-
Medical journals
- Career
Ophthalmological finding in a patient with lowe syndrome
Authors: D. Tomčíková 1; A. Gerinec 1; V. Bzdúch 2; V. Krásnik 3; B. Bušányová 1; K. Brennerová 2
Authors‘ workplace: Klinika detskej oftalmológie DFNsP LFUK Bratislava, Limbová 1, 83340 Bratislava., Prednosta: MUDr. Dana Tomčíková, PhD, MHA. 1; Detská klinika DFNsP LFUK Bratislava, Limbová 1, 83340 Bratislava., Prednosta: prof. MUDr. Ľudmila Podracká, CSc. 2; Klinika oftalmológie UNB a LFUK Bratislava, Ružinovská 6, 82606 Bratislava., Prednosta: doc. MUDr. Vladimír Krásnik, PhD. 3
Published in: Čes. a slov. Oftal., 74, 2018, No. 3, p. 104-106
Category: Case Report
doi: https://doi.org/10.31348/2018/1/4-3-2018Overview
The authors present the ophthamological finding in a patient who at the age of 4.5 months was admitted due to a finding of total bilateral congenital cataract. The patient was observed by a neurologist for central hypotonia and mental retardation. Upon a complex examination of the patient, suspicion of Lowe syndrome was stated, which was confirmed by a metabolic examination and also by genetic tests. Upon an examination of the family, a genetic defect (mutation of OCRL1 gene) was confirmed also in the mother of the patient. A mild subcapsular opacification was present in the mother, beneath the posterior capsule. The patient was operated on for bilateral congenital cataract. Upon an examination under general anaesthesia, trabeculodysgenesis was diagnosed. Intraocular pressure remains within the norm. The patient is now aged 8 years, regularly monitored with regard to metabolic compensation, and by a neurologist and ophthalmologist, with satisfactory visual functions. Early diagnosis of the Lowe syndrome was determined on the basis of a complex examination of the patient within the framework of etiological diagnosis of bilateral congenital cataract.
Key words:
Lowe syndrome, oculo – cerebro – renal syndrome, congenital cataract, glaucoma, nystagmus.Introduction
Lowe syndrome (oculocerebrorenal syndrome, with a prevalence of 1 : 500 000 of the population) is a hereditary disorder linked to the X chromosome, which thus affects virtually exclusively males, while females are the carriers of the disorder. The pathology primarily afflicts the eyes (congenital cataract, glaucoma), brain (pyschomotor retardation, hypotonia) and kidneys (Fanconi syndrome). The syndrome was first described by Lowe in 1952 (3). Of the general symptoms, characteristic are retardation of growth, pale skin, mental retardation, areflexia, hypotonia, convulsions, non-inflammatory swelling of the joints and especially generalised dysfunction of the proximal tubule, which leads to excessive discharge of water, bicarbonates, glucose and amino acids, which is manifested in polyuria and leads to polydipsia. Metabolic breakdown linked with kidney failure is generally fatal, often in the 2nd decade of life (6). Various ocular symptoms, especially congenital, infantile cataract and glaucoma occur within the framework of several metabolic, hereditary and systemic pathologies. They are frequently the first symptoms which cause the patient to consult a doctor. As a result it is important to pay attention to the etiological diagnosis of the pathology. Upon bilateral congenital and infantile cataract it is necessary to focus on metabolic examination, which may reveal a metabolic defect, etiologically conditioning the occurrence of cataract. Its compensation may prevent irreparable damage to the organism and ensure better quality of life.
Method
Within the framework of the opthalmological examination the following were examined: central visual acuity (CVA), intraocular pressure, local finding on the anterior segment, optical media and ocular fundus. Central visual acuity of the proband was examined with the aid of preverbal Cardiff acuity cards, in the mother with the aid of Snellen eye charts. For examination of the lens we used a slit lamp Zeiss SLO 10, for the proband under the age of 3 years a manual slit lamp. The examination was conducted in artificial mydriasis. For photo-documentation we used a photographic slit lamp CSO SL 9900. Gonioscopy was examined under general anaesthesia with the aid of a three-sided Goldmann lens. The finding on the ocular fundus of the proband and his mother was examined by indirect ophthalmoscope, also in artificial mydriasis. In addition to the ophthalmological examination, a biochemical examination and genetic examination were conducted.
Results
The 4.5-month-old infant was sent to the Department of Paediatric Ophthalmology at the Paediatric Clinic of the Faculty of Medicine, Comenius University in Bratislava, with a finding of bilateral congenital cataract. From the age of 1 month the child had been monitored by a neurologist for psychomotor retardation and hypotonia. At the same time an adverse reaction to visual stimuli was determined. The family anamnesis was negative. Upon examination at our clinic, metabolic screening was conducted within the framework of etiological diagnosis of congenital cataracts. Upon a urine examination, increased aminoaciduria, increased excretion of oligosaccharides and increased excretion of metabolites of the Krebs cycle were determined. Suspicion of Lowe syndrome was stated, and was subsequently confirmed also by a genetic test. Mutation of the OCRL 1 (c.2083C >T(Arg695Ter)) gene in a hemizygote state was determined in both the patient and his mother, who was thereby confirmed as a carrier of the pathological gene. Typical cortical opacities of the lens were not determined in the mother. Only mild opacification was present beneath the posterior capsule. Congenital cataracts in the patient were successfully operated on at the age of 5 and 6 months. The later date of the operation was due to the late sending of the patient for surgery, and at the same time infection of the upper respiratory tracts, as a result of which general anaesthesia had to be deferred. The patient is being regularly monitored. At the last examination at the age of 8 years, CVA of the patient was 6/18 Cardiff with aphakic correction (fig. 1). We did not record increased intraocular pressure, despite a finding of trabeculodysgenesis. With regard to the high risk of occurrence of glaucoma, intraocular lenses were not implanted in the patient. The local finding is satisfactory. In the mother of the patient, who is a carrier of the pathological mutation, no typical cortical opacities were determined, either at the time of diagnosis of the disorder in the proband or after 8 years. Only mild opacification beneath the posterior capsule was present (fig. 2).
1. Aphakic left eye of proband at the age of 8 years. 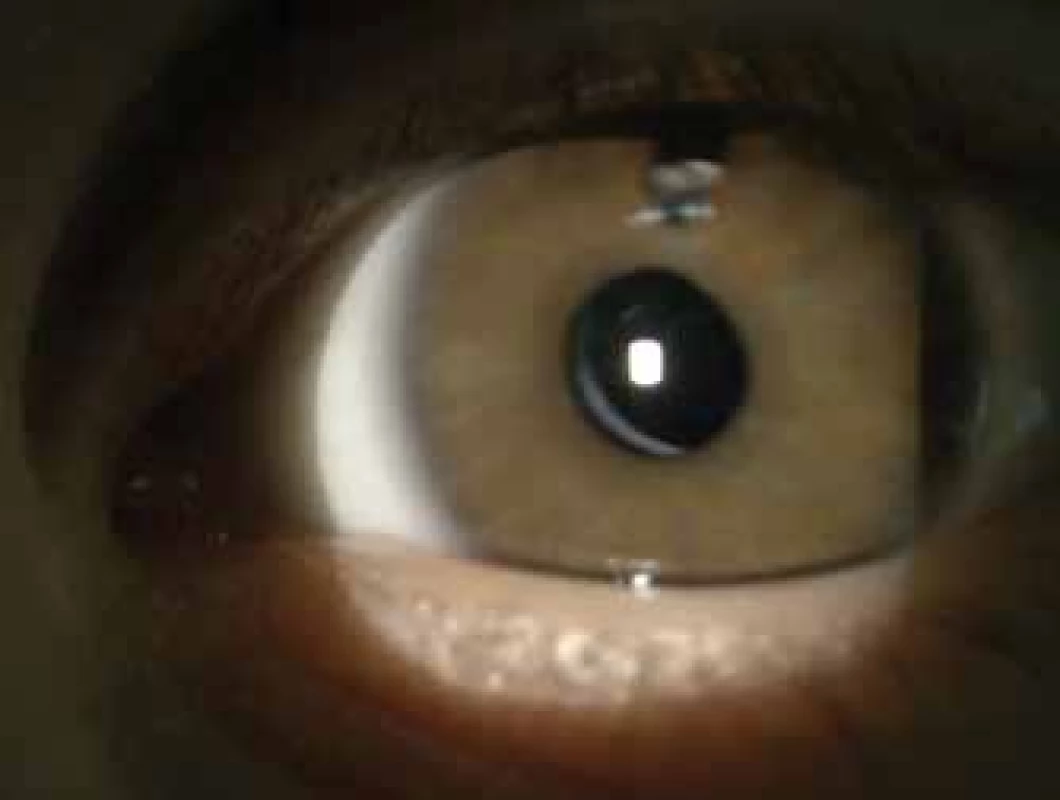
2. Lens of mother of proband without finding of typical cortical opacities, only with mild opacification beneath the posterior capsule. 
Discussion
The primary finding within the framework of the ocular pathology of Lowe syndrome is cataract. Congenital total bilateral cataract is typical in a patient with Lowe syndrome (3, 2). For carriers of the pathological mutation of the ORCL 1 gene, typical manifestations are spotted whitish or greyish-white opacities in the lenses, localised in all levels of the cortex, with a predilection in the anterior cortex in the region of the equator, which points to their origin in adult life. They are not localised in the nucleus. Sometimes opacity may be present beneath the posterior cortex centrally (4, 5). The size of the opacities may be from microns to several millimetres. The occurrence of more than 25 cortical opacities in 1 quadrant of the lens in the second decade of life is pathognomonic for the carriers of this disease (2). Some authors state a 93 to 100% incidence of lenticular opacities in carriers (2, 4). Despite the fact that at the time of diagnosis of the syndrome the mother of the proband was aged 25 years, we did not record the occurrence of typical lenticular opacities in her. Upon an examination of the mother at the age of 33 years, the finding was again negative with regard to the occurrence of cortical lenticular opacities. Only mild opacification beneath the posterior capsule was present. This finding runs contrary to the assertion (2) that the presence of cortical lenticular opacities is so pathognomonic that their diagnosis has been proposed as a screening method for the diagnosis of carriers of the Lowe syndrome. The presence of the mutation of the ORCL 1 gene also in the mother however excludes any doubts that she is a carrier of the disease. On the basis of microscopic morphological studies, characteristic lenticular opacities in the Lowe syndrome are conditioned by a genetic defect of the lens cells. The defect is manifested during early embryogenesis and leads to the malformation and subsequent degeneration of the primary posterior lens lobes, which leads to the formation of a flat, discoid or ringed cataract. Anterior polar cataract, posterior lenticonus and subcapsular plaque are not typical of Lowe syndrome (5). In the patient there was a finding of typical bilateral total cataracts, as a result of which extracapsular extraction of the lens was performed at the age of 5 and 6 months. We did not implant intraocular lenses due to the increased risk of glaucoma with difficult compensation (1). Correction with contact lenses is similarly not recommended due to the risk of the formation of keloid scars of the cornea (4). Severe glaucoma, conditioned by goniodysgenesis, which requires surgical solution, occurs in as many as 50% of cases (4). In our patient intraocular pressure so far remains within the physiological range. Best corrected visual acuity is rarely better than 0.2, which was confirmed also in our patient. The worse functional result was caused, in addition to damage to the central nervous system, also due to the late cataract operation with concurrent incidence of nystagmus. The patient is in generally good condition, which is due to the timely diagnosis and endeavour to achieve the most optimal compensation of the metabolic defect in the patient.
Conclusion
Within the framework of etiological diagnostics, we diagnosed Lowe syndrome in an infant with bilateral congenital cataracts. Ocular symptoms occur within the framework of many metabolic, hereditary and systemic pathologies. They are frequently the initial symptoms of the disorder. As a result it is important to pay attention to the etiological diagnosis of the pathology. Upon bilateral congenital or infantile cataract it is necessary to focus on metabolic examination, which may reveal a metabolic defect, etiologically conditioning the occurrence of cataract. Its compensation may prevent irreparable damage to the organism and ensure better quality of life. In the mother of the patient, despite genetically confirmed mutation of the ORCL 1 gene we did not determine opacities of the lens which are characteristic of carriers of the disease.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Dana Tomčíková, PhD, MHA
Klinika detskej oftalmológie NÚDCH - LFUK Limbová 1, 83340 Bratislava
Sources
- Bökenkamp, A., Ludwig, M.: The oculocerebrorenal syndrome of Lowe: an update. Pediatr Nephrol., (12); 2016 : 2201-2212.
- Cibis, G.W., Waeltermann, J. M., Whitcraft, Ch. T.: Lenticular opacities in Carriers of Lowe´s Syndrome. Ophthalmology, (8); 1986 : 1041-5.
- Curtin, V.C., Joyce, E.E., Ballin, N.: Ocular Pathology in the Oculo-Cerebro-Renal Syndrome of Lowe. AJO, (64): 533/15–543/25.
- Lin,T., Lewis, R.A., Nussbaum, R.L.: Molecular confirmation of carriers for Lowe syndrome. Ophthalmology, (106); 1999 : 119–122.
- Tripathi, R.C., Cibis, G.W., Tripathi, B.J.: Pathogenesis of Cataracts in Patients with Lowe’s Syndrome. Ophthalmology, (93); 1986 : 1046-51.
- Wright, K.W., Spiengel, P. H.: Pediatric Ophthalmology and Strabismus, Springer, New York 2003, p.1021-1058.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 3-
All articles in this issue
- Ophthalmological finding in a patient with lowe syndrome
- Marshall and stickler syndrome in one family
- Congenital central toxoplasmic chorioretinitis - case study
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Conjuctival lesions - the relationship of papillomas and squamous cell carcinoma to HPV infection
- Ophthalmic manifestations of acute leukaemias
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ophthalmic manifestations of acute leukaemias
- Asphercial iols and their effect on visual, depth of field, spherical aberration and contrast sensitivity
- Congenital central toxoplasmic chorioretinitis - case study
- Marshall and stickler syndrome in one family
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

