-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
Authors: O. Vlasák 1,2; J. Škorpíková 1; Z. Hlinomazová 2; V. Kalandrová 2
Authors place of work: Biofyzikální ústav Lékařské fakulty MU, Brno, přednosta prof. RNDr. Vojtěch Mornstein, CSc. 1; Evropská oční klinika Lexum, lékařská ředitelka doc. MUDr. Zuzana Hlinomazová, Ph. D. 2
Published in the journal: Čes. a slov. Oftal., 74, 2018, No. 3, p. 87-91
Category: Původní práce
doi: https://doi.org/10.31348/2018/1/1-3-2018Summary
The work compares visual functions after cataract surgery and implantation of spherical (AAB00) and aspherical (ZCB00, MX60) intraocular lenses (IOL). The study was conducted in the years 2017–2018 at the European Eye Clinic Lexum Brno. The examined group contains 60 eyes. The study focused primarily on the comparison of distance corrected visual acuity (DCVA), the postoperative value of the total spherical aberration (SA), the depth of field (DoF) for the near and the contrast sensitivity. A single-factor ANOVA test was used for statistical analysis. Nearly all of the monitored values were statistically significantly better for the aspheric IOL group. It was DCVA (ZCB00: p = 0.048, MX60: p = 0.001), the total postoperative SA (ZCB00: p <0.000, MX60: p = 0.003) and contrast sensitivity in lower mesopic conditions (ZCB00: p=0,041; MX60: p = 0.012). Only DoF was statistically insignificant.
Keywords:
Spherical aberration, depth of field, contrast sensitivity, ZCB00, AAB00, MX60, DCVINTRODUCTION
In general, we know that of third-order aberrations, due to the low spatial angles, coma and spherical aberrations have the largest influence on vision. Other higher-order aberrations are virtually equal to zero in the ocular system. Thanks to angular symmetry, the possibility of correcting spherical aberration is better in comparison with angular asymmetric coma (1). The average corneal spherical aberration (SA) is +0.27 µm, in individuals of Asiatic race +0.37 µm (2). A spherical intraocular lens adds to this SA a further +0.15 µm. An aspherical lens provides better reduction of optical aberrations not only near the optical angle of the lens but also outside of it. As a result, it is an advantage to choose this lens for example in the case of decentred pupils, capsules or loosened suspensory apparatus of the lens. We also know from physical optics that both positive and negative SA increase the depth of field. Studies also show that SA with a value of -0.15 µm has a better influence on the depth of acuity than its positive form (3, 4). If SA is equal to zero, the patient should have higher maximum visual acuity at the expense of a lower depth of field (DoF) interval.
Fig. 1. Emmetropic eyes with 6 mm pupil and positive (A), negative (B) spherical aberration. The peripheral rays are refracted more than the paraxial. Same eyes after accommodative miosis (C and D). Elimination of peripheral rays and thereby also SA causes a hypermetropic (C) and myopic (D) shift. In the case of B-D there is therefore an improvement of near vision. 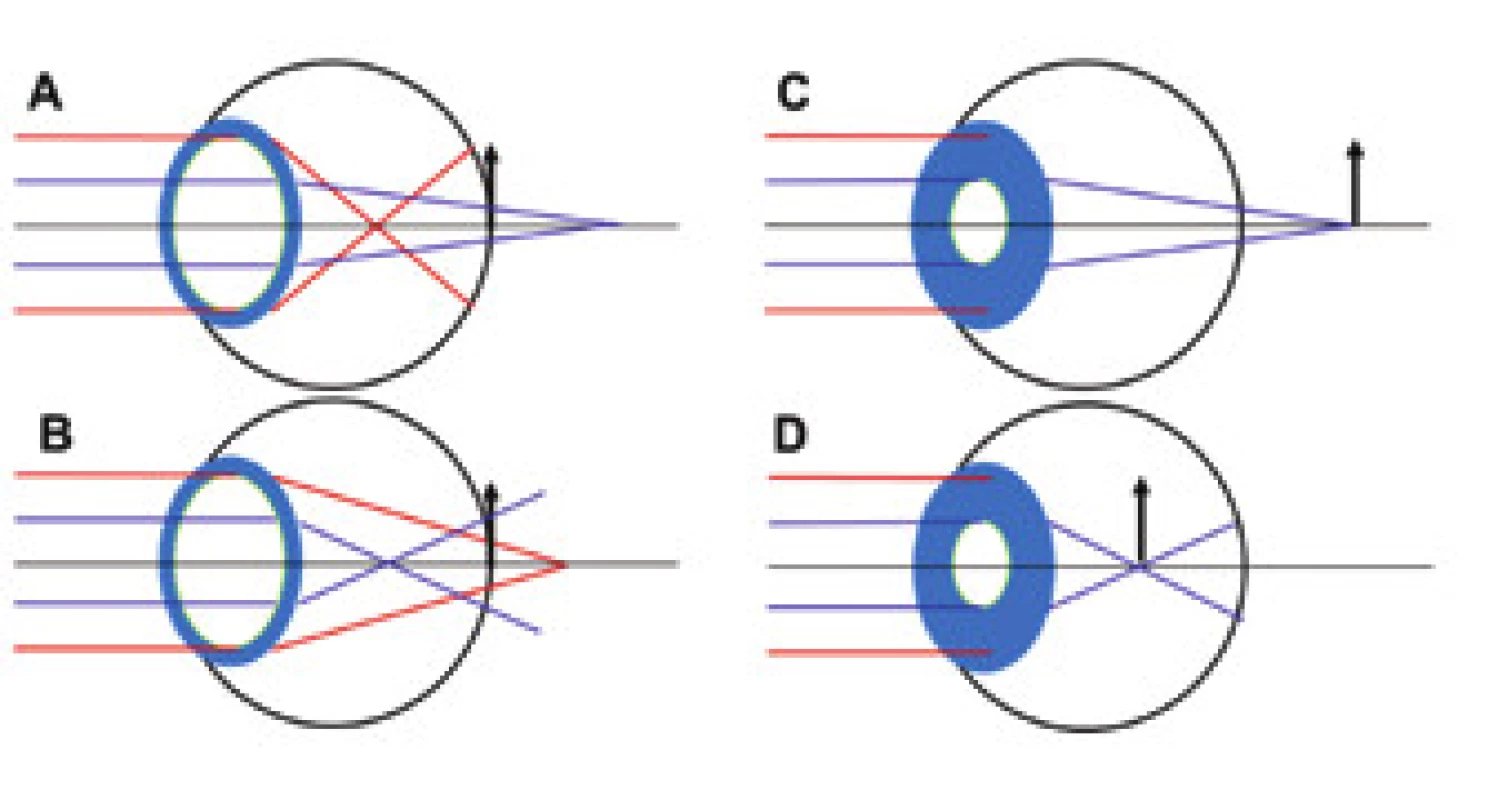
METHOD
The retrospective study contained 3 types of intraocular lens (IOL): aspherical enVista MX60 (n=20), Tecnis ZCB00 (n=20) and spherical Sensar AAB00 (n=20). These lenses influence SA in 6 mm of its optical part by the following values: enVista MX60 0.00 µm, Tecnis ZCB00 0.27 µm and AAB00 +0.15 µm. Corneal SA was measured preoperatively and postoperatively (min. 1 month) on an Atlas instrument (Carl Zeiss Meditec, Oberkochen, Germany) and Pentacam (Oculus Optikgerate GmbH, Wetzlar, Germany). Total SA was determined one month after surgery on a WASCA instrument (Carl Zeiss Meditec, Oberkochen, Germany). Pupil width was measured under lower mesopic conditions of approx. 1 lux (night vision with clear moon) (5). The evaluation was directly dependent on pupil width, i.e. if a pupil was measured at 3.65 mm, the values of higher-order aberrations were calculated from a zone of 3.5 mm, these zones were graded at 0.5 mm intervals. The minimum analysed zone in the study was 2.5 mm (pupil width was 2.65 mm), maximum 5.5 mm (pupil width was 5.66 mm). Only patients of European race were included in the study. Eyes which manifested any pathology influencing contrast sensitivity were excluded. Visual acuity and contrast sensitivity were measured with the aid of an automatic phoropter CV-5000Pro and optotype CC-100XP (Topcon, Tokyo, Japan). A total of 76 eyes were measured, of which 60 met the criteria for the study. The content of the postoperative follow-up examination was monocular and binocular subjective refraction (only Schöber's test), measurement of contrast sensitivity, depth of field with main level of acuity at 40 cm. Measurement of subjective refraction and affiliated quantities took place with lighting of approx. 301 lux (28fc). Contrast sensitivity was examined monocularly on 0.8 row with progressive reduction of contrast. For example, a resulting value of 1.0 means that the patient read row 0.8, which had contrast reduced by 50%. The main level of acuity (MLA) for near vision was set at a distance of 40 cm, in 100% of cases it was attained with the aid of the addition of +2.50 D. After stipulating the correct value of addition, DoF was measured. The patient was asked to fixate on 3 adjacent letters from a row 0.8 of the Snellen eye chart for near vision (this represents a size of 1 on Jaeger charts). The text was then progressively moved closer until the patient stated that he/she was no longer reliably able to distinguish the given letters. The text was then moved even closer until complete defocussing of perception took place, and the text was subsequently moved further away until the patient was again able to focus on the three letters. An arithmetical average was calculated from these two distance values, and the result was recorded as the near point with correction for near vision (Push up test). A similar procedure was applied in order to determine the far point with correction for near vision, with the difference that a more distant focus was sought. The resulting value of DoF was equal to the vergence of the difference of these two distances, and represented the “pseudo-accommodation” width of the patient's eye with a single-focus IOL (the depth at which the patient was able to read row 0.8). Patients were operated on by 3 experienced surgeons. A temporal entry incision with a width of 2.2 mm was always used. Data analysis was conducted in the STATISTICA 12 program (Statistica, Tulsa, OK, US). According to the frequency and graphic appearance of the histograms of data, a single-factor ANOVA test was used for statistical analysis. The statistical significance of the results was evaluated at a 5% level of significance (p <0.05).
RESULTS
Below we present selected results which we consider the most significant. The values of postoperative SA, DoF, DCVA and contrast sensitivity are graphically illustrated. A table with a description is affiliated to each graph. The value M represents the median of measured values for the given type of IOL.
Graph 1. Box graph of postoperative SA values 
Graph 2. Box graph of postoperative DCVA values 
Graph 3. Box graph of postoperative DoF values Box graph of depth of field in D grouped type of lens asph iol1 and 38v*60c 
Graph 4. Box graph of postoperative contrast sensitivity values. 
DISCUSSION
The preoperative value of corneal SA was 0.10 ± 0.06 µm, and did not differ statistically from the postoperative values (p=0.46). It is therefore possible to state that SA was not influenced by the surgical procedure upon cataract surgery. The same conclusion was reached also by T.M. Al-Sayyari (6). Jian-ping Liu (7) et al. conducted a meta-analysis of 7 studies examining the difference between a spherical AcrySof Natural and aspherical AcrySof IQ. Similarly as in our study, they determined that eyes after implantation of an aspherical IOL have statistically better contrast sensitivity in mesopic conditions and a lower value of total postoperative SA than eyes with spherical IOLs. They also stated that they did not find any statistically significant difference in postoperative visual acuity between these lenses (p=0.137), which differs from our study (ZCBOO: p=0.048; MX60: p=0.001). Few studies exist for an assessment of depth of field for near vision between spherical and aspherical IOLs. The best known studies are presented and compared by Xian-Hui Gong (8). These studies differ in their opinion of the effect of SA on DoF. K. Rocha and S. Marcos (4, 9) state that DoF is statistically higher in the group with higher SA. By contrast, M.R. Santhiago et al. (10) found no statistically significant correlation between SA and DoF. Xian also agrees with this situation, as do our results - our study confirmed a statistically significant difference in the total value of postoperative SA (ZCB00: p <0.000; MX60: p=0.003), while the DoF value between the groups however was statistically insignificant (ZCB00: p=0.97; MX60: p=0.51). The aspherical ZCB00 in fact had a slightly higher DoF value than AAB00 (1.35 D as against 1.32 D). Secondarily we observed maximum acuity for near distance. In the case of a spherical IOL, visual acuity in full DoF was relatively constant (row 0.8 virtually throughout the entire field), in the case of aspherical IOLs it attained higher maximum values (row 1.0+ in the centre of DoF and also a reduction of visual acuity occurred). Unfortunately we did not have Snellen eye charts for near vision for a higher value of vision 1.0, and for this reason we did not statistically evaluate this matter. However, it is possible to state that aspherical IOLs probably have a higher maximum visual acuity than spherical IOLs also for reading distance, without reducing DoF.
Tab. 1. Descriptive statistics of the whole sample 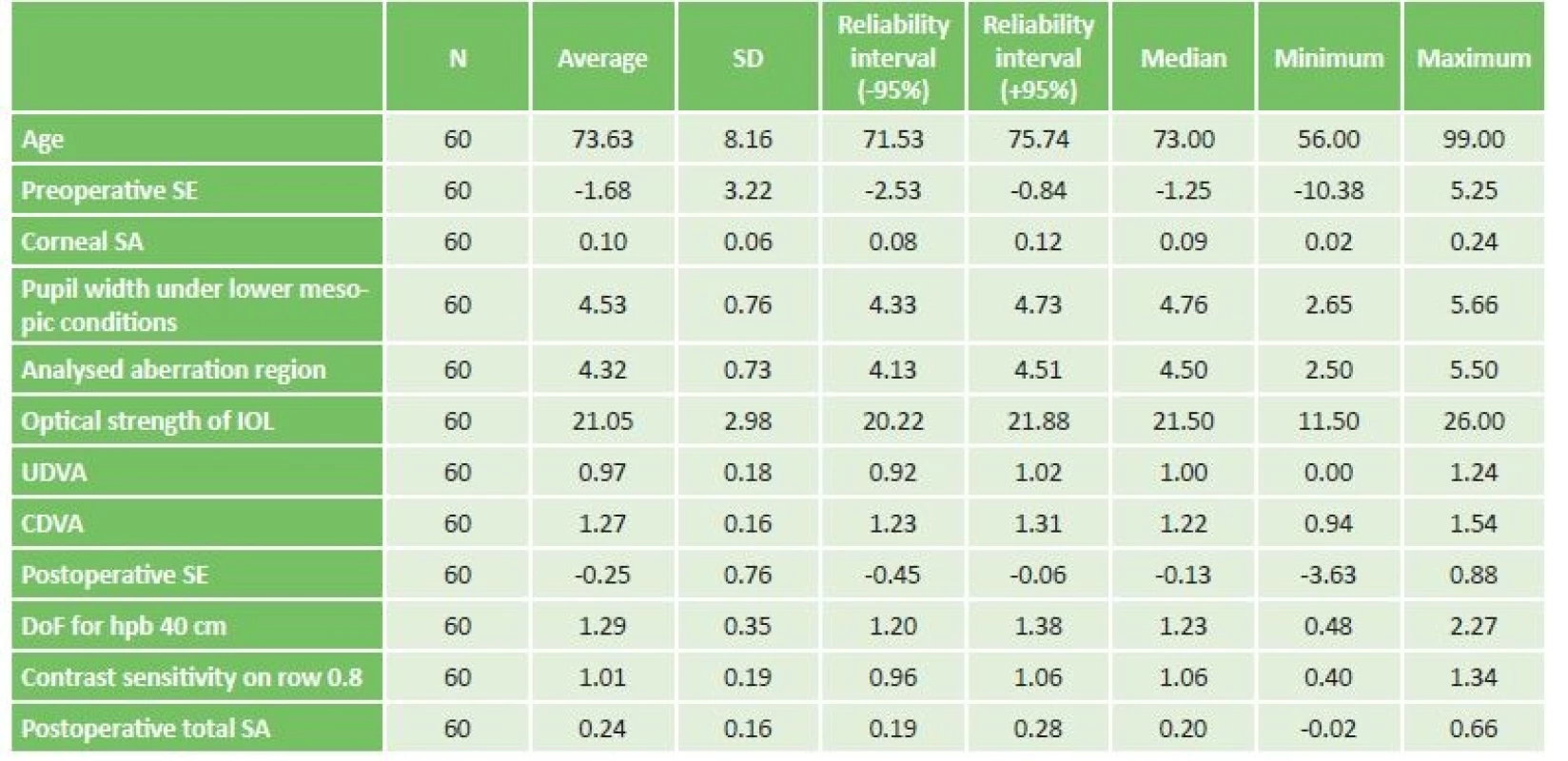
Abbreviations: SE – spherical equivalent, SA – spherical aberration, IOL – intraocular lens, UDVA – uncorrected distance visual acuity, CDVA – corrected distance visual acuity, DoF – depth of field Tab. 2. Category description of tested sample. 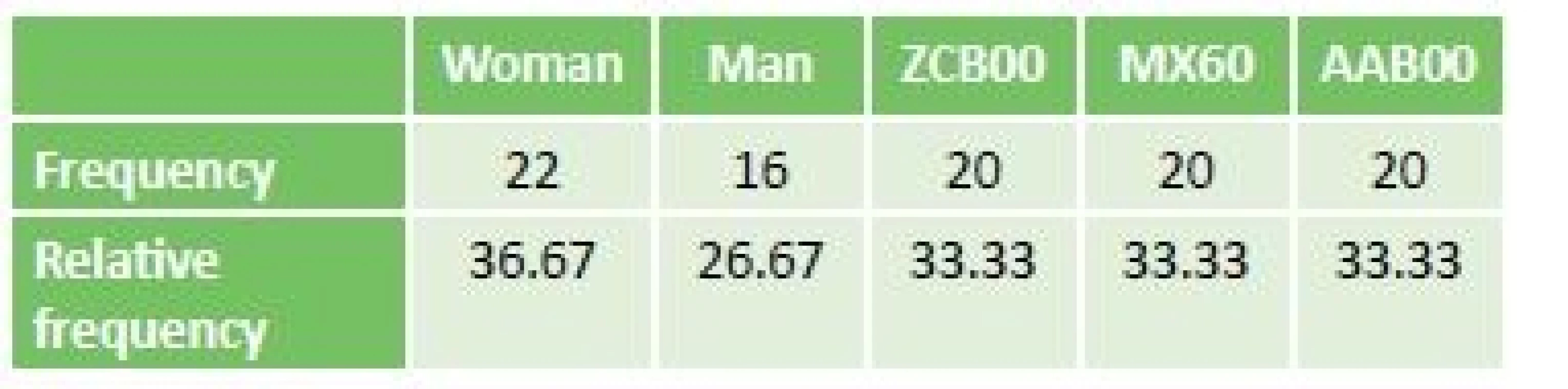
Tab. 3. Scanning descriptive statistics of the whole sample. 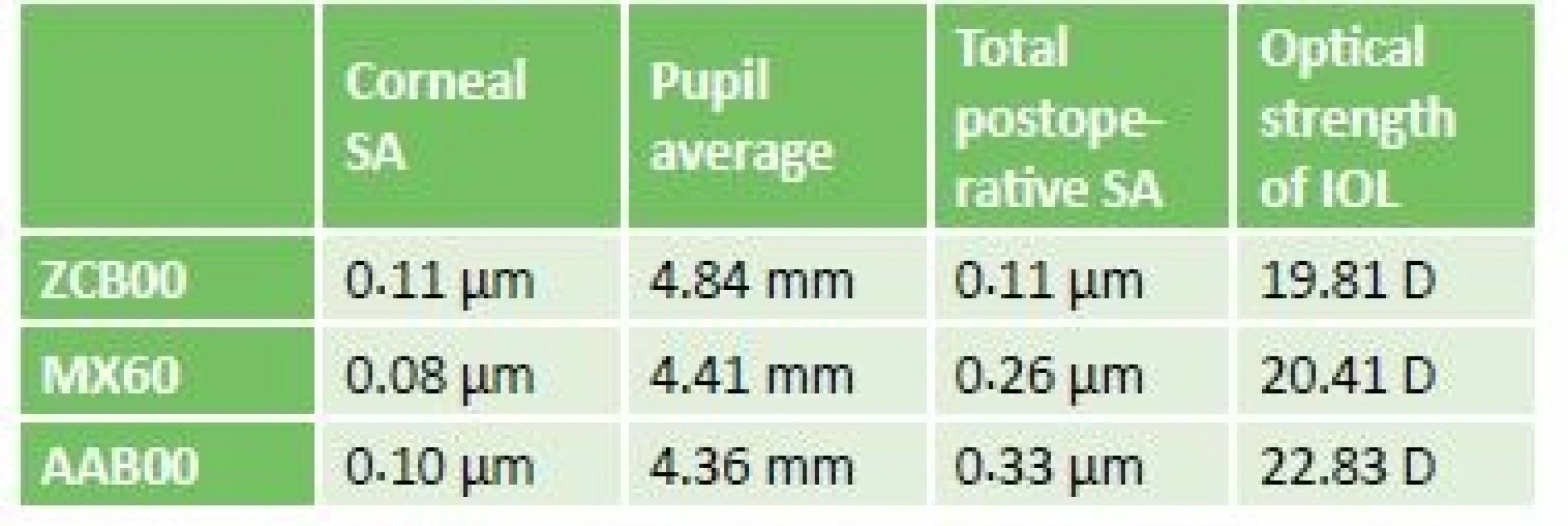
Initial values of SA, pupil widths were not significantly statistically different. Optical strength of IOL was statistically significantly higher in AAB00 implantations in comparison with ZCB00 (p = 0.007) and MX60 (p=0.038) Tab. 4. Statistics of difference of 3 types of IOL for SA. 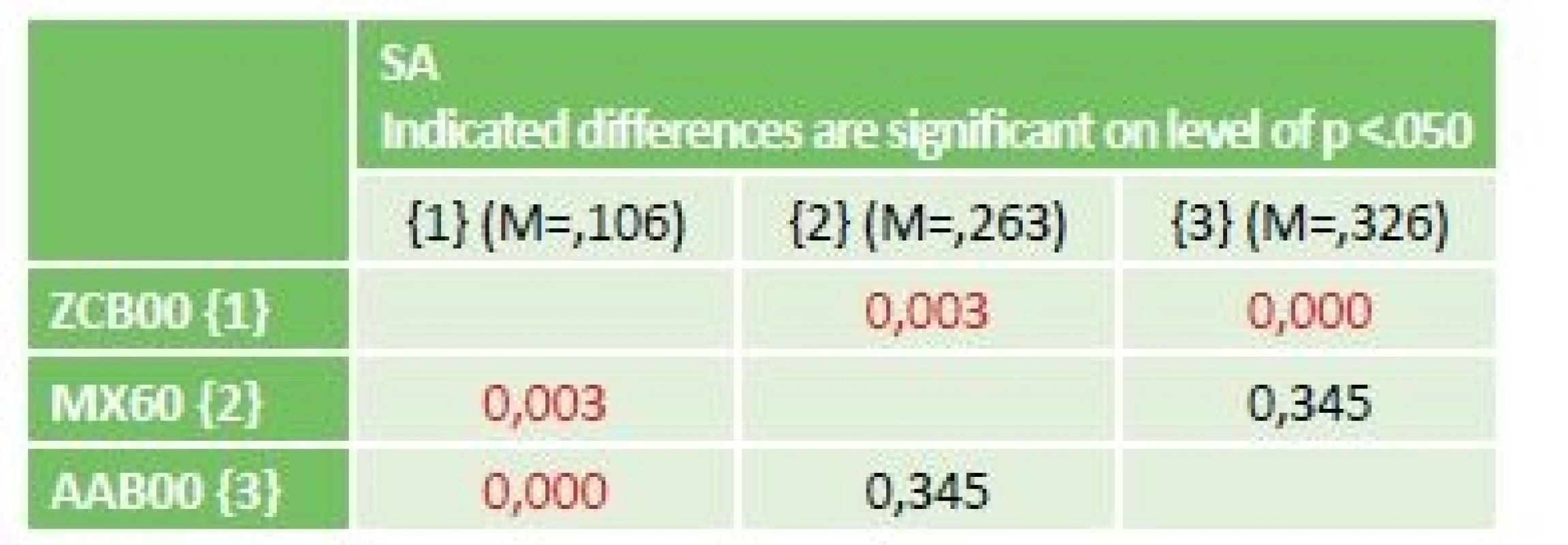
Total spherical aberration is postoperatively statistically significantly lower in the case of aspherical IOLs in comparison with spherical ones. Nominally ZCB00 (p<0.000), MX60 (p=0.003). Tab. 5. Statistics of difference of DCVA for 3 types of IOL. 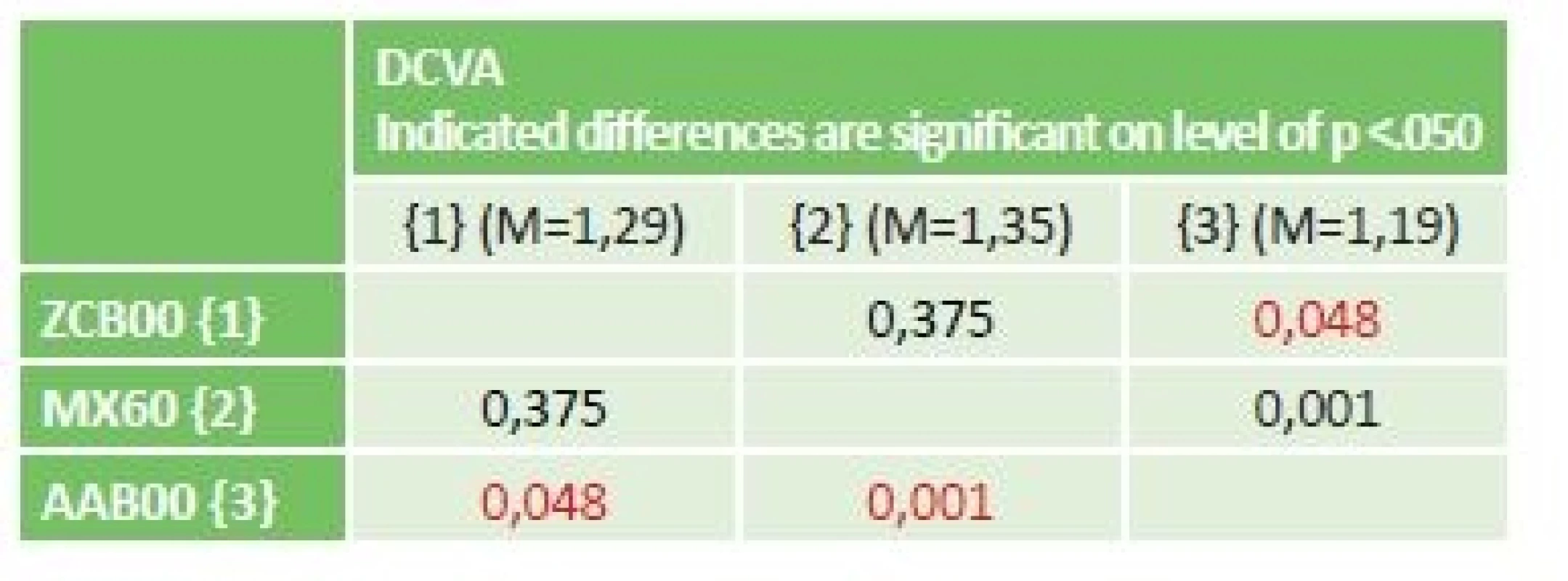
DCVA is postoperatively statistically significantly higher Tab. 6. Statistics of difference of DoF for 3 types of IOL. 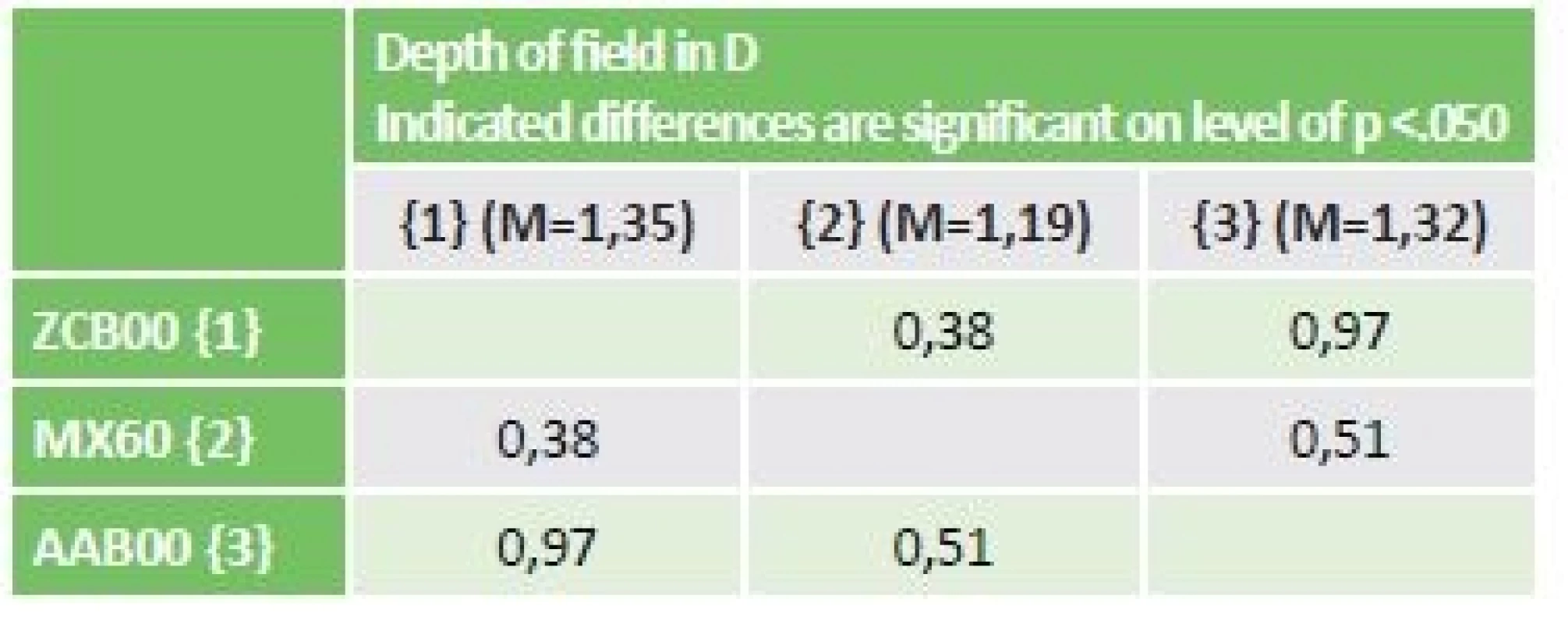
Tab. 7. Statistics of difference of contrast sensitivity for 3 types of IOL. 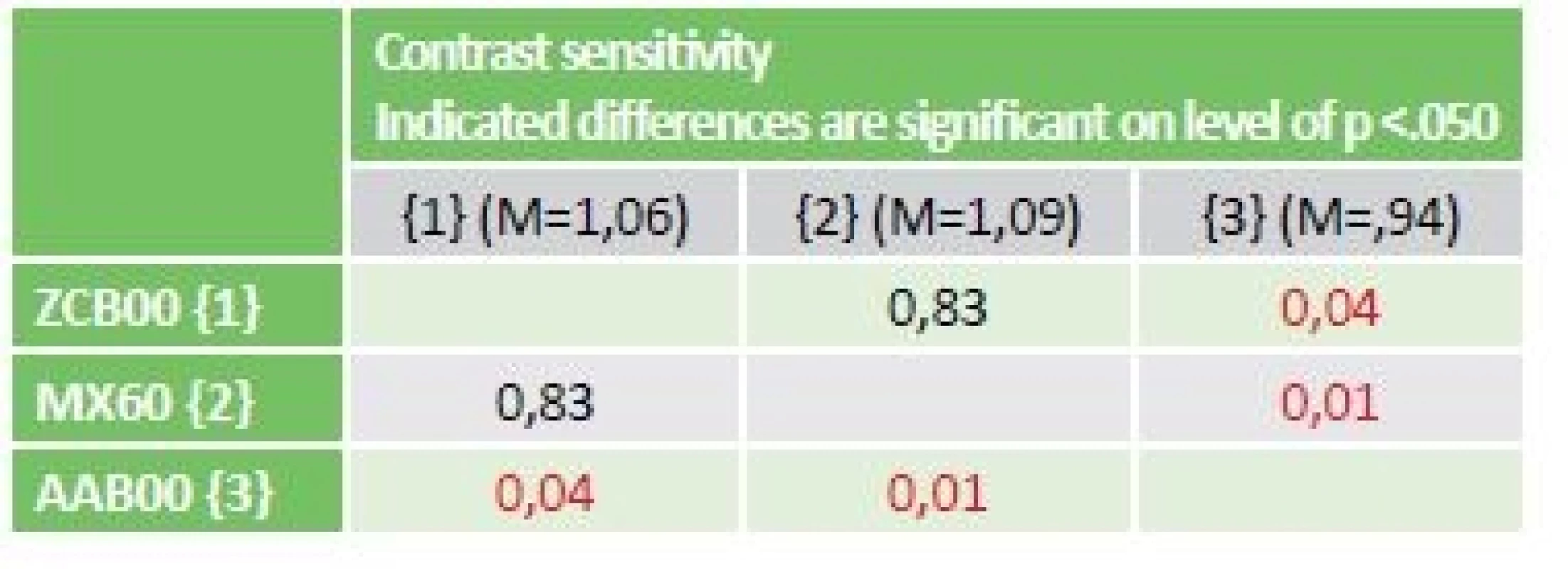
Tab. 8. Scanning descriptive statistics of depth of field 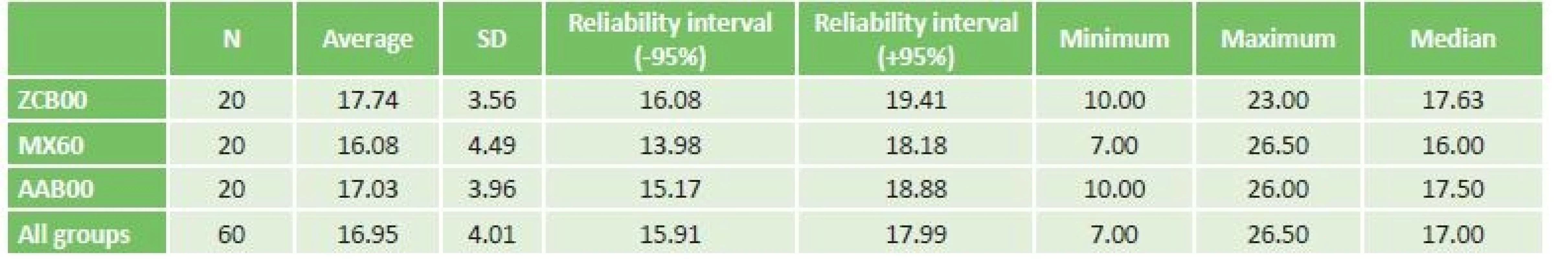
Overview of DoF values in cm for all three types of IOL. CONCLUSION
From the measured results and the above information, it ensues that the choice of an aspherical intraocular lens is ideal for patients with wide pupils, with a requirement for maximum possible visual acuity and contrast, and also for patients with a higher dioptric value of the IOL. Scientific articles written on this issue also mention a benefit in the form of better optical homogeneity, which is thus an advantage for patients with a decentred optic system of the eye (loosened suspensory apparatus, eccentric pupil etc.) (11). Both aspherical IOLs (ZCB00, MX60) attained higher values of corrected distance visual acuity (ZCB00: p=0.048; MX60: p=0.001), better contrast sensitivity in lower mesopic conditions (ZCB00: p=0.041; MX60: p=0.012) and lower total postoperative SA (ZCB00: p<0.000; MX60: p=0.003) than in the case of the spherical AAB00. The difference in depth of field for near vision (40 cm) between these IOLs was not statistically significant.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Mgr. Ondřej Vlasák, Ph.D.
Biofyzikální ústav Lékařské fakulty MU, Brno
Zdroje
1. Porter, J., Guirao, A., Cox, IG. et al.: Monochromatic aberrations of the human eye in a large population. J Opt Soc Am A Opt Image Sci Vis. 2001;18(8):1793-1803.
2. Beiko, G.: Understanding Corneal Asphericity and IOLs. https://www.reviewofophthalmology.com/article/understanding-corneal-asphericity-and-iols. Accessed June 26, 2018.
3. Bakaraju, RC., Ehrmann, K., Papas, EB. et al.: Depth-of-Focus and its Association with the Spherical Aberration Sign. A Ray-Tracing Analysis. J Optom. 2010;3(1):51-59. doi:10.3921/joptom.2010.51
4. Marcos, S., Barbero, S., Jiménez-Alfaro, I.: Optical quality and depth-of-field of eyes implanted with spherical and aspheric intraocular lenses. J Refract Surg Thorofare NJ 1995. 2005;21(3):223-235.
5. Zele, AJ., Cao, D.: Vision under mesopic and scotopic illumination. Front Psychol. 2015;5. doi:10.3389/fpsyg.2014.01594
6. Al-Sayyari, TM., Fawzy, SM., Al-Saleh, AA.: Corneal spherical aberration and its impact on choosing an intraocular lens for cataract surgery. Saudi J Ophthalmol. 2014;28(4):274-280. doi:10.1016/j.sjopt.2014.06.005
7. Liu, J-P., Zhang, F., Zhao, J-Y. et al.: Visual function and higher order aberration after implantation of aspheric and spherical multifocal intraocular lenses: a meta-analysis. Int J Ophthalmol. 2013;6(5):690-695. doi:10.3980/j.issn.2222-3959.2013.05.27
8. Gong, X-H., Zheng, Q-X., Wang, N. et al.: Visual and optical performance of eyes with different corneal spherical aberration implanted with aspheric intraocular lens. Int J Ophthalmol. 2012;5(3):323-328. doi:10.3980/j.issn. 2222-3959.2012.03.14
9. Rocha, KM., Soriano, ES., Chamon, W. et al.: Spherical aberration and depth of focus in eyes implanted with aspheric and spherical intraocular lenses: a prospective randomized study. Ophthalmology. 2007;114(11):2050-2054. doi: 10.1016/j.ophtha.2007.01.024
10. Santhiago, MR., Netto, MV., Barreto, J. et al.: Wavefront analysis, contrast sensitivity, and depth of focus after cataract surgery with aspherical intraocular lens implantation. Am J Ophthalmol. 2010;149(3):383-389.e1-2. doi:10.1016/j.ajo. 2009.09.019
11. Atchison, DA.: Optical design of intraocular lenses. II. Off-axis performance. Optom Vis Sci Off Publ Am Acad Optom. 1989;66(9):579-590.
Štítky
Oftalmologie
Článek vyšel v časopiseČeská a slovenská oftalmologie
Nejčtenější tento týden
2018 Číslo 3- Stillova choroba: vzácné a závažné systémové onemocnění
- Familiární středomořská horečka
- Léčba chronické blefaritidy vyžaduje dlouhodobou péči
- První schválený léčivý přípravek pro terapii Leberovy hereditární optické neuropatie dostupný rovněž v ČR
- Kontaktní dermatitida očních víček
-
Všechny články tohoto čísla
- Očný nález u pacienta s loweovým synrómom
- Rodina s výskytom marshallovho a stickelerovho syndrómu
- Vrozená centrální choriorentinitida toxoplasmové etiologie - kazuistika
- 24. výroční konference Eye Advance 2018
- Zemřela moje maminka, MUDr. Vlasta Doležalová, CSc.
- Asférické čočky a jejich vliv na zrakovou ostrost, hloubku ostrosti, sférickou aberaci a kontrastní citlivost
- Spojkové lézie - vzťah papilómov a skvamocelulárného karcinómu spojovky s infekciou HPV
- Oční nálezy u akutních leukémií
- Česká a slovenská oftalmologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Oční nálezy u akutních leukémií
- Asférické čočky a jejich vliv na zrakovou ostrost, hloubku ostrosti, sférickou aberaci a kontrastní citlivost
- Vrozená centrální choriorentinitida toxoplasmové etiologie - kazuistika
- Rodina s výskytom marshallovho a stickelerovho syndrómu
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



