-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaIntimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies
Background:
Depression and suicide are responsible for a substantial burden of disease globally. Evidence suggests that intimate partner violence (IPV) experience is associated with increased risk of depression, but also that people with mental disorders are at increased risk of violence. We aimed to investigate the extent to which IPV experience is associated with incident depression and suicide attempts, and vice versa, in both women and men.Methods and Findings:
We conducted a systematic review and meta-analysis of longitudinal studies published before February 1, 2013. More than 22,000 records from 20 databases were searched for studies examining physical and/or sexual intimate partner or dating violence and symptoms of depression, diagnosed major depressive disorder, dysthymia, mild depression, or suicide attempts. Random effects meta-analyses were used to generate pooled odds ratios (ORs). Sixteen studies with 36,163 participants met our inclusion criteria. All studies included female participants; four studies also included male participants. Few controlled for key potential confounders other than demographics. All but one depression study measured only depressive symptoms. For women, there was clear evidence of an association between IPV and incident depressive symptoms, with 12 of 13 studies showing a positive direction of association and 11 reaching statistical significance; pooled OR from six studies = 1.97 (95% CI 1.56–2.48, I2 = 50.4%, pheterogeneity = 0.073). There was also evidence of an association in the reverse direction between depressive symptoms and incident IPV (pooled OR from four studies = 1.93, 95% CI 1.51–2.48, I2 = 0%, p = 0.481). IPV was also associated with incident suicide attempts. For men, evidence suggested that IPV was associated with incident depressive symptoms, but there was no clear evidence of an association between IPV and suicide attempts or depression and incident IPV.Conclusions:
In women, IPV was associated with incident depressive symptoms, and depressive symptoms with incident IPV. IPV was associated with incident suicide attempts. In men, few studies were conducted, but evidence suggested IPV was associated with incident depressive symptoms. There was no clear evidence of association with suicide attempts.
Please see later in the article for the Editors' Summary
Published in the journal: . PLoS Med 10(5): e32767. doi:10.1371/journal.pmed.1001439
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001439Summary
Background:
Depression and suicide are responsible for a substantial burden of disease globally. Evidence suggests that intimate partner violence (IPV) experience is associated with increased risk of depression, but also that people with mental disorders are at increased risk of violence. We aimed to investigate the extent to which IPV experience is associated with incident depression and suicide attempts, and vice versa, in both women and men.Methods and Findings:
We conducted a systematic review and meta-analysis of longitudinal studies published before February 1, 2013. More than 22,000 records from 20 databases were searched for studies examining physical and/or sexual intimate partner or dating violence and symptoms of depression, diagnosed major depressive disorder, dysthymia, mild depression, or suicide attempts. Random effects meta-analyses were used to generate pooled odds ratios (ORs). Sixteen studies with 36,163 participants met our inclusion criteria. All studies included female participants; four studies also included male participants. Few controlled for key potential confounders other than demographics. All but one depression study measured only depressive symptoms. For women, there was clear evidence of an association between IPV and incident depressive symptoms, with 12 of 13 studies showing a positive direction of association and 11 reaching statistical significance; pooled OR from six studies = 1.97 (95% CI 1.56–2.48, I2 = 50.4%, pheterogeneity = 0.073). There was also evidence of an association in the reverse direction between depressive symptoms and incident IPV (pooled OR from four studies = 1.93, 95% CI 1.51–2.48, I2 = 0%, p = 0.481). IPV was also associated with incident suicide attempts. For men, evidence suggested that IPV was associated with incident depressive symptoms, but there was no clear evidence of an association between IPV and suicide attempts or depression and incident IPV.Conclusions:
In women, IPV was associated with incident depressive symptoms, and depressive symptoms with incident IPV. IPV was associated with incident suicide attempts. In men, few studies were conducted, but evidence suggested IPV was associated with incident depressive symptoms. There was no clear evidence of association with suicide attempts.
Please see later in the article for the Editors' SummaryBackground
Unipolar depressive disorders are the second leading cause of disease burden in women aged 15–44 y worldwide, and self-inflicted injuries are the seventh leading cause of disease burden [1]. Intimate partner violence (IPV) is also common, being reported by 15%–71% of women over their lifetime [2]. These conditions are linked—IPV experience is strongly and consistently associated with depression, including depressive symptoms and depressive disorders, and suicide in cross-sectional studies of women in both high - and lower-income settings [3]–[7]. There is less research on men, but cross-sectional studies also show that depressive symptoms are associated with IPV experience [8]. Several authors have speculated that the increased exposure to various forms of violence among women relative to men may help to explain the greater prevalence of depression, suicide attempts, and other common mental disorders in women versus men [9],[10].
While it is easy to assume that IPV is causally related to subsequent depression and suicidal behaviour, evidence suggests a more complex relationship. There are three modes of association, which are possible in any combination: (1) IPV exposure causes subsequent depression and suicide attempts, (2) depression and/or suicide attempts cause subsequent IPV, and (3) there are common risk factors for both IPV and depression and suicide attempts that explain the association between them.
Traumatic stress is the main mechanism by which IPV might cause subsequent depression and suicide attempts. Traumatic events can lead to stress, fear, and isolation, which in turn may lead to depression and suicidal behaviour [9]. A recent meta-analysis of three longitudinal studies provides support for this direction of association with depression, but this analysis pooled depressive disorders, depressive symptoms, and postpartum depression; included only a subset of known studies; and examined only one direction of association (that IPV is a risk factor for depression) [5]. To our knowledge there are no meta-analyses of the associations between IPV and suicide attempts.
Conversely, other studies suggest that women with severe mental health difficulties are more likely to experience violent victimisation [11],[12]. The same may hold for more minor forms of depression. Studies among US teenagers suggest that depression precedes first incidents of dating violence [13]. It is plausible that depressive symptoms may influence partner selection, such that young men and women are more accepting of partners with poor impulse control, conduct disorders, or other factors that predispose partners to use violence. Although it is clear that violence must precede completed suicides, most studies on violence and suicide actually measure suicide attempts, which could precede violent experiences.
Developmental and early life exposures to violence and other traumas may also play a role in predicting both violence and depression, for example, by contributing to the formation of insecure or disorganised attachment styles, which are associated with both increased IPV and depression risk [14],[15]. Although the mechanism remains unclear, women who have experienced childhood sexual abuse (CSA) also have an increased risk of subsequent experience of IPV [16]. Usually, longitudinal twin studies provide the best means of ruling out the confounding effect of early life factors, and two twin studies that have investigated exposure to general trauma suggest that traumatic events are causally associated with increased risk of major depressive disorder and suicide [9],[10],[17],[18]. However, to our knowledge no twin studies have examined the role of IPV victimisation specifically.
To assess the magnitude and direction of the relationship between IPV and depression and suicide attempts, we conducted a systematic review and meta-analysis of longitudinal studies examining the association of depression and suicide attempts with IPV experience in women and men. This study was conducted as part of the work of the Expert Working Group on Violence, for the Global Burden of Disease Study 2010 [19]. We aimed to (1) describe the characteristics of included studies, (2) report on magnitude and direction of association, and (3) document and explore potential sources of heterogeneity.
Methods
Searches
We searched 20 different health and social science databases, including Medline, Embase, CINAHL (Cumulative Index to Nursing and Allied Health Literature), and region-specific databases from first record until February 1, 2009. This initial search was conducted as part of a larger set of systematic reviews, and included studies looking at health conditions in addition to depression and suicide. We updated the search in Medline to February 1, 2013, focusing on only depression and suicide studies. Strategies were designed in consultation with a librarian. Controlled vocabulary terms related to study design, violence, depression, and suicide were used for each database. The search and screening process is summarised in Figure 1. A list of databases and an example search strategy are provided in Text S2, and a PRIMSA checklist in Text S1.
Fig. 1. Flow of studies through the review. 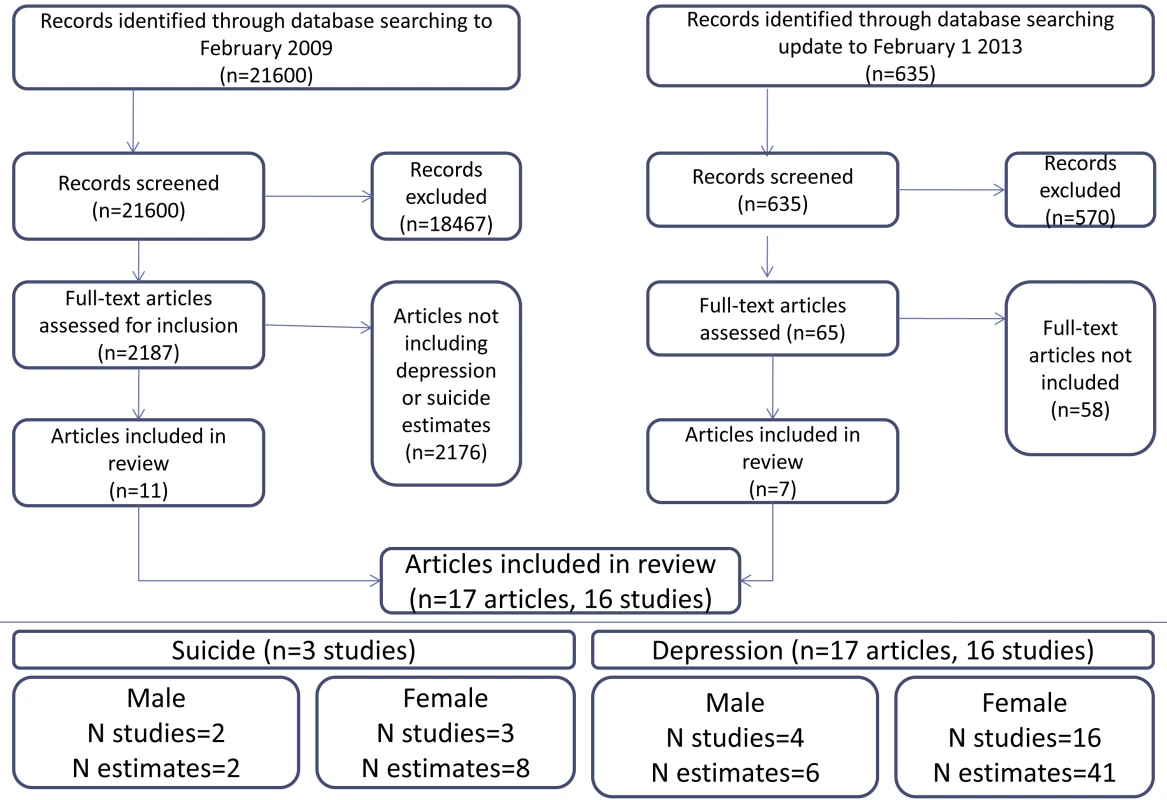
Inclusion Criteria
Longitudinal studies in any population of male and/or female participants were considered. Studies were deemed longitudinal if either the exposure or the outcome was measured at more than one time point. Papers reporting data from existing cohorts where both the exposure and outcome were assessed at the same time point were not included. All author definitions of IPV experience and all author definitions of depression (including symptoms and diagnoses) and measures of suicide attempts were eligible for inclusion. Papers reporting only on postpartum or antenatal depression were not included. Papers reporting only on suicidal thoughts or plans were not included.
Screening and Data Extraction
For the original search, abstracts were screened by one reviewer; full text articles were appraised by JM, JC, GF, or LB and re-appraised by KMD. Data were extracted by one reviewer (JM, JC, GF, or LB) onto a standardised form, and checked by KMD. For the update, all steps were performed by KMD. Information about study population, exposure and outcome definitions, length of follow-up, effect estimates and uncertainty, analysis and control for confounding, and study quality were extracted.
Quality Assessment
We appraised the quality of each effect estimate. We considered the definitions of the violence and depression/suicide measures and whether these were measured using valid, reliable instruments. We considered how the reference groups for each exposure were constructed (if they were truly unexposed or if there could potentially have been some misclassification). This is especially important for research examining the effects of IPV, as different forms of IPV (physical and sexual) are often only moderately correlated [2]. Studies measuring only one form of violence therefore potentially have a comparison group with exposure to the other form of violence.
We also considered control for potential confounders in key areas. First, because both IPV and depression commonly occur episodically over a period of time, events of either that are incident over the study period could be a continuation of previous violence/depression. Thus, we examined whether time one levels (at the beginning of the study period) of the outcome variable were adjusted for. Second, both IPV and depression/suicide attempts are associated with childhood adverse events, substance use, demographics, and other common risk factors that may explain the association between them. Because of the complexity of the potential causal pathways involved, we did not define a minimum set of confounders or common risk factors that should be adjusted for, but we aimed to consider results in light of which variables were included in analyses.
Data Synthesis
Overall results on study characteristics and quality are summarised descriptively. Studies reported a range of different types of effect estimates (for example, relative risks, odds ratios [ORs], and correlation coefficients). They also varied on whether violence and depression outcomes were measured as binary or continuous variables, making it difficult to quantitatively summarise results. Where information was not reported, we calculated effect estimates and uncertainty as far as possible. Therefore, we present (1) results of all studies meeting the inclusion criteria in their original metrics in tabular format, and (2) where possible, pooled measures of effect using random effects meta-analysis. Heterogeneity was measured using Higgins I2, with p<0.10 taken to indicate possible heterogeneity. For each meta-analysis, only one estimate per data source was included. The estimate least subject to bias according to the quality criteria above was selected. We had too few studies to quantitatively examine sources of heterogeneity.
Ethics Statement
All data used in this review were already in the public domain; no ethical approval was required.
Results
Study Characteristics
Sixteen studies with 36,163 participants met the inclusion criteria. These were reported in 17 papers and contained 55 relevant effect estimates. Ten of these studies were from the US, two from Australia [20],[21], one from Sweden [22], one from India [23], one from Nicaragua [24], and one from South Africa [25]. Three studies from the US [13],[26],[27] included adolescents and focused on dating violence; all of the other studies focused on IPV in adults. Four studies sampled participants from secondary schools [13],[22],[26],[27], four studies were individual or household surveys of the general population [20],[21],[23],[28], one was conducted at a college [29], one was conducted among hospital employees [30], and three sampled from a variety of venues [25],[31],[32]. The three remaining studies recruited pregnant women, two from hospitals [33],[34] and one from households in the general population [24]. Details of study characteristics are described in Table S1.
The median follow-up time was 36 mo (interquartile range 12–60 mo) (range 2 mo [29] to 14 y [31]). Median attrition rate was 22.5% (interquartile range 17%–28.6%) (range 4.5% [31] to 57.1% [34]). Ten studies made use of two waves of data collection, two had three waves [23],[34], two had four waves [26],[30], one had five waves [33], and one had 14 [31]. The majority of studies included only female participants; the four studies that recruited from secondary schools also included males.
IPV measurement and potential misclassification
Nearly all (14 of 16) studies used measures of experience of specific acts of violence based in whole or in part on the Conflict Tactics Scale [35] or the World Health Organization instrument [24],[25]; one was based on the Abuse Assessment Screen [30] and one on the Severity of Violence Against Women Scales [33]. All of these instruments measure self-reported experience of specific acts of violence, for example, “Have you ever been slapped, punched, kicked, hit with an object”, and so on. Although measuring specific acts avoids misclassification associated with participants having different perceptions of whether what they have experienced constitutes “violence” or not [2], nearly half of all studies (six studies; seven papers) measured exposure to physical violence or sexual violence only [13],[28],[29],[31],[36],[37], leaving open the possibility of substantial misclassification of total violence exposure. Loxton et al. asked only if the respondent had “been in a violent relationship with a spouse” [20] and Jonsson et al. asked if participants “had ever been physically abused or had their life threatened” [22].
Depression
Sixteen studies (reported in 17 papers—two papers used data from Add Health [13],[37]) provided 47 estimates of association between IPV and depressive symptoms or disorder. Forty-one estimates from 16 studies were for women, and six estimates from four studies were for male populations. Taking only the least biased estimate from each study gives 23 estimates from 16 studies. These 23 estimates are outlined in Table 1 and considered below; more detailed study information, including other effect estimates, is presented in Table S1.
Tab. 1. Summary of studies of depression and IPV, in women. 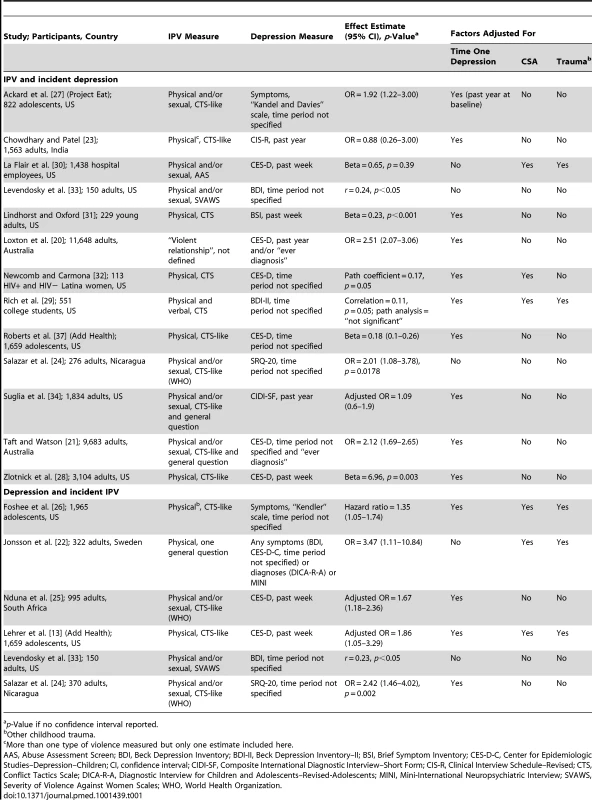
p-Value if no confidence interval reported. Depression measurement
Of the 16 studies included, eight measured depressive symptoms over a defined time period (five were over the 1 wk prior to the survey, three were over the past year, and the remainder did not specify). Seven studies used the Center for Epidemiologic Studies Depression Scale (CES-D) [13],[20],[21],[25],[28],[30],[36], two used the Beck Depression Inventory [29],[33], one used the Self-Report Questionnaire–20 (SRQ-20) [24], one used the Brief Symptom Inventory [31], one used the Composite International Diagnostic Interview–Short Form [34], one used a scale from K. S. Kendler [26], and one used a scale from D. B. Kandel and M. Davies [27]. The one study that measured incident depressive disorders [23] used the Clinical Interview Schedule–Revised. Jonsson et al. used the CES-D and Beck Depression Inventory but also the Diagnostic Interview for Children and Adolescents–Revised–Adolescents and the Mini-International Neuropsychiatric Interview. All measures were combined for analysis [22].
Common risk factors/confounding
Of the estimates for women, presented in Table 1, most were adjusted for time one measures of the outcome, but five estimates were unadjusted. Chowdhary and Patel [23] excluded lifetime suicide and depressive disorder diagnosis at baseline from analyses; however, this likely resulted in the exclusion of many cases of violence that preceded suicide attempts or depressive symptoms or disorder at baseline—the resulting cases of violence being few and not representative of women experiencing IPV. Nearly all studies (14 of 16) also controlled for demographic factors, but in general, other confounders were not comprehensively controlled. Often the estimates included in the meta-analyses, only two controlled for CSA and/or other early life experiences [13],[22]. None controlled for alcohol use. Of the seven studies not included in the meta-analyses (those with continuous measures of depression), 5/7 controlled for demographic factors [28]–[31],[37], but only 2/7 for CSA [29],[30], one for early life factors [30], and one for early risk behaviour [37]. Despite these differences in variables controlled for across analyses, there were no discernible differences in effect estimates: regardless of which confounders were adjusted for, all studies found similar directions and varying magnitudes of association. For men (Table 2), the picture was similar: most studies adjusted for time one levels of the outcome, but other key confounders were not adjusted for.
Tab. 2. Summary of studies of depression and IPV, in men. 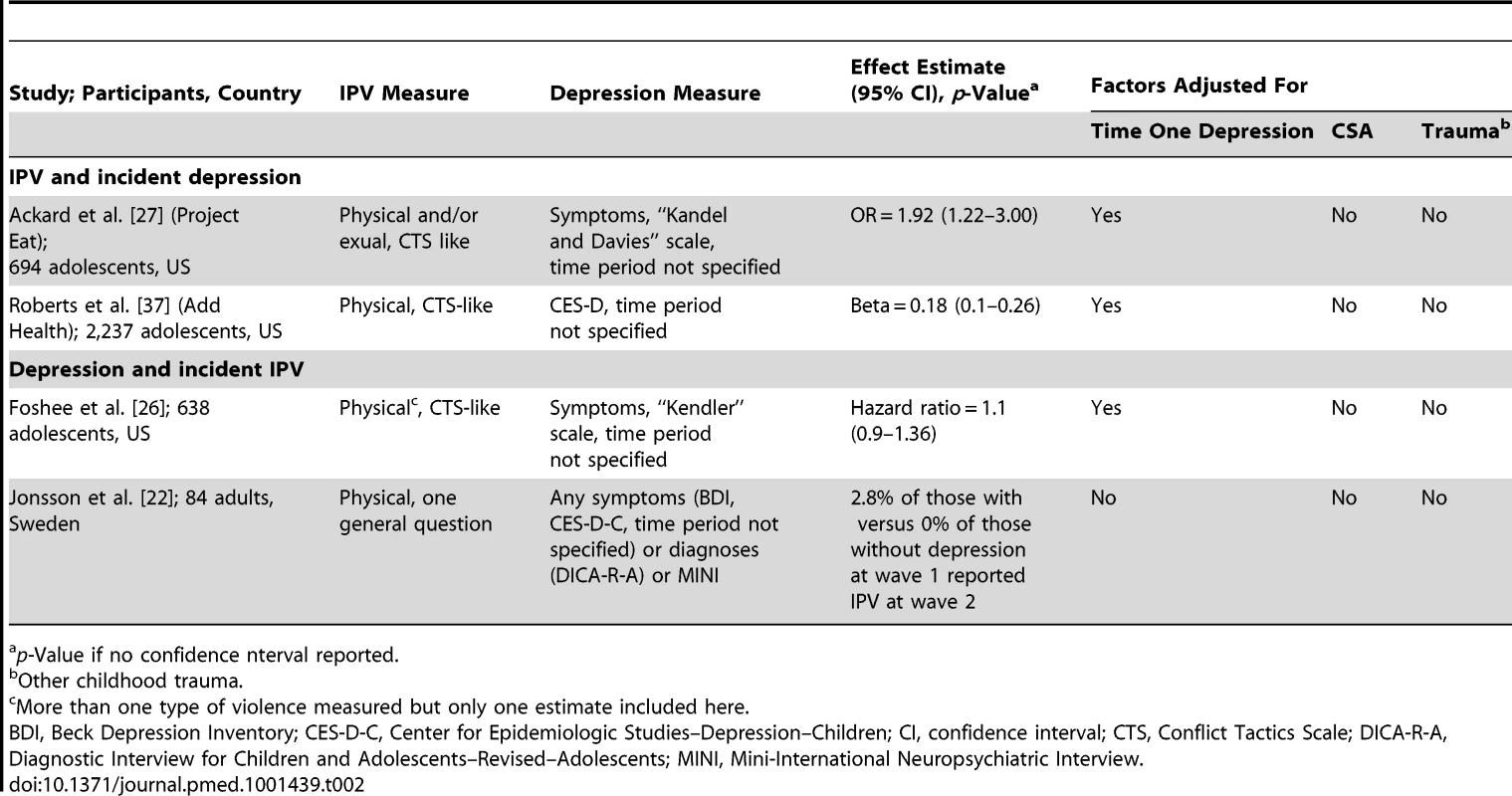
p-Value if no confidence nterval reported. Effect estimates for depressive disorder and symptoms in women
Of the 16 studies looking at depressive symptoms or disorder and IPV in women, 13 provided estimates of IPV and incident depressive symptoms or disorder and six provided estimates of depressive symptoms and incident IPV (Table 1). Twelve of 13 estimates showed a positive direction of association between experience of IPV and incident depressive symptoms, with 11 reaching statistical significance. All six estimates looking at depressive symptoms and incident IPV also showed positive associations, which were statistically significant.
We were able to include all estimates reporting binary violence measures and binary depressive symptoms or disorder measures in meta-analyses (Figure 2). For IPV and incident depressive symptoms or disorder, the pooled OR from six estimates was 1.97 (95% CI 1.56–2.48). This was heterogeneous (I2 = 50.4%, p = 0.073), although almost all studies had a positive direction of effect. Removing the outlier (Chowdhary and Patel [23]) did not improve heterogeneity estimates. Four estimates were included in the meta-analysis of the relationship between depressive symptoms and incident IPV, resulting in a pooled OR of 1.93 (95% CI 1.51–2.48, I2 = 0%, p = 0.481).
Fig. 2. Meta-analyses of the association between IPV and depressive symptoms or disorder in women. 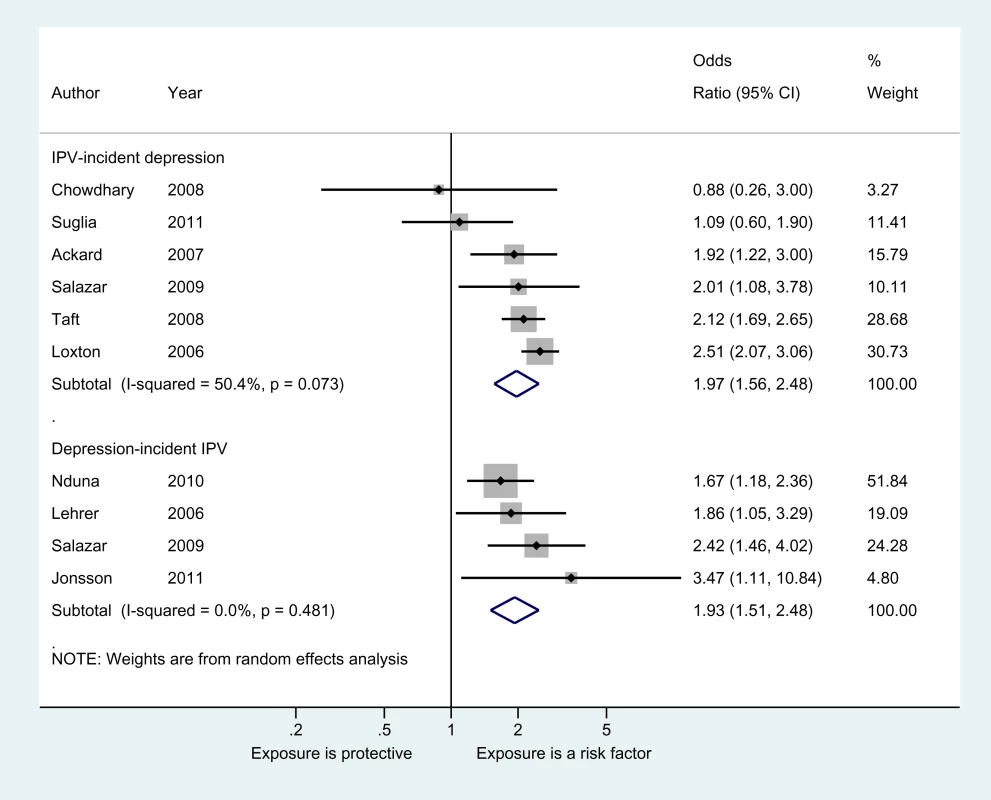
Effect estimates for depressive symptoms in men
For men (Table 2), two studies [27],[37] examined experience of IPV and incident depressive symptoms, and both studies showed a significant association in a positive direction. Foshee et al. examined depressive symptoms and time to onset of physical and sexual victimisation, as well as “chronic victimisation”, and found non-significant relationships in a positive direction (bivariate model) [26]. Jonsson et al. found that 2.5% of adult men reporting depressive symptoms as adolescents also reported adult experiences of IPV, versus 0% of adult men who did not report depressive symptoms in adolescence [22].
Suicide Attempts
Three studies investigating suicide attempts met our inclusion criteria [23],[27],[37]. These studies reported eight estimates of association of experience of IPV with incident suicidal attempts. Six were for female populations, and two were for male populations. Ackard et al. and Roberts et al. both sampled US adolescents and the IPV measured was dating violence (for both male and female adolescents) [27],[37]. Chowdhary and Patel sampled a cohort of adults from Goa, India, comprising adult women only [23]. No studies examined suicide attempts and incident IPV.
Suicide measures
All studies modelled lifetime suicide attempts as a binary variable, and assessed attempts with a single question. No studies had completed suicides as an outcome.
Common risk factors/confounding
Ackard et al. [27] and Roberts et al. [37] controlled for time one suicide attempts; Chowdhary and Patel [23] excluded participants with lifetime suicide attempts at baseline. None controlled for early life factors, including experience of CSA.
Effect estimates for suicide attempts in women
Chowdhary and Patel [23], Ackard et al. [27], and Roberts et al. [37] examined violence and incident suicide attempts: all three studies showed positive relationships, of which two were statistically significant and one was of borderline significance (Table 3).
Tab. 3. Summary of studies of suicide and IPV, in women. 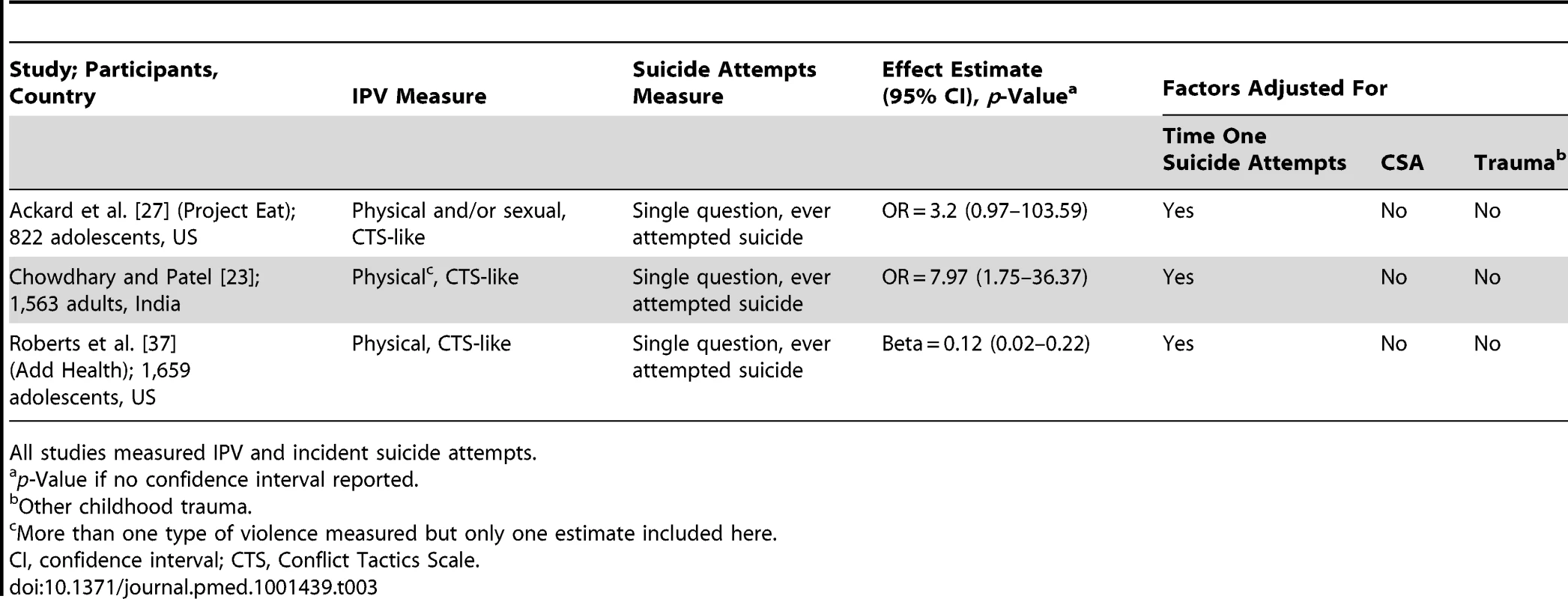
All studies measured IPV and incident suicide attempts. Effect estimates for suicide attempts in men
Two studies examined violence and incident suicide attempts [27],[37]: both found non-significant relationships, one in a positive direction and the other with exactly no association (Table 4). Both of these studies included adolescent or young adult US men; both also controlled for time one suicide attempts.
Tab. 4. Summary of studies of suicide and IPV, in men. 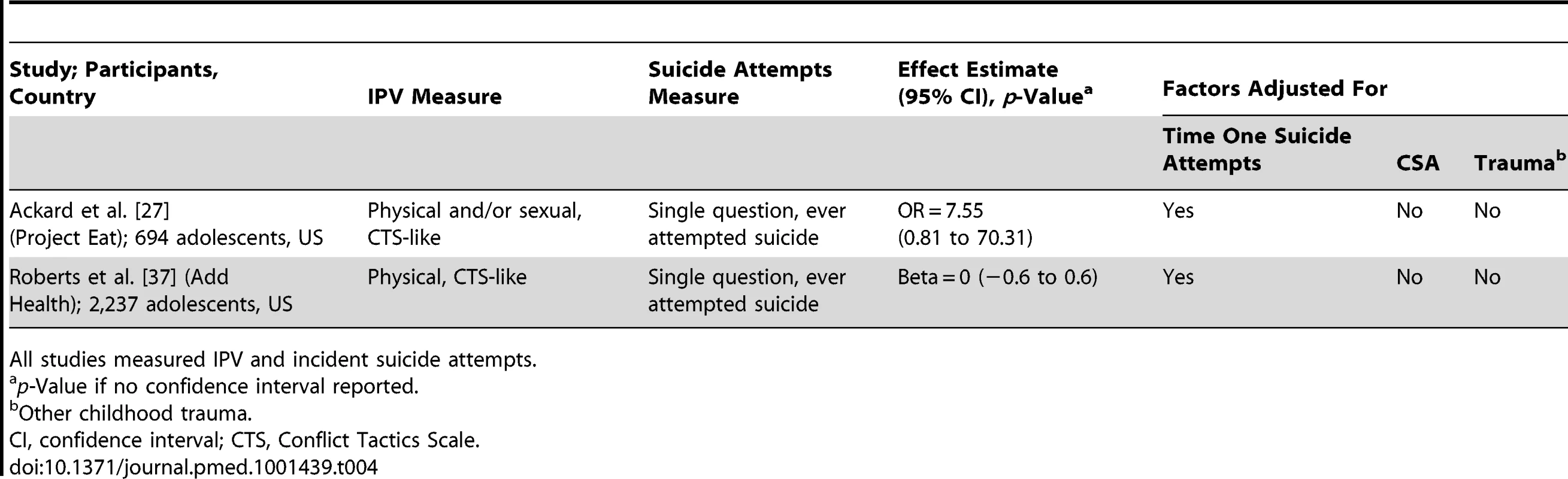
All studies measured IPV and incident suicide attempts. Discussion
Summary of Main Findings
Our review provides evidence that experience of IPV increases the odds of incident depressive symptoms and of suicide attempts among women. We also found evidence that depressive symptoms can increase the odds of incident IPV in women. However, our ability to draw firm conclusions is limited by the quality of the available studies, in particular the lack of adjustment for common risk factors. Relatively few studies included men, but these studies suggested a relationship between IPV and incident depressive symptoms. For men, there was no clear evidence of an association between IPV and incident suicide attempts, or between depressive symptoms and incident IPV.
Limitations of This Review
Our review employed extensive searches of global literature in multiple languages. Despite this, our review has some limitations. Because of the large volume of search results returned, we were unable to employ double screening of abstracts, and for our update, double data extraction. We also did not contact authors for additional information. The different scales of measurement (binary or continuous) employed across various studies meant that we were unable to combine all measures of effect, which limited the number of studies in our meta-analyses. However, studies that we could not include in meta-analyses showed a positive direction of effect consistent with that of the studies included in the meta-analyses. Too few studies met the inclusion criteria to meaningfully assess publication bias.
Sources of Bias and Limitations of Included Studies
The main limitation of included studies relates to lack of comprehensive control of potential confounders. Both IPV and depression can be conceptualised as chronic episodic conditions, and most studies controlled for time one levels of the outcome variable or excluded baseline cases in their analyses. However, alcohol use and childhood adversity, including early experiences of violence and trauma, were generally not controlled for, making it difficult to rule out these other factors as contributors to the causation of outcomes. We did find that studies generally showed a positive direction of association regardless of which potentially confounding variables were adjusted for, and there was also no clear pattern of differing magnitude of association, indicating that the relationships between IPV and depressive symptoms and suicide are not likely to be entirely accounted for by shared risk factors.
Almost all included studies on depression measured depressive symptoms rather than major depressive disorder, dysthymia, or other depressive disorders using Diagnostic and Statistical Manual of Mental Disorders or International Classification of Diseases diagnostic criteria. Only around one-third to one-half of people who score above recommended CES-D cutoffs are diagnosed with major depressive disorder [38],[39]. The relationship between violence experience and depressive disorders may differ from the relationship between violence experience and depressive symptoms. Major depressive disorder has a substantial heritability [40] and has been shown to be more heritable than less severe forms of depression [41]; situational causes such as violence may therefore play a more important etiological role in the less severe forms of depression. Conversely, experiences of violence may predict more severe depression and thus have a stronger association with depressive disorders than with depressive symptoms. When examining violence in relation to depression, including subthreshold depressive symptoms and depressive disorders could either dilute or inflate effect estimates.
Most studies were from high-income countries, and four were of adolescents or college students. In high-income contexts, in these samples, relationships will be primarily in dating relationships. In dating relationships where there is no cohabitation, there may be a lower likelihood of chronic exposure to violence within the intimate partnership [42],[43], which may lessen any subsequent mental health impact. Other studies of the features of intimate partner abuse have shown that fear, entrapment, and feelings of inability to escape from violent situations specifically contribute to increased adverse mental health outcomes [42]—these relationship features are likely to be less pronounced in dating relationships, which could mean that effects are underestimated in studies including only adolescents.
Emotional violence, which we did not include here, may also be an important predictor of adverse mental health outcomes [44]. The epidemiological study of emotional IPV is in its infancy, but at least one study that has modelled combined measures of physical, sexual, and emotional IPV has shown a relationship between these forms of abuse and incident suicide attempts in Indian women [45].
Most studies also measured exposure only to physical violence, or modelled exposure to physical violence and sexual violence separately. Most studies constructed reference categories as binary opposites, meaning that some participants in the reference group may have been exposed to other forms of violence by intimate partners that were not measured or modelled. This approach may bias the effect estimates towards the null, and underestimate the magnitude of the association between violence experience and depression outcomes. Several studies also included only women who were in relationships for all time points of data collection. The prevalence of IPV is usually higher in women who no longer have a partner versus women currently in a partnership (for example, [46]). Not including these women may bias associations towards the null. Similarly, it is conceivable that women who are no longer in a partnership may have higher or lower odds of depression/suicide attempts. If they are not surveyed in subsequent waves, associations may be biased in different directions.
Is the Relationship between IPV, Depression, and Suicide Causal?
Cross-sectional evidence suggests that lifetime experience of IPV is consistently associated with both SRQ-20 score (representing probable cases of depression and/or anxiety) [4] and suicide attempts among women in a range of low - and middle-income countries [3]. Several studies have shown a dose–response relationship, where IPV is associated with increased frequency of depressive episodes [20], and other studies have shown that depression is more strongly predictive of incident severe IPV than it is of less severe IPV [13]. Twin studies provide evidence for a plausible causal mechanism, that exposure to traumatic events, including sexual assault and violence, can cause increased risk of depression, ruling out early life confounders [10],[18].
Our review presents evidence for a temporal relationship between IPV experience and depressive symptoms, but also shows that women with existing depressive symptoms are more likely to subsequently experience IPV. Our finding is consistent with other longitudinal studies that have considered combined measures of IPV perpetration and experience, which found that women with depression were more likely to be in an abusive relationship, but also that being in an abusive relationship predicted incident major depressive disorder [47]. In summary, it seems that the relationship between IPV and depression is bidirectional, with women who are exposed to IPV being at increased risk of depression symptoms, and women who report depressive symptoms being more likely to subsequently experience IPV. For young men, we found no clear evidence of a relationship between IPV, depressive symptoms, and suicide, but very few studies included men. Further studies that include male participants are needed to clearly establish whether or not there is an association.
Implications
The different forms of depression—major depressive disorder, dysthymia, and mild depression—as well as suicidal behaviour, are some of the largest causes of disease burden in women globally. Our findings suggest that interventions to prevent violence need to be explored for their efficacy in reducing different forms of depression. Similarly, for women already receiving mental health treatments or presenting with symptoms of depression, attention must be paid to experiences of violence and risk of future violence. Because IPV often occurs as a pattern of ongoing events [43], treatment strategies that fail to address womens' experience of violence may do harm. For example, if violence is not suspected as a potential causative factor, patients who have attempted suicide may be encouraged to return to partners/relatives, which could increase the risk of further violence and eventual suicide [48]. Anti-depressant medication may also interfere with women's ability to make decisions about how to respond to violence [49].
Further research is needed to explore why having depressive symptoms can lead to incident violence—it may be that young women with depressive symptoms are predisposed to choose partners who use violence. Depression can also lead to maladaptive coping with stress, cognitive distortions about risk, and loss of self-efficacy. Young people who have experienced early traumatic events, including violence in their families, are at higher risk for poor mental health as adolescents [50]. Longitudinal studies where both violence exposure and depression are measured at multiple time points are needed to more clearly elucidate causal mechanisms. It is clear that addressing the burden of untreated mental disorders in a population could have substantial effects on the prevalence of violence.
Conclusion
Interventions to prevent violence should be explored for their efficacy in reducing the burden of depressive symptoms and disorders as well as suicide attempts in women. Women who have experienced violence may benefit from tailored interventions that address the changes that come with prolonged exposure to trauma in order to prevent future depression and suicidal behaviour.
Supporting Information
Zdroje
1. RibeiroPS, JacobsenKH, MathersCD, Garcia-MorenoC (2008) Priorities for women's health from the Global Burden of Disease study. Int J Gynecol Obstet 102 : 82–90.
2. Garcia-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C (2005) WHO multi-country study on women's health and domestic violence against women. Geneva: World Health Organization.
3. DevriesKM, KissL, WattsC, YoshihamaM, DeyessaN, et al. (2011) Violence against women is strongly associated with suicide attempts: evidence from the WHO multi-country study on women's health and domestic violence against women. Soc Sci Med 73 : 79–86.
4. EllsbergM, JansenHAFM, HeiseL, WattsCH, Garcia-MorenoC, et al. (2008) Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet 371 : 1165–1172.
5. BeydounHA, BeydounM, KaufmanJS, LoB, ZondermanAB (2012) Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Soc Sci Med 75 : 959–975.
6. DeyessaN, BerhaneY, AlemA, EllsbergM, EmmelinM, et al. (2009) Intimate partner violence and depression among women in rural Ethiopia: a cross-sectional study. Clin Pract Epidemiol Ment Health 5 : 8.
7. BonomiAE, AndersonML, ReidR, RivaraFP, CarrellD, et al. (2009) Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Int Med 169 : 1692–1697.
8. BreidingMJ, BlackMC, RyanGW (2008) Prevalence and risk factors of intimate partner violence in eighteen U.S. states/territories, 2005. Am J Prev Med 34 : 112–118.
9. HydeJS, MezulisAH, AbramsonLY (2008) The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev 115 : 291–313.
10. KendlerKS, ThorntonLM, PrescottCA (2001) Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry 157 : 587–593.
11. KhalifehH, DeanK (2010) Gender and violence against people with severe mental illness. Int Rev Psychiatry 22 : 535–546.
12. McPhersonM, DelvaJ, CranfordJA (2007) A longitudinal investigation of intimate partner violence among mothers with mental illness. Psychiatr Serv 58 : 675–680.
13. LehrerJA, BukaS, GortmakerS, ShrierLA (2006) Depressive symptomatology as a predictor of exposure to intimate partner violence among US female adolescents and young adults. Arch Pediatr Adolesc Med 160 : 270–276.
14. BifulcoA, KwonJ, JacobsC, MoranPM, BunnA, et al. (2006) Adult attachment style as mediator between childhood neglect/abuse and adult depression and anxiety. Soc Psychiatry Psychiatr Epidemiol 41 : 796–805.
15. DoumasDM, PearsonCL, ElginJE, McKinleyLL (2008) Adult attachment as a risk factor for intimate partner violence: the “mispairing” of partners' attachment styles. J Interpers Violence 23 : 616–634.
16. BanyardVL, WilliamsLM, SiegelJA (2001) The long-term mental health consequences of child sexual abuse: an exploratory study of the impact of multiple traumas in a sample of women. J Trauma Stress 14 : 697–715.
17. MelhemN, BrentD, ZieglerM, IyengarS, KolkoD, et al. (2007) Familial pathways to early-onset suicidal behaviour: familial and individual antecedents of suicidal behaviour. Am J Psychiatry 164 : 1364–1370.
18. KendlerKS, KarkowskiLM, PrescottCA (1999) Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry 156 : 837–841.
19. The Global Burden of Disease Study 2010. Lancet 380 : 2053–2260.
20. LoxtonD, SchofieldM, HussainR (2006) Psychological health in midlife among women who have ever lived with a violent partner or spouse. J Interpers Violence 21 : 1092–1107.
21. TaftAJ, WatsonLF (2008) Depression and termination of pregnancy (induced abortion) in a national cohort of young Australian women: the confounding effect of women's experience of violence. BMC Public Health 8 : 75.
22. JonssonU, BohmanH, HjernA, von KnorringL, PaarenA, et al. (2011) Intimate relationships and childbearing after adolescent depression: a population-based 15 year follow-up study. Soc Psychiatry Psychiatr Epidemiol 46 : 711–721.
23. ChowdharyN, PatelV (2008) The effect of spousal violence on women's health: findings from the Stree Arogya Shodh in Goa, India. J Postgrad Med 54 : 306–312.
24. SalazarM, ValladaresE, OhmanA, HogbergU (2009) Ending intimate partner violence after pregnancy: findings from a community-based longitudinal study in Nicaragua. BMC Public Health 9 : 350.
25. NdunaM, JewkesRK, DunkleKL, ShaiNP, ColmanI (2010) Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. J Int AIDS Soc 13 : 44.
26. FosheeVA, BenefieldTS, EnnettST, BaumanKE, SuchindranC (2004) Longitudinal predictors of serious physical and sexual dating violence victimization during adolescence. Prev Med 39 : 1007–1016.
27. AckardDM, EisenbergME, Neumark-SztainerD (2007) Long-term impact of adolescent dating violence on the behavioral and psychological health of male and female youth. J Pediatr 151 : 476–481.
28. ZlotnickC, JohnsonDM, KohnR (2006) Intimate partner violence and long-term psychosocial functioning in a national sample of American women. J Interpers Violence 21 : 262–275.
29. RichCL, GidyczC, WarkentinJ, LohcC, WeilandP (2005) Child and adolescent abuse and subsequent victimization: a prospective study. Child Abuse Negl 29 : 1373–1394.
30. La FlairLN, BradshawCP, CampbellJC (2011) Intimate partner violence/abuse and depressive symptoms among female health care workers: longitudinal findings. Womens Health Issues 22: e53–e59.
31. LindhorstT, OxfordM (2008) The long-term effects of intimate partner violence on adolescent mothers' depressive symptoms. Soc Sci Med 66 : 1322–1333.
32. NewcombMD, CarmonaJV (2004) Adult trauma and HIV status among Latinas: effects upon psychological adjustment and substance use. AIDS Behav 8 : 417–428.
33. LevendoskyAA, BogatGA, Huth-BocksAC, RosenblumK, von EyeA (2011) The effects of domestic violence on the stability of attachment from infancy to preschool. J Clin Child Adolesc Psychol 40 : 398–410.
34. SugliaSF, DuarteCS, SandelMT (2011) Housing quality, housing instability, and maternal mental health. J Urban Health 88 : 1105–1116.
35. StrausM, DouglasE (2004) A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence Vict 19 : 507–520.
36. NewcombMD, MunozDT, CarmonaJV (2009) Child sexual abuse consequences in community samples of Latino and European American adolescents. Child Abuse Negl 33 : 533–544.
37. RobertsTA, KleinJD, FisherS (2003) Longitudinal effect of intimate partner abuse on high-risk behavior among adolescents. Arch Pediatr Adolesc Med 157 : 875–881.
38. ThomasJL, JonesGN, ScarinciIC, MehanDJ, BrantleyPJ (2001) The utility of the CES-D as a depression screening measure among low-income women attending primary care clinics. The Center for Epidemiologic Studies-Depression. Int J Psychiatry Med 31 : 25–40.
39. BreslauN (1985) Depressive symptoms, major depression, and generalized anxiety: a comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatr Res 15 : 219–229.
40. SullivanPF, NealeMC, KendlerKS (2000) Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry 157 : 1552–1562.
41. LyonsMJ, EisenSA, GoldbergJ, TrueW, LinN, et al. (1998) A registry-based twin study of depression in men. Arch Gen Psychiatry 55 : 468–472.
42. BrowneA (1993) Violence against women by male partners: prevalence, outcomes, and policy implications. Am Psychol 48 : 1077–1087.
43. JohnsonMP (1995) Patriarchal terrorism and common couple violence: two forms of violence against women. J Marriage Fam 57 : 283–294.
44. JewkesR (2010) Gender inequities must be addressed in HIV prevention. Science 329 : 145–147.
45. MaselkoJ, PatelV (2008) Why women attempt suicide: the role of mental illness and social disadvantage in a community cohort study in India. J Epidemiol Community Health 62 : 817–822.
46. Nyamayemombe C, Mishra V, Rusakaniko S, Benedikt C, Gwazane M, et al.. (2010) The association between violence against women and hiv: evidence from a national population-based survey in Zimbabwe. Calverton (Maryland): ICF Macro.
47. EhrensaftMK, MoffittTE, CaspiA (2006) Is domestic violence followed by an increased risk of psychiatric disorders among women but not among men? A longitudinal cohort study. Am J Psychiatry 163 : 885–892.
48. Stark E, Flitcraft A (1996) Women at risk: domestic violence and women's health. Thousand Oaks (California): Sage.
49. WuestJ, Ford-GilboeM, Merritt-Gray, BermanH (2003) Intrustion: the central problem for family health promotion among children and single mothers after leaving an abusive partner. Qual Health Res 13 : 597.
50. DubeSR, AndaRF, FelittiVJ, ChapmanDP, WilliamsonDF, et al. (2001) Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span. Findings from the Adverse Childhood Experiences Study. JAMA 286 : 3089–3096.
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2013 Číslo 5- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
- Ferinject: správně indikovat, správně podat, správně vykázat
- Optimální dávkování apixabanu v léčbě fibrilace síní
-
Všechny články tohoto čísla
- Measuring Coverage in MNCH: Challenges and Opportunities in the Selection of Coverage Indicators for Global Monitoring
- Measuring Coverage in MNCH: Tracking Progress in Health for Women and Children Using DHS and MICS Household Surveys
- Measuring Coverage in MNCH: Population HIV-Free Survival among Children under Two Years of Age in Four African Countries
- Tobacco Company Efforts to Influence the Food and Drug Administration-Commissioned Institute of Medicine Report An Analysis of Documents Released through Litigation
- Irreconcilable Conflict: The Tobacco Industry and the Public Health Challenge of Tobacco Use
- Providing Impetus, Tools, and Guidance to Strengthen National Capacity for Antimicrobial Stewardship in Viet Nam
- Measuring Coverage in MNCH: New Findings, New Strategies, and Recommendations for Action
- Grand Challenges: Integrating Maternal Mental Health into Maternal and Child Health Programmes
- Measuring Coverage in MNCH: Challenges in Monitoring the Proportion of Young Children with Pneumonia Who Receive Antibiotic Treatment
- Measuring Coverage in MNCH: Current Indicators for Measuring Coverage of Diarrhea Treatment Interventions and Opportunities for Improvement
- Measuring Coverage in MNCH: Evaluation of Community-Based Treatment of Childhood Illnesses through Household Surveys
- Measuring Coverage in MNCH: Accuracy of Measuring Diagnosis and Treatment of Childhood Malaria from Household Surveys in Zambia
- Grand Challenges: Integrating Mental Health Care into the Non-Communicable Disease Agenda
- Integrating Global and National Knowledge to Select Medicines for Children: The Ghana National Drugs Programme
- Grand Challenges: Integrating Mental Health Services into Priority Health Care Platforms
- Disability Transitions and Health Expectancies among Adults 45 Years and Older in Malawi: A Cohort-Based Model
- Comparative Efficacy of Seven Psychotherapeutic Interventions for Patients with Depression: A Network Meta-Analysis
- Measuring Coverage in MNCH: Design, Implementation, and Interpretation Challenges Associated with Tracking Vaccination Coverage Using Household Surveys
- Measuring Coverage in MNCH: A Prospective Validation Study in Pakistan and Bangladesh on Measuring Correct Treatment of Childhood Pneumonia
- Contribution of and Smoking Trends to US Incidence of Intestinal-Type Noncardia Gastric Adenocarcinoma: A Microsimulation Model
- Carriage of in the Upper Respiratory Tract of Symptomatic and Asymptomatic Children: An Observational Study
- Setting Research Priorities to Reduce Mortality and Morbidity of Childhood Diarrhoeal Disease in the Next 15 Years
- Grand Challenges: Improving HIV Treatment Outcomes by Integrating Interventions for Co-Morbid Mental Illness
- Gene Expression Classification of Colon Cancer into Molecular Subtypes: Characterization, Validation, and Prognostic Value
- Domestic Violence and Perinatal Mental Disorders: A Systematic Review and Meta-Analysis
- Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies
- Effect of Facilitation of Local Maternal-and-Newborn Stakeholder Groups on Neonatal Mortality: Cluster-Randomized Controlled Trial
- Intimate Partner Violence and Population Mental Health: Why Poverty and Gender Inequities Matter
- Assessing Population Aging and Disability in Sub-Saharan Africa: Lessons from Malawi?
- The Paradox of Mental Health: Over-Treatment and Under-Recognition
- Measuring Coverage in MNCH: Determining and Interpreting Inequalities in Coverage of Maternal, Newborn, and Child Health Interventions
- Measuring Coverage in MNCH: Total Survey Error and the Interpretation of Intervention Coverage Estimates from Household Surveys
- Measuring Coverage in MNCH: Indicators for Global Tracking of Newborn Care
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Gene Expression Classification of Colon Cancer into Molecular Subtypes: Characterization, Validation, and Prognostic Value
- Domestic Violence and Perinatal Mental Disorders: A Systematic Review and Meta-Analysis
- Intimate Partner Violence and Incident Depressive Symptoms and Suicide Attempts: A Systematic Review of Longitudinal Studies
- Measuring Coverage in MNCH: Challenges in Monitoring the Proportion of Young Children with Pneumonia Who Receive Antibiotic Treatment
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Revma Focus: Spondyloartritidy
nový kurz
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



