-
Články
Top novinky
Reklama- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
Top novinky
Reklama- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Top novinky
ReklamaChanged Eye Functions and Quality of Life of Seniors with Diabetic Retinopathy
Authors: Ľ. Majerníková 1; A. Hudáková 1; M. Kaščáková 1; A. Obročníková 1
Authors place of work: Prešovská univerzita v Prešove, Fakulta zdravotníckych odborov, Katedra ošetrovateľstva 1
Published in the journal: Čes. a slov. Oftal., 76, 2020, No. 6, p. 266-271
Category: Původní práce
doi: https://doi.org/10.31348/2020/37Summary
Aim. To monitor and evaluate the differences in the evaluation of monitored indicators of quality of life of patients with proliferative and non-proliferative diabetic retinopathy (DR).
Methods. The research sample comprised a total of 80 patients with DR.The first group consisted of 27 patients with proliferative diabetic retinopathy and the second group of 53 patients with non-proliferative diabetic retinopathy. The comparison was carried out according to the degree of DR. The data were collected using the standardized National Eye Institute Visual Function Questionnaire (NEI VFQ-25).
Results. In both compared patient groups, T-tests showed significant differences in all studied quality of life parameters: general health and vision, difficulty seeing far away and up close, the impact of the disease on achieving life goals, being limited in control over and in length of their activities, being limited to their homes, relying on the information provided by other people and needing help from others.
Conclusion. In a holistic concept, i.e. biological, psychological and social dimensions, partial or complete loss of the ability to see due to diabetes has a negative impact on the quality of life of patients with proliferative DR. Therefore, this chronic complication must be prevented by any available means.
Keywords:
Vision – visual impairment – Diabetic retinopathy – Quality of life
INTRODUCTION
Diabetic retinopathy (DR) represents a serious risk of a deficit of visual functions. The level of hyperglycaemia is evaluated as the main and high risk factor, relating to types 1 and 2 diabetes [1]. Other mechanisms that worsen the prognosis of DR include hypertension and hyperlipidaemia [2]. The development of changes in the eye as a consequence of hyperglycaemia is dependent on several factors, and according to severity is divided into three clinical stages and one subclinical, “fluorophotometric” stage [3].
It is necessary to view the quality of life of patients with DR from two closely linked perspectives, in which we include the aspect of life with restrictions in connection with general compensation of diabetes mellitus (DM) and the aspect of life with visual affliction with all its consequences on overall quality of life. Damage to the retinal blood vessels as a consequence of DM, especially if it is linked with a temporary or permanent reduction of visual functions, brings about an entirely new life situation, a new problem in the life of the patient with DM and his or her family, which in some cases can be managed only with great difficulty [4]. Statistical indicators confirm that in developed countries, DR and its severe complications are the most common cause of newly occurring loss of vision in persons aged up to 74 years of age. Upon duration of DM for longer than 20 years DR affects 80-100 % of patients with type 1 DM, and more than 60 % of those with type 2 DM [5]. For the above reasons, an evaluation and analysis of quality of life of patients with DR is necessary for timely and effective intervention.
The aim of the study was to monitor and determine differentiations in the evaluation of the influence of visual functions on quality of life in selected senior citizens with DR. We wished to monitor the influence of damage to visual functions in connection with colour and peripheral vision in relation to DR in the examined sample and assess the use of the tool used to verify quality of life in connection with health.
Method and cohort
For the purposes of the planned investigation, a total of 80 standardised National Eye Institute Visual Function Questionnaires (NEI VFQ – 25) were distributed to patients with DR [6]. The used questionnaire is designated for the evaluation of visual functions using the criterion of the Likert scale. The questionnaire consists of 25 questions focusing on seven basic areas, assessing the following: general condition of health and sight, problems in activities using near and distance vision, problems in peripheral and colour vision, social functions, psychological problems and experience, and reaction to problems due to affliction of vision [7]. The questionnaires were distributed via the angiology outpatient centre of the department of ophthalmology at the J. A. Reiman University Hospital in Prešov. The return rate of the questionnaires was 100 %, due to the fact that their completion took place in the form of an individually structured interview between a researcher and each patient selectively. The questionnaire NIE VFQ – 25 and the manual are freely available on the internet. For the purposes of use we met the required criteria from the authors of the questionnaire, with the consent of the ethical commission.
The research sample comprised 80 patients with DM, in whom DR had been diagnosed. For the purposes of statistical comparison we divided the patients into two groups. The first group was composed of 27 patients with proliferative diabetic retinopathy (PDR), and the second group of 53 patients with non-proliferative diabetic retinopathy (NPDR). Despite the fact that the division of the groups shows minimal signs of homogeneity, we needed to preserve a certain authenticity of patients with regard to adhering to their current number.
The demographic data from our study provides information about sex, length of treatment of DM and ocular complications in connection with the type of DR.
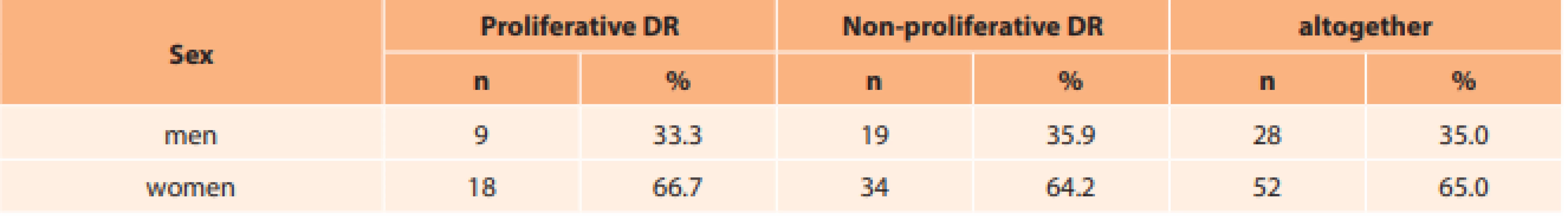
The participants in the study were 9 men (33.3 %) and 18 women (66.7 %) with PDR, and 19 men (35.9 %) and 34 women (64.2 %) with NPDR. There was an overall predominance of the female population in the research, with 52 women (65.0 %) and 28 men (35.0 %) (Table 1).
PDR with a duration of 5-10 years was stated in 3 patients (11.1 %), a duration of 11-20 years in 6 (22.2 %) and of 21-40 years in 18 patients (66.7 %). None of the patients had been treated for > 41 years. NPDR with a duration of 5-10 years was stated in 10 patients (18.9 %), of 11-20 years in 26 (49.1 %) and 21-40 years in 16 patients (30.2 %). Only one respondent had been treated for NPDR for > 41 years (1.9 %) (Table 2).
Tab. 2. Length of treatment for diabetes 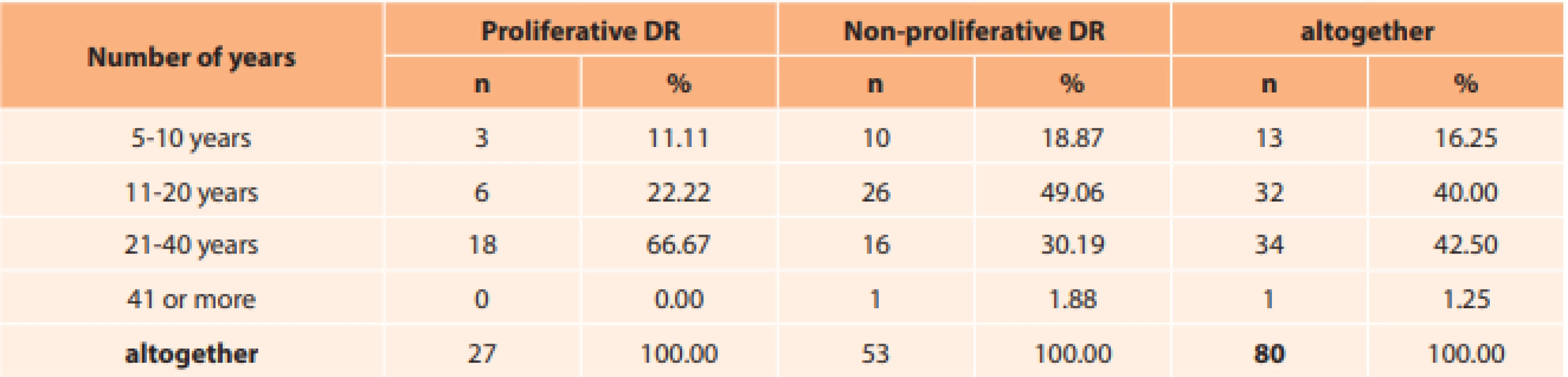
Regarding ocular complications upon a background of PDR, 9 patients (33.3 %) had been observed for a period of 5-10 years, 15 patients (55.6 %) for 11-20 years and 3 patients (11.1 %) for 21-40 years. For ocular complications upon a background of NPDR, 47 patients (88.7 %) were evaluated with a duration of 5-10 years, 5 patients (9.4 %) with a duration of 11-20 years and 1 patient (1.9 %) with a duration of 21-40 years. No patients were represented in the category of 41 or more years either in the category of PDR or NPDR (Table 3).
Tab. 3. Length of treatment for ocular complications as a consequence of diabetes 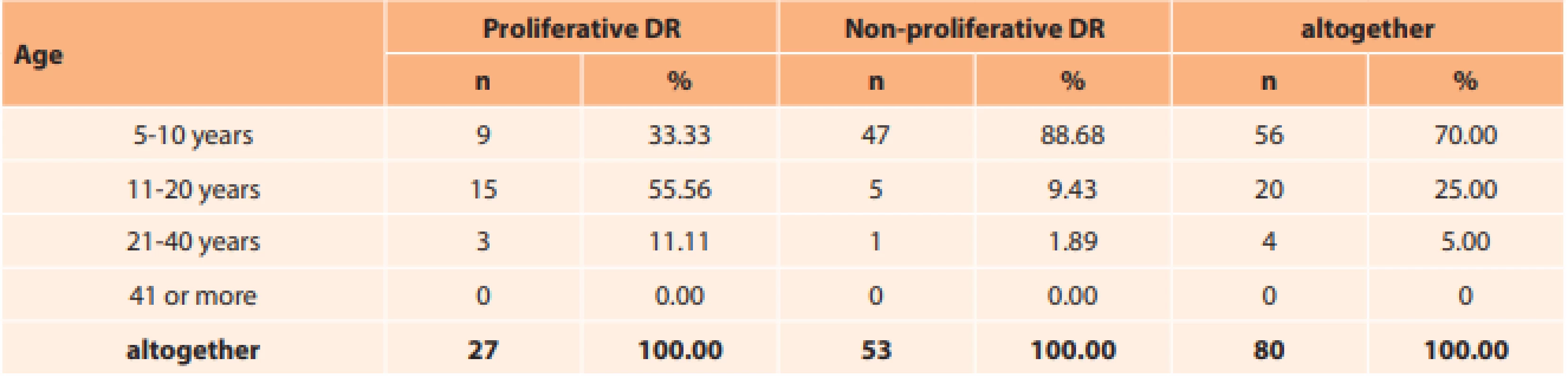
Within the framework of the study, stage 1 PDR was confirmed by 4 respondents (14.8 %), stage 2 by 18 (66.7 %) and stage 3 by 5 (18.5 %) respondents. In terms of NPDR, stage 1 was confirmed by 5 respondents (9.4 %), stage 2 by 29 (54.7 %) and stage 3 by 19 (35.5%). In total, the study in both phases of the disease in stage 1 included 9 (11.2 %) senior citizens, stage 2 included 47 (58.8 %) and stage 3 included 24 (30 %) (Table 4).Evaluation of the stages of DR in this group is of fundamental significance with regard to preserving visual function and prognostically known changes.
Tab. 4. Type of diabetic retinopathy 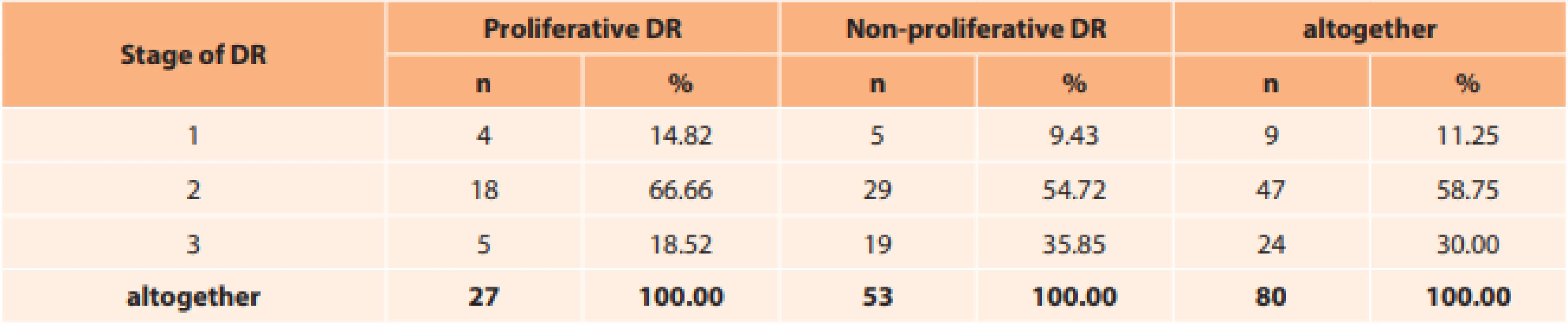
RESULTS
An analysis of selected items of the questionnaire NIE VFQ – 25 is presented in table 5.
Tab. 5. Statistical evaluation of subjective perception of activities requiring good eyesight, peripheral and colour vision 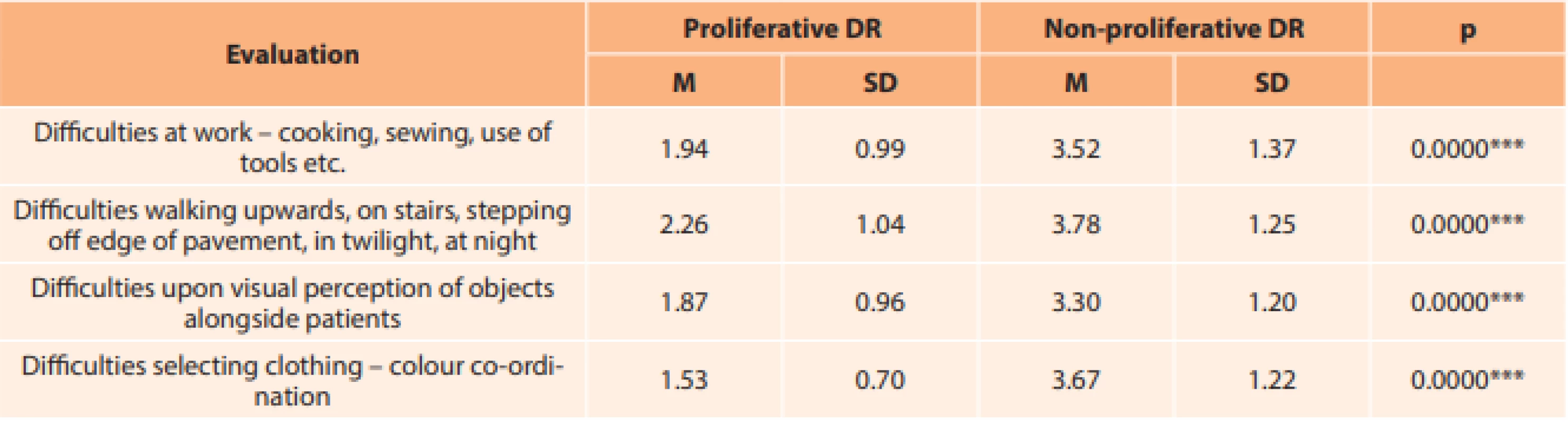
* p < .05; ** p < .01; *** p < .001 Through a comparison of the observed groups of patients with NPDR and PDR, we recorded significant differences in the perception of all the observed indicators. With the aid of a T-test, in both of the compared groups of patients we determined significant differences in activities which require good eyesight, peripheral and colour vision (p < .001). This especially concerns difficulties at work (cooking, sewing, use of tools), difficulties walking upwards, on stairs, stepping off the edge of pavements, in twilight, during night hours, as well as difficulties with visual perception of objects alongside the patients. The stated items evaluate self-sufficiency of senior citizens in instrumental daily activities, which evidently support their independence of functioning in everyday life. Several of the items from the used tool NEI VFQ – 25 indicate the need for safety and security, for example difficulties with visual perception of objects alongside the patients from the perspective of movement outside the patients’ own home (traffic flow etc.).
We recorded the most pronounced differences in the area of malfunction of colour vision, colour co-ordination in selection of clothing, which patients with NPDR evaluated with an average score of 1.5, which correlated to values on the Likert scale of 1 (no difficulties whatsoever) to 2 (slight difficulties), while patients with PDR evaluated on an average level of 3.7, which corresponds to a value of 3 (medium difficulties) to 4 (extreme difficulties in selection and co-ordination of coloured clothing) (Table 5).
Colour co-ordination in selection of clothing may stimulate aesthetic changes in senior citizens. The fundamental significance of this change in colour differentiation is intensified by a situation in which colour visual signals on electrical appliances are not observed or decoded sufficiently in time, traffic lights are ignored etc.
The NIE VFQ – 25 questionnaire is a measuring instrument for evaluating quality of life in connection with vision, and is available in Slovak language. In the Slovak version it is a fully valid and reliable tool for measuring quality of life in patients with age-related macular degeneration (ARMD) and DME, on whom it has been tested [7].The presented comparative study was conducted on 80 patients, depending on the stage of DR. For a statistical comparison we divided the senior citizens into a group with NPDR (n = 53) and with PDR (n = 27). The results of medical examinations and treatment do not provide relevant information about quality of life, and our endeavour was to conduct an evaluation within the broader context of activities on the level of visual functions. Using the obtained data from patients by means of the standardised questionnaire NIE VFQ – 25, we identified significant differences in quality of life in peripheral and colour vision.The current international classification divides DR into NPDR and PDR, further stating the presence or absence of diabetic macular edema (DME) (which is a yellow stain on the retina and the place of sharpest vision in the human eye). DME most often accompanies the non-proliferative phase of the disease, but may appear also in the proliferative phase [8]. DME is the most common cause of deterioration of vision in patients with DM [5].DISCUSSION
From the monitored demographic indicators, we would like to draw attention to an analysis of the socio-demographic indicators. The female population was represented in a larger number than the male population. The highest representation was in the age group of 60 to 70 years and over in both groups, which directs our attention to one of the risk factors of type 2 DM, namely age. Time was also confirmed as another risk factor. The duration of treatment of DM (from 11 to 40 years) and ocular complications as a consequence of DM (from 5 to 20 years) were the most highly represented in both groups.
DR is not necessarily manifested bilaterally. The occurrence of DR increases with the duration of DM, if DM persists for more than twenty years its incidence is almost 100 % unless the disease is adequately compensated [9].
Sosna states that the age at which DM appeared in the patient and the length of its duration are indisputably the most serious extraocular factors affecting the eye [10]. In all the selected sub-scales of the questionnaire evaluating activities in connection with colour and peripheral vision, we determined a significantly more positive difference between the investigated samples in favour of NPDR in comparison with the group with PDR (p < 0.0000). Patients with NPDR reported visual comfort in that they had no difficulties whatsoever, and even when visual problems appeared this was only to a small extent. In the group of patients with PDR, vision is substantially restricted, and patients are capable of performing these activities only with extreme difficulties, or in some cases are incapable of performing them whatsoever. An example is the study conducted by Trento et al, which evaluates quality of life in connection with vision in 196 patients with DR. Reduced visual acuity was linked with a lower score for activities using near and distance vision, difficulties with tasks using colour and peripheral vision (p < 0.01), similarly as in our study. The female population attained a higher score in the sub-scales of activities requiring near vision (p < 0.005), distance vision activities (p < 0.006) and colour vision (p < 0.012) [11].
Similar results were determined also in a study on 104 patients with NPDR and PDR with the aid of two measuring tools: NEI VFQ-25 and the Vision Preference Value Scale (VPVS). Differences in the score were recorded for activities requiring near and distance vision, difficulties with tasks and colour and peripheral vision (p < 0.01). In these sub-scales, the patients with PDR suffered a loss of 25-30 points in comparison with the patients with NPDR (100 point scale). The authors of the study state that NEI VFQ-25 is an excellent instrument for evaluating quality of life in connection with visual capacities for patients with DR, because it evaluates visual functions, mental and emotional aspects of the disease as a consequence of visual affliction within the broader context [12].
The NIE VFQ-25 questionnaire was also used in a Turkish study, where average glycated haemoglobin (HbAlc) of 8.1±2 mmol/mol was recorded in a sample of 93 patients with DM. Out of the entire cohort, 64.5 % of patients had comorbidities, 75.3 % had PDR, 40 % had DME. The highest score was attained in the sub-scale of colour vision (79.9 ± 25), the lowest score in the sub-scale of overall condition of health (51.5 ± 15). In patients with better visual acuity and colour vision, the VFQ-25 score was significantly higher (p < 0.01) [13].
Demographic factors such as age and sex, and independent factors such as overall condition of health and overall comorbidity of eyes were tested as variables in the VRQOL study. Spearman’s correlation coefficients confirmed the strongest correlations in the following categories: difficulties managing role, near vision activities, distance vision activities and mental health problems. Patients with PDR scored 30 points less than patients with NDPR on these scales. The results of the study confirmed that visual acuity does not reflect the entire spectrum of symptoms of altered visual functions upon a background of DR. It was also determined that the questionnaire of visual functions includes a sub-scale of mental health (fears, frustration and others), which confirms the influence of DR on emotional well-being in addition to the evaluation of visual functions [14].
DR occurs in 24 % of patients with DM. Every year the vision of 12 000 – 24 000 patients with DM is affected, which represents 12 % of new cases of blindness. Several studies have demonstrated a qualitative and quantitative decrease in quality of life in connection with health in persons with DR [15,16].
A recent Indian study, similarly to our study, examined correlations in individual sub-scales of quality of life in patients with DR using the tool NIE VFO-25. The investigated cohort of 123 patients with DM included patients with DR (n = 97) and a control group without clinically detectable changes of DR (n = 26). Statistically significant differences (p < 0.001) were determined in all sub-scales. With regard to the increase in the stage of DR, the overall score of NIE VFQ-25 substantially decreased, which was statistically significant for all sub-scales (p < 0.005), with the exception of ocular pain. Quality of life was markedly lower in patients with DR in comparison with those without ocular complications with maximum effect on overall vision. Quality of life was reduced because the duration and degree of severity of DR increased [15]. Similarly as in the previous study of severity of the degree of DR, this study also indicated a positive correlation between the duration of DM and its impact on quality of life [17].
Any degree of visual affliction negatively influences the quality of life in patients with DM, including self-management of the disease [18]. The above statement corresponds with the results of the study conducted by Coyne et al., who evaluated visual capacity in patients with NPDR, PDR and without ocular complications. As a consequence of visual affliction, the group with PDR lost several aspects of life in activities in connection with diabetic care (exercise, reading nutritional information, preparation of insulin injections and glucose testing). In patients without ocular complications of DM, the threat of potential loss of sight was a significantly devastating aspect [19].
Validation of the Slovak version of the “Visual Function Questionnaire – 25” (NEI VFQ – 25) on 211 patients with chronic ocular pathologies produced the following findings. The lowest standard score in evaluation of quality of life in connection with vision for the group with DME at 69.9±4.6, for the group with ARMD 68.5±4.3, while the highest score was recorded in the control group of 91.2±1.8 [7]. Similar findings were determined in patients with type 2 DM and DME, who recorded a lower score than patients with ARMD. The above study confirms that patients with visual affliction as a consequence of DR have a feeling of discomfort in everyday life and lose their autonomy in everyday functioning, with a loss of their capacity to perform specific visual tasks, confirming partial or total loss of their basal and instrumental activities [20]. At present it is appropriate to conduct a Comprehensive Geriatric Assessment (CGA) in clinical practice. This represents a multi-dimensional diagnostic approach, which in addition to the patient’s somatic and psychological condition also makes use of a functional examination with the aim of compiling a comprehensive plan for care of senior citizens. Among other factors, the CGA also uses evaluation tools and tests which detect the functioning of a specific organs, therefore including visual functions, in a timely manner [21].
CONCLUSION
The study is unique, in that within the conditions of Eastern Slovakia, no similar research has been conducted due to the specific nature of the problem of quality of life in senior citizens with ocular problems. Partial or complete loss of sight in connection with DM has negative consequences on quality of life in patients with DR, which is also confirmed by our findings. The aim of treatment of DM is to avert ocular complications and prevent the progression of DR, afflicting one or both eyes [22]. It is of fundamental importance to prevent complications and to detect DR in patients of senior age in a timely manner, in which the possibility of conducting a Comprehensive Geriatric Assessment on these patients is offered.
The CGA is characterised by its focus on the senior population, emphasising the patient’s condition of (in)capability, (lack of) self-sufficiency, and by its focus on the area of quality of life. It also supports a multi-disciplinary approach, wherein its realisation involves not only the participation of a doctor, but also a physiotherapist, social worker, nurse and other healthcare professionals.
In the study we determined significant differences in both compared groups in activities such as difficulties at work (cooking, sewing, use of tools), difficulties walking upwards, on stairs, stepping off the edge of pavements, in twilight, during night hours, as well as difficulties with visual perception of objects alongside the patients. These items are a part of the functioning of a senior citizen in everyday life, which a nurse may detect with the aid of an IADL (Instrumental Activity Daily Living) test as a direct component of the CGA.
We recorded the most pronounced differences in the area of malfunction of colour vision, which may represent a high risk for senior citizens with regard to safety in traffic flow (traffic lights etc.).
Early detection of ocular changes in patients with DM in the group of senior citizens by means of an eye examination, implementation of evaluation tests and scales within the framework of CGA, as well as subsequent educational activity provided by a nurse, can help ensure a preventative effect upon the occurrence of chronic microvascular complications of DM.
The authors of the study hereby declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company. We further declare that this study has not been submitted to any other journal or printed elsewhere, with the exception of congress abstracts and recommended procedures.
This contribution was issued within the framework of the grant project KEGA: 002PU-4/2020 Proposal for method of evaluating quality of life for patients with multiple sclerosis
Zdroje
- Švancarová R, Sosna T. Oční komplikace diabetu [Eye complications of diabetes] Med. praxi 2012; 9(3):127–130.
- Máliš V, Javorková N. Diabetes mellitus z pohľadu oftalmológa. Via pract. 2008; 5(7/8):319–322.
- Fabryová Ľ. Diabetes mellitus 2.typu - celosvetová iniciatíva: 10 praktických krokov na dosiahnutie lepšej glykemickej kompenzácie. Interná med. 2006; 6(4): 239-244.
- Sosna T. Diabetická retinopatie. Med Pro Praxi. 2009; 6(5):270–275.
- Bezdéšová-Bohunická N, Skorkovská Š, Synek S, Kaňovský R, Mašková Z, Synková M. Diabetici v populácii pacientov liečených pars plana vitrektómiou [Diabetics in Population of Patients Treated by Pars Plana Vitrectomy] Cesk Slov Oftalmol. 2007; 63(6):431–441.
- Mangione CM, Berry S, Lee PP, et al. Identifying the content area for the National Eye Institute Vision Function Questionnaire (NEI-VFQ): Results from focus groups with visually impaired persons. Arch Ophthalmol. 1998;116 : 227-238.
- Vodrážková E, Šefčiková S, Helbich M. Psychometrická validácia verzie „Dotazníka zrakových funkcií – 5“ v podmienkach Slovenska [Psychometric Validation of Visual Function Questionnaire (NEI VQF-25) under Local Conditions in Slovakia] Cesk Slov Oftalmol. 2012;68(3):102–108.
- Rencová E. Praktické aspekty postižení očí diabetika [Practical aspects of the eye effection of diabetics] Med Pro Praxi 2010;7(1):28-31.
- Babcak M, Dimunová L, Kisko, A. Vybrané kapitoly z internej propedeutiky, výživy a ošetrovateľstva. Prešov: DAH. 2009, p. 228.
- Sosna T, Švancarová R, Netuková M. Diabetická retinopatie - rizikové faktory, prevence a terapie [Diabetic Retinopathy - risk factors, prevention and therapy]. Cesk Slov Oftalmol. 2010; 66(5):195-203.
- Trento M, Passera P, Trevisan M, et al. Quality of life, impaired vision and social role in people with diabetes: a multicenter observational study. Acta Diabetol 2013;50(6):873-877. doi: 10.1007/s00592-013-0470-1.
- Sharma S, Oliver-Fernandez A, Liu W, Buchholz P, Walt J. The impact of diabetic retinopathy on health-related quality of life. Curr Opin Ophthalmol. 2005;16(3):155-159. doi:10.1097/01.icu.0000161227.21797.3d.
- Rajavi Z, Safi S, Javadi MA, et al. Diabetic Retinopathy Clinical Practice Guidelines: Customized for Iranian Population. J Ophthalmic Vis Res. 2016;11(4):394-414. doi:10.4103/2008-322X.194131.
- Gabrielian A, Hariprasad S, Jager R, et al. The utility of visual function questionnaire in the assessment of the impact of diabetic retinopathy on vision-related quality of life. Eye 2010;24 : 29–35. [cited 2020 Feb 07]. Available from: https://doi.org/10.1038/eye.2009.56.
- Pereira DM, Shah A, D'Souza M, et al. Quality of Life in People with Diabetic Retinopathy: Indian Study. J Clin Diagn Res. 2017;11(4):NC01-NC06. doi:10.7860/JCDR/2017/24496.9686.
- Alcubierre N, Rubinat E, Traveset A, Martinez-Alonso M, Hernandez M, Jurjo C, et al. A prospective cross-sectional study on quality of life and treatment satisfaction in type 2 diabetic patients with retinopathy without other major late diabetic complications. Health Qual Life Outcomes. 2014;112 : 131.
- Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T. et al. Global Prevalence and Major Risk Factors of Diabetic Retinopathy. Diabetes Care Mar 2012, 35(3):556-564. doi: 10.2337/dc11-1909.
- Rybka J, Adamíková A, Langová D, Macháček J, Švestka L. Diabetologie pro sestry. Praha, Czech Republic: Grada Publishing. 2006, p. 288.
- Coyne KS, Margolis MK, Kennedy-Martin T, Baker TM, Klein R, Paul MD, et al. The impact of diabetic retinopathy: perspectives from patient focus groups. Fam Pract. 2004; 4(21):447-453. doi: 10.1093/fampra/cmh417.
- Hariprasad SM, Mieler WF, Grassi M, Green JL, Jager RD, Miller L. Vision-related quality of life in patients with diabetic macular oedema. Br J Ophthalmol. 2008;92(1):89-92. doi:10.1136/bjo.2007.122416.
- Németh F, Derňárová Ľ, Hudáková A. Komplexné geriatrické hodnotenie a ošetrovanie seniorov. Prešov: PU FZO. 2011, p. 216.
- Mazhar K, Varma R, Choudhury F, et al. Severity of diabetic retinopathy and health-related quality of life: the Los Angeles Latino Eye Study Ophthalmology. 2011;118(4):649-655. doi:10.1016/j.ophtha.2010.08.003.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2020 Číslo 6- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Diagnostický algoritmus při podezření na syndrom periodické horečky
- Normotenzní glaukom: prevalence a zásady terapie
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
-
Všechny články tohoto čísla
- Uveal Melanoma Biopsy. A Review
- VISUAL FUNCTIONS AFTER IMPLANTATION OF ACRYSOF MONOFOCAL INTRAOCULAR LENSES.
- Evaluation of Patients Presenting to the Ophthalmology Department of a Tertiary Hospital for Nonemergency Reasons During the Covid-19 Pandemic
- Changed Eye Functions and Quality of Life of Seniors with Diabetic Retinopathy
- Can Visual Function Be Affected by an Open Foramen Ovale?
- Late Functional and Morphological Findings after Methylalcohol Poisoning
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Can Visual Function Be Affected by an Open Foramen Ovale?
- VISUAL FUNCTIONS AFTER IMPLANTATION OF ACRYSOF MONOFOCAL INTRAOCULAR LENSES.
- Late Functional and Morphological Findings after Methylalcohol Poisoning
- Uveal Melanoma Biopsy. A Review
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání