-
Medical journals
- Career
PATIENT SATISFACTION AFTER BREAST RECONSTRUCTION: IMPLANTS VS. AUTOLOGOUS TISSUES
Authors: S. Fracon; N. Renzi; M. Manara; V. Ramella; G. Papa; Z. M. Arnež
Authors‘ workplace: Department of Medicine, Surgery and health Sciences, University of Trieste, Italy
Published in: ACTA CHIRURGIAE PLASTICAE, 59, 3-4, 2017, pp. 120-128
INTRODUCTION
At present breast reconstruction is increasingly considered an integral part of the treatment of breast cancer. 1,2
Other than physical, it offers to the reconstructed patients also the psycho-social satisfaction. This is the reason why, today, reconstructive surgery should be proposed to all women who will be/are having oncologic breast surgery.3
Due to the increasing number of patients seeking breast reconstruction, it is necessary to evaluate the impact of the results of reconstruction on the patients’ quality of life.4
Basically, there are two different types of breast reconstruction: alloplastic reconstruction by tissue expanders and/or implants, or autologous reconstruction by pedicle or free flaps.
To obtain the best possible result, the two types of reconstruction can be used also in combination.
Flaps used in breast reconstruction are, either local (e.g LICAP – lateral intercostal artery perforator flap, AICAP – anterior intercostal artery perforator flap), regional (e.g LD – latissimus dorsi flap, TDAP – thoracodorsal artery perforator flap), distant (pedicled TRAM – transverse rectus abdominis flap) or free (e.g. DIEAP – deep inferior epigastric perforator flap, SGAP/IGAP – superior or inferior gluteal artery perforator flap, TUG – transverse upper gracillis flap etc.). In most patients the treatment is concluded with nipple reconstruction and areola-nipple complex tattoo.
In their studies many authors searched for the best technique of breast reconstruction.
Tam et al. analysed 63 articles to compare results obtained in terms of breast reconstruction.5 He found a consensus in the literature on higher patient satisfaction with autologous reconstruction. On the other hand, however, he found that breast reconstruction by implants was by far more popular. This fact can be explained by greater complexity, invasiveness as well as longer hospital-stay and rehabilitation after autologous reconstruction.
Damen et al. found that 90% of women reconstructed by DIEAP flaps perceived the reconstructed breast as their own.6
Fischer et al. report that free flap reconstructions needed fewer surgical procedures, the complications and failures were not frequent and the patients required fewer clinical visits and reached a complete result faster than patients reconstructed with expanders/implants.7
Tsoi et al confirmed this evidence.8 They found that the infection rate and operation failure rate (removal of the implant), was higher in patients reconstructed with implants compared to those reconstructed with autologous tissue. The risk factors associated with failure of reconstruction include smoking, obesity, paucity of donor tissues and type II diabetes mellitus (DMII).9,10
Ohkuma et al. showed improvement of the quality of life postoperatively after both autologous and alloplastic breast reconstruction.11 However, they also found that autologous reconstruction was associated with a higher rate of functional impairment.
Macadam et al. studied the alloplastic breast reconstruction and showed that silicone implants were associated with greater satisfaction with breast reconstruction outcome (physical, psychological and sexual).12
This was confirmed by McCarthy who stressed also the negative effects of radiotherapy on reconstructed tissues.13
Reaby et al. and Ng et al. showed that some women refused breast reconstruction, which could be explained by advanced age, their greater fear of a second operation, but also with problems in communication with their surgeon.14,15
Regarding the last, Ho et al. showed that a woman satisfied with the communication with the surgeon was also happier with the final aesthetic result of reconstruction.16
The aim of our study is to investigate which technique of breast reconstruction (by alloplastic or autologous technique), offered the highest quality of life to the patients. For this reason, we surveyed all women who experienced a successful breast reconstruction at our institution between 2007 and 2016. We used the BREAST-Q patient-reported outcomes measurement as the primary instrument to measure their quality of life and satisfaction with the outcomes.
MATERIAL AND METHODS
This study was aimed at all patients who underwent breast reconstruction after mastectomy at the University Hospital “ASUITS” in Trieste, between 2007 and 2016.
The patients were divided into two groups: alloplastic reconstructions (with or without a flap) and autologous reconstructions.
The initial cohort of patients was composed of 98 patients reconstructed with a DIEAP flap, 137 reconstructed with implants, 16 with latissimus dorsi flap only and 19 with latissimus dorsi flap and an implant.
Only the patients who had successfully completed the reconstruction were included into the study.
From this reason we excluded all patients who had had complications in terms of failure of the reconstructive procedure such as loss of the flap or the implant.
The full completion of breast reconstruction means reconstruction of the breast mound with or without nipple-areola complex reconstruction or contralateral adjustment.
Excluded from the study were also women who did not sign the informed consent form, did not attend outpatient clinics until removal of all sutures and women with psychiatric disorders.
The study involved patients seen for follow-up visits at the Plastic and Reconstructive Surgery Unit of Cattinara Hospital, from November 2015 until April 2016.
109 patients were enrolled into the study, 59 (54%) women were reconstructed with implants and 50 (46%) with autologous tissues (Fig.1).
1. The group of patients in the study 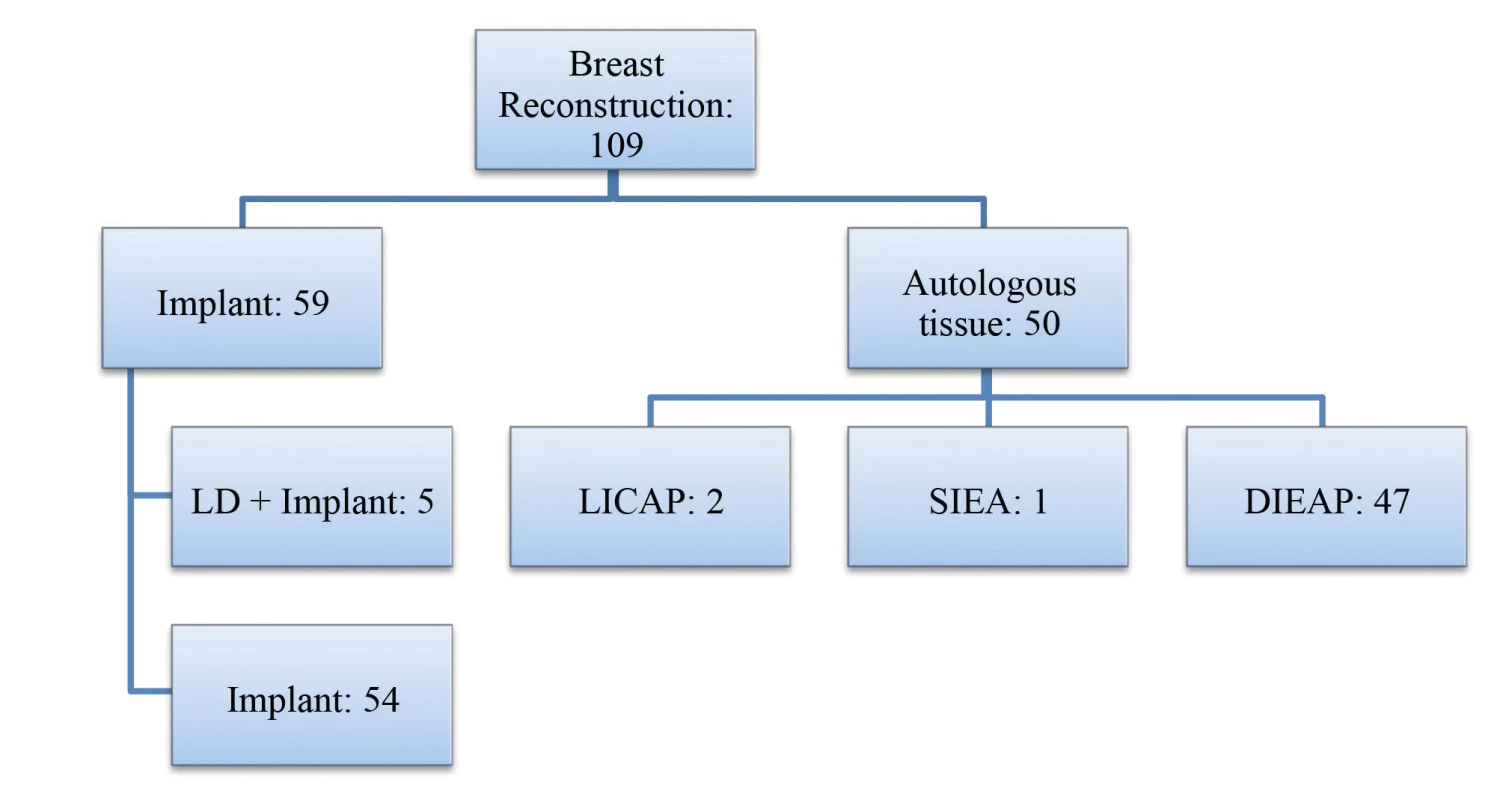
The BREAST-Q patient-reported outcomes measure was used to evaluate the outcome of breast reconstruction as perceived by the patients.17
BREAST-Q questionnaire is one of the few instruments in reconstructive breast surgery that satisfies the international standards in terms of development and validation.
The aim of BREAST-Q is to evaluate the impact of breast reconstruction on quality of life and satisfaction from the patient’s perspective.
We used the BREAST-Q postoperative reconstruction module (https://eprovide.mapi-trust.org/), consisting of nine scales. Each one consists of three to five items using a Likert scale.
The score obtained from each scale is transformed into a 100-point scale, where 0 means very dissatisfied and 100 very satisfied.
The score transformation is made by a free software available at the same Internet website.
By using BREAST-Q it is possible to evaluate the quality of life in terms of psychosocial, sexual and physical wellbeing as well as satisfaction with outcomes of breast reconstruction and information.
All scales have a good internal consistency (Cronbach alpha varies from 0.88 to 0.97).3
The two groups were divided according to the time passed from surgery, to assess if and how it affected the overall satisfaction of patients. We divided the patients into four time intervals: 0–6 months, 6–12 months, 1 to 3 years and more than 3 years after reconstruction.
For each patient we analysed her medical history (other surgical treatments, radiotherapy, chemotherapy, age at the reconstruction and at the questionnaire (Table 1, Table 2), body mass index (BMI), comorbidity, and smoking (Table 3). We also divided complications into major – those requiring operative interventions (e.g. postoperative thrombotic event, flap loss, haematoma) and minor – requiring non-surgical therapy (cellulitis, seroma, infections).
1. Patient’s age distribution for each time intervals at the reconstruction 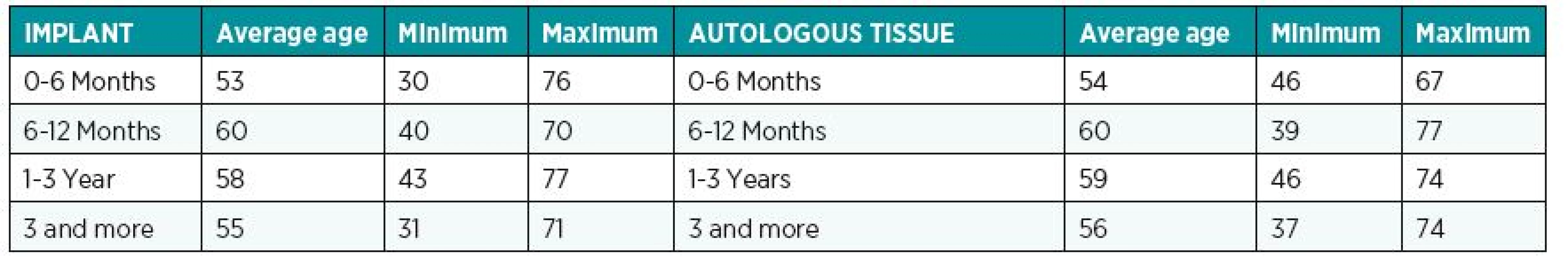
2. Patient’s age distribution for each time intervals at the Breast-Q questionnaire 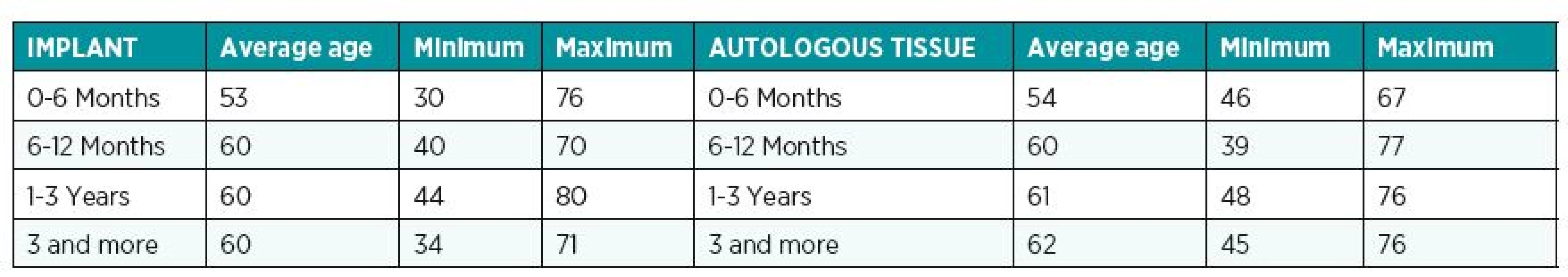
3. Distribution of smoking, CT (chemotherapy), RT (radiotherapy), hypertension, dyslipidemia, diabetes, NAC (nipple areola complex), reconstruction, BMI (body mass index), complications for each groups 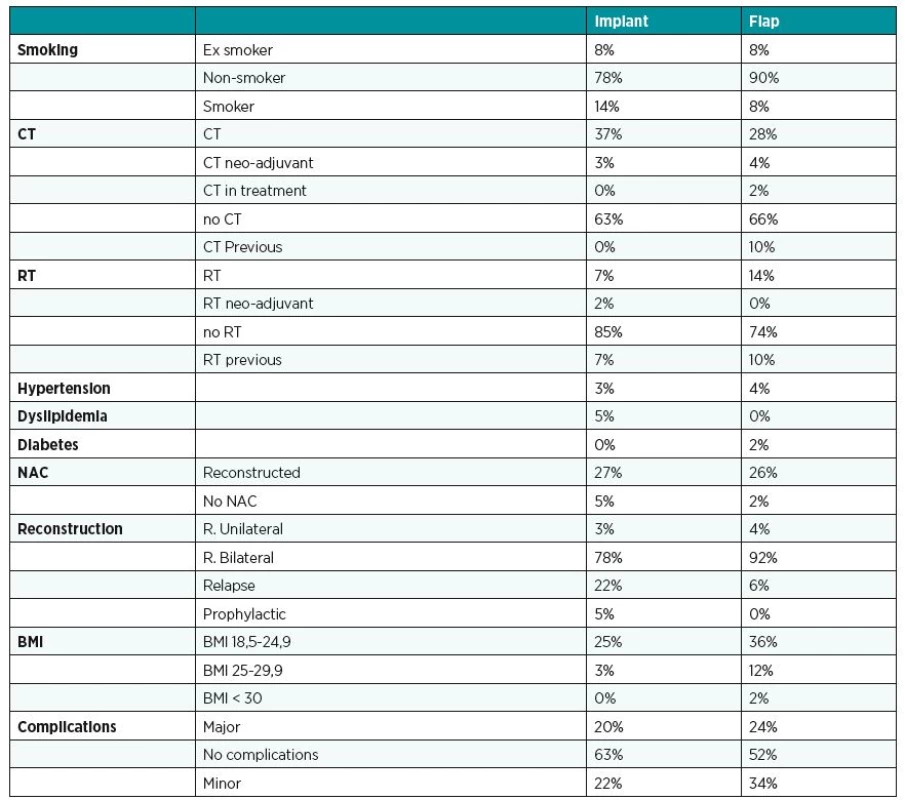
The second phase of the study focused on assessing possible interactions between the reconstructive techniques and previously described variables.
We studied the two groups in relation to the score obtained in the test: satisfied patients (score ³ 60/100) and those not satisfied (<60/100).
Descriptive statistics was used to describe baseline characteristics, for which the women were analysed according to their autologous or implant breast reconstruction.
For each time interval we calculated the mean BREAST-Q score and we used Mann-Whitney U test for statistical analysis. A value of p < 0.05 was used to indicate significance.
RESULTS
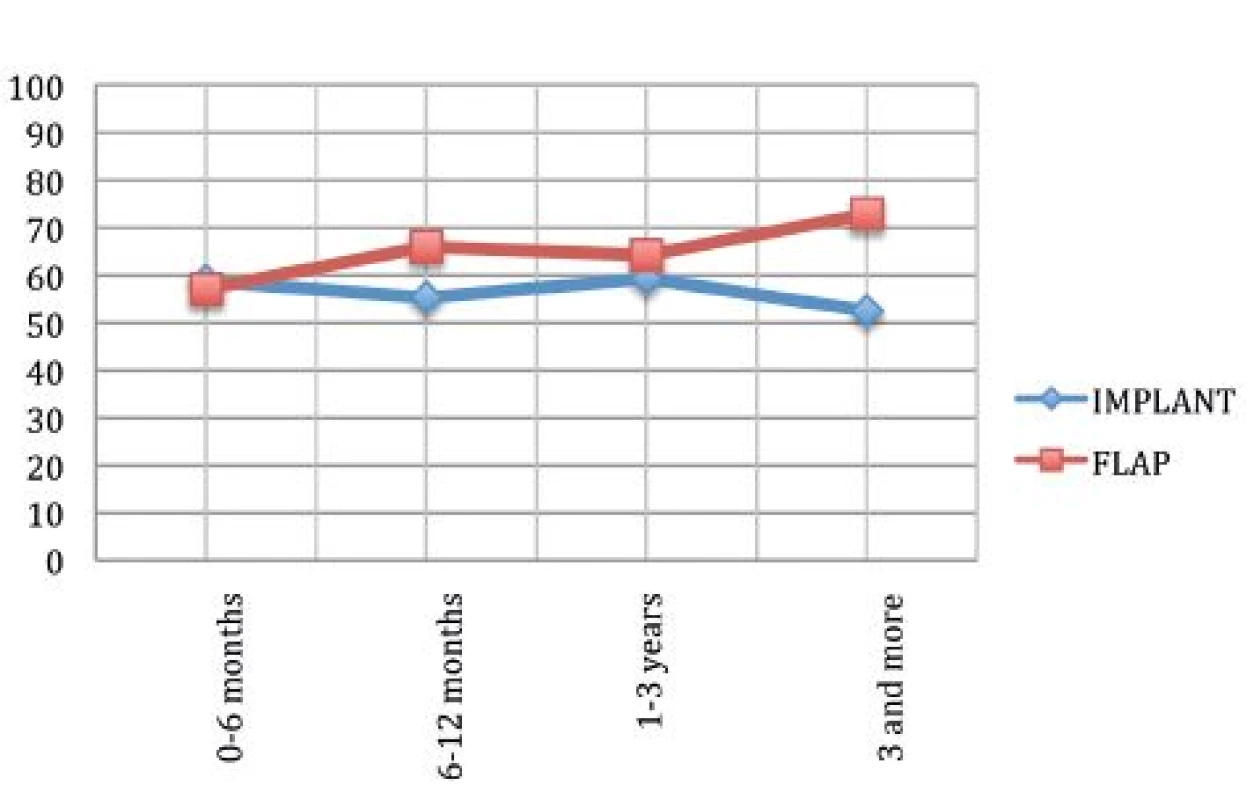
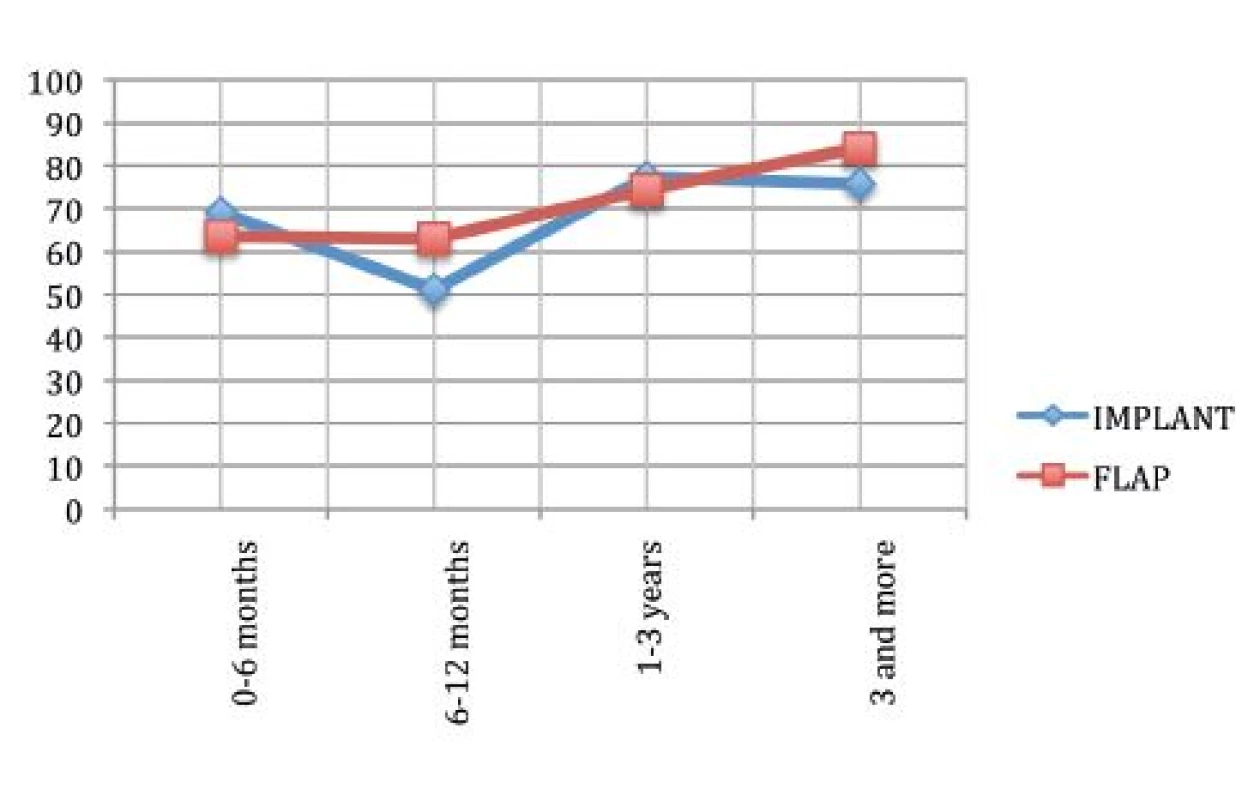
Satisfaction with the reconstructed breast
Fig. 2 shows that the mean satisfaction with breast reconstruction in the first time period was the same but as time passed the satisfaction of the patients treated with autologous tissue improved while the satisfaction with the reconstruction by implants decreased.
We noticed higher values of satisfaction in the time period beyond 3 years with autologous reconstructions, which is in accordance with the fact that the flap requires a longer time to settle completely than the implant. On the other hand, satisfaction with implant based reconstruction in that time period started to decrease, probably because of the onset of implant-related complications such as the capsular contracture.
Statistical analysis confirmed the initial assumptions (p=0.00596).4,18-21
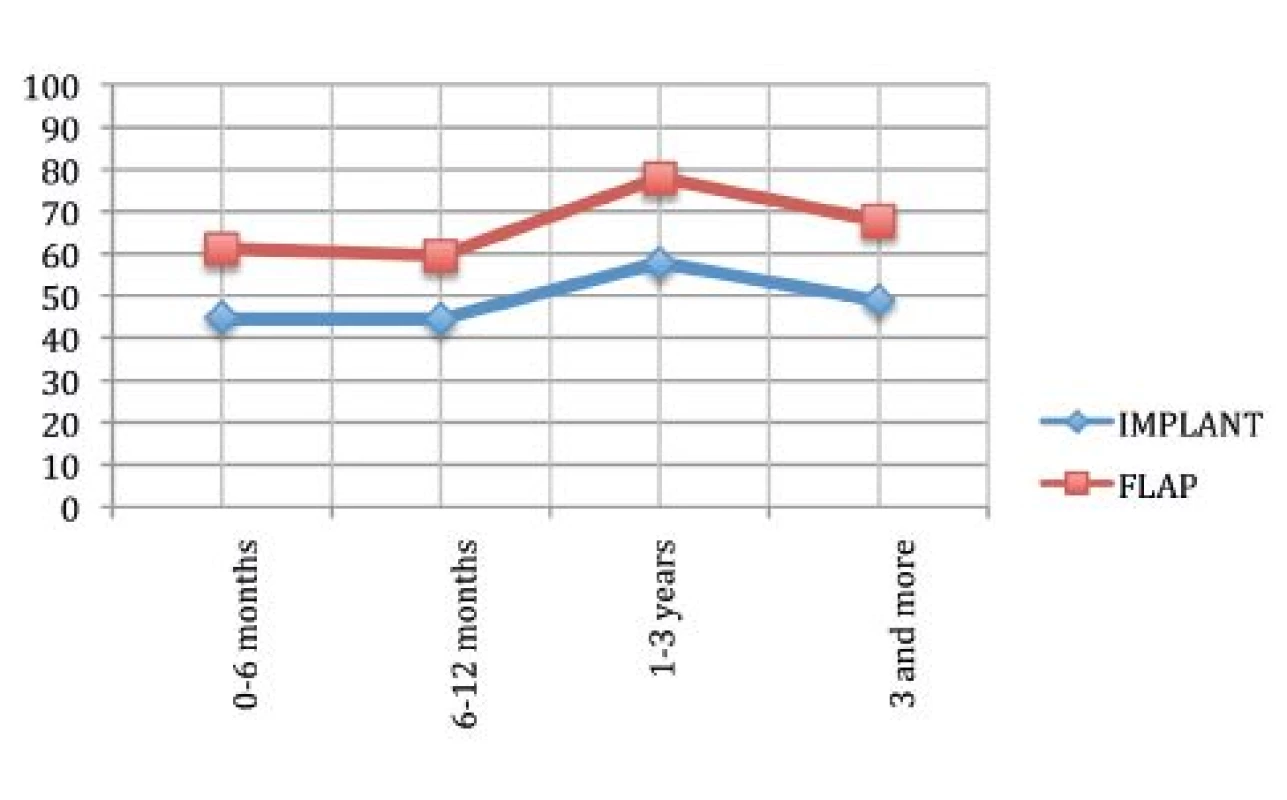
Satisfaction with the outcome
Fig. 3 describes the satisfaction with the outcome. Our data showed no difference between the two mean satisfactions (p=0.58).
This evidence doesn’t confirm the initial assumption of higher satisfaction in patients treated with autologous tissue reconstruction.19
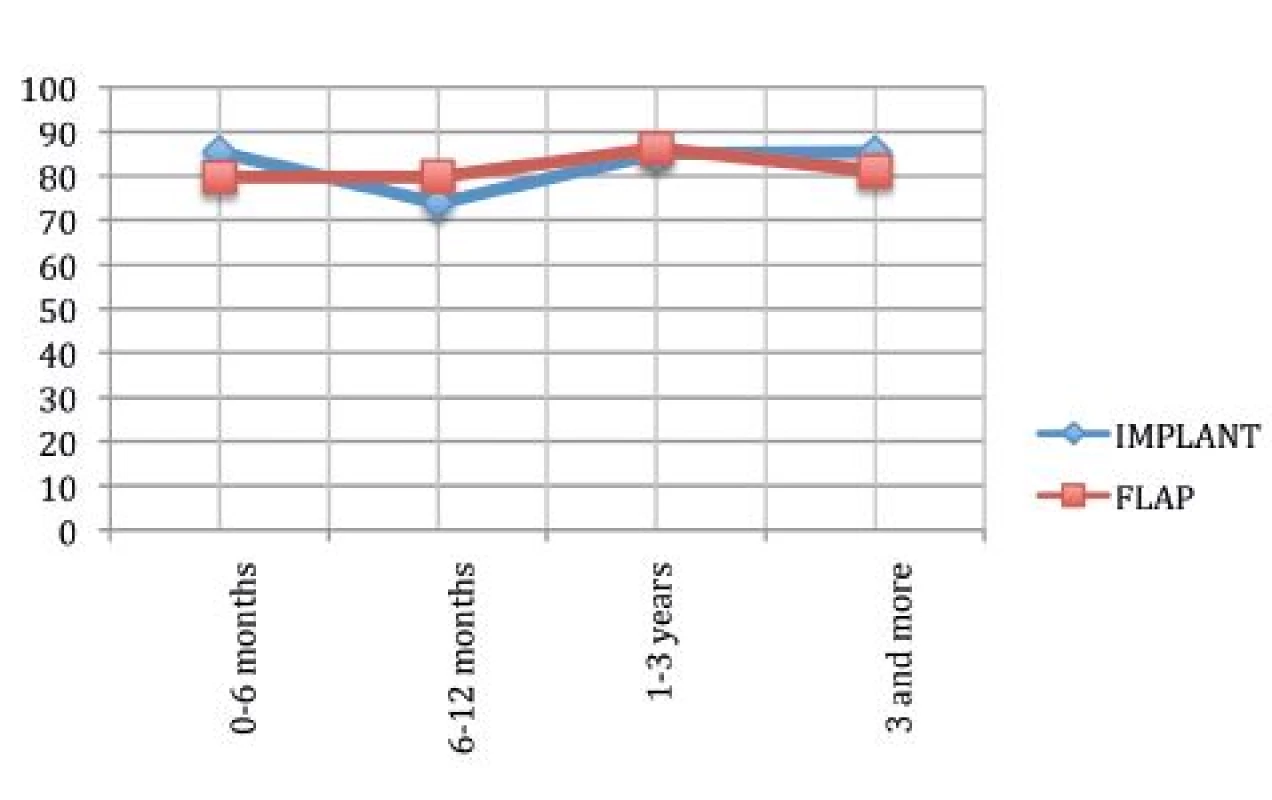
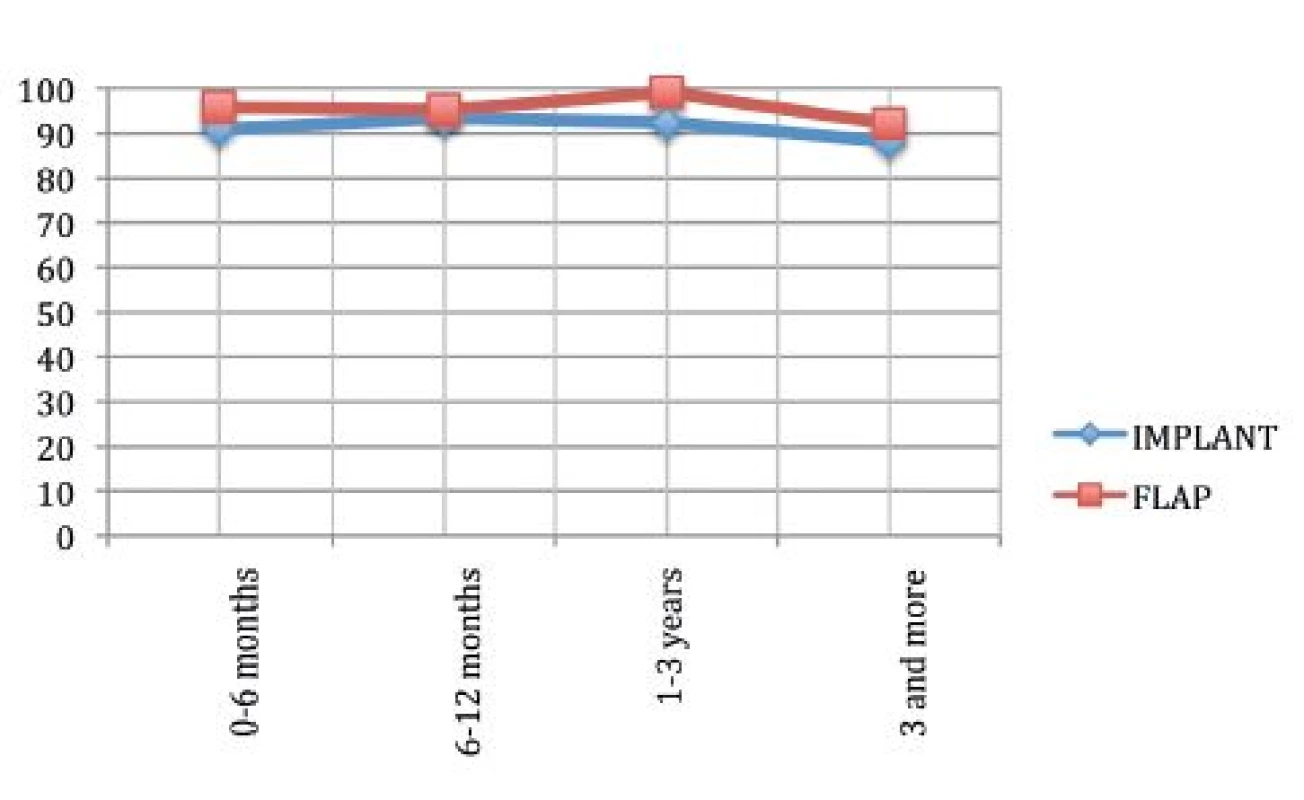
Psycho-social wellbeing
The analysis of psychosocial wellbeing showed that the autologous tissue reconstruction offered higher satisfaction compared to that with implants (p=0.04).
Fig. 4 shows that the mean satisfaction of patients reconstructed with implants was lower compared to the autologous one, but in the last time period both of the curves pointed down. This might be due to the older age of patients in this phase, as described in Tables 1 and 2.
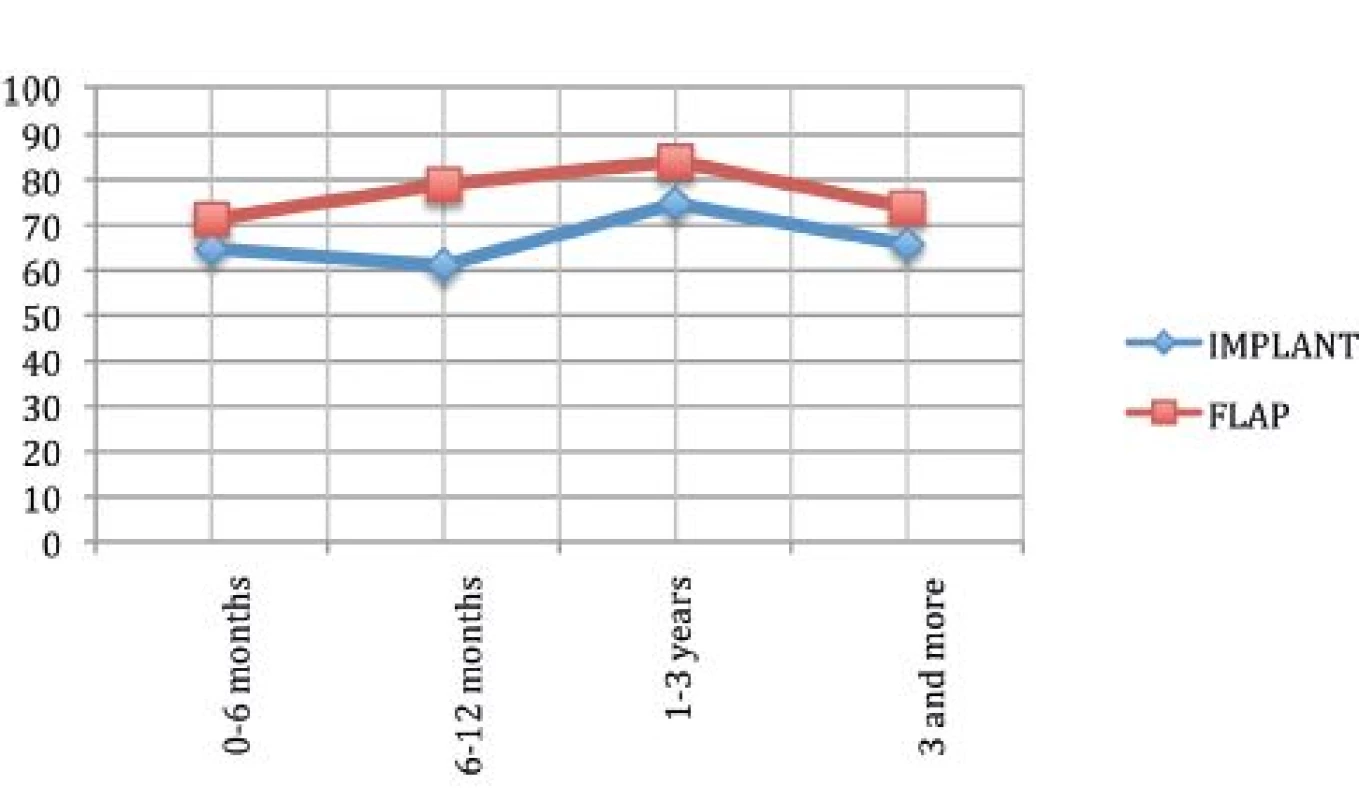
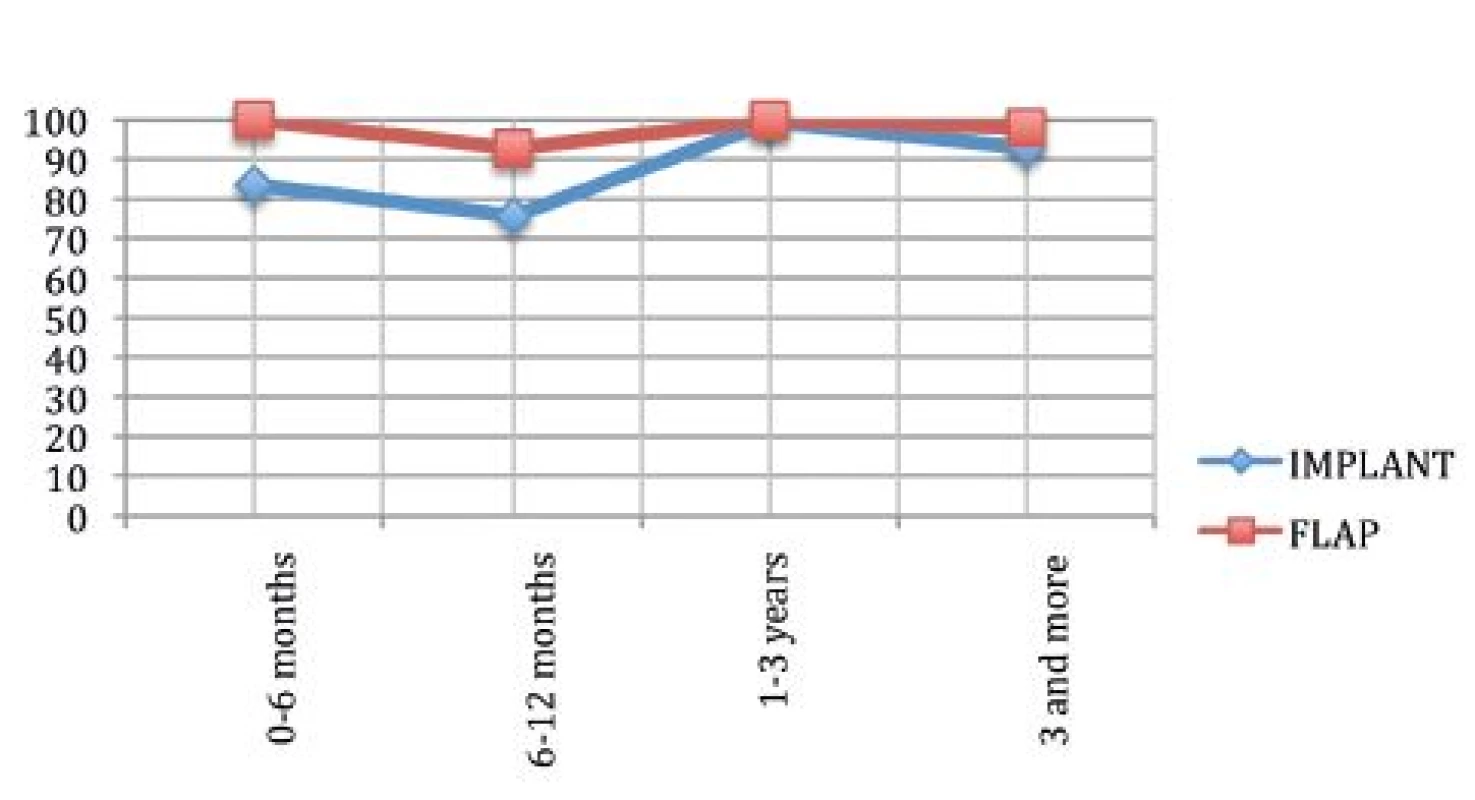
Sexual wellbeing
Fig. 5 describes the sexual well-being. It can be clearly seen that the autologous tissue offers a higher satisfaction than an implant (p=0.00068). We agree with the data in the literature indicating that flaps need a longer time to achieve the maximum degree of satisfaction but, at the end, this is higher than satisfaction with implants.19
It is interesting that in the last time period both techniques show the same trend as in Fig. 4.
We report that 9% of women from both groups decided to tick “not applicable” to confirm that the age can influence sexual wellbeing.
Physical wellbeing: Chest
The analysis noticed no statistical difference between the two techniques (p=0.4413).
Our results do not agree with the data from the literature that quote a higher satisfaction rate for reconstruction with autologous tissue.23
It is important to stress that both techniques show a positive trend. (Fig.6.)
Physical wellbeing: Abdomen
BREAST-Q can analyse the physical wellbeing regarding the abdomen for DIEAP and TRAM flaps. Our patients treated with DIEAP flaps experienced a high satisfaction with their abdomen after surgery with a positive trend with time.
Our data do not agree with literature that quotes a 52% of satisfaction; in our population it is higher. (Fig. 7.)24
7. Physical wellbeing: Abdomen 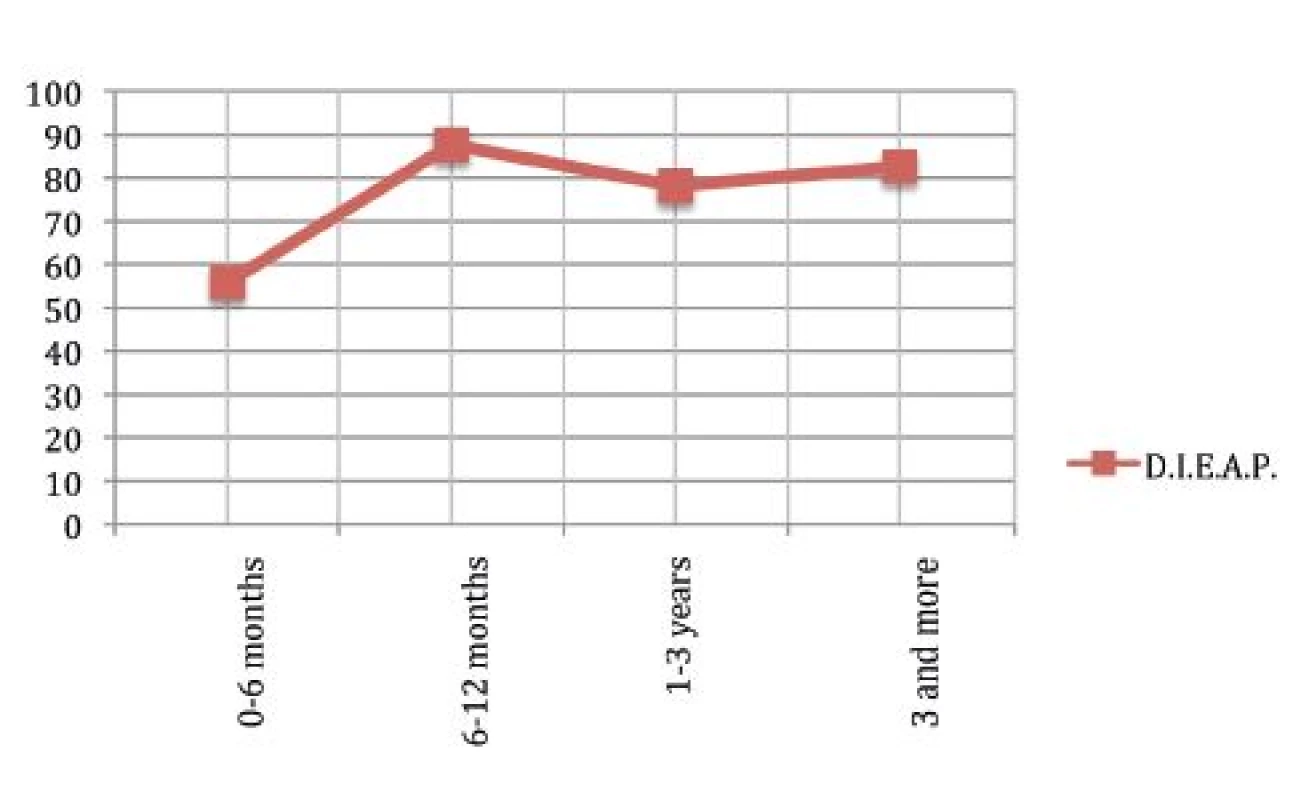
Satisfaction with information, surgeon and staff
The last part of questionnaire analyses the satisfaction with information given to the patient by the surgeon and the staff. The data are shown in Fig. 8, 9 and 10.
8. Satisfaction with Information 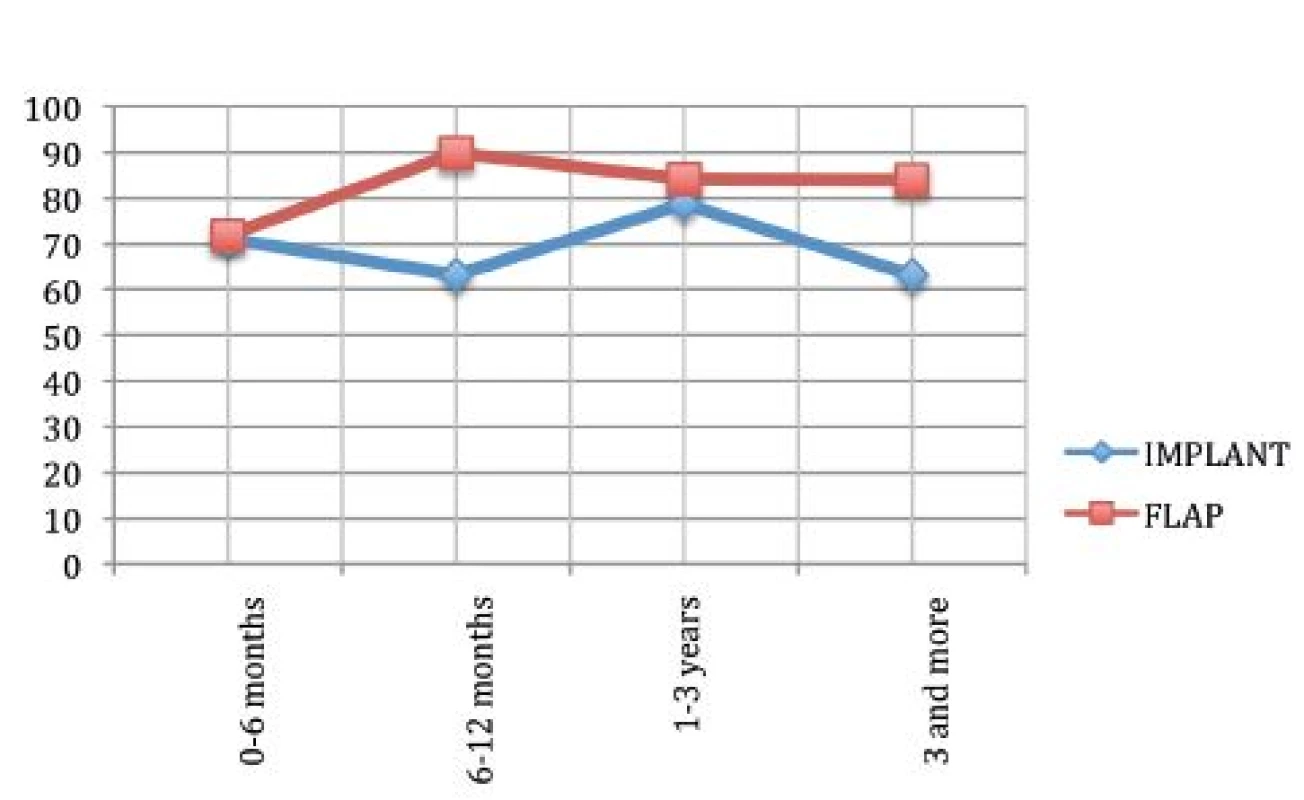
The statistical analysis shows a significant difference between the two groups in satisfaction with information (p=0.0003). There is no significant difference in satisfaction with surgeon (p=1) and staff (p=0.23). In our institute we evidenced a satisfaction level close to 100% in this questionnaire module.
Our data agree with the data from the literature and show how a woman patient satisfied with her relationship with her surgeon will be more satisfied with her reconstructed breast.15,19
Results of the 2nd phase
We studied in detail the data about satisfaction with the reconstructed breast because the first phase of our study showed a statistical difference. Our analysis noticed that in the autologous group 52% of patients were satisfied compared to only 41% in the implant group.
Furthermore we found a higher degree of satisfaction in patients with implants that have not undergone radiotherapy, had a normal BMI and were without complications, as well as in patients with autologous reconstruction if they were non-smokers, or had a bilateral reconstruction.
It is interesting that the patients with unilateral reconstruction were more dissatisfied.
DISCUSSION
The findings of our study are in agreement with the data found in the literature, attributing greater satisfaction with physical, mental and social wellbeing, as well as with elements having repercussion on sexual wellbeing, to autologous breast reconstruction.25-33
We found a significant difference in the quality of life after autologous breast reconstruction and reconstruction by implants.
Our study shows no significant difference between the two techniques concerning satisfaction with outcome, physical wellbeing regarding chest and relationship with the surgeon.
Bresser et al. showed that almost half of the patients treated with implants felt their reconstructed breasts as not being “their-own”.31
This is confirmed by our study that describes how the autologous tissue reconstruction shows a positive trend in satisfaction with breast with time, while breast reconstruction by implants shows a negative trend with time.
This might be due to the fact that the use of implants might need several re-operations or even implant replacement for the capsular contracture.
For this reason, Drazan et al., recommends reconstruction by autologous tissue, specifically the DIEAP flap, because it allows achieving a more stable and lasting satisfaction with time.34
The feeling that the autologous tissue is able to achieve a stable, long-lasting reconstruction, obviously, influences the sexual, physical and psychosocial wellbeing positively.
We agree with the findings in the literature that patients reconstructed by autologous tissue have higher satisfaction rates compared to those with reconstruction by implants but on the other hand the satisfaction with the reconstructed breast is influenced also by the way in which the woman faces the cancer.35
It is true that reconstruction by flaps, especially, if microsurgical, is technically more demanding than the one by implants, but it is also true that this technique allows for a single stage reconstruction, with psychological and aesthetic benefits.33,36
These features probably affect the satisfaction, especially shortly after reconstruction.
In the module “satisfaction with outcome” BREAST-Q evaluates if the patient has repented of her choice and how the reconstruction had changed her life.
We want to stress that in both groups women didn’t change their mind and they were still happy with the outcome.
Ho et al. showed the importance of communications and the relationship with patients for achieving high satisfaction rates.16
In our institute we noticed a satisfaction rate close to 100%.
The literature reports a lot of variables that could be associated with satisfaction, so we analysed them in the second phase of our study.37
The data suggests a significant difference between the satisfied patients and those who are not satisfied.
This evidence could be a starting point for other studies to analyse the relationship between the variables and the satisfaction (Table 4).
4. Distribution of smoking, CT (chemotherapy), RT (radiotherapy), hypertension, dyslipidemia, diabetes, NAC (nipple areola complex), reconstruction, BMI (body mass index), complications for each groups divided in satisfied and not satisfied 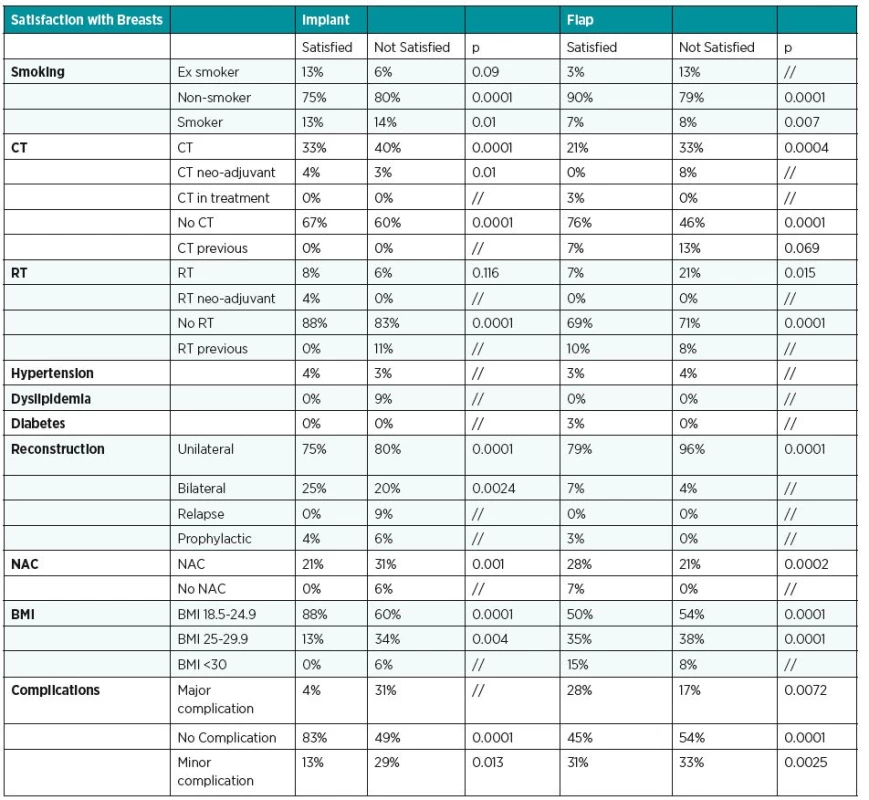
We found that there were more satisfied women in the implant group if they hadn’t had complications, if they had a bilateral reconstruction, if they had no radiotherapy and if they had a normal BMI.
If we analysed patients reconstructed by autologous tissue and with a BMI > 30, we were able to notice that there were more satisfied patients than unsatisfied patients in this group.
Smoking can be a risk factor for satisfaction; in fact non-smokers are more satisfied than smokers.
Our data show that autologous tissue breast reconstruction needed more secondary corrections compared with reconstructions with implants (32% vs. 16%).4
We noticed more complications in patients treated with radiotherapy versus patients not treated, also in patients with autologous tissue reconstructions.
No significant difference was seen between the two groups for the middle age women.
As described in the literature, immediate breast reconstruction is preferred when possible.36
In our unit all patients treated by autologous reconstruction had immediate reconstruction, while only 8 women treated with implant had an immediate reconstruction, the other had a two-stage tissue expander-to-implant reconstruction.
We excluded women with implant or flap failure.
This might be considered a drawback, but we agree with data from the literature that their quality of life represents features of a different process compared with patients after a successful breast reconstruction.4 We did not distinguish between unilateral and bilateral breast reconstruction within the breast reconstruction groups.
Most likely, our cohort of patients entering the study was too small for significant results to be detected, so we consider this study a pilot study in preparation for conducting a larger, prospective study.
CONCLUSIONS
Women after a successful breast reconstruction are generally satisfied and have a good quality of life. This study investigated which surgical technique was associated with better outcomes according to the patients. We confirm that autologous breast reconstruction allows achieving a higher degree of satisfaction than implant breast reconstruction. We found no difference in the quality of life between the autologous and implant techniques.
The conclusions of this study may be interesting for professionals dealing with breast reconstruction. This may helps patients and surgeons in making informed decisions for breast reconstruction. To strengthen the evidence regarding satisfaction with the entire breast procedure, it is necessary to perform prospective studies with larger and more homogeneous groups.
Corresponding author:
Prof. Zoran M. Arnež, M.D., PhD.
Cattinara Hospital, Strada di Fiume, 447
34149, Trieste, Italy
E-mail: zoran.arnez@asuits.sanita.fvg.it
Sources
1. Dean NR, Yip JM, Birrell S. Rotation flap approach mastectomy. ANZ J Surg. 2013 Mar;83(3):139-45.
2. Eltahir Y, Werners LL, Dreise MM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. 2013 Aug;132(2):201e-209e.
3. Cano SJ, Klassen A, Pusic AL. The science behind quality-of-life measurement: a primer for plastic surgeons. Plast Reconstr Surg. 2009 Mar;123(3):98e-106e.
4. Eltahir Y, Werners LL, Dreise MM, Zeijlmans van Emmichoven IA, Werker PM, de Bock GH. Which breast is the best? Successful autologous or alloplastic breast reconstruction: patient-reported quality-of-life outcomes. Plast Reconstr Surg. 2015 Jan;135(1):43-50.
5. Quinn TT, Miller GS, Rostek M, Cabalag MS, Rozen WM, Hunter-Smith DJ. Prosthetic breast reconstruction: indications and update. Gland Surg. 2016 Apr;5(2):174-86.
6. Damen TH, Timman R, Kunst EH, et al. A. High satisfaction rates in women after DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2010 Jan;63(1):93-100.
7. Fischer JP, Nelson JA, Cleveland E, Sieber B, Rohrbach JI, Serletti JM, Kanchwala S. Breast reconstruction modality outcome study: a comparison of expander/implants and free flaps in select patients. Plast Reconstr Surg. 2013 May;131(5):928-34.
8. Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O’Reilly D, Goeree R. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg. 2014 Feb;133(2):234-49.
9. Bailey MH, Smith JW, Casas L, et al. Immediate breast reconstruction: reducing the risks. Plast Reconstr Surg. 1989 May;83(5):845-51.
10. Cowen D, Gross E, Rouannet P, et al. Immediate post-mastectomy breast reconstruction followed by radiotherapy: risk factors for complications. Breast Cancer Res Treat. 2010 Jun;121(3):627-34.
11. Ohkuma R, Lacayo B, Rad AN, et al. Health related quality of life after breast reconstructive surgery: An interim analysis. Plast Reconstr Surg. 2013 May;131(5S):84.
12. Macadam SA, Ho AL, Cook EF Jr, Lennox PA, Pusic AL. Patient satisfaction and health-related quality of life following breast reconstruction: patient-reported outcomes among saline and silicone implant recipients. Plast Reconstr Surg. 2010 Mar;125(3):761-71.
13. McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants. Cancer. 2010 Dec 15;116(24):5584-91.
14. Reaby LL. Reasons why women who have mastectomy decide to have or not to have breast reconstruction. Plast Reconstr Surg. 1998 Jun;101(7):1810-8.
15. Ng SK, Hare RM, Kuang RJ, Smith KM, Brown BJ, Hunter-Smith DJ. Breast Reconstruction Post Mastectomy: Patient Satisfaction and Decision Making. Ann Plast Surg. 2016 Jun;76(6):640-4.
16. Ho AL, Klassen AF, Cano S, Scott AM, Pusic AL. Optimizing patient-centered care in breast reconstruction: the importance of preoperative information and patient-physician communication. Plast Reconstr Surg. 2013 Aug;132(2):212e-220e.
17. Pusic AL, Chen CM, Cano S, et al. Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg. 2007 Sep 15;120(4):823-37; discussion 838-9.
18. Atisha DM, Rushing CN, Samsa GP, et al. A national snapshot of satisfaction with breast cancer procedures. Ann Surg Oncol. 2015 Feb;22(2):361-9.
19. Liu C, Zhuang Y, Momeni A, Luan J, Chung MT, Wright E, Lee GK. Quality of life and patient satisfaction after microsurgical abdominal flap versus staged expander/implant breast reconstruction: a critical study of unilateral immediate breast reconstruction using patient-reported outcomes instrument BREAST-Q. Breast Cancer Res Treat. 2014 Jul;146(1):117-26.
20. Clough KB, O’Donoghue JM, Fitoussi AD, Nos C, Falcou MC. Prospective evaluation of late cosmetic results following breast reconstruction: I. Implant reconstruction. Plast Reconstr Surg. 2001 Jun;107(7):1702-9.
21. Clough KB, O’Donoghue JM, Fitoussi AD, Vlastos G, Falcou MC. Prospective evaluation of late cosmetic results following breast reconstruction: II. Tram flap reconstruction. Plast Reconstr Surg. 2001 Jun;107(7):1710-6.
22. Peled AW, Duralde E, Foster RD, et al. Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction. Ann Plast Surg. 2014 May;72 Suppl 1:S48-52.
23. McCarthy CM, Mehrara BJ, Long T, et al. Chest and upper body morbidity following immediate postmastectomy breast reconstruction. Ann Surg Oncol. 2014 Jan;21(1):107-12.
24. Niddam J, Bosc R, Lange F, et al. DIEP flap for breast reconstruction: retrospective evaluation of patient satisfaction on abdominal results. J Plast Reconstr Aesthet Surg. 2014 Jun;67(6):789-96.
25. Quinn TT, Miller GS, Rostek M, Cabalag MS, Rozen WM, Hunter-Smith DJ. Prosthetic breast reconstruction: indications and update. Gland Surg. 2016 Apr;5(2):174-86.
26. Cano SJ, Klassen A, Pusic AL. The science behind quality-of-life measurement: a primer for plastic surgeons. Plast Reconstr Surg. 2009 Mar;123(3):98e-106e.
27. Cohen WA, Mundy LR, Ballard TN, et al. The BREAST-Q in surgical research: A review of the literature 2009-2015. J Plast Reconstr Aesthet Surg. 2016 Feb;69(2):149-62.
28. Jeevan R, Cromwell DA, Browne JP, et al. Findings of a national comparative audit of mastectomy and breast reconstruction surgery in England. J Plast Reconstr Aesthet Surg. 2014 Oct;67(10):1333-44.
29. Eltahir Y, Werners LL, Dreise MM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. 2013 Aug;132(2):201e-209e.
30. Alderman AK, Wilkins EG, Lowery JC, Kim M, Davis JA. Determinants of patient satisfaction in postmastectomy breast reconstruction. Plast Reconstr Surg. 2000 Sep;106(4):769-76.
31. Bresser PJ, Seynaeve C, Van Gool AR, et al. Satisfaction with prophylactic mastectomy and breast reconstruction in genetically predisposed women. Plast Reconstr Surg. 2006 May;117(6):1675-82; discussion 1683-4.
32. Mlodinow AS, Ver Halen JP, Lim S, Nguyen KT, Gaido JA, Kim JY. Predictors of readmission after breast reconstruction: a multi-institutional analysis of 5012 patients. Ann Plast Surg. 2013 Oct;71(4):335-41.
33. Fischer JP, Nelson JA, Cleveland E, et al. Breast reconstruction modality outcome study: A comparison of expander/implants and free flaps in select patients. Plast Reconstr Surg. 2013 May;131(5):928–34.
34. Drazan L, Vesely J, Hyza P, et al. Bilateral breast reconstruction with DIEP flaps: 4 years’ experience. J Plast Reconstr Aesthet Surg. 2008 Nov;61(11):1309-15.
35. Boughton B. Emotional outcome after breast surgery is highly individual. J Natl Cancer Inst. 2000 Sep 6;92(17):1375-6.
36. Serletti JM, Fosnot J, Nelson JA, Disa JJ, Bucky LP. Breast reconstruction after breast cancer. Plast Reconstr Surg. 2011 Jun;127(6):124e-35e.
37. Hershman DL, Richards CA, Kalinsky K, et al. Influence of health insurance, hospital factors and physician volume on receipt of immediate post-mastectomy reconstruction in women with invasive and non-invasive breast cancer. Breast Cancer Res Treat. 2012 Nov;136(2):535-45.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2017 Issue 3-4-
All articles in this issue
- Editorial
- PATIENT SATISFACTION AFTER BREAST RECONSTRUCTION: IMPLANTS VS. AUTOLOGOUS TISSUES
- OLEOGEL-S10 TO ACCELERATE HEALING OF DONOR SITES: MONOCENTRIC RESULTS OF PHASE III CLINICAL TRIAL
- THE NASOLABIAL FLAP: THE MOST VERSATILE METHOD IN FACIAL RECONSTRUCTION
- CURRENT TREATMENT OPTIONS OF DUPUYTREN´S DISEASE
- SURGICAL TREATMENT OF MELANOMA
- POSTOPERATIVE FIXATION AFTER REPOSITIONING OF PREMAXILLA IN A PATIENT WITH BILATERAL CLEFT LIP AND PALATE – CASE REPORT
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- THE NASOLABIAL FLAP: THE MOST VERSATILE METHOD IN FACIAL RECONSTRUCTION
- CURRENT TREATMENT OPTIONS OF DUPUYTREN´S DISEASE
- PATIENT SATISFACTION AFTER BREAST RECONSTRUCTION: IMPLANTS VS. AUTOLOGOUS TISSUES
- OLEOGEL-S10 TO ACCELERATE HEALING OF DONOR SITES: MONOCENTRIC RESULTS OF PHASE III CLINICAL TRIAL
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career