-
Články
- Vzdělávání
- Časopisy
Top články
Nové číslo
- Témata
- Kongresy
- Videa
- Podcasty
Nové podcasty
Reklama- Kariéra
Doporučené pozice
Reklama- Praxe
Comparative Analysis of the Results of Laparoscopic and Traditional Cholecystectomy in the Patients with Acute Cholecystitis
Srovnávací analýza výsledků laparoskopické a tradiční cholecystektomie u pacientů s akutní cholecystitidou
Cíl:
Účelem studie je srovnávací analýza chirurgické léčby pacientů s akutní cholecystitidou, kteří se podrobili laparoskopické nebo tradiční cholecystektomii. Metody a výsledky: Byly analyzovány výsledky léčby 204 pacientů přijatých do vojenské nemocnice ministerstva obrany republiky Uzbekistán. 109 pacientům byla provedena laparoskopická cholecystektomie (LCE – skupina I ) a 95 pacientům byla provedena tradiční cholecystektomie (TCE – skupina II). Věk pacientů se pohyboval mezi 16 a 79 roky, žen bylo 161 (78,9 %) a mužů 43 (21,1 %). Katarální cholecystitida byla diagnostikována u 73 (35,3 %), flegmonozní u 84 (41,2 %) a gangrenozní u 48 (23,5 %) pacientů. U všech těchto pacientů jsme chtěli provést laparoskopickou operaci. Pokud v době přijetí nebyly sonografické známky destrukce stěny žlučníku a konzervativní léčba byla účinná během 12–24 hodin, pak byla operace provedena odloženě. Pokud se objevily destruktivní změny ve stěně žlučníku, byla provedena okamžitá operace. Ozáření low power laserem na oblast žlučníku před operací mělo příznivý vliv na zmenšení zánětlivých změn ve stěně žlučníku i okolí, infiltrativní a jizevnaté změny se staly snadněji preparovatelnými a okolní struktury byly snadněji identifikovány. Úmrtnost byla 2 pacienti (1,4 %) z 98 ve skupině tradiční cholecystektomie a žádná úmrtnost ve skupině laparoskopické. Závěr: 1. Časná laparoskopická operace u destruktivní formy akutní cholecystitidy dovoluje snížit výskyt intraoperačních komplikací a zkrátit dobu výkonu. 2. U nemocných se značnými jizevnatými změnami v oblasti zadní stěny žlučníku a při obtížné preparaci oblasti jaterního parenchymu byla použita plazmalaserová nebo elektrická koagulace. 3. Použití nízkovoltážního laserového ozáření v předoperační přípravě pacientů s akutní cholecystitidou podstatně usnadnilo techniku LCE a snížilo výskyt intra - i postoperačních komplikací.Klíčová slova:
akutní cholecystitis – laparoskopická cholecystektomie – tradiční cholecystektomie
Authors: B. N. Shamirzaev
Authors place of work: The Central Military Clinical Hospital of the Ministry of Defense, Tashkent, The Republic of Uzbekistan
Published in the journal: Gastroent Hepatol 2010; 64(5): 10-14
Category: Původní práce
Summary
The aim:
A comparative analysis and ways to improve the results of surgical treatment of patients with acute cholecystitis who have undergone laparoscopic or traditional methods. Methods and Results: This report presents an analysis of the results of the treatment of 204 patients admitted to the Military Clinical Hospital of the Ministry of Defence of the Republic of Uzbekistan with acute caculous cholecystitis. Of them, 109 patients underwent laparoscopic cholecystectomy (LCE – group I) and 95 traditional cholecystectomy (TCE – group II). The age of the patients fluctuated from 16 to 79 years, females made up 161 of patients (78.9%), males 43 (21.1%). Catarrhal cholecystitis was diagnosed in 72 (35.3%) patients, acute phlegmonous in 84 (41.2%) and acute gangrenous in 48 (23.5%) patients. We consider that the attempt to perform LCE may be carried out on all patients with acute cholecystitis. If at the moment of admission to the hospital echo-signs of gallbladder wall destruction were not found, conservative therapy, as a rule, gave positive effects even after 12–24 hours, resulting in a reduction in the inflammatory process – the surgery was carried out after delayed period. During the appearance of destructive changes in the gallbladder wall, urgent surgical intervention was performed. The use of low-power laser irradiation (LGLR) on the area of the gallbladder in the process of the patient’s preoperative preparation resulted in a significant decrease in inflammatory changes in its wall and in the surrounding tissues. During the operation, infiltrates and scar tissues become loose, easily separated, and the effect of “sliding” occurs allowing fast identification of the organs and tubular structures in the zone of operation. The total lethality was 2 (1.4%) of 95 patients after TCE. There were no lethal outcomes in the group of patients who had undergone the laparoscopic method of treatment. Conclusion: 1. The performance of early laparoscopic operation in destructive forms of acute cholecystitis allows the avoidance of intraoperative complications during separation of the rough scar-infiltrative conglomerates in the hepato-pancreatic-duodenal zone, and shortening of the duration of the operation. 2. In patients with rough scar changes in the area of the gallbladder posterior wall, all the posterior wall or such parts of it that cannot be isolated from the liver bed remain in place with consequent performance of plasma laser or electric coagulation of the mucous membrane. 3. The use of low-power laser irradiation in the preoperative period considerably facilitates the technique of LCE in patients with acute cholecystitis, and reduced intra - and postoperative complications. 4. The course of laser therapy in different forms of acute cholecystitis results in a decrease in morphological changes in the organs of the hepato-pancreatic-duodenal zone.Key words:
cholecystitis – laparoscopic cholecystectomy – open cholecystectomyIntroduction
The problem of surgical treatment of the cholelethiasis still remains significant all over the world [4,5,8,13]. The worldwide distribution of cholelethiasis and the appearance of new surgical technologies define this problem as extremely important in modern surgery, despite existing unresolved and disputable issues [3–5,11].
For today, a cholecystectomy, according to its frequency rate of performance, lies first in the list of operations of scheduled abdominal surgery [1,4,5,12]. In modern clinics around the world the rate of laparoscopic cholecystectomies carried out even in acute cholecystitis exceeds 90% [2,3,6,7].
The indications for laparoscopic surgery of the gallbladder and bile ducts have considerable increased in recent years, however, problems have remained. Among the most important are: disadvantages of intraoperative diagnosis, duct injuries in non-complicated and complicated cholecystitis, difficult cholecystectomies in infiltrated, sclerotic processes of the hepato-pancreatic-duodenal zone, choledocholithiasis, Mirizzi‘s syndrome, cholecysto-intestinal fistulas, scars after previous laparotomies, accompanying diseases, thromboembolic complications in laparoscopic procedures and others [9,10,12].
The purpose of our study was to carry out a comparative analysis and find ways to improve the results of surgical treatment of patients with acute cholecystitis who had undergone laparoscopic and traditional methods.
Materials and Methods
This work presents an analysis of the results of the treatment of 204 patients admitted with acute calculous cholecystitis to the Central Military Clinical Hospital of the Ministry of Defence of the Republic of Uzbekistan. Of them, 109 patients underwent laparoscopic cholecystectomy (LCE – group I) and 95 patients – traditional cholecystectomy (TCE – group II). The age of patients fluctuated from 16 to 79 years, 161 (78.9%) patients were female and 43 (21.1%) male. The distribution of patients according to age is presented in tab. 1. Catarrhal cholecystitis was diagnosed in 72 (35.3%) patients, acute phlegmonous in 84 (41.2%) and acute gangrenous in 48 (23.5%) (tab. 2).
Tab. 1. Distribution of patients in relation to age. Tab. 1. Rozdělení pacientů podle věku. 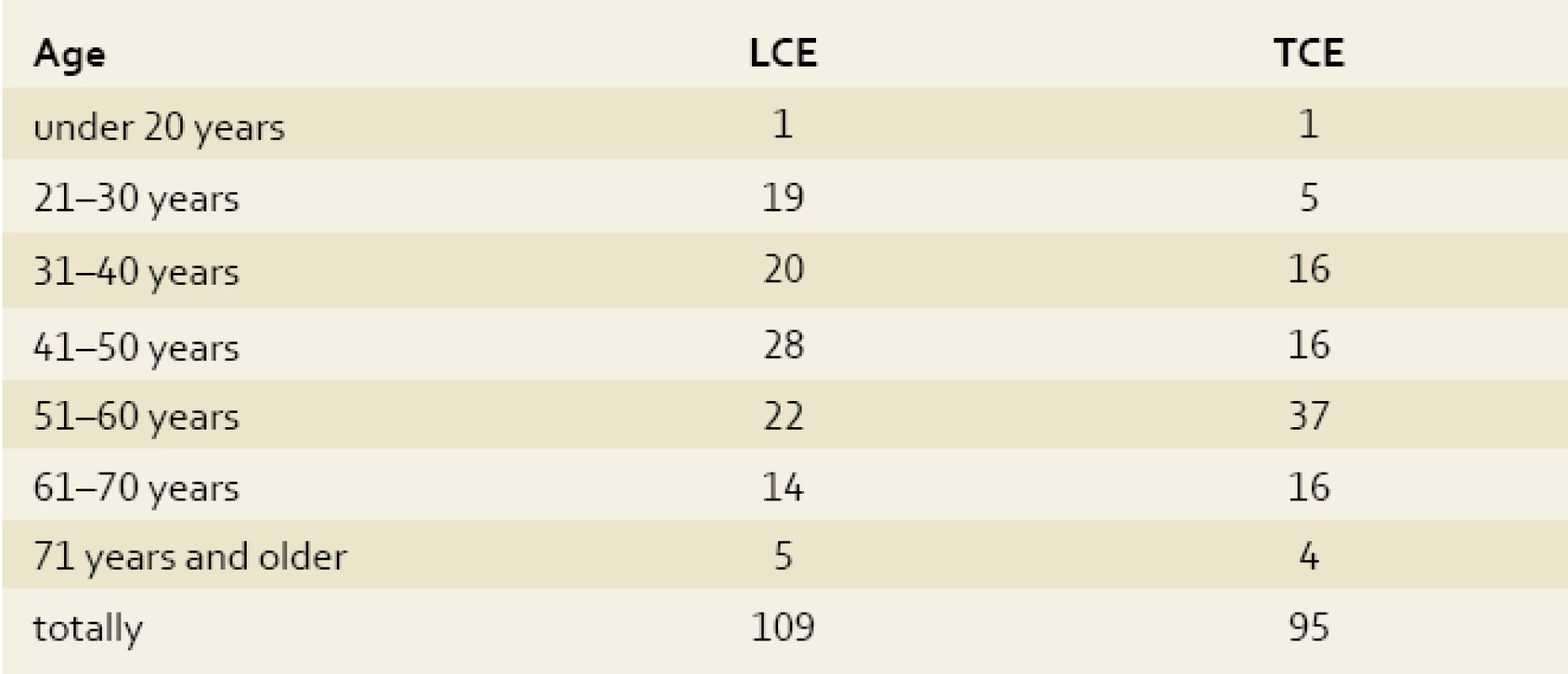
Tab. 2. Clinical forms of acute calculous cholecystitis. Tab. 2. Klinické formy akutní kalkulózní cholecystitidy. 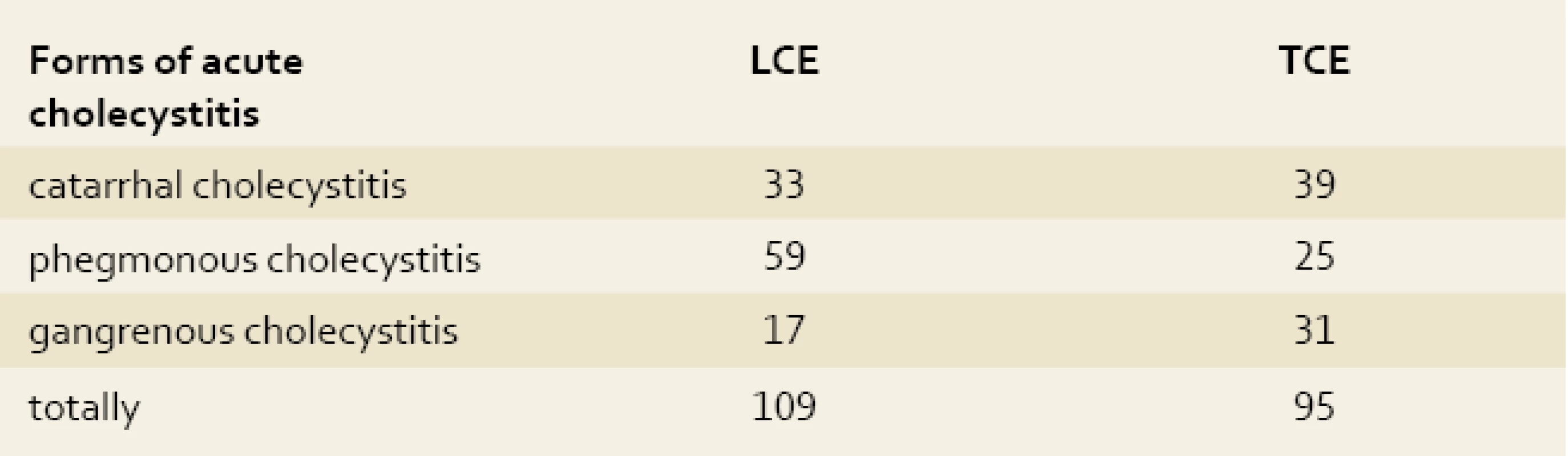
The gallbladder was isolated in half the patients in LCE and TCE. Paracystic abscesses were noted in 4 patients, 2 cases in each group. Vesico-choledocheal and vesico-duodenal fistulas were diagnosed in 3 patients in the first group and in one patient from the second group. Serous and serous-fibrinous local limited peritonitis was noted in 10 patients from group I and 2 patients in group II.
At admission, all the patients underwent general clinical, biochemical blood and urine analysis, coagulogram, electrocardiography (ECG), ultrasound investigations of the abdominal cavity (US), X-ray investigation of the lungs, echocardiography if required, fibrogastroduodenoscopy, computed tomography, and endoscopic retrograde pancreatocholangiography (ERPC). Ultrasound investigations were performed with convex (3.5 MHz), linear (7.5 MHz) and multifrequency transformers using Logic-200 ultrasound scanners from Philips (Holland) and the Prosound “Aloka-3500” (Japan) in real time. FGDS was performed by the standard technique of the 30K Getex video systems series (Japan) with the use of a 9.8 mm EG-2931K gastroscope. ERPC and stones extraction from biliary ducts was performed with the use of 12mm JF 1T2O duodenoscopes from Olympus (Japan) and pools of instruments including papillotomes from Demling and a Dormia basket. Laparoscopic operations were performed with the use of apparatuses from Karl Storz (Germany) and instruments from Karl Storz and PPP (Russia). The procedures were performed under endotracheal anaesthesia by standard technique in the American variant.
For open laparoscopy from the mini--approach there was used the “Mini assistant” (LIGA-7) suite of instruments developed by SAN (Yekaterinburg). Operative access was transrectal incision in the right hypochondrium of length 3.5–5 cm (mean – 4 cm) beginning from the costal arch and 2–2.5 cm to the right of the middle line.
Preoperative preparation of 30 patients with acute forms of cholecystitis before LCE included radiation on the area of the gallbladder and epigastric puncture with low-intensity magneto-infrared laser for which a Sogdiana magnetolaser apparatus (Russia) generating laser radiation in the impulse regimen and infrared spectrum with wave length 0.89 µm in the persistent magnetic field with voltage 35 mTl was used. The power of laser irradiation in the impulse was 8–14 mWt, output mean power was 4–7 mWt. The frequency of the impulse was 600–100 Hz. The radiation was performed transcutaneously at 3–5 points for 60–120 sec.
Tissue samples from the liver and gallbladder were fixed in 10–12% solution of formalin with phosphate buffer from Lilly for light microscopy. Paraffin slices were stained with hematoxylin-eosin.
Results and Discussion
The major part of patients in the preoperative period received conservative treatment as a preoperative preparation. During treatment, all patients were under dynamic ultrasonographic observation. If at the moment of admission to the hospital echo signs of gallbladder wall destruction were not visualized, then a conservative therapy, as a rule, even in 12–24 hours gave a positive response resulting in a reduction in the inflammatory process.
Out of 109 laparoscopic operations, performance of LCE was achieved in 95 (87.15%) patients. The causes of conversion of laparoscopy into laparotomy are shown in tab. 3.
Tab. 3. The causes of conversion to the open surgery or mini-laparotomy access. Tab. 3. Příčiny přechodu na otevřený chirurgický zákrok nebo minilaparotomii. 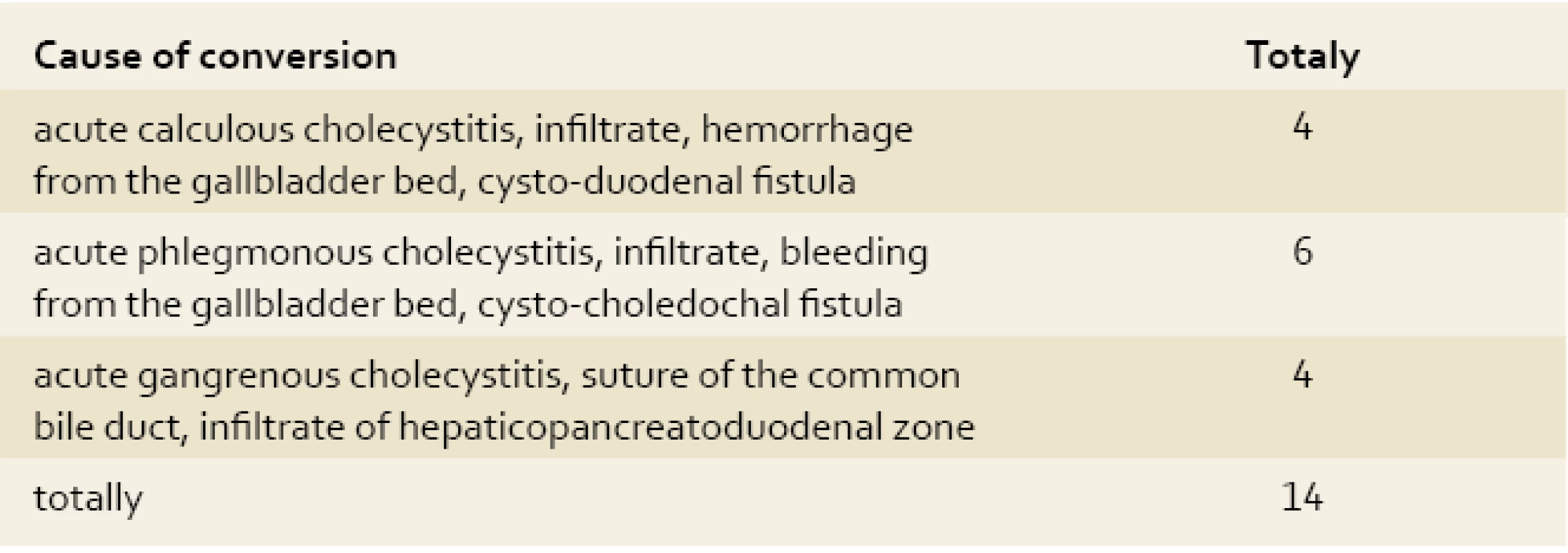
Patients with obstructive cholecystitis immediately received conservative treatment. If destruction was not seen during the first day then treatment was considered successful and continued until the inflammatory process disappeared and late surgery was indicated. If destruction of the gallbladder wall was recognised, an urgent surgical procedure was performed.
The attempts at conservative treatment of patients suffering from destructive cholecystitis failed in all of them. There was noted the obvious fact of a lack of correlation between ultrasound findings of the disease and its clinical symptoms. In 5 of the 109 patients receiving prolonged conservative treatment due to acute destructive cholecystitis, gangrene of the gallbladder wall developed with a marked infiltrative and adhesive process in surrounding organs, including the gallbladder. All 5 patients had conversion of laparoscopy into laparotomy or mini-laparotomy.
In our experience, LCE should be performed on all patients with acute cholecystitis. However, it is recommended to complete the operation with the laparotomy method if during the laparoscopy process scarring and infiltrative changes in the area of the operation are seen, to avoid prolongation of operation time and iatrogenic lesions of the surrounding organs. The time factor is very important for performance of LCE. A delayed operation in destructive forms of cholecystitis increases technical difficulties during cholecystectomy.
In ten patients during laparoscopic cholecystectomy we saw a situation where it was impossible to detach the posterior wall of the gallbladder from the liver bed without injury. In the initial stages of the use of this technique, in 4 patients we tried to remove the whole gallbladder and 2 patients received bile discharge from the bed with the development of peritonitis in one patient. In one patient we had to tamponate the bed of the gallbladder through epigastric puncture and in the other one perform laparotomy with suturing of the bleeding bed. Later the whole posterior wall or its sites which cannot be isolated from the liver bed were preserved with the performance of plasma laser or electric coagulation. No complications in any patient were noted.
The most frequent intraoperative complication during cholecystectomy in acute cholecystitis was bleeding from a damaged cystic artery or its branches (tab. 4). The difficulties of stopping parenchymatous hepatic bleeding during open laparotomy procedure were the reason for tampon insertion into the bed of the gallbladder in 3 (3.15%) patients. Such surgical tactics induce healing of the postoperative wound with secondary tension, and a defect in the aponeurosis to the formation of postoperative hernia.
Tab. 4. Intraoperative complications in the patients with acute calculous cholecystitis. Tab. 4. Intraoperační komplikace u pacientů s akutní kalkulózní cholecystitidou. 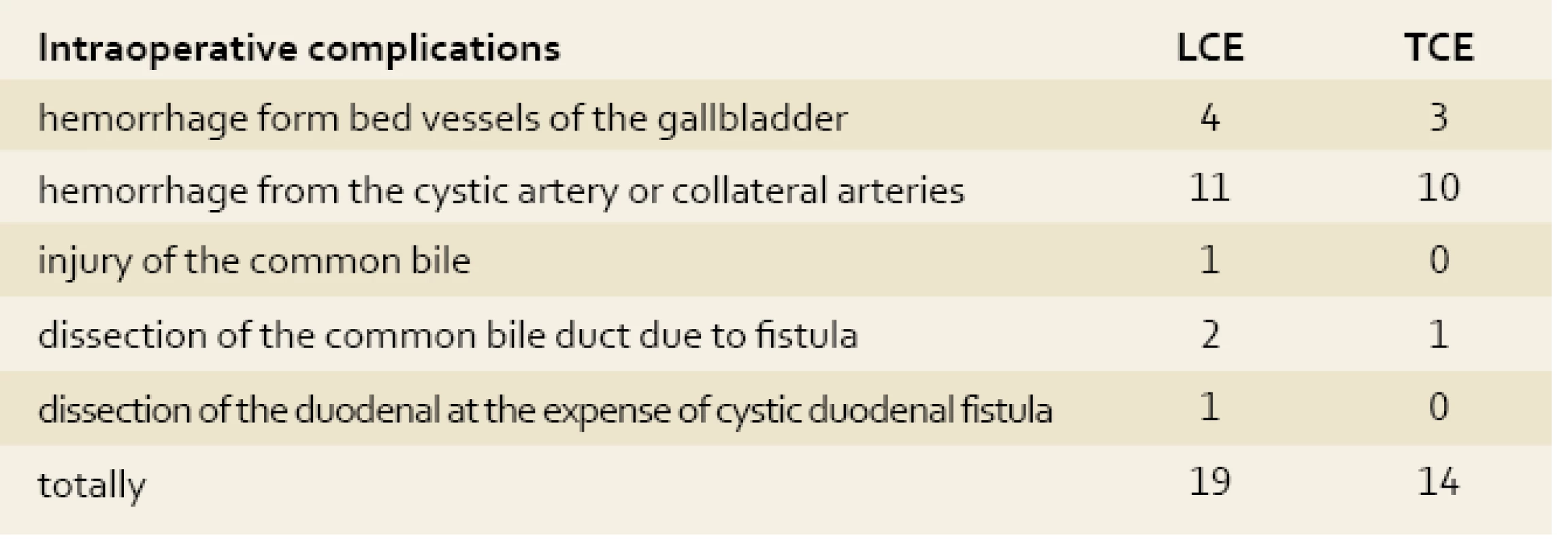
The number of postoperative complications in LCE was 2 times lower than in TCE (tab. 5). The number of suppurations of postoperative wound and trocar punctures in both groups was almost equal, however, the consequences of these suppurations have a more severe course than in patients with laparotomy.
Tab. 5. Postoperative complications in the patients with acute cholecystitis Tab. 5. Postoperační komplikace u pacientů s akutní cholecystitidou. 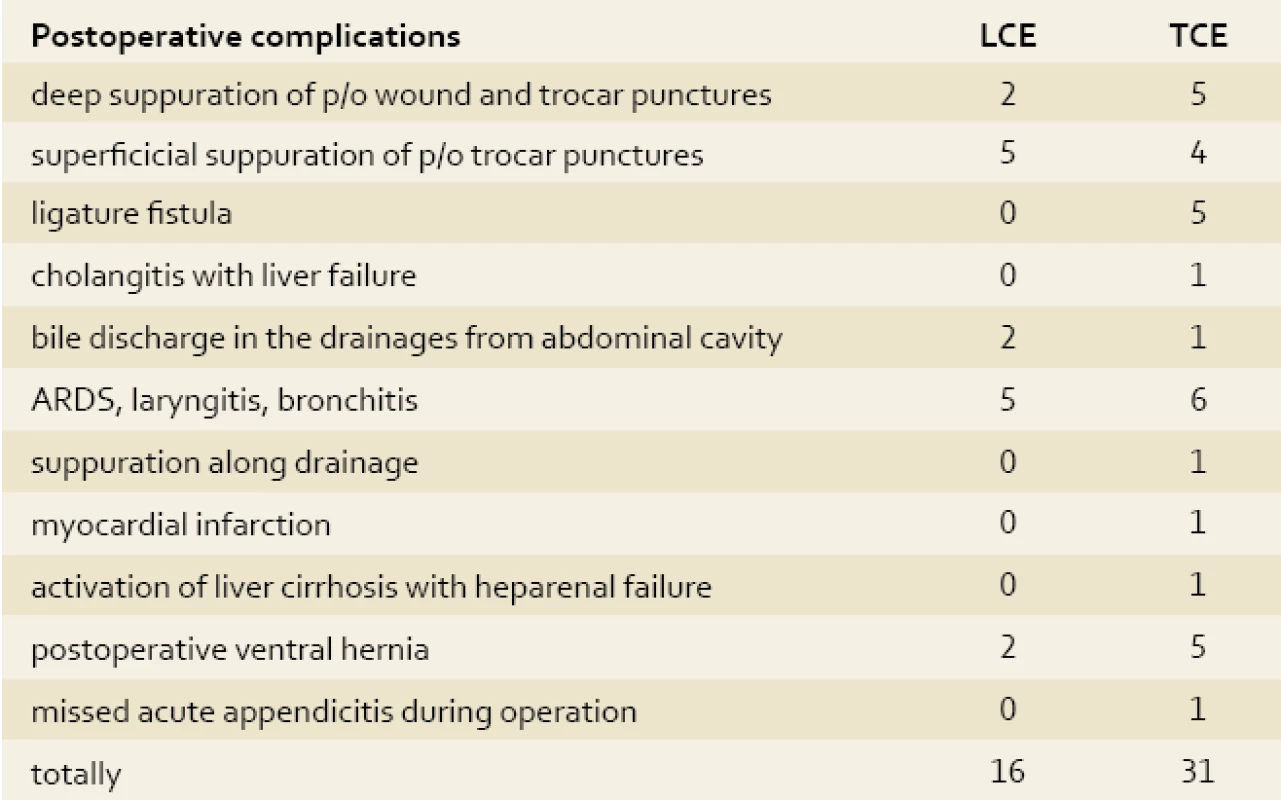
As the results of operations and morphological investigations showed, even 1–2 laser irradiations of the zone of the gallbladder during the process of patient preparation for the operative procedure significantly reduced inflammatory changes in its wall and surrounding tissues. Reduction of signs of oedema and inflammatory changes was particularly marked in the mucosa and muscular membranes. The above-mentioned processes were accompanied with changes in the microvessels of both the blood and lymphatic beds. During operation, infiltrates and scarred tissues become loose, easily separate, the effect of “sliding” occurs allowing quick identification of organs and tubular structures in the zone of operation. There was no infection found in the epigastral puncture (point of gallbladder removal) in any patient after irradiation by low-intensity laser irradiation.
The operation time in laparoscopic intervention is related considerably to terms of operation from the moment of destructive changes appearing in the gallbladder wall. In active surgical tactics during urgent operation after identification of the ultrasonographic picture of acute destructive cholecystitis, the average time was 93 minutes and in waiting tactics 162 minutes.
The period of rehabilitation depended directly on the time of operation. The shorter the duration of anaesthesia and operative intervention, the faster the rehabilitation of the patients.
The number of postoperative bed-days is the most characteristic indicator of the efficacy of treatment of patients undergoing laparoscopic and traditional laparotomy methods. The duration of patients’ stays in hospital after traditional laparotomic cholecystectomy was approximately 2 times longer than after laparoscopic (5–7 and 3–4, resp.). The severity of the postoperative period significantly depends on the presence and severity of accompanying diseases and the level of homeostasis disturbance at the moment of intervention. Trauma of the laparotomy operation, as a rule, intensifies the clinical course of accompanying pathology. In spite of marked inflammatory changes in HPDZ, the absence of additional trauma of the anterior gallbladder wall appeared to be critical and provides quicker rehabilitation of patients who have undergone the laparoscopic procedure.
The total lethality was 2 (1.4%) patients out of 95 after TCE. The activation of liver cirrhosis with hepatorenal insufficiency and large myocardial infarction were the causes of the lethal outcome in both patients. There were no lethal outcomes in the group of patients with laparoscopy procedure.
Conclusion
- Early laparoscopic cholecystectomy in the destructive form of acute cholecystitis allows the avoidance of intraoperative complications due to separation of rough scarred-infiltrative adhesions in the hepato-pancreatic-duodenal zone and shortening of operation time.
- In patients with rough scar changes in the area of the gallbladder posterior wall, the whole wall or such parts of it that cannot be separated from the liver bed remained present after performing plasma laser or electric coagulation of mucosa.
- The use of low-intensity laser irradiation in the preoperative period significantly facilitates the technique of LCE performance in patients with acute cholecystitis and reduces intra - and operative complications.
- The course of laser therapy in different forms of acute cholecystitis reduces the severity of morphological changes in the organs of the hepato-pancreatic-duodenal area.
Shamirsaev Bakhtier Nadjiyullaevich Candidate of Medical Sciences
The Central Military Clinical Hospital of the Ministry of Defense
Tashkent, 100202
The Republic of Uzbekistan
bahtier-88@inbox.ru
Zdroje
1. Emelyanov SI. Illustrirovannoe rukovodstvo po endoskopicheskoj chirurgii.Moskau. 2004 : 214.
2. Madartov KM, Dustbaev A, Goziev AK et al. Laparoskopicheskaya hirurgiya ostrogo holecistita. Materiali XII moskovskogo mejdunarodnogo kongressa po endoskopicheskoy hirurgii. Moscow 2008 : 256–257.
3. Ukhanov AP,Baydo SV, Chahmakhchev SR et al. Ispolzovanie laparoskopicheskoy holecystectomii pri ostrom chorecystite u geriatricheskih bolnih Material XII Moskovskogo mejdunarodnogo kongressa po endoskopicheskoy horurgii. Moscow 2008 : 428–430.
4. Fedorov AV, Krivtcov GA, Karpov OE et al. Puti uluchsheniya resultatov lechenia bolnih jelchekamennoy boleznyu. Emdoskopicheskaya hirurgia 2008; 4 : 3–5.
5. Fedorov IV, Sigal EI, Clavin LE. Endoskopicheskaya hirurgiya. Moskau, GEOTAR-Media 2009 : 544.
6. Yarosh VN, Romanov YA. Laparoscopic cholecystectomy v lechenii zabolevaniy jelchnogo pusira. Material XII Moskovskogo mejdunarodnogo kongressa po endoskopicheskoy horurgii. Moscow 2008 : 489–491.
7. Yartcev PA, Gulayev AA, Blagovestov DA et al. Videolaparoskopia v urgentnoy abdominalnoy hirurgii. Material XII Moskovskogo mejdunarodnogo kongressa po endoskopicheskoy horurgii. Moscow 2008 : 491–493.
8. Gurusamy K, Samraj K, Gluud C et al. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 2010; 97(2): 141–150.
9. Paran H, Zissin R, Rosenberg E et al. Prospective evaluation of patients with acute cholecystitis treated with percutaneous cholecystectomy and interval laparoscopic cholecystectomy. Int J Surg 2006; 4 (2): 101–105.
10. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients Surg.Endosc, 2009, Dec 25/ (Epub ahead of print).
11. Salih M, Hamid S, Shah HA et al. Endoscopic management of biliary leaks afteropen and laparoscopic cholecystectomy. J Pak Med Assoc 2007; 57(3): 117–119.
12. Singhal T, Balakrishnan S, Hussain A et al. Laparoscopic subtotal cholecystectomy: initial experience with laparoscopic management of difficult cholecystitis. Surgeon 2009; 7(5): 263–268.
13. Wilson E, Gurusamy K, Gluud C et al. Cost-utility and value-of-formation analysis of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 2009; 97(2): 210–219.
Štítky
Dětská gastroenterologie Gastroenterologie a hepatologie Chirurgie všeobecná
Článek vyšel v časopiseGastroenterologie a hepatologie
Nejčtenější tento týden
2010 Číslo 5- Horní limit denní dávky vitaminu D: Jaké množství je ještě bezpečné?
- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejlepší kůže je zdravá kůže: 3 úrovně ochrany v moderní péči o stomii
-
Všechny články tohoto čísla
- Comparative Analysis of the Results of Laparoscopic and Traditional Cholecystectomy in the Patients with Acute Cholecystitis
- Place of sorafenib in the treatment of hepatocellular carcinoma
- Gastrointestinal Stromal Tumour: Cause of Obscure Gastrointestinal Bleeding
-
The efficacy of maintenance therapy in ulcerative colitis is influenced by the pharmacokinetics of mesalazine and by adherence to medicamentous therapy
Commentary to the PODIUM study - Prof. MUDr. Jiří Ehrmann CSc. turned seventy
- ASNEMGE/EAGE 7th summer school of gastroenterology
-
Jiří Ehrmann, Petr Hůlek. Hepatologie.
Praha: Grada 2010.
616 stran - Kalendář gastroenterologických akcí 2011
- Treatment of patients with acute pancreatitis in the Slovak Republic – survey
- Gastroenterologie a hepatologie
- Archiv čísel
- Aktuální číslo
- Informace o časopisu
Nejčtenější v tomto čísle- Prof. MUDr. Jiří Ehrmann CSc. turned seventy
- Treatment of patients with acute pancreatitis in the Slovak Republic – survey
- Place of sorafenib in the treatment of hepatocellular carcinoma
- Comparative Analysis of the Results of Laparoscopic and Traditional Cholecystectomy in the Patients with Acute Cholecystitis
Kurzy
Zvyšte si kvalifikaci online z pohodlí domova
Autoři: prof. MUDr. Vladimír Palička, CSc., Dr.h.c., doc. MUDr. Václav Vyskočil, Ph.D., MUDr. Petr Kasalický, CSc., MUDr. Jan Rosa, Ing. Pavel Havlík, Ing. Jan Adam, Hana Hejnová, DiS., Jana Křenková
Autoři: MUDr. Irena Krčmová, CSc.
Autoři: MDDr. Eleonóra Ivančová, PhD., MHA
Autoři: prof. MUDr. Eva Kubala Havrdová, DrSc.
Všechny kurzyPřihlášení#ADS_BOTTOM_SCRIPTS#Zapomenuté hesloZadejte e-mailovou adresu, se kterou jste vytvářel(a) účet, budou Vám na ni zaslány informace k nastavení nového hesla.
- Vzdělávání



