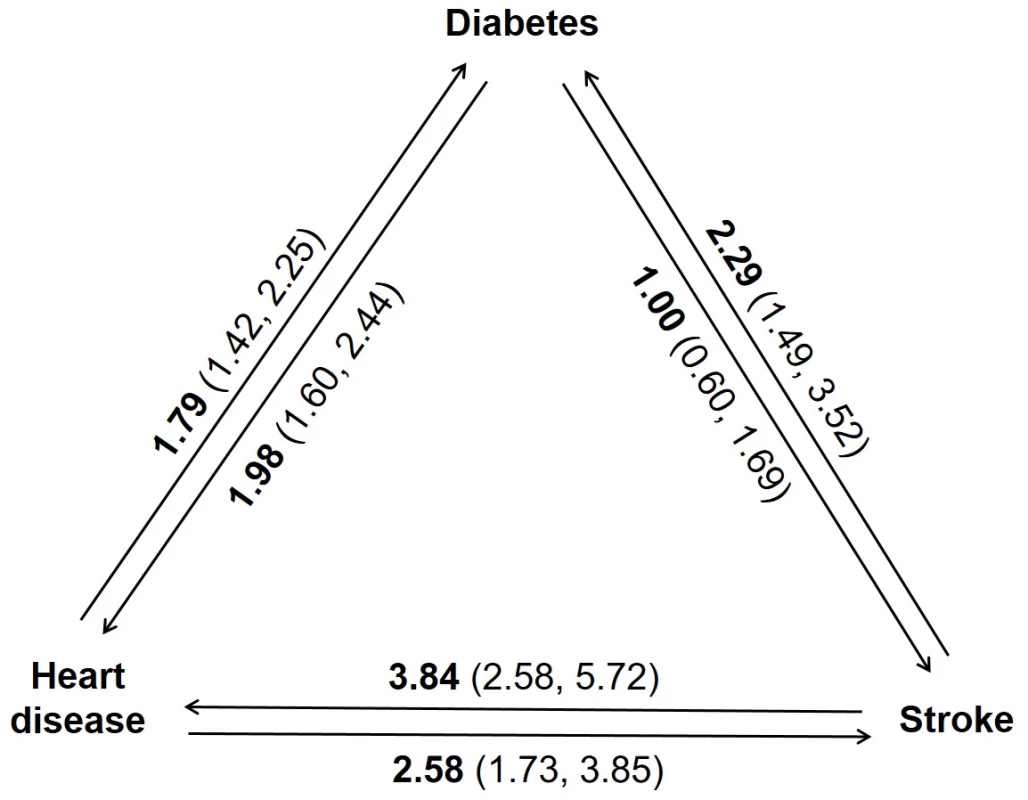
The ORs and 95% CIs in the figure were estimated using repeated measures logistic regression of existing conditions on the incidence of each of the other two conditions, adjusted for age at baseline and time period. CI, confidence interval; OR, odds ratio. The odds for progressing to one condition and accumulation of multimorbidity increased over time, with the accumulation of multimorbidity accelerating between Surveys 4 and 5 (Fig 5). Over a 3-year period, the age-adjusted odds of two or more conditions were approximately twice that of developing one new condition, compared to women who did not develop any new conditions. For example, the odds for developing one new condition between Surveys 7 and 8 were 2.29 (95% CI, 1.93–2.72), whereas the odds for developing two or more conditions were 6.51 (95% CI, 3.95–10.75).
Fig. 5. Longitudinal odds of progressing to any one condition and accumulation of multimorbidity. 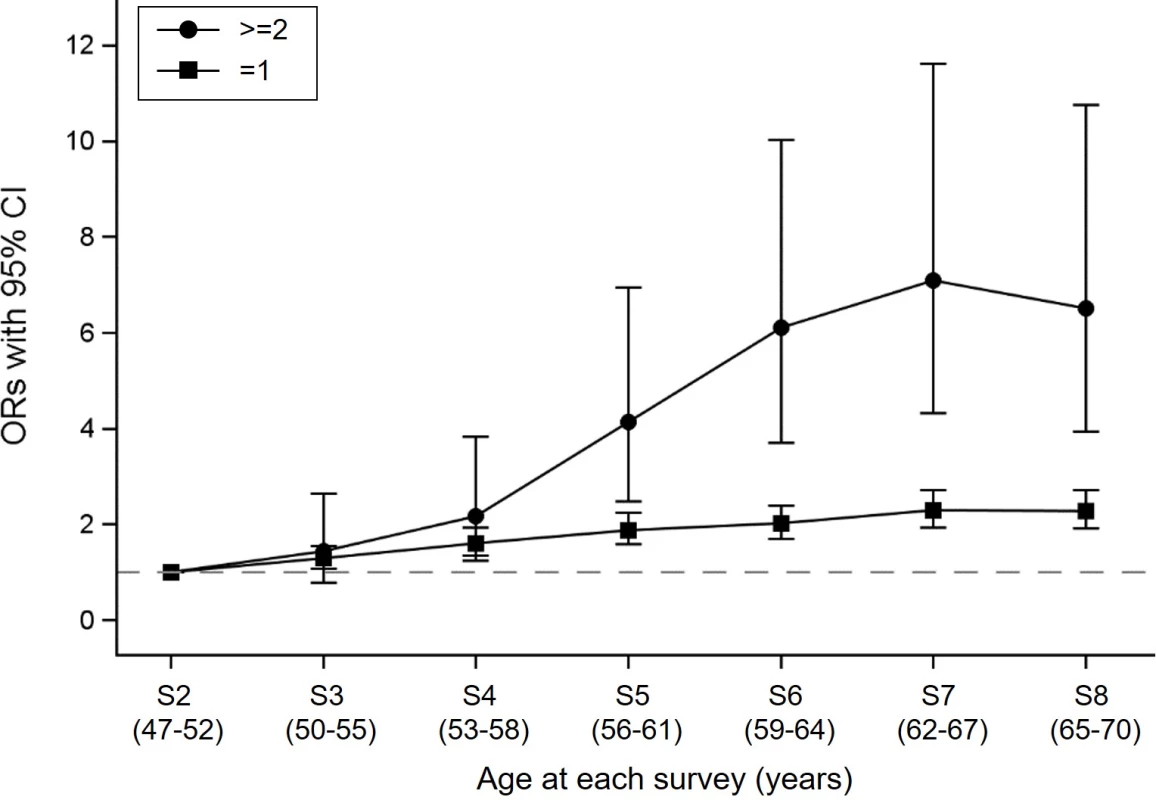
The dashed line indicates the reference group of women who did not develop any new conditions. The ORs were estimated using repeated measures logistic regression, adjusted for age at baseline. The legend “≥2” indicates the transition from none or one to two or three, or from two to three conditions. CI, confidence interval; OR, odds ratio; S, survey number. The Sankey diagram in Fig 6 illustrates the longitudinal progression and transitions among different combinations of diabetes, heart disease, and stroke in women who developed at least one of these conditions. This diagram shows the transitions from “healthy” state (no condition) to any one condition and then to multimorbidity. Over the 20 years of follow-up, the highest rate of progression from one condition to another was observed in women with stroke (Fig 7). The overall incidences of multimorbidity after the first onset of diabetes, heart disease, and stroke were 9.9% (95% CI, 7.9%–12.4%), 11.4% (95% CI, 9.1%–14.4%), and 23.4% (95% CI, 16.3%–32.2%), respectively.
Fig. 6. Sankey diagram showing the longitudinal progression and transitions among different combinations of diabetes, heart disease, and stroke in women who developed at least one of these conditions (N = 2,511). 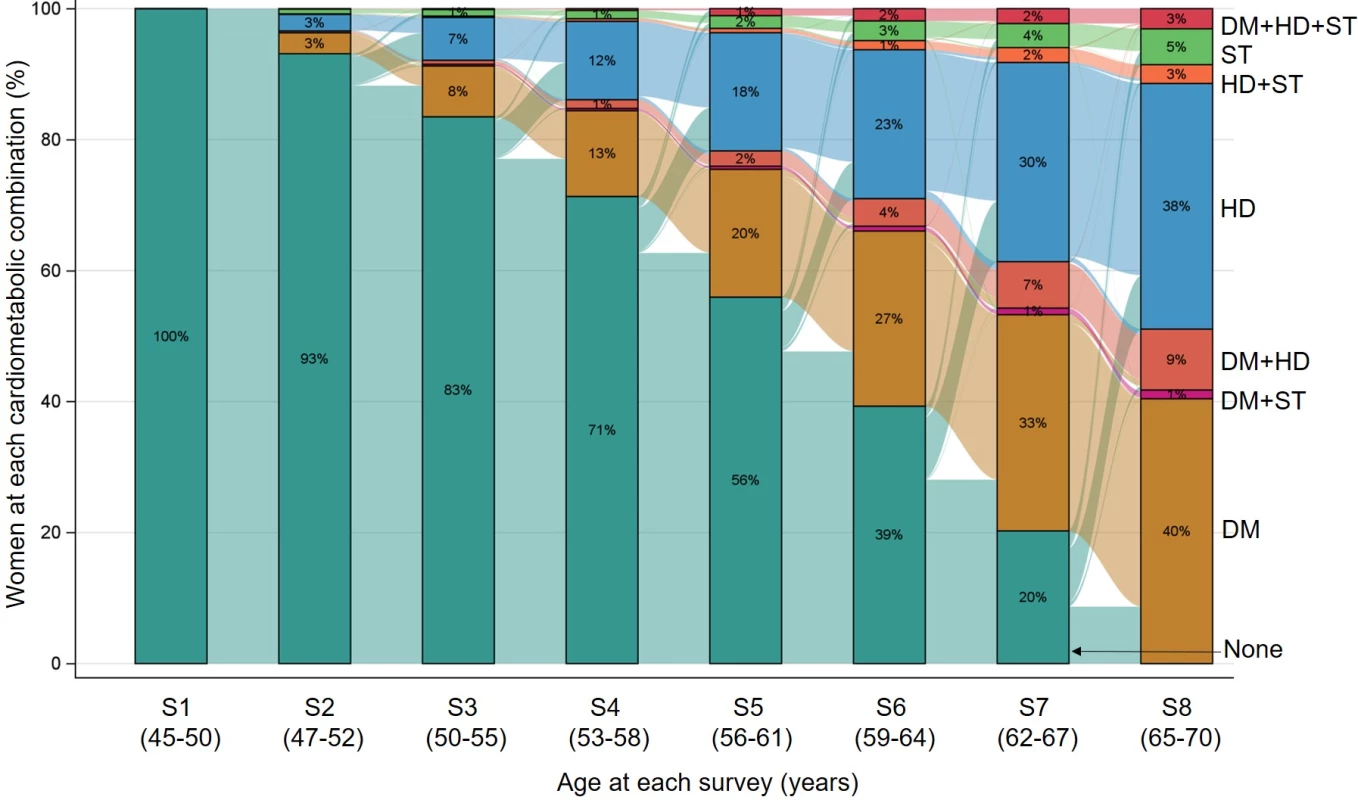
The bars with different colors show the distribution of different conditions at each survey, and the links between bars show the flow from one condition to another. DM, diabetes; HD, heart disease; S, survey number; ST, stroke. Fig. 7. The cumulative incidence of the other two conditions after the first onset of each index condition. 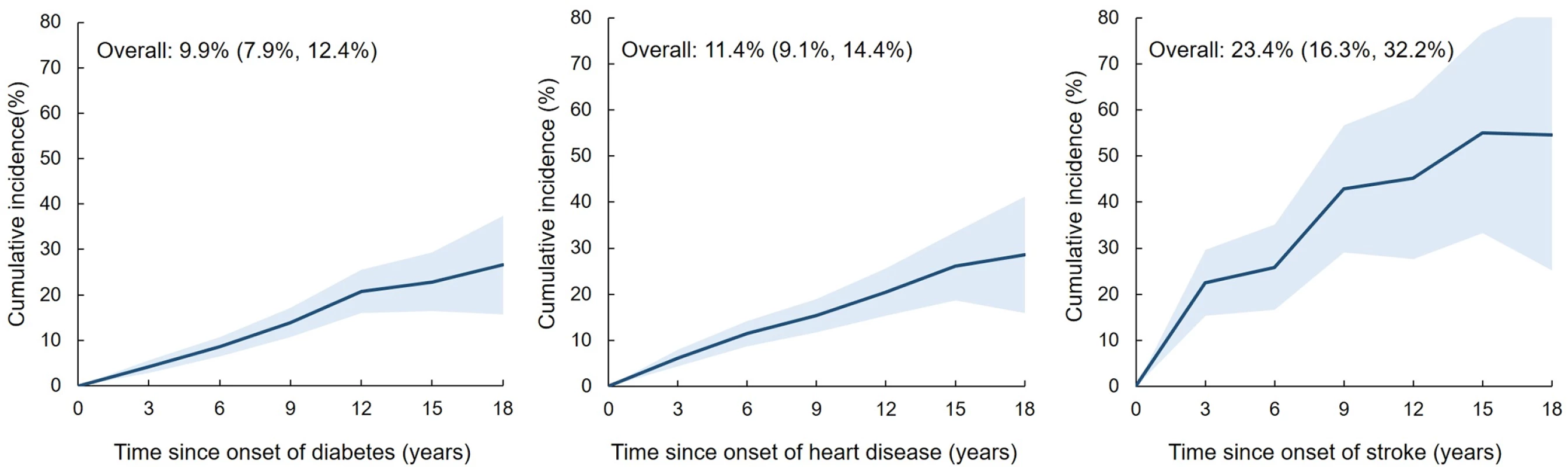
Left, diabetes (N = 1,193); middle, heart disease (N = 996); right, stroke (N = 171). Time 0 indicates the first onset of the index condition. Solid lines represent cumulative incidence, with the shaded bands representing 95% CIs. The three figures were plotted using estimates from repeated measures logistic regression, adjusted for age at time 0. CI, confidence interval. Predictors of accumulation of diabetes, heart disease, and stroke multimorbidity
After controlling for other covariates, being separated, divorced, or widowed; having lower education level; being born in another country; and having difficulties in managing on income were significantly associated with increased odds of accumulating multimorbidity (Table 2). A U-shaped relationship between BMI and the incidence of one condition and accumulation of multimorbidity was seen; obesity was associated with 2.6 - and 3.0-fold increased odds of one condition and accumulation of multimorbidity (OR = 2.58, 95% CI, 2.28–2.92 and 3.01, 95% CI, 2.21–4.08, respectively). Compared with women without prior hypertension, the OR for progressing to one condition was 1.55 (95% CI, 1.40–1.71) and for accumulation of multimorbidity was 2.19 (95% CI, 1.74–2.75). Being sedentary and current smoking were also associated with increased odds of one condition and accumulation of multimorbidity, as were a number of other chronic conditions (Table 2).
Tab. 2. Associations of time-varying sociodemographic and lifestyle factors with 3-year incidence of one condition and accumulation of multimorbidity (N = 11,941). 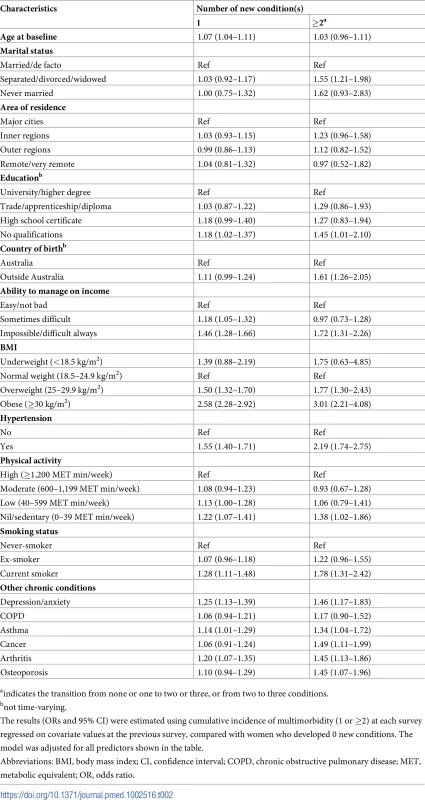
aindicates the transition from none or one to two or three, or from two to three conditions. Similar findings were observed based on multinomial logistic regression of the predictors at baseline (S3 Table). However, being sedentary, having depression/anxiety, asthma, cancer, or osteoporosis at baseline were not associated with the incidence of multimorbidity during follow-up using this simpler model.
Similar findings were also observed with the multinomial regression models of the different combinations of these conditions (S4 Table). Although obesity was consistently associated with multimorbidity, the odds varied depending on the condition sequence. For example, the OR for diabetes followed by CVD was 1.85 (95% CI, 1.25–2.73), whereas for CVD followed by diabetes it was 2.43 (95% CI, 1.28–4.29).
Sensitivity analyses
The trends of cumulative incidence of the three individual conditions and the accumulation of multimorbidity were similar when analyses were performed on the complete case data (N = 6,718 women), with 12.1%, 11.8%, and 2.9% of women progressing to diabetes, heart disease, and stroke at Survey 8, respectively (S1 Fig). The ORs for the incidence of one condition and accumulation of multimorbidity among sociodemographic and lifestyle factors and other chronic conditions were also consistent in complete cases, compared with the main results using all cases (S5 Table).
Discussion
We found that the age-adjusted odds of two or more conditions were approximately twice that of developing one new condition compared to women who did not develop any new conditions, and the onset of stroke is associated with increased risk of progression to heart disease and diabetes. Furthermore, being separated, divorced, or widowed; being born outside Australia; having difficulties with management on income; being overweight or obese; being physically inactive; having hypertension; currently smoking; and having other chronic conditions (i.e, mental disorders, asthma, cancer, osteoporosis, and arthritis) were also associated with this progression.
Comparison with other studies
There has been an extensive discussion in the literature on the associations of diabetes with heart disease and stroke [5–9,12,13,20,21]. However, the longitudinal progression of these conditions remains unclear. To our knowledge, this is the first study to delineate the progression of diabetes, heart disease, and stroke multimorbidity.
The Emerging Risk Factor Collaboration of 91 cohort studies showed that cardiometabolic multimorbidity (defined as a history of two or three from diabetes, stroke, myocardial infarction) is associated with increased mortality risk (hazard ratios for mortality of only one condition, a combination of any two, and a combination of all three were about 2, 4, and 8, respectively), suggesting that development of cardiometabolic conditions accelerates progression to death [4]. In this study, we focused on the early stages of the disease course to investigate progression to individual conditions and multimorbidity. Our results showed that progression to cardiometabolic conditions accelerates as women age, in particular after their mid-50s (Fig 5). The findings of these two studies collectively suggest that interventions that could slow progression to cardiometabolic conditions may have the potential to lead to significant increases in life expectancy.
The relationships among the three conditions are complex. Evidence from systematic reviews suggests that compared with men with diabetes, women with diabetes have a greater risk of coronary heart disease and stroke [8,9]. One population-based cohort study suggested that one-third of patients with heart disease developed new-onset diabetes or impaired fasting glucose during 3.5 years of follow-up [10]. Our study is consistent with these findings. Furthermore, we found that all three conditions were associated with each other, and the onset of stroke may be associated with the progression to other conditions. With self-reported data, a potential explanation for the onset of diabetes following heart disease or stroke is that these women had undiagnosed diabetes (or “prediabetes”) before their heart disease or stroke event. However, statins are recommended for secondary prevention following heart disease or stroke in Australia [22]; hence, heart disease or stroke could have led to statin use, which may have increased the risk of diabetes. Our previous study using data from the 1921–1926 cohort of ALSWH found a 33% increased risk of new-onset diabetes associated with statin exposure [23].
A pooled analysis of individual-level data from 16 cohort studies suggested that overweight and obesity (at baseline) were strongly associated with the incidence of cardiometabolic multimorbidity (at least two from type 2 diabetes, coronary heart disease, and stroke) during a mean follow-up of 10.7 years [11]. Our study is consistent with this study, using multiple follow-up intervals of 3 years and treating BMI as a time-varying variable. However, we found smaller ORs for obesity at baseline on the different combinations of conditions during follow-up. In our study, the ORs associated with obesity varied between 1.10 and 2.43 (95% CI varied between 0.93 and 4.29) depending on the combination of conditions, compared to the previously reported ORs that ranged from 1.5 to 29.8 (95% CI varied between 1.2 and 40.8). Possible explanations for this difference are that the participants in our study were women aged 45–50 at baseline, and they were followed up for 20 years, whereas the previous study included both men and women with a wider age range of 35–105 and a shorter period of follow-up (10.7 years).
The relationship between hypertension and individual diabetes, heart disease, and stroke is well established [24,25], but the results are controversial when considering the sequences of these conditions [24]. We found that women with prior hypertension are more like to progress to multimorbidity. This finding suggests that hypertension might play a major role in the longitudinal progression of the three conditions over time [25]. There have been few studies that have investigated the associations of other chronic conditions with diabetes, heart disease, and stroke multimorbidity [21,26]. A cross-sectional study using data from the UK Biobank found rheumatoid arthritis was associated with the increasing numbers of the three conditions [21], a result consistent with our findings.
Strengths and limitations
A strength of this study is the large, nationally representative sample and the longitudinal nature of the data, which allowed us to document disease progression over time [27]. Also, as the onset and experience of chronic conditions often occur during midlife [28], the use of a cohort of middle-aged women who were initially healthy reflects the “real-world experience” of disease progression, particularly in the early stages of the course of disease [29]. Furthermore, we used time-varying lifestyle factors and other chronic conditions to capture the dynamic changes of these predictors over time [30]. This may be important, as illustrated by the differing results for the effect of physical activity on the incidence of multimorbidity depending on whether this variable was treated as time-varying or fixed at baseline.
Several methodological limitations of the study should also be noted. First, diabetes, heart disease, stroke, and other chronic conditions are based on self-report, which may have introduced bias in outcome ascertainment. However, the cumulative incidence of the three conditions at the age of 65–70 (Survey 8) in our study population was almost the same as that for women of this age reported in the Australian National Health Survey (2014–2015) [31]. Furthermore, previous studies have validated self-report of various chronic diseases in the ALSWH. For example, the prevalence and bias-adjusted kappa for diabetes, heart disease, stroke, and hypertension from hospital data were 0.93, 0.91, 0.98, and 0.53, respectively [17]. Cancer information included in the study has been validated against Cancer Registry data with 89% sensitivity and 97% specificity [32]. Several other studies have demonstrated the validity of self-reported conditions, BMI, physical activity, and other risk factors [19,33–38].
Second, the small number of cases with more than one condition, potential undiagnosed cases of diabetes, and unknown information on heart disease and stroke type [39,40] might all have led to increased uncertainty and potential underestimation of the odds obtained from the regression models. Third, although we conducted a sensitivity analysis to check the robustness of our findings with complete case data, we did not account for the competing risk of women dying before they could potentially progress to one or more of diabetes, heart disease, and stroke [41]. However, we compared the mortality of all participants and of just the women who developed the three conditions, and the proportions were quite similar and low (4.63% [553/11,941] versus 4.70% [118/2,511], respectively). Fourth, although the attrition rates were low during the 20-year follow-up (S1 Table), there is potential for bias in the estimates presented due to attrition or restricting the analysis to complete cases. Fifth, the study sample was women aged 45–50 at baseline, which limits the generalizability of the findings to other groups. However, the study sample is broadly representative of all women born in 1945–1950 in Australia [15]. Finally, the inclusion of information on treatments in the analysis may have influenced the results.
Further studies with a large number of validated cases and for women and men in different age groups are needed to establish the generalizability of these findings and to explore interventions that might slow cardiometabolic progression [27,42].
Conclusion
Our findings indicate that the odds for accumulation of diabetes, heart disease, and stroke multimorbidity was higher than the odds of progressing to one condition in middle-aged women. Stroke was associated with increased risk of progression to diabetes and heart disease. Social inequality, overweight and obesity, hypertension, physical inactivity, smoking, and having prior chronic conditions (i.e., mental disorders, asthma, cancer, osteoporosis, and arthritis) are all associated with increased risk of accumulation of multimorbidity.
These findings could have significant clinical and public health implications for the treatment and prevention of diabetes, heart disease, and stroke multimorbidity. Delineation of the disease progression may assist in the evaluation of risk for additional conditions during clinical practice. The identified risk factors from this study are appropriate targets for reducing the risk of multimorbidity.
Supporting Information
Zdroje
1. Jackson CA, Dobson AJ, Tooth LR, Mishra GD. Lifestyle and socioeconomic determinants of multimorbidity patterns among mid-aged women: a longitudinal study. PLoS ONE. 2016;11(6). doi: 10.1371/journal.pone.0156804 27258649.
2. Dunlay SM, Chamberlain AM. Multimorbidity in older patients with cardiovascular disease. Curr Cardiovasc Risk Rep. 2016;10. doi: 10.1007/s12170-016-0491-8 27274775.
3. SL R., Wei MY, Kim M, Narayan KMV, Saydah SS. Multimorbidity of four cardiometabolic and chronic pulmonary disease groups: prevalence and attributable fraction in US adults, 2007–2012. J Comorbidity. 2017;7(1):11. doi: 10.15256/joc.2017.7.89 29090186.
4. Emerging Risk Factors Collaboration, Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. 2015;314(1):52–60. doi: 10.1001/jama.2015.7008 26151266.
5. Lyall DM, Celis-Morales CA, Anderson J, Gill JMR, Mackay DF, McIntosh AM, et al. Associations between single and multiple cardiometabolic diseases and cognitive abilities in 474 129 UK Biobank participants. Eur Heart J. 2017;38(8):577–83. doi: 10.1093/eurheartj/ehw528 28363219.
6. Martín-Timón I, Sevillano-Collantes C, Segura-Galindo A, del Cañizo-Gómez FJ. Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diabetes. 2014;5(4):444. doi: 10.4239/wjd.v5.i4.444 25126392.
7. Sattar N, McConnachie A, Shaper AG, Blauw GJ, Buckley BM, de Craen AJ, et al. Can metabolic syndrome usefully predict cardiovascular disease and diabetes? Outcome data from two prospective studies. Lancet. 2008;371(9628):1927–35. doi: 10.1016/S0140-6736(08)60602-9 18501419.
8. Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ. 2006;332(7533):73–8. doi: 10.1136/bmj.38678.389583.7C 16371403.
9. Peters SAE, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775 385 individuals and 12 539 strokes. Lancet. 2014;383(9933):1973–80. doi: 10.1016/S0140-6736(14)60040-4 24613026.
10. Mozaffarian D, Marfisi R, Levantesi G, Silletta MG, Tavazzi L, Tognoni G, et al. Incidence of new-onset diabetes and impaired fasting glucose in patients with recent myocardial infarction and the effect of clinical and lifestyle risk factors. Lancet. 2007;370(9588):667–75. Epub 2007/08/28. doi: 10.1016/S0140-6736(07)61343-9 17720018.
11. Kivimaki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. 2017;2(6):e277–e85. doi: 10.1016/S2468-2667(17)30074-9 28626830.
12. Rawshani A, Rawshani A, Franzen S, Eliasson B, Svensson AM, Miftaraj M, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376(15):1407–18. Epub 2017/04/14. doi: 10.1056/NEJMoa1608664 28402770.
13. Cholesterol Treatment Trialists Collaborators, Kearney PM, Blackwell L, Collins R, Keech A, Simes J, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371(9607):117–25. doi: 10.1016/S0140-6736(08)60104-X 18191683.
14. Matuleviciene-Anangen V, Rosengren A, Svensson AM, Pivodic A, Gudbjornsdottir S, Wedel H, et al. Glycaemic control and excess risk of major coronary events in persons with type 1 diabetes. Heart. 2017. doi: 10.1136/heartjnl-2016-311050 28710186.
15. Dobson AJ, Hockey R, Brown WJ, Byles JE, Loxton DJ, McLaughlin D, et al. Cohort profile update: Australian Longitudinal Study on Women's Health. Int J Epidemiol. 2015;44(5):1547-f. doi: 10.1093/ije/dyv110 26130741
16. Lee C, Dobson AJ, Brown WJ, Bryson L, Byles J, Warner-Smith P, et al. Cohort Profile: the Australian Longitudinal Study on Women's Health. Int J Epidemiol. 2005;34(5):987–91. doi: 10.1093/ije/dyi098 15894591.
17. Navin Cristina TJ, Stewart Williams JA, Parkinson L, Sibbritt DW, Byles JE. Identification of diabetes, heart disease, hypertension and stroke in mid - and older-aged women: Comparing self-report and administrative hospital data records. Geriatr Gerontol Int. 2015. doi: 10.1111/ggi.12442 25613080.
18. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. Geneva: World Health Organization, 2000 9241208945 Contract No.: 894.
19. Brown WJ, Trost SG, Bauman A, Mummery K, Owen N. Test-retest reliability of four physical activity measures used in population surveys. J Sci Med Sport. 2004;7(2):205–15. doi: 10.1016/S1440-2440(04)80010-0 15362316.
20. Schaan BD, de Figueiredo Neto JA, Moreira LB, Ledur P, Mattos LAP, Magnoni D, et al. Diabetes and cardiovascular events in high-risk patients: Insights from a multicenter registry in a middle-income country. Diabetes Res Clin Pract. 2017;127 : 275–84. doi: 10.1016/j.diabres.2017.03.021 28412543.
21. Dregan A, Chowienczyk P, Molokhia M. Cardiovascular and type 2 diabetes morbidity and all-cause mortality among diverse chronic inflammatory disorders. Heart. 2017. doi: 10.1136/heartjnl-2017-311214 28601812
22. National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand. Reducing risk in heart disease: an expert guide to clinical practice for secondary prevention of coronary heart disease. Melbourne: National Heart Foundation of Australia, 2012.
23. Jones M, Tett S, Peeters GM, Mishra GD, Dobson A. New-Onset Diabetes After Statin Exposure in Elderly Women: The Australian Longitudinal Study on Women's Health. Drugs Aging. 2017;34(3):203–9. doi: 10.1007/s40266-017-0435-0 28138911.
24. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957–67. doi: 10.1016/S0140-6736(15)01225-8 26724178.
25. Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension. 2001;37(4):1053–9. 11304502.
26. Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):962–9. doi: 10.1183/09031936.00012408 18579551.
27. Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev. 2017;37 : 53–68. doi: 10.1016/j.arr.2017.05.003 28511964.
28. Byles J, Hockey R, McLaughlin D, Dobson A, Brown W, Loxton D, et al. Chronic conditions, physical function and health care use: Findings from the Australian Longitudinal Study on Women’s Health. Report prepared for the Australian Government Department of Health. 2015.
29. van Oostrom SH, Gijsen R, Stirbu I, Korevaar JC, Schellevis FG, Picavet HS, et al. Time trends in prevalence of chronic diseases and multimorbidity not only due to aging: data from general practices and health surveys. PLoS ONE. 2016;11(8):e0160264. doi: 10.1371/journal.pone.0160264 27482903.
30. Arnold M, Jiang L, Stefanick ML, Johnson KC, Lane DS, LeBlanc ES, et al. Duration of Adulthood Overweight, Obesity, and Cancer Risk in the Women's Health Initiative: A Longitudinal Study from the United States. PLoS Med. 2016;13(8):e1002081. doi: 10.1371/journal.pmed.1002081 27529652.
31. Australian Bureau of Statistics. National Health Survey: First results, 2014–15. Canberra: 2015 Contract No.: 4364.0.55.001.
32. Stavrou E, Vajdic CM, Loxton D, Pearson SA. The validity of self-reported cancer diagnoses and factors associated with accurate reporting in a cohort of older Australian women. Cancer Epidemiol. 2011;35(6):e75–80. doi: 10.1016/j.canep.2011.02.005 21474409.
33. Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57(10):1096–103. doi: 10.1016/j.jclinepi.2004.04.005 15528061.
34. Hansen H, Schafer I, Schon G, Riedel-Heller S, Gensichen J, Weyerer S, et al. Agreement between self-reported and general practitioner-reported chronic conditions among multimorbid patients in primary care—results of the MultiCare Cohort Study. Bmc Family Practice. 2014;15. doi: 10.1186/1471-2296-15-39 24580758.
35. Burton NW, Brown W, Dobson A. Accuracy of body mass index estimated from self-reported height and weight in mid-aged Australian women. Aust N Z J Public Health. 2010;34(6):620–3. doi: 10.1111/j.1753-6405.2010.00618.x 21134066.
36. Jackson CA, Mishra GD, Tooth L, Byles J, Dobson A. Moderate agreement between self-reported stroke and hospital-recorded stroke in two cohorts of Australian women: a validation study. BMC Med Res Methodol. 2015;15 : 7. doi: 10.1186/1471-2288-15-7 25613556.
37. Parkinson L, Curryer C, Gibberd A, Cunich M, Byles JE. Good agreement between self-report and centralized hospitalizations data for arthritis-related surgeries. J Clin Epidemiol. 2013;66(10):1128–34. doi: 10.1016/j.jclinepi.2013.04.012 23845185.
38. Peeters G, Parkinson L, Badley E, Jones M, Brown WJ, Dobson AJ, et al. Contemporaneous severity of symptoms and functioning reflected by variations in reporting doctor-diagnosed osteoarthritis. Arthritis Care Res (Hoboken). 2013;65(6):945–53. doi: 10.1002/acr.21929 23281307.
39. Jackson CA, Mishra GD. Depression and risk of stroke in midaged women: a prospective longitudinal study. Stroke. 2013;44(6):1555–60. doi: 10.1161/STROKEAHA.113.001147 23686976.
40. Alhazmi A, Stojanovski E, McEvoy M, Brown W, Garg ML. Diet quality score is a predictor of type 2 diabetes risk in women: the Australian Longitudinal Study on Women's Health. Br J Nutr. 2014;112(6):945–51. doi: 10.1017/S0007114514001688 25201303.
41. Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Stat Med. 2007;26(11):2389–430. doi: 10.1002/sim.2712 17031868.
42. Xu X, Mishra GD, Jones M. Mapping the global research landscape and knowledge gaps on multimorbidity: a bibliometric study. J Glob Health. 2017;7(1):010414. doi: 10.7189/jogh.07.010414 28685036.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2018 Číslo 3- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Ferinject: správně indikovat, správně podat, správně vykázat
- Optimální dávkování apixabanu v léčbě fibrilace síní
-
Všechny články tohoto čísla
- What is the value of multidisciplinary care for chronic kidney disease?
- 2017 Reviewer and Editorial Board Thank You
- Delays in completion and results reporting of clinical trials under the Paediatric Regulation in the European Union: A cohort study
- Surveillance of antimicrobial consumption in animal production sectors of low- and middle-income countries: Optimizing use and addressing antimicrobial resistance
- Causes of death and infant mortality rates among full-term births in the United States between 2010 and 2012: An observational study
- Time for high-burden countries to lead the tuberculosis research agenda
- The importance and challenges of shared decision making in older people with multimorbidity
- Trajectories of functional decline in older adults with neuropsychiatric and cardiovascular multimorbidity: A Swedish cohort study
- Mortality, ethnicity, and country of birth on a national scale, 2001–2013: A retrospective cohort (Scottish Health and Ethnicity Linkage Study)
- Validation of a genetic risk score for atrial fibrillation: A prospective multicenter cohort study
- Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: Latent class analysis of a nationwide population-based cohort
- Integration of postpartum healthcare services for HIV-infected women and their infants in South Africa: A randomised controlled trial
- Cost-effectiveness of multidisciplinary care in mild to moderate chronic kidney disease in the United States: A modeling study
- Role of heme in lung bacterial infection after trauma hemorrhage and stored red blood cell transfusion: A preclinical experimental study
- Patterns and temporal trends of comorbidity among adult patients with incident cardiovascular disease in the UK between 2000 and 2014: A population-based cohort study
- Global child and adolescent mental health: The orphan of development assistance for health
- Cardiovascular disease and multimorbidity: A call for interdisciplinary research and personalized cardiovascular care
- Forced anal examinations to ascertain sexual orientation and sexual behavior: An abusive and medically unsound practice
- Primary prevention of cardiovascular disease: The past, present, and future of blood pressure- and cholesterol-lowering treatments
- Physical activity levels in adults and older adults 3–4 years after pedometer-based walking interventions: Long-term follow-up of participants from two randomised controlled trials in UK primary care
- Effect and cost-effectiveness of educating mothers about childhood DPT vaccination on immunisation uptake, knowledge, and perceptions in Uttar Pradesh, India: A randomised controlled trial
- Comorbidity health pathways in heart failure patients: A sequences-of-regressions analysis using cross-sectional data from 10,575 patients in the Swedish Heart Failure Registry
- Multimorbidity in patients with heart failure from 11 Asian regions: A prospective cohort study using the ASIAN-HF registry
- Antiviral efficacy of favipiravir against Ebola virus: A translational study in cynomolgus macaques
- Transmission of HIV-1 drug resistance mutations within partner-pairs: A cross-sectional study of a primary HIV infection cohort
- A clinical decision support tool for improving adherence to guidelines on anticoagulant therapy in patients with atrial fibrillation at risk of stroke: A cluster-randomized trial in a Swedish primary care setting (the CDS-AF study)
- Integrating HIV and hypertension management in low-resource settings: Lessons from Malawi
- The epidemiology of adolescents living with perinatally acquired HIV: A cross-region global cohort analysis
- Polycystic ovary syndrome, androgen excess, and the risk of nonalcoholic fatty liver disease in women: A longitudinal study based on a United Kingdom primary care database
- Blood pressure-lowering treatment strategies based on cardiovascular risk versus blood pressure: A meta-analysis of individual participant data
- Cerebral white matter disease and functional decline in older adults from the Northern Manhattan Study: A longitudinal cohort study
- HIV treatment eligibility expansion and timely antiretroviral treatment initiation following enrollment in HIV care: A metaregression analysis of programmatic data from 22 countries
- The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: A microsimulation study
- Cardiovascular disease: The rise of the genetic risk score
- Comparative analysis of the association between 35 frailty scores and cardiovascular events, cancer, and total mortality in an elderly general population in England: An observational study
- Progression of diabetes, heart disease, and stroke multimorbidity in middle-aged women: A 20-year cohort study
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Forced anal examinations to ascertain sexual orientation and sexual behavior: An abusive and medically unsound practice
- Polycystic ovary syndrome, androgen excess, and the risk of nonalcoholic fatty liver disease in women: A longitudinal study based on a United Kingdom primary care database
- The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: A microsimulation study
- Cardiovascular disease and multimorbidity: A call for interdisciplinary research and personalized cardiovascular care
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



