-
Medical journals
- Career
Propofol vs. sevoflurane as anaesthetic maintenance agents in patients undergoing brain aneurysm coiling – randomized prospective study
Authors: Ahmed S. El Akkad 1; Saniova Beata 2; Bakalar Bohumil 1; Adamicova Katarina 3; Husni Al Khalili 4
Authors‘ workplace: Department of Anaesthesia and Intensive care, Doncaster and Bassetlaw Hospitals NHS Foundation Trust, United Kingdom 1; Department of Anaesthesia and Intensive Care, Jessenius Medical Faculty Comenius University and University Medical Hospital in Martin, Slovakia 2; Department of Pathological Anatomy, Jessenius Medical Faculty Comenius University and University Medical Hospital in Martin, Slovakia 3; Department of Community Paediatric, Victoria Hospital, Glasgow, United Kingdom 4
Published in: Anest. intenziv. Med., 23, 2012, č. 1, s. 28-32
Category: Anaesthesiology - Original Paper
Overview
Background:
Sevoflurane and propofol are commonly used anaesthetic agents for general anaesthesia. It has not been established which of them is more suitable for maintaining general anaesthesia during brain aneurysm treatment with endovascular coiling.Objective:
We studied an effect of two anaesthetic maintenance agents on perioperative hemodynamic stability and the rate of complications in patients undergoing brain aneurysm coiling.Design:
Prospective randomised trial.Setting:
The tertiary level university hospital.Patients:
110 patients with brain aneurysms treated by endovascular coiling under general anaesthesia.Interventions:
Patients were randomised into 2 groups. The first group (S, 55 patients) received sevoflurane, the second group (P, 55 patients) received propofol infusion to maintain general anaesthesia. Induction into anaesthetic was the same in both groups.Measurements and Main Results:
Group S patients were significantly more hemodynamically stable in the term of mean arterial pressure (p = 0.001). Recovery time was shorter in S group. Perioperative bradycardia occurred in the Group P more often (P = 0.039) meanwhile hypertension was more frequent in the Group S (P = 0.001).Conclusions:
Our results suggest that sevoflurane can be better choice than propofol infusion for patients with brain aneurysms treated by endovascular coiling under general anaesthesia.Key words:
brain aneurysm – coiling – general anaesthesia – sevoflurane – propofolIntroduction
A brain aneurysm, also called a cerebral or intracranial aneurysm, is enlargement, distension, dilation or bulging of the wall of a cerebral artery. It is estimated that up to one in 15 people will develop brain aneurysm during their lifetime [1]. Brain aneurysms are often discovered when they rupture, causing bleeding into the brain tissue or into the subarachnoid space. Aneurysms that rupture can result in brain damage, severe disability or death.
Brain aneurysms occur in all age groups, but aneurysm sufferers are rarely young. Incidence of aneurysm is low in those under 20 years of age. In contrast, aneurysms are relatively common in people over 65 years of age. Women are more likely to get brain aneurysm than men, with a ratio of 3 : 2 [2].
In the past, brain aneurysms were treated mainly by surgical clipping via craniotomy. Now, due to rapid advances in diagnostic and interventional radiology and neuroradiology in last two decades [3], most of intracranial vascular pathologies can be successfully managed with endovascular approach, thus either avoiding surgical intervention or making it safer for the patient [4].
The use of endovascular techniques, especially Guglielmi detachable coils, represents a major technological advance in aneurysm treatment, though they are not suitable for treatment of all aneurysms. Coiling is now firmly established as a treatment option for management of cerebral aneurysm [5]. Nevertheless, it is not established yet what kind of anaesthetic technique is preferable for treatment of brain aneurysms by endovascular coiling.
The anaesthetist has a crucial role in facilitating neuroradiological procedures, understanding the procedures, their risks, side effects and complications like intracranial haemorrhage and thromboembolic stroke with incidence rate of 2.4% and 3.5% respectively [6], their management and treatment.
Sedation is an option but some authors point out high incidence of its failure to provide suitable conditions for the patient and radiographer and suggest to use general anaesthesia instead. General anaesthesia seems to be a better choice because it provides an immobile patient with improved image quality, patient comfort, and better control of the respiratory and hemodynamic profile. Nevertheless, most endovascular procedures are done in the interventional radiology suite and it has been shown that patients undergoing endovascular coiling have generally worse monitoring than those undergoing surgical treatment in operating theatre. Among main disadvantages of general anaesthesia belong an inability to perform neurological assessment perioperatively, and consequences of endotracheal intubation like hypertension, coughing or straining which can cause raised intracranial pressure.
Choice of anaesthetic drugs depends mainly on local practice and policy. They are also used, apart from anaesthesia and analgesia, to ensure brain protection from ischemia, decrease brain metabolism, and keep cardiovascular stability. Short-acting anaesthetics are preferred due to ability to assess patient’s neurological status early after intervention. Clinical studies dealing with the choice of anaesthetics brought some recommendations. Nevertheless, there is a lack of clinical data to support decision. Our study compared two frequently used short-acting anaesthetic agents, sevoflurane and propfol, to find out their effect on perioperative hemodynamic stability, rate of complications, and recovery time from anaesthesia.
Patients and methods
Patients
The study was approved by the Ethical Committee of the Martin University Hospital.
Suitable patients were randomly divided into two groups using quasi method. Exclusion criteria were: age below 18 years, pregnancy, severe heamodynamical instability requiring inotropic infusion preoperatively, and Glasgow Coma Scale below nine. Patients with uncontrolled hypertension, chronic anticoagulation therapy and coagulation disorders were also excluded from the study.
Their informed consent was aquired during pre-operative consultation. The Acute Physiology and Chronic Health Evaluation (APACHE II) and The American Society of Anaesthetists physical status classification system (ASA) were performed before the operation. All patients were treated by the same therapeutic protocol. Study physicians did not participate in clinical decisions. Study patients were not involved in other trials. Patient’s demographic and clinical state data are in the Table 1.
1. General characteristics of the patients at baseline 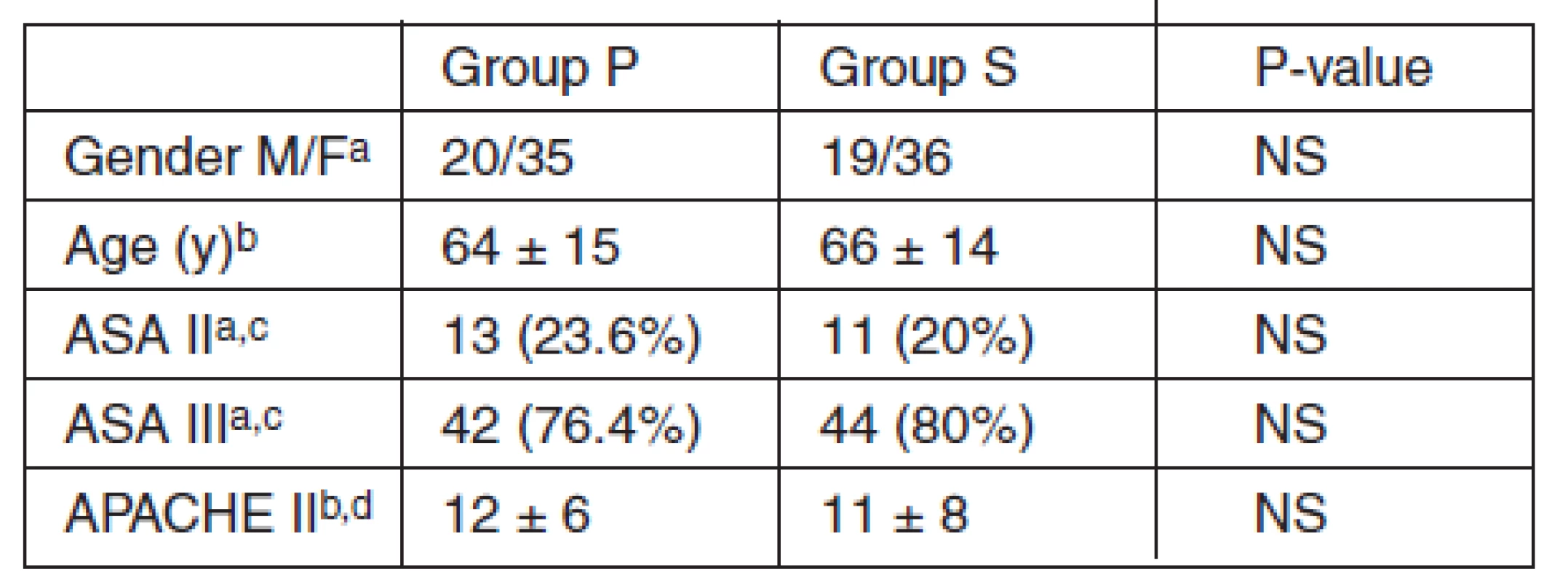
aNumber bMeans ± SD cAPACHE II, the Acute Physiology and Chronic Health Evaluation II dAmerican Society of Anaesthesiologists physical status classification system Patients‘neurology and aneurysm status on admission is in the Table 2.
2. Patients‘ neurology and aneurysm status on admission 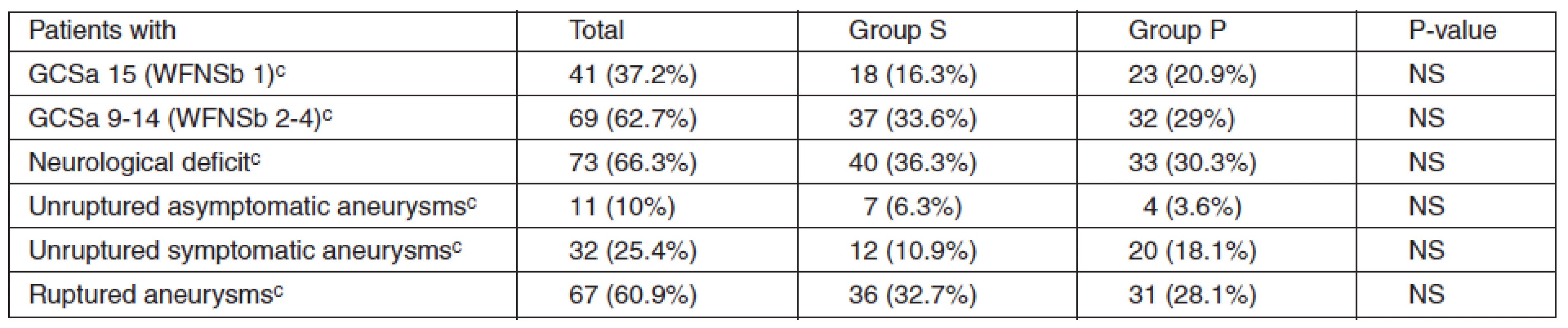
aGlasgow Coma Scale bWorld Federation of Neurosurgeons Scale cNumber Patient’s underlying medical condition is in the Table 3.
3. Underlying comorbidities 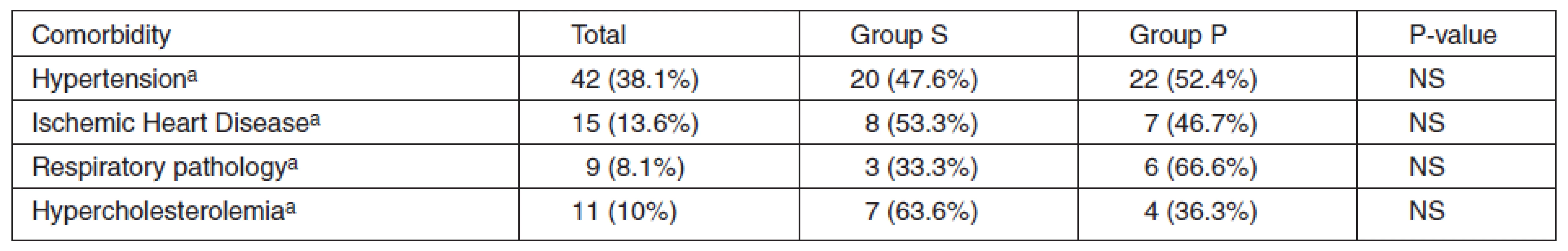
aNumber Method
All patients enrolled in the study were given nimodipine infusion continuously 20 mcg/kg/h to prevent vasospasm.
All patients were given heparin infusion continuously at a standard therapeutic dose sufficient to prolong the APTT ratio to twice that of normal.
We measured noninvasive or invasive blood pressure via catheter in radial artery of non-dominant hand, ECG, CVP via internal jugular or subclavian vein, SpO2, and diuresis.
All patients received 50 mg of tramadol IM 1 hour before operation.
All patients received 2 mg/kg of propofol, 1 mcg/kg of fentanyl, and 0.5 mg/kg of atracurium IV for induction of anaestesia. All were intubated and ventilated with volume control ventilation, tidal volume of 8 ml/kg, respiratory rate of 9–13/min according to ETCO2 (targeted to 4.5 kPa), and with PEEP of 4 cm of H2O.
Both groups were ventilated with a mixture of O2 and air in the ratio of 1 : 1. For maintance of anaesthesia, Group P patients were given 6 mg/kg/h of propofol IV in continuous infusion. Group S patients were given sevoflurane via inhalation in concentration of 1.1 MAC. Analgesia was done with fentanyl infusion of 1 mcg/kg/h, and we used atracurium infusion of 0.4 mg/kg/h for maintenance of neuromuscular block. Fentanyl and atracurium infusions were stopped 30–40 min before the end of surgery. Propofol and sevoflurane were discontinued immediately after the end of the procedure. All patients were extubated when protective functions of airways were restored.
None of the patients had any neurological monitoring during the procedure.
9 patients were excluded from the study (4 from Group P and 5 from Group S) during or after the operation due to urgent postoperative transfer to ITU and use of treatment influencing this study. It was due to cardiac failure (2 patients, one in each group), prolonged muscle paralysis (4 patients, 1 in Group P and 3 in Group S) and subarachnoid haemorrhage (3 patients, 2 in Group P and 1 in Group S). All of mentioned patients were excluded from the study due to urgent transfer to ITU and use of medications, which influence our study.
The Shapiro-Wilk W test was used for testing normality of distribution. This distribution was not normal so non-parametric methods were used for statistical analysis. Subjects’ baseline characteristics data (see Table 1) were analysed by contingency table or Kolmogorov-Smirnov’s test. Paired sample comparison was tested by Signed-Rank test. Differences between groups were examined by Mann-Whitney’s (Wilcoxon’s) test. P values less than 0.05 were considered significant.
Results
Study patients
110 patients were enrolled into the study and randomly divided into two groups. There was no statistical difference between the two study groups.
Parameters of hemodynamic
Mean arterial pressure in Group P was significantly lower then in Group S since the 10th minute of anaesthetics (Graph 1) till the end. This difference was statistically significant (P = 0.045).
1. Changes in MAP in the first 60 min after induction 
Heart rate varied more in Group S than in Group P but these differences were not statistically significant (See Graph 2).
2. Changes in heart rate in the first 60 min after induction 
Central venous pressure differences were without statistical significance between groups.
Parameters of ventilation
There were no significant differences in mean airway pressure and SpO2 between groups.
Perioperative complications
The study analysed complications occurring perioperatively only.
Higher incidence of bradycardia (defined as HR below 60 bpm) was seen in the Group P (P = 0.05). Higher incidence of hypertension (defined as systolic blood pressure over 150 torr) was seen in the Group S (P = 0.05).
For incidence of all complications see Table 4.
4. Incidence of perioperative complications 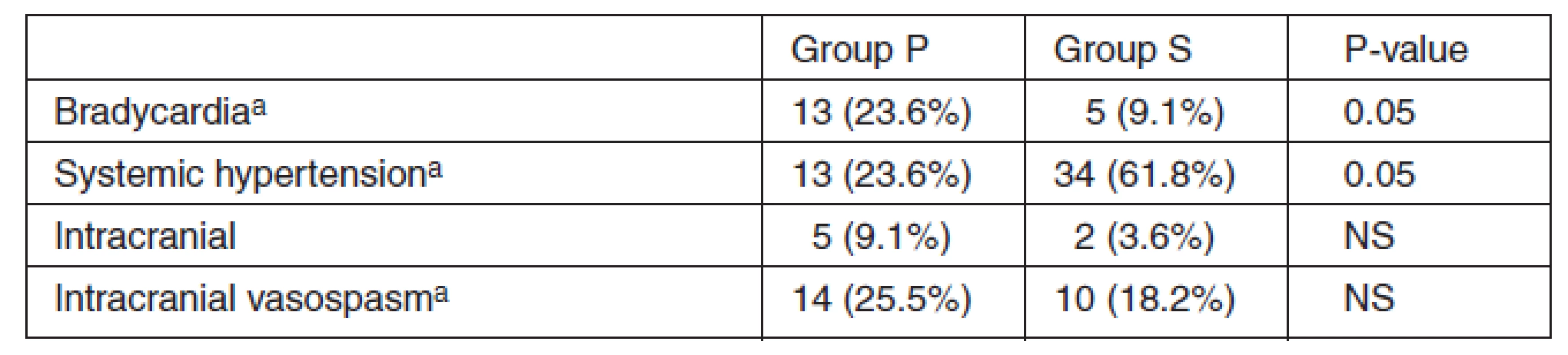
aNumber Discussion
Anaesthesia for endovascular treatment of brain aneurysms must provide hemodynamic stability, maintenance of cerebral perfusion pressure, control of intracranial pressure, as well as good conditions for the patient and the surgeon. An anaesthetist must plan smooth emergence, rapid awakening, and early neurological assessment of the patient in the postoperative period.
Balanced general anesthesia with sevoflurane or propofol has been widely accepted as anaesthetic management for patients undergoing neurosurgical procedures. Both agents demonstrate similar characteristics for anaesthetic induction, maintenance, emergence time, and early cognitive function [7, 8] although their cerebral effects are still matter of debate.
Propofol is one of the most used anaesthetic agents for induction. It is also used for the anaesthetic maintenance as total intravenous anaesthesia. There are some theoretical advantages of propofol over sevoflurane in brain protection. It posses anticonvulsive activity and decreases brain metabolism. Propofol is not associated with a significant modification of cerebral hemodynamics and demonstrates possible avoidance of undesirable effects in neuroanesthesia [9, 10]. On the other hand, its negative inotropic effect on blood pressure is well known. Its negative impact on blood pressure may lead to decreased intracranial pressure (ICP) and cerebral perfusion pressure (CPP).
Sevoflurane effect on cardiovascular system is dose depending. In comparison to other anaesthetic drugs, autoregulation of brain perfusion is well preserved with sevoflurane. Dilation of brain vessels is dose dependent and less evident in comparison with other inhalational agents [11] but may cause increased CPP and ICP during spontaneous ventilation.
In this study, propofol anaesthesia showed unfavourable decrease of mean arterial pressure and higher incidence of bradycardia in comparison to sevoflurane. Nevertheless, some pitfalls of this study should be mentionted. First, it is a lack of neurological monitoring of the depth of anaesthesia, for example by measuring Bispectral Index. Second, metabolic activity of the brain was not estimated, for example by SvjO2 measurement. We didn’t measure brain blood flow either, for example by transcranial Doppler ultrasound examination. The reason is that at the time of this study, there were not any of the equipments available in the hospital.
Conclusion
Our study results suggest that maintenance of general anaesthesia performed with sevoflurane may be more suitable anaesthetic option than anaesthesia with propofol infusion in patients undergoing brain aneurysm coiling. Nevertheless, larger study with perioperative neurological monitoring would be necessary to decide whether one of these anaesthetic agents is more preferable in neuroanaesthesia.
Do redakce došlo dne 21. 7. 2011.
Přijato do tisku dne 15. 1. 2012.
Adresa pro korespondenci:
Dr Ahmed S. El Akkad, MD
Anaesthetic & Intensive Care Consultant
Department of Anaesthesia and Intensive care, Doncaster and Bassetlaw General Hospital, Worksop, S81 0BD, United Kingdom
e-mail: elakkadahmed@yahoo.com
Sources
1. Alaraj, A., Wallace, A., Mander, N., Aletich, V., Charbel, F. T., Amin-Hanjani, S. Outcome following symptomatic cerebral vasospasm on presentation in aneurysmal subarachnoid hemorrhage: coiling vs. clipping. World Neurosurg., 2010, Jul, 74, 1, p. 138–142.
2. Dupont, S. A., Wijdicks, E. F., Lanzino, G., Rabinstein, A. A. Aneurysmal subarachnoid hemorrhage: an overview for the practicing neurologist. Semin. Neurol., 2010, Nov, 30, 5, p. 545–554.
3. Webb, S. T., Farling, P. A. Survey of arrangements for anaesthesia for interventional neuroradiology for aneurismal subarachnoid haemorrhage. Anaesthesia, 2005, 60, p. 560–564.
4. International Subarachnoid Aneurysm Trial (ISAT) Collaborative group. ISAT of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet, 2002, 360, p. 1267–1274.
5. Henkes, H., Fischer, S., Weber, W. et al. Endovascular coil occlusion of 1811 intracranial aneurysms: early angiographic and clinical results. Neurosurgery, 2004, 54, p. 268–280.
6. Osborn, I. P. Anesthetic considerations for interventional neuroradiology. Int. Anesthesiol. Clin., 2003, 41, p. 69.
7. Magni, G., Baisi, F., La Rosa, I., Imperiale, C., Fabbrini, V., Pennacchiotti, M. L. et al. No difference in emergence time and early cognitive function between sevoflurane-fentanyl and propofol-remifentanil in patients undergoing craniotomy for supratentorial intracranial surgery. J. Neurosurg. Anesthesiol., 2005, 17, p. 134–138.
8. Sneyd, J. R., Andrews, C. J., Tsubokawa, T. Comparison of propofol/remifentanil and sevoflurane/remifentanil for maintenance of anaesthesia for elective intracranial surgery. Br. J. Anaesth., 2005, 94, p. 778–783.
9. De Cosmo, G., Cancelli, I., Adduci, A., Merlino, G., Aceto, P., Valente, M. Changes in hemodynamics during isofluraneand propofol anesthesia: a comparison study. Neurol. Res., 2005, 27, p. 433–435.
10. Kaisti, K. K., Metsähonkala, L., Teräs, M., Oikonen, V., Aalto, S., Jääskeläinen, S. et al. Effects of surgical levels of propofol and sevoflurane anesthesia on cerebral blood flow in healthy subjects studied with positron emission tomography. Anesthesiology, 2002, 96, p. 1358–1370.
11. Holmström, A., Akeson, J. Sevoflurane induces less cerebral vasodilation than Isoflurane at the same A-line autoregressive index level. Acta Anaesthesiol. Scand., 2005, 49, p. 16–22.
Labels
Anaesthesiology, Resuscitation and Inten Intensive Care Medicine
Article was published inAnaesthesiology and Intensive Care Medicine

2012 Issue 1-
All articles in this issue
- Use of neuromuscular blocking agents in general anaesthesia for surgery: A three-month, single-centre study in a Czech regional hospital
- Kardiorelax 2011 – a five-day observational study of neuromuscular blockade during adult cardiac surgery in the Czech Republic
- Influence of age and gender on the pharmacodynamic parameters of rocuronium during total intravenous anaesthesia – a prospective study
- Quality of epidural analgesia and incidence of early complications after major surgery
- Thromboprophylaxis and neuroaxial anaesthesia in obstetrics
- Propofol vs. sevoflurane as anaesthetic maintenance agents in patients undergoing brain aneurysm coiling – randomized prospective study
- Anaesthesiology and Intensive Care Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Quality of epidural analgesia and incidence of early complications after major surgery
- Thromboprophylaxis and neuroaxial anaesthesia in obstetrics
- Use of neuromuscular blocking agents in general anaesthesia for surgery: A three-month, single-centre study in a Czech regional hospital
- Propofol vs. sevoflurane as anaesthetic maintenance agents in patients undergoing brain aneurysm coiling – randomized prospective study
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

