-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Increased Duration of Paid Maternity Leave Lowers Infant Mortality in Low- and Middle-Income Countries: A Quasi-Experimental Study
Nandi and colleagues, in a large study analyzing data from 20 countries, show that extended, paid maternity leave effectively reduces infant mortality in LMICs.
Published in the journal: . PLoS Med 13(3): e32767. doi:10.1371/journal.pmed.1001985
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001985Summary
Nandi and colleagues, in a large study analyzing data from 20 countries, show that extended, paid maternity leave effectively reduces infant mortality in LMICs.
Introduction
Paid leave for new parents, often specifically designated for new mothers, is a standard social benefit in most of the world. Over 180 countries have enacted legislation granting paid leave from employment in connection with the birth of a child, either in the form of maternity leave or gender-neutral parental leave [1].
Paid maternity and parental leave policies are consistently associated with improvements in child health in high-income countries [1–5]. For example, Ruhm found that increases in weeks of paid leave were associated with lower infant mortality in 16 European countries, although effects on perinatal and neonatal mortality were more modest [3]. Similarly, Tanaka showed that increases in paid parental leave were associated with decreases in perinatal, neonatal, post-neonatal, infant, and child mortality in a sample of 18 Organisation for Economic Co-operation and Development countries [4]. Recent work also showed that unpaid maternal leave provided through the Family and Medical Leave Act of 1993 in the United States was associated with decreases in neonatal, post-neonatal, and infant mortality, but only among women who were married and had graduated from college, suggesting that women of lower socioeconomic position may have been unable to take unpaid leave [5].
Paid maternity leave may affect neonatal and infant mortality through several mechanisms. First, paid maternity leave may increase access to pre - and postnatal health services. Some maternity leave policies allow for a short period of leave to be taken immediately prior to birth, which might increase receipt of third-trimester prenatal care. In the postnatal period, mothers able to take leave from employment may have more time to care for an ill child and seek medical care when necessary. Second, policies that provide income and ensure job protection during maternity leave may benefit women economically, reduce stress in the prenatal period, and improve maternal health after birth [6–8]; these factors might reduce adverse birth outcomes, including preterm birth and low birth weight [9–11]. Third, paid maternity leave might facilitate preventive care; for example, women able to take leave from employment are more likely to initiate breastfeeding and to continue breastfeeding for longer durations [12–15]. Paid maternity leave may also improve adherence to childhood vaccination schedules [16–18]. These mechanisms may interact synergistically; for example, increased income may be associated with more access to resources to support healthy behaviors and child-rearing practices [19,20].
Extant evaluations of paid maternity leave policies have been conducted almost exclusively in high-income countries. Whether these results can be generalized to lower-income contexts is unclear, given differences in the nature of non-parental child-care options as well as in women’s participation in the formal economy. In this study, we provide the first evaluation, to our knowledge, of whether paid maternity leave policies affect infant (<1 y), neonatal (<28 d), and post-neonatal (between 28 d and 1 y after birth) mortality in low - and middle-income countries (LMICs). We constructed a database of maternity leave policies for LMICs over time, merged this information to a sample of live births occurring between 2000 and 2008 in 20 LMICs surveyed as part of the Demographic and Health Surveys (DHS), and utilized a difference-in-differences approach to estimate the influence of paid maternity leave on mortality during the first year of life.
Methods
Sample
Information on birth outcomes was derived from the DHS. The authors had full access to the DHS data from which the analytic sample is derived. The DHS collect comparable information on demographic, socioeconomic, nutritional, behavioral, fertility, and health characteristics from a nationally representative sample of households in LMICs using a two-stage cluster sampling design. Individuals are selected for interviews from household rosters; information is collected on women of reproductive age (15–49 y), men (usually aged 15–54 or 15–59 y), and children under the age of 5 y. Trained interviewers and standardized tools and measurement techniques are used to ensure comparability of surveys across countries and survey waves. Further details regarding sampling strategies and study procedures are available elsewhere [21,22].
Our sample comprised all live births occurring to DHS respondents from 20 LMICs between 2000 and 2008. These 20 countries were selected because they administered at least two DHS surveys between 2001 and 2011, which permitted analyses of policy changes occurring within countries over time. Briefly, mothers surveyed in the DHS were asked to provide information concerning all children born alive in the previous 5 y. These data were used to construct a panel of live births, each with information on vital status, over a consistent set of years and countries. We created two separate samples, one for our analyses of infant and post-neonatal mortality and the other for analyses of neonatal mortality. We restricted these samples to the 282,836 and 304,294 live births that occurred at least 1 y and at least 28 d prior to the DHS interview date, respectively, in order to ascertain whether each child survived the infant (1 y) and neonatal (28 d) periods following birth. After further excluding observations with missing information on key covariates, our samples were composed of 282,751 live births between 2000 and 2007 for analyses of infant and post-neonatal mortality and 304,201 live births between 2001 and 2008 for analyses of neonatal mortality. Table 1 reports survey years and sample sizes for the sampled countries. The Institutional Review Board of McGill University reviewed and approved this study.
Tab. 1. Demographic and Health Surveys survey years, sample sizes, and rates of infant, neonatal, and post-neonatal mortality. 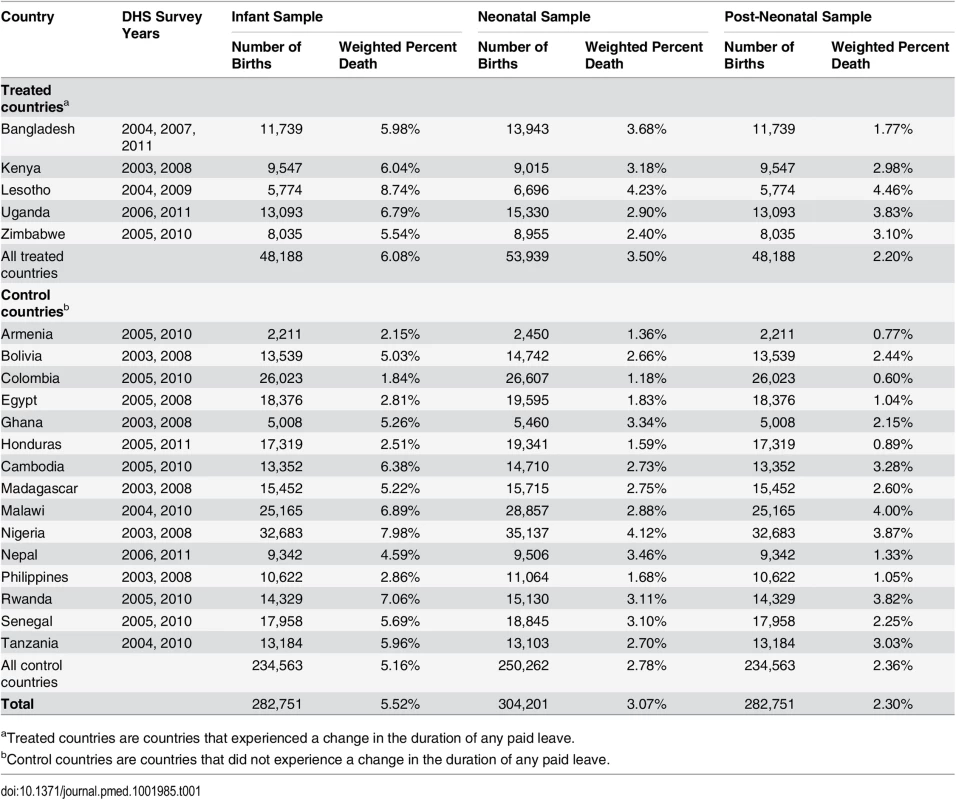
aTreated countries are countries that experienced a change in the duration of any paid leave. Measures
The exposure of interest in our study was the legislated length of paid maternity leave for each country and year. Data on current maternity leave policies for each sampled country were provided by the University of California Los Angeles World Legal Rights Data Centre, and data on past maternity leave policies back to 1995 were collected by McGill University’s Maternal and Child Health Equity (MACHEquity) research program. We defined the duration of paid maternity leave as the legislated length of paid leave available to mothers only. We did not distinguish leave that could be taken in the prenatal period from leave that could be taken after birth; however, few maternity leave policies in LMICs mandate specifically prenatal versus postnatal leave. Further details regarding the collection and coding of global maternity leave policies are available elsewhere [1].
The outcome variables—infant, neonatal, and post-neonatal mortality—were measured using the 5-y birth histories provided by women interviewed in the DHS. We created binary indicators for infant, neonatal, and post-neonatal mortality to measure whether each child died within 1 y, within the first 28 d of life, or between 28 d and 1 y after birth, respectively.
We collected information on potential confounders and other characteristics based on a review of the literature on determinants of neonatal and infant mortality in LMICs [23–31]. Individual and household-level socio-demographic characteristics included the child’s gender, mother’s educational attainment in completed years, urban/rural residence, and household socioeconomic status (SES). Household SES, categorized into five equal groups using quintiles, was determined from the continuous wealth index provided by the DHS, which is based on ownership of specific assets (e.g., bicycle, radio, and television), environmental conditions, and housing characteristics (e.g., type of water source, sanitation facilities, materials used for housing construction), and was constructed using the method proposed by Filmer and Pritchett [32,33]. Birth characteristics included the interval between births (defined as short if it was less than 24 mo), maternal age at the time of each birth (categorized as <20, 20–39, or 40 y and older), and whether there was a skilled birth attendant present at the time of delivery. Aside from the length of paid leave, another defining feature of paid maternity leave policies is the percentage at which wages are replaced. Because changes in the wage replacement rate sometimes coincided (i.e., in Lesotho) with changes in the legislated length of leave, we controlled for the wage replacement rate as a potential confounder. Additional time-varying country-level covariates included levels of economic development (measured by gross domestic product [GDP] per capita based on purchasing power parity [PPP], in constant 2005 international dollars), female labor force participation (the proportion of women age 15 y and older in the labor force), per capita total health expenditure (PPP, in constant 2005 international dollars), and per capita government health expenditure (PPP, in constant 2005 international dollars), which were available from the World Bank’s World Development Indicators and Global Development Finance databases [34].
Statistical Analysis
We linked data on paid maternity leave policies to outcomes and covariates from the DHS by country and birth year and examined the effects of an increase in the duration of paid maternity leave on the risk of mortality during the first year of life. Specifically, we estimated for birth i the effect of an additional month of paid leave (lagged by 1 y to respect the temporal ordering between the policy and outcome) on the probabilities of infant, neonatal, and post-neonatal mortality using a linear probability model of the general form Yijt = αj + βMjt−1 + λt + ϵijt, where β measures the effect of a 1-mo increase in maternity leave in the prior year, Mjt−1 (where j indexes the country and t the birth year), on infant, neonatal, and post-neonatal death, Yijt. We included fixed effects for country (αj) and year (λt) to control for unobserved time-invariant confounders that vary across countries and any temporal trends in mortality that are shared across countries, respectively. The effects of paid maternity leave policies were therefore identified by changes in outcomes occurring within countries that modified their maternity leave policies during the study period (treated countries) relative to corresponding changes in outcomes in countries that did not modify their policies during the study period (control countries).
In the first model, we estimated the effect of an additional month of paid maternity leave on infant, neonatal, and post-neonatal mortality after including country and year fixed effects (Model 1). In the second model, we additionally controlled for measured individual, household, and country-level characteristics, including the lagged wage replacement rate, natural log per capita GDP, and female labor force participation (Model 2). In the third model, we included controls for natural log per capita total and government health expenditures (Model 3); these data were unavailable for all years for Zimbabwe, and observations from Zimbabwe were therefore dropped from Model 3 analyses. In order to examine potential nonlinearity in the effect of paid maternity leave, we introduced a quadratic duration-of-paid-leave variable into our fully adjusted model (Model 3). We also estimated the fully adjusted model on the risk ratio (RR) scale. All analyses incorporated respondent-level sampling weights to account for individual survey sample designs. Per DHS guidelines, we used information on the number of women aged 15–49 y in each survey-year, provided by the Population Division of the United Nations [35], and applied the de-normalization of standard weights approach described in the DHS Sampling and Household Listing Manual [36], in order to calculate an appropriate weight for each observation in the analyses. All models incorporated robust standard errors to account for clustering at the country level [37].
Sensitivity Analyses
We conducted sensitivity analyses to assess the robustness of our main findings. First, because there is no standard metric for maternity leave policies, we measured the effects of paid leave in full-time equivalent (FTE) units, obtained by multiplying the legislated length of leave by the wage replacement rate, in addition to the duration of any paid leave. Further details regarding the calculation of FTE units of paid leave are available elsewhere [1,16]. Second, we examined whether results were sensitive to the inclusion of sampling weights. Third, we added to our primary exposure, paid maternity leave in year t − 1, parameters representing paid maternity leave in preceding years (t − 3, t − 2), the birth year (t), and subsequent years (t + 1, t + 2, t + 3). These analyses assessed if there were persistent effects of the policy changes, as well as whether observed effects were responses to policy changes that occurred in the period during or before the measurement of our outcomes, as we would expect if the effects of paid maternity leave policies were causal. Fourth, as described in S1 Text, we assessed whether our findings were sensitive to the particular selection of control countries. In these analyses, we examined trends in infant, neonatal, and post-neonatal mortality occurring in the decade before our treated countries changed their legislated length of paid maternity leave and then restricted the sample of controls to those countries with parallel pre-intervention trends.
Results
Table 1 shows the rates of infant, neonatal, and post-neonatal mortality for the 20 DHS countries; average rates of infant, neonatal, and post-neonatal mortality over the study period were 55.2, 30.7, and 23.0 per 1,000 live births, respectively. Table 2 shows trends in paid maternity leave benefits and country-level characteristics for the five treated and 15 control countries; baseline values for key covariates are provided for each country in S1 Table and trends in the duration of paid leave for individual treated countries are shown in S1 Fig. For treated countries, the average length of paid leave increased from 7.6 (standard deviation [SD] = 5.4) wk in 2000 to 12.2 (SD = 3.8) wk in 2008. The average length of paid leave in control countries was 12.2 (SD = 3.0) wk.
Tab. 2. Trends in paid maternity leave benefits and country-level characteristics for treated and control countries, 2000–2008. 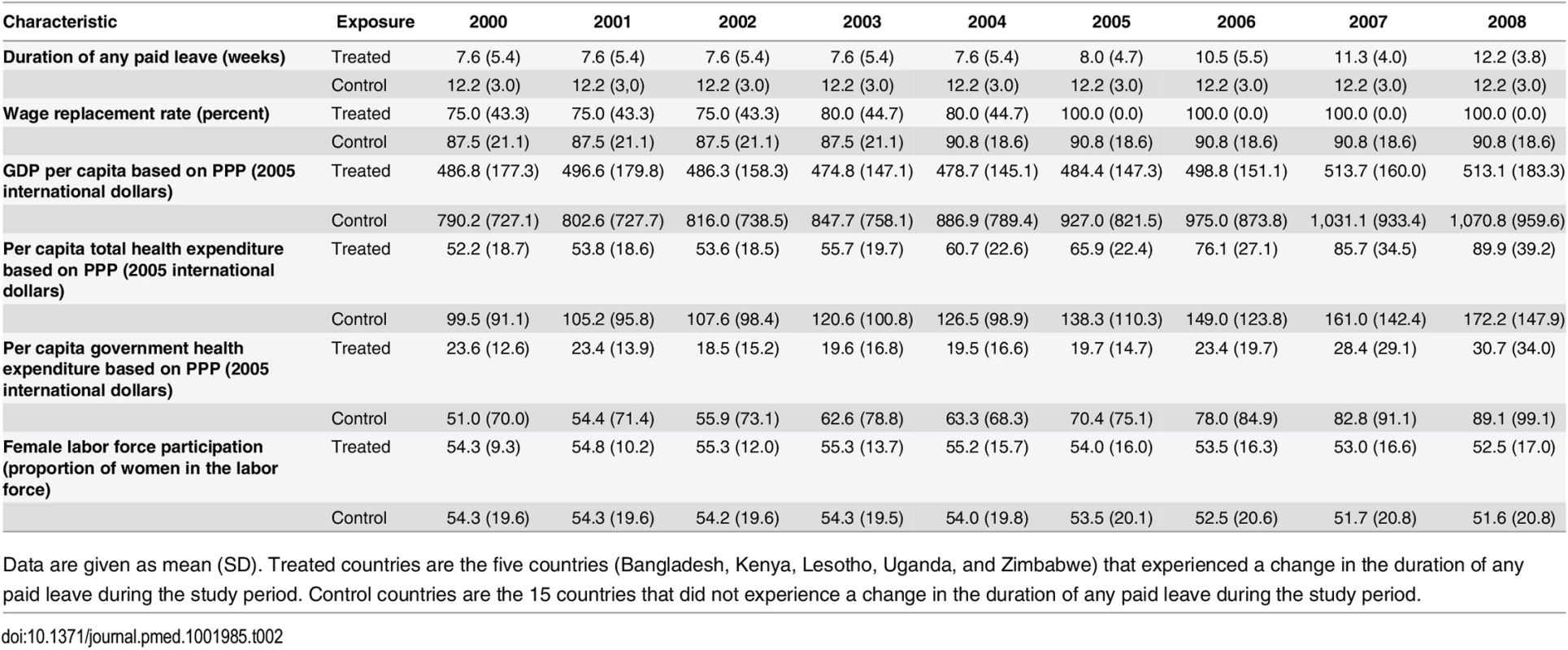
Data are given as mean (SD). Treated countries are the five countries (Bangladesh, Kenya, Lesotho, Uganda, and Zimbabwe) that experienced a change in the duration of any paid leave during the study period. Control countries are the 15 countries that did not experience a change in the duration of any paid leave during the study period. Tables 3, 4 and 5 show the effects of an additional month of paid maternity leave on the probability of infant, neonatal, and post-neonatal death, respectively. In the fully adjusted model (Model 3), an additional month of paid maternity leave was associated with 7.9 (95% CI 3.7, 12.0) fewer infant deaths per 1,000 live births. Each additional month of paid leave was associated with 2.9 (95% CI –0.2, 6.0) fewer neonatal and 4.4 (95% CI 0.9, 8.0) fewer post-neonatal deaths per 1,000 live births. On the RR scale, each additional month of paid leave was associated with a 13% (RR = 0.87, 95% CI 0.81, 0.93), 9% (RR = 0.91, 95% CI 0.83, 1.00), and 18% (RR = 0.82, 95% CI 0.64, 1.05) reduction in infant, neonatal, and post-neonatal mortality, respectively (S2 Table). There was some evidence for a nonlinear effect of an additional month of paid maternity leave on the probabilities of infant and post-neonatal mortality, but not neonatal mortality (S3 Table). In particular, an additional month of paid leave was associated with a larger absolute reduction in infant and post-neonatal mortality when shorter durations of paid leave were available (S2 Fig).
Tab. 3. Effect of a 1-mo increase in paid maternity leave on the number of infant deaths per 1,000 live births, Demographic and Health Surveys, 2000–2007. 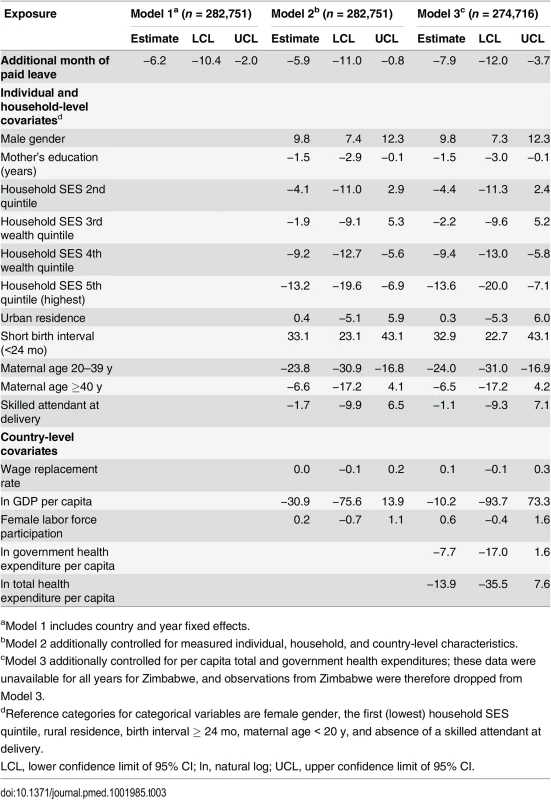
aModel 1 includes country and year fixed effects. Tab. 4. Effects of a 1-mo increase in paid maternity leave on the number of neonatal deaths per 1,000 live births, Demographic and Health Surveys, 2001–2008. 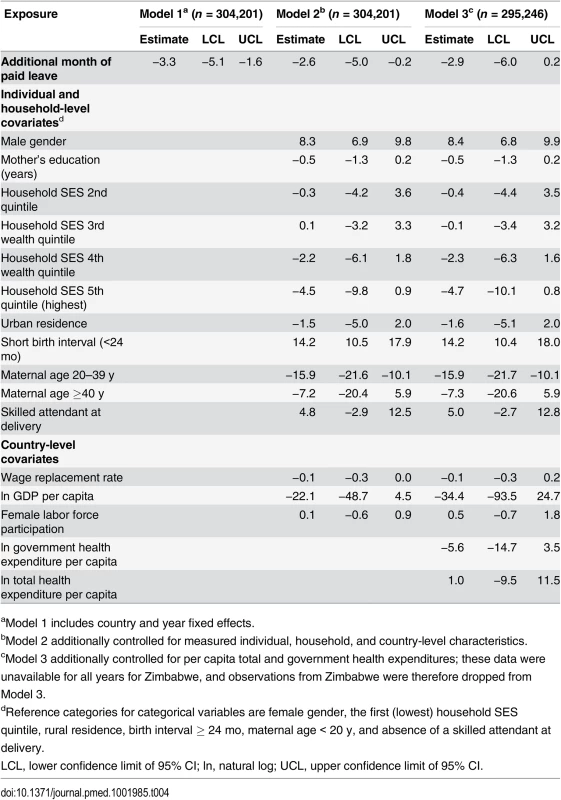
aModel 1 includes country and year fixed effects. Tab. 5. Effects of a 1-mo increase in paid maternity leave on the number of post-neonatal deaths per 1,000 live births, Demographic and Health Surveys, 2000–2007. 
aModel 1 includes country and year fixed effects. There were pronounced socioeconomic gradients in infant and post-neonatal, but not neonatal, mortality; there were, on average, 13.6 (95% CI 7.1, 20.0) fewer infant deaths per 1,000 live births in households in the highest quintile of household SES compared to the lowest quintile. Birth characteristics, including short birth interval (<24 mo) and lower maternal age (<20 y), were consistently associated with neonatal and infant mortality. For example, a short birth interval was associated with an additional 32.9 (95% CI 22.7, 43.1) infant, 14.2 (95% CI 10.4, 18.0) neonatal, and 15.7 (95% CI 10.8, 20.7) post-neonatal deaths per 1,000 live births. Country-level characteristics were not associated with mortality.
Sensitivity Analyses
Results from sensitivity analyses for infant, neonatal, and post-neonatal outcomes are shown in S4 Table, S5 Table, and S6 Table, respectively. The effects of paid leave policies on infant mortality were fairly robust. When paid leave was measured in FTE units, an additional month of leave was associated with a smaller decrease in infant mortality of 3.6 (95% CI −2.4, 9.6) fewer deaths per 1,000 live births (Model A). Unweighted estimates suggested that an additional month of paid leave was associated with 10.3 (95% CI 4.9, 15.7) fewer infant deaths per 1,000 live births (Model B). The effects of paid leave on infant mortality were isolated to responses to policy changes that occurred in the year preceding the measurement of the outcome (Model C). Additionally, our results were qualitatively similar after we restricted our sample of control countries to those with similar pre-intervention trends in infant mortality between 1990 and 2000 (Model D). By contrast, the effects of paid maternity leave policies on neonatal mortality varied substantially across alternative model specifications. In particular, an increase in the duration of paid leave was no longer associated with neonatal mortality in models that were unweighted (Model B). Additionally, estimates of the effects of paid leave modeled separately in years before and after the policy change were relatively imprecise (Model C). The effect of paid maternity leave on post-neonatal mortality was similar in unweighted and weighted models (Model B); however, the effects of lagged and lead effects were unstable and difficult to interpret (Model C).
Discussion
We merged longitudinal information on the legislated duration of paid maternity leave in 20 LMICs with a panel of approximately 300,000 live births recorded in DHS surveys in those countries between 2000 and 2008 and used this dataset to conduct the first evaluation, to our knowledge, of the impact of paid maternity leave on infant mortality in LMICs. Difference-in-differences analyses suggested that each additional month of paid maternal leave was associated with approximately eight fewer infant deaths per 1,000 live births. These findings were relatively robust to alternative model specifications.
Policies guaranteeing new mothers paid leave from work provide new mothers with the opportunity to rest and recover after childbirth, increase their job protection and labor force attachment [38], and may benefit their mental and physical health [7,8,39]. Moreover, a growing literature suggests that paid maternity leave policies have a beneficial effect on maternal health behaviors, including breastfeeding [12–15], and infant health in higher-income countries [3–5]. Given the lack of evidence, it has been unclear if these findings can be generalized to poorer countries, where rates of female labor force participation in the formal economy are generally lower. Our results indicate that more generous paid maternity leave policies may have an even greater potential to reduce infant mortality in LMICs than in higher-income countries [3,4], both in absolute and relative terms, although prior work in high-income countries considered parental leave rather than maternity leave per se. Furthermore, our findings suggest that the benefits of additional paid maternity leave in terms of reducing infant mortality were larger when shorter durations of paid leave were available. Heterogeneity in the impact of paid maternity leave across countries warrants further investigation. Although a smaller proportion of women may be eligible for leave in LMICs than in high-income countries, and leave policy implementation may be poorer, the actual benefit to child health conditional on being eligible may be substantial, given higher infant mortality rates in poorer contexts. Furthermore, a greater proportion of women in LMICs may be benefiting from leave benefits than we might anticipate. Labor reforms targeting the formal economy may have spillover effects that influence workers in the informal economy. Moreover, many international labor standards and national laws are constructed to encompass all types of workers.
Similar to observations from higher-income countries [3,4], extending the duration of paid leave available to new mothers resulted in larger reductions in mortality in the post-neonatal than in the neonatal period. An increase in the duration of paid leave available to mothers might influence postnatal factors, including the duration of breastfeeding and vaccination uptake, which are consistently associated with better infant health [40–42]. Recent work, for example, showed that increases in paid maternity leave were associated with increased uptake of diphtheria, pertussis, and tetanus immunizations [43]. Epidemiologic evidence suggests that neonatal mortality, by contrast, is determined to a greater extent by antenatal factors that are less likely to be influenced by increases in maternity leave, unless that leave is taken before birth; these factors include maternal and reproductive factors, such as maternal age and birth spacing, as well as health services characteristics, including the use of antenatal care and the place of delivery [44–50]. Further research into the effects of maternity leave policies on utilization of health services and behavioral risk factors for neonatal and infant mortality is needed.
Our findings suggest there is potential for improving infant health by increasing the duration of paid maternity leave in LMICs. Recently, the Countdown to 2015 report suggested that only one-third of the 75 “Countdown countries,” those accounting for more than 95% of global maternal and infant deaths, achieved the Millennium Development Goal 4 of reducing child (<5 y) mortality by two-thirds by 2015 [51]. As others have argued [52], in order to end preventable deaths among children, countries will need to address neonatal and infant deaths more effectively. Data from the MACHEquity research program showed that one-quarter of the Countdown countries provided less than 12 wk of paid maternity leave in 2012 (median = 12.9 wk). Our findings suggest that social interventions, in addition to health policy interventions [53], warrant further discussion in the post-2015 development agenda. More generous paid maternity leave policies represent a potential instrument for facilitating early-life interventions and reducing infant mortality in LMICs.
There were limitations to our study. First, as in any non-experimental study, there is the potential for unmeasured confounding. However, we controlled for potential confounding by individual, household, and country-level characteristics. We also included fixed effects for country and year to account for unobserved time-invariant confounders that vary across countries and any temporal trends in mortality that are shared across countries, respectively. Therefore, any unmeasured confounders that would remain to bias our estimates would have to coincide with policy changes occurring within treated countries and also influence mortality, which markedly reduces the list of potential unobserved confounders. However, the adoption of several policies, including paid leave policies, simultaneously would conflate effects and potentially bias our results. Second, the determination of our outcomes, neonatal and infant mortality, depends on maternal recall, and mothers may underreport the births and deaths of children who are not alive at the time of the interview. Such underreporting would bias our estimates only if it were different between our treatment and control countries. Third, our measure of paid maternity leave is calculated based on legislated maternity leave and does not account for other leave (i.e., parental leave) that might also be available to mothers. Fourth, in order to model the longitudinal effect of maternity leave policies on neonatal and infant mortality, we limited our analyses to 20 selected LMICs with at least two DHS surveys between 2001 and 2011; the inclusion of sampling weights allows us to generalize our results to these 20 countries, but not to all LMICs.
Caveats considered, our analyses suggest that an additional month of paid maternity leave is associated with as much as a 13% reduction in infant mortality in LMICs. From a policy planning perspective, further work is needed to elucidate the mechanisms that explain the beneficial effects of paid maternity leave on infant mortality and to evaluate the optimal balance of leave from employment prior to and following delivery, as well as varying levels of compensation. Further work is also needed to document the effects of paid maternity leave on women’s labor force participation, health, and well-being in LMICs.
Supporting Information
Zdroje
1. Heymann J, Raub A, Earle A (2011) Creating and using new data sources to analyze the relationship between social policy and global health: the case of maternal leave. Public Health Rep 126 (Suppl 3): 127–134. 21836745
2. Winegarden CR, Bracy PM (1995) Demographic consequences of maternal-leave programs in industrial countries: evidence from fixed-effects models. South Econ J 61 : 1020–1035.
3. Ruhm CJ (2000) Parental leave and child health. J Health Econ 19 : 931–960. 11186852
4. Tanaka S (2005) Parental leave and child health across OECD countries. Econ J 115: F7–F28.
5. Rossin M (2011) The effects of maternity leave on children’s birth and infant health outcomes in the United States. J Health Econ 30 : 221–239. doi: 10.1016/j.jhealeco.2011.01.005 21300415
6. Chatterji P, Markowitz S (2005) Does the length of maternity leave affect maternal health? South Econ J 72 : 16–41. doi: 10.2307/20062092
7. Chatterji P, Markowitz S (2012) Family leave after childbirth and the mental health of new mothers. J Ment Health Policy Econ 15 : 61–76. 22813939
8. Dagher RK, McGovern PM, Dowd BE (2014) Maternity leave duration and postpartum mental and physical health: implications for leave policies. J Health Polit Policy Law 39 : 369–416. doi: 10.1215/03616878-2416247 24305845
9. Shapiro GD, Fraser WD, Frasch MG, Seguin JR (2013) Psychosocial stress in pregnancy and preterm birth: associations and mechanisms. J Perinat Med 41 : 631–45. doi: 10.1515/jpm-2012-0295 24216160
10. Wadhwa PD, Entringer S, Buss C, Lu MC (2011) The contribution of maternal stress to preterm birth: issues and considerations. Clin Perinatol 38 : 351–84. doi: 10.1016/j.clp.2011.06.007 21890014
11. Torche F (2011) The effect of maternal stress on birth outcomes: exploiting a natural experiment. Demography 48 : 1473–1491. doi: 10.1007/s13524-011-0054-z 21870187
12. Baker M, Milligan K (2008) Maternal employment, breastfeeding, and health: evidence from maternity leave mandates. J Health Econ 27 : 871–887. doi: 10.1016/j.jhealeco.2008.02.006 18387682
13. Chatterji P, Frick KD (2005) Does returning to work after childbirth affect breastfeeding practices? Rev Econ Househ 3 : 315–335.
14. Guendelman S, Kosa JL, Pearl M, Graham S, Goodman J, et al. (2009) Juggling work and breastfeeding: effects of maternity leave and occupational characteristics. Pediatrics 123: e38–e46. doi: 10.1542/peds.2008-2244 19117845
15. Hawkins SS, Griffiths LJ, Dezateux C (2007) The impact of maternal employment on breast-feeding duration in the UK Millennium Cohort Study. Public Health Nutr 10 : 891–896. 17381907
16. Daku M, Raub A, Heymann J (2012) Maternal leave policies and vaccination coverage: a global analysis. Soc Sci Med 74 : 120–124. doi: 10.1016/j.socscimed.2011.10.013 22196248
17. Berger LM, Hill J, Waldfogel J (2005) Maternity leave, early maternal employment and child health and development in the US. Econ J 115: F29–F47.
18. Ueda M, Kondo N, Takada M, Hashimoto H (2014) Maternal work conditions, socioeconomic and educational status, and vaccination of children: a community-based household survey in Japan. Prev Med 66 : 17–21. doi: 10.1016/j.ypmed.2014.05.018 24879891
19. Hasselmann MH, Werneck GL, Silva CV (2008) Symptoms of postpartum depression and early interruption of exclusive breastfeeding in the first two months of life. Cad Saude Publica 24: s341–s352. 18670714
20. Patel V, Rahman A, Jacob K, Hughes M (2004) Effect of maternal mental health on infant growth in low income countries: new evidence from South Asia. BMJ 328 : 820–823. 15070641
21. Rutstein SO, Rojas G (2006) Guide to DHS statistics. Calverton (Maryland): ORC Macro.
22. Corsi DJ, Neuman M, Finlay JE, Subramanian SV (2012) Demographic and health surveys: a profile. Int J Epidemiol 41 : 1602–1613. doi: 10.1093/ije/dys184 23148108
23. Agha S (2000) The determinants of infant mortality in Pakistan. Soc Sci Med 51 : 199–208. 10832568
24. Titaley C, Dibley M, Agho K, Roberts C, Hall J (2008) Determinants of neonatal mortality in Indonesia. BMC Public Health 8 : 232. doi: 10.1186/1471-2458-8-232 18613953
25. Lawoyin T (2001) Risk factors for infant mortality in a rural community in Nigeria. J R Soc Promot Health 121 : 114–118. 11467203
26. Jahan S (2008) Poverty and infant mortality in the Eastern Mediterranean region: a meta-analysis. J Epidemiol Community Health 62 : 745–751. doi: 10.1136/jech.2007.068031 18621962
27. Madise NJ, Banda EM, Benaya KW (2003) Infant mortality in Zambia: socioeconomic and demographic correlates. Soc Biol 50 : 148–166. 15510542
28. Whitworth A, Stephenson R (2002) Birth spacing, sibling rivalry and child mortality in India. Soc Sci Med 55 : 2107–2119. 12409124
29. Hanmer L, Lensink R, White H (2003) Infant and child mortality in developing countries: analysing the data for robust determinants. J Dev Stud 40 : 101–118.
30. Alves D, Belluzzo W (2004) Infant mortality and child health in Brazil. Econ Hum Biol 2 : 391–410. 15576245
31. Filmer D, Pritchett L (1999) The impact of public spending on health: does money matter? Soc Sci Med 49 : 1309–1323. 10509822
32. Filmer D, Pritchett LH (2001) Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 38 : 115–132. 11227840
33. Filmer D, Pritchett L (1999) The effect of household wealth on educational attainment: evidence from 35 countries. Popul Dev Rev 25 : 85–120. doi: 10.1111/j.1728-4457.1999.00085.x
34. World Bank (2014) World development indicators. Available: http://data.worldbank.org/data-catalog/world-development-indicators. Accessed 26 Jan 2014.
35. Department for Economic and Social Affairs (2013) World population prospects: the 2012 revision. New York: United Nations.
36. ICF International (2012) Demographic and Health Survey sampling and household listing manual. Calverton (Maryland): ICF International.
37. Bertrand M, Duflo E, Mullainathan S (2004) How much should we trust difference-in-differences estimates? Q J Econ 119 : 249–275.
38. Brugiavini A, Pasini G, Trevisan E (2013) The direct impact of maternity benefits on leave taking: evidence from complete fertility histories. Adv Life Course Res 18 : 46–67. doi: 10.1016/j.alcr.2012.10.003 24797466
39. Staehelin K, Bertea PC, Stutz EZ (2007) Length of maternity leave and health of mother and child—a review. Int J Public Health 52 : 202–209. 18030952
40. Richardson V, Hernandez-Pichardo J, Quintanar-Solares M, Esparza-Aguilar M, Johnson B, et al. (2010) Effect of rotavirus vaccination on death from childhood diarrhea in Mexico. N Engl J Med 362 : 299–305. doi: 10.1056/NEJMoa0905211 20107215
41. Aaby P, Samb B, Simondon F, Seck AMC, Knudsen K, et al. (1995) Non-specific beneficial effect of measles immunisation: analysis of mortality studies from developing countries. BMJ 311 : 481–485. 7647643
42. WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality (2000) Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. Lancet 355 : 451–455. 10841125
43. Hajizadeh M, Heymann J, Strumpf E, Harper S, Nandi A (2015) Paid maternity leave and childhood vaccination uptake: longitudinal evidence from 20 low-and-middle-income countries. Soc Sci Med 140 : 104–117. doi: 10.1016/j.socscimed.2015.07.008 26210658
44. Ezeh OK, Agho KE, Dibley MJ, Hall J, Page AN (2014) Determinants of neonatal mortality in Nigeria: evidence from the 2008 demographic and health survey. BMC Public Health 14 : 521. doi: 10.1186/1471-2458-14-521 24886517
45. Zwane E, Masango S (2012) Factors influencing neonatal mortality: an analysis using the Swaziland Demographic Health Survey 2007. J Public Health Africa 3 : 18.
46. Mekonnen Y, Tensou B, Telake DS, Degefie T, Bekele A (2013) Neonatal mortality in Ethiopia: trends and determinants. BMC Public Health 13 : 483. doi: 10.1186/1471-2458-13-483 23683315
47. Titaley CR, Dibley MJ, Roberts CL (2012) Type of delivery attendant, place of delivery and risk of early neonatal mortality: analyses of the 1994–2007 Indonesia Demographic and Health Surveys. Health Policy Plan 27 : 405–416. doi: 10.1093/heapol/czr053 21810892
48. Nisar YB, Dibley MJ. (2014) Determinants of neonatal mortality in Pakistan: secondary analysis of Pakistan Demographic and Health Survey 2006–07. BMC Public Health 14 : 663. doi: 10.1186/1471-2458-14-663 24972633
49. Titaley CR, Dibley MJ (2012) Antenatal iron/folic acid supplements, but not postnatal care, prevents neonatal deaths in Indonesia: analysis of Indonesia Demographic and Health Surveys 2002/2003–2007 (a retrospective cohort study). BMJ Open 2: e001399. doi: 10.1136/bmjopen-2012-001399 23117564
50. Kumar C, Singh PK, Rai RK, Singh L (2013) Early neonatal mortality in India, 1990–2006. J Community Health 38 : 120–130. doi: 10.1007/s10900-012-9590-8 22797909
51. Victora CG, Requejo JH, Barros AJ, Berman P, Bhutta Z, Boerma T, et al. (2015) Countdown to 2015: a decade of tracking progress for maternal, newborn, and child survival. Lancet. 2015 Oct 15. doi: 10.1016/S0140-6736(15)00519-X
52. Oestergaard MZ, Inoue M, Yoshida S, Mahanani WR, Gore FM, Cousens S, et al. (2011) Neonatal mortality levels for 193 countries in 2009 with trends since 1990: a systematic analysis of progress, projections, and priorities. PLoS Med 8: e1001080. doi: 10.1371/journal.pmed.1001080 21918640
53. Vega J (2013) Universal health coverage: the post-2015 development agenda. Lancet 381 : 179–180. doi: 10.1016/S0140-6736(13)60062-8 23332947
Štítky
Interní lékařství
Článek vyšel v časopisePLOS Medicine
Nejčtenější tento týden
2016 Číslo 3- Není statin jako statin aneb praktický přehled rozdílů jednotlivých molekul
- Magnosolv a jeho využití v neurologii
- Moje zkušenosti s Magnosolvem podávaným pacientům jako profylaxe migrény a u pacientů s diagnostikovanou spazmofilní tetanií i při normomagnezémii - MUDr. Dana Pecharová, neurolog
- S prof. Vladimírem Paličkou o racionální suplementaci kalcia a vitaminu D v každodenní praxi
- Biomarker NT-proBNP má v praxi široké využití. Usnadněte si jeho vyšetření POCT analyzátorem Afias 1
-
Všechny články tohoto čísla
- Trans-Pacific Partnership Provisions in Intellectual Property, Transparency, and Investment Chapters Threaten Access to Medicines in the US and Elsewhere
- An Uninformative Truth: The Logic of Amarin’s Off-Label Promotion
- Performance of the GeneXpert Ebola Assay for Diagnosis of Ebola Virus Disease in Sierra Leone: A Field Evaluation Study
- Pragmatic Trials for Noncommunicable Diseases: Relieving Constraints
- Antibiotic Resistance in India: Drivers and Opportunities for Action
- Global Role and Burden of Influenza in Pediatric Respiratory Hospitalizations, 1982–2012: A Systematic Analysis
- Routine Pediatric Enterovirus 71 Vaccination in China: a Cost-Effectiveness Analysis
- Increased Duration of Paid Maternity Leave Lowers Infant Mortality in Low- and Middle-Income Countries: A Quasi-Experimental Study
- Planned Repeat Cesarean Section at Term and Adverse Childhood Health Outcomes: A Record-Linkage Study
- Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea
- A Novel Brief Therapy for Patients Who Attempt Suicide: A 24-months Follow-Up Randomized Controlled Study of the Attempted Suicide Short Intervention Program (ASSIP)
- Comparison of the Schwartz and CKD-EPI Equations for Estimating Glomerular Filtration Rate in Children, Adolescents, and Adults: A Retrospective Cross-Sectional Study
- Cardiovascular and Renal Outcomes of Renin–Angiotensin System Blockade in Adult Patients with Diabetes Mellitus: A Systematic Review with Network Meta-Analyses
- Length of Stay After Childbirth in 92 Countries and Associated Factors in 30 Low- and Middle-Income Countries: Compilation of Reported Data and a Cross-sectional Analysis from Nationally Representative Surveys
- Transformative Innovations in Reproductive, Maternal, Newborn, and Child Health over the Next 20 Years
- Compassionate and Proactive Interventions by Health Workers in the United Kingdom: A Better Approach to Prevent and Respond to Female Genital Mutilation?
- Translational Research for Tuberculosis Elimination: Priorities, Challenges, and Actions
- The Community As the Patient in Malaria-Endemic Areas: Preempting Drug Resistance with Multiple First-Line Therapies
- PLOS Medicine
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Experimental Treatment with Favipiravir for Ebola Virus Disease (the JIKI Trial): A Historically Controlled, Single-Arm Proof-of-Concept Trial in Guinea
- Comparison of the Schwartz and CKD-EPI Equations for Estimating Glomerular Filtration Rate in Children, Adolescents, and Adults: A Retrospective Cross-Sectional Study
- Performance of the GeneXpert Ebola Assay for Diagnosis of Ebola Virus Disease in Sierra Leone: A Field Evaluation Study
- A Novel Brief Therapy for Patients Who Attempt Suicide: A 24-months Follow-Up Randomized Controlled Study of the Attempted Suicide Short Intervention Program (ASSIP)
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



