-
Medical journals
- Career
THE INTERPOLATION NASOLABIAL FLAP: THE ADVANTAGEOUS SOLUTION FOR NASAL TIP RECONSTRUCTION IN ELDERLY AND POLYMORBID PATIENTS
Authors: J. Bayer; M. Duskova; P. Horyna; M. Haas; K. Schwarzmannová
Authors‘ workplace: Department of Plastic Surgery, 3rd Faculty of Medicine, Charles University and Faculty Hospital Královské Vinohrady, Prague, Czech Republic
Published in: ACTA CHIRURGIAE PLASTICAE, 55, 2, 2013, pp. 44-48
INTRODUCTION
The primary skin cancer is the most frequent type of malignant tumor. Its incidence has an increasing tendency. The predominating causes of skin tumors include skin phototype and exposure to UV light. The accumulation of mutation alterations and reduced immunity related to other diseases such as diabetes or immunosupression after organ transplantation are the most common explanations of higher incidence in the elderly and in polymorbid patients. The most frequently affected area is the face and especially the nose, due to its permanent exposure to the sun (3). Tumors often occur on the nasal tip. The postsurgical deformity of this area is rather noticeable, because it is the center of the facial triangle. Patient may be very old and even suffering from several serious comorbidities, a lot of them enjoy social life, which is severely affected by any unacceptable deformity. The subsequent reconstruction is therefore an essential condition for every patient. In common practice the decision about the most suitable method of nasal tip reconstruction is often a result of a compromise between the cosmetic effect and acceptable stress for the patient.
Depending on the general condition, local finding, and patient expectations the possible approaches of nasal tip reconstruction include the following:
- Full thickness skin graft
- Local advancement flap – bilobed flap – dorsal nasal flap
- Forehead flap
- Nasolabial flap
The last one is probably the most frequent method for reconstruction in the facial triangle area due to its versatility and effectiveness. (1, 8, 9) The nasolabial (so-called melolabial) flap is also one of the first local flaps used for closure of defects in the midfacial area. (3, 4, 5, 6, 10, 11, 13) It was described in 1846 by a German surgeon Johann Friedrich Dieffenbach and still remains the most useful option (2, 7).
For the nasal tip reconstruction the variant of the nasolabial flap - so-called interpolation nasolabial flap - is the most suitable (12). Its pedicle is not closely adjacent to the recipient site. The body of flap crosses a healthy skin to reach the defect. Thus an interpolation flap is a two-stage surgery, because bridge must be divided when the new vascular connection is established between the wound and the flap (usually 3 weeks) (2, 7, 12). (Fig. 1, 2.)
Fig. 1. Interpolation nasolabial flap 
Fig. 2. Interpolation nasolabial flap 
MATERIAL AND METHOD
From total amount of 165 patients suffering from basal cell carcinoma of the nasal tip and operated between the years 2010 and 2012 a final group of fifty patients was chosen for the research (29 males/21 females). The subjects for each group were chosen according to the similarity of their defect and they were divided into the following five groups based on the type of the reconstructive surgery method: skin graft, bilobed flap, dorsal nasal flap, forehead flap and interpolation nasolabial flap. At the time of surgery the patients were in the age between 54 and 86 years, the average age was 67.3 years. They all suffered from basal cell carcinoma of the nasal tip and various comorbidities: ischemic heart disease, status post myocardial infarction, status post ictus, chronic obstructive pulmonary disease, hypertension, diabetes, and chronic renal failure.
We started the surgery with drawing of tumor excision. Then we performed excision of the tumor area. According to the size and character of the defect an appropriate method of reconstruction was chosen. To homogenize our group we selected patients with similar defects of 14–18 mm in diameter (average 15.8 mm).
In 7 cases we used the skin flap in combination with a cartilage graft according to the depth of tumor involvement. The division of the flap followed in 18–21 days (aver. 19.2) after the primary surgery.
A standardized questionnaire was used to objectivize the final cosmetic effect.
RESULTS
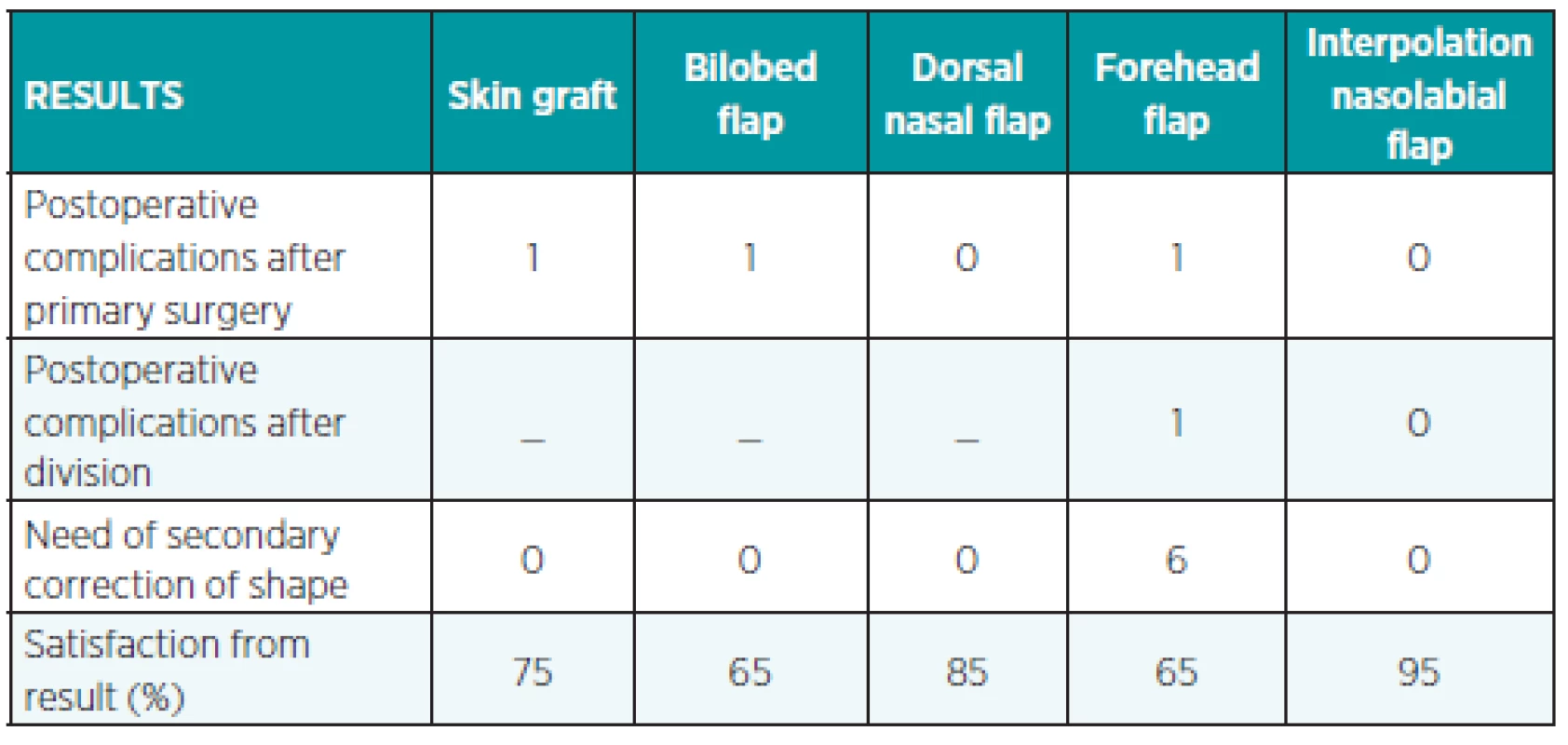
Results of the research are provided in Table 1.
According to the desired characteristics – good vascular supply, matching skin color and texture, sufficient amount of material, possibility to cover exposed cartilage or to combine it with cartilaginous graft; scars of minimal visibility, perfect aesthetic outcome, use of local anesthesia, short surgical time, and technical simplicity – the interpolation nasolabial flap was selected as the most appropriate.
CASE REPORT
86-year-old man with the following comorbidities: hypertension, ischemic heart disease, right-handed plegia after ischemic ictus and hypacusis.
Clinical finding: pinkish nodular tumor of the nasal tip, 9x10 mm.
The excision of the tumor resulted in a defect with the dimension of 12x14 mm, involving the full-thickness of the skin and perichondrium, with exposure of the alar cartilage.
Histological examination: completely removed basal cell carcinoma, mainly solid, partially cystic.
This condition was treated with an interpolation nasolabial flap with a length of 75 mm and width of 14 mm. The flap was divided after 20 days. In both phases the healing was without problems. (Fig. 3, 4, 5, 6.)
Fig. 3. Basocellular carcinoma of the nasal tip 
Fig. 5. Result after three weeks before division 
Fig. 6. Result after four months 
DISCUSSION
When choosing the method of nasal tip reconstruction, it is necessary to consider surgical stress for patient carefully, as well as local condition of the defect, technical demands of the approach, and type of anesthesia. These circumstances must meet the expected benefit of the surgery. The surgery must remove the disease completely, however, it is necessary to preserve good function and acceptable appearance. The need of functional and aesthetic effect may be different according to individual expectations. The simplest method for closure of nasal tip defect is a skin graft. It can be used merely in the superficial defects with suitable vascular bed (8). The cosmetic outcome of skin grafts may be poor due to the color and texture mismatch. The local flaps such as a nasolabial or a dorsal nasal flap provide better results. Bilobed flaps are now largely abandoned in nasal reconstruction, because they harm the subunit principle either at the donor site or at the recipient site (11). Dorsal nasal flaps are often linked with apparent scars and are insufficient for large tip defects (2). In case of deep and large defects of the nasal tip only interpolation nasolabial flap and forehead flap can be used. Both are two-stage procedures and can be combined with cartilaginous grafts. Forehead flap, which is more suitable for larger defects of the nasal dorsum and tip, represents more demanding surgery, which requires general anesthesia and results in a more visible scar at the donor area (12). The postoperative morbidity can be considerably higher for forehead flaps than for nasolabial flaps (4). The review of different reconstructive methods including their advantages, disadvantages, and limitations is provided in Table 2.
2. Review of methods for nasal tip reconstruction 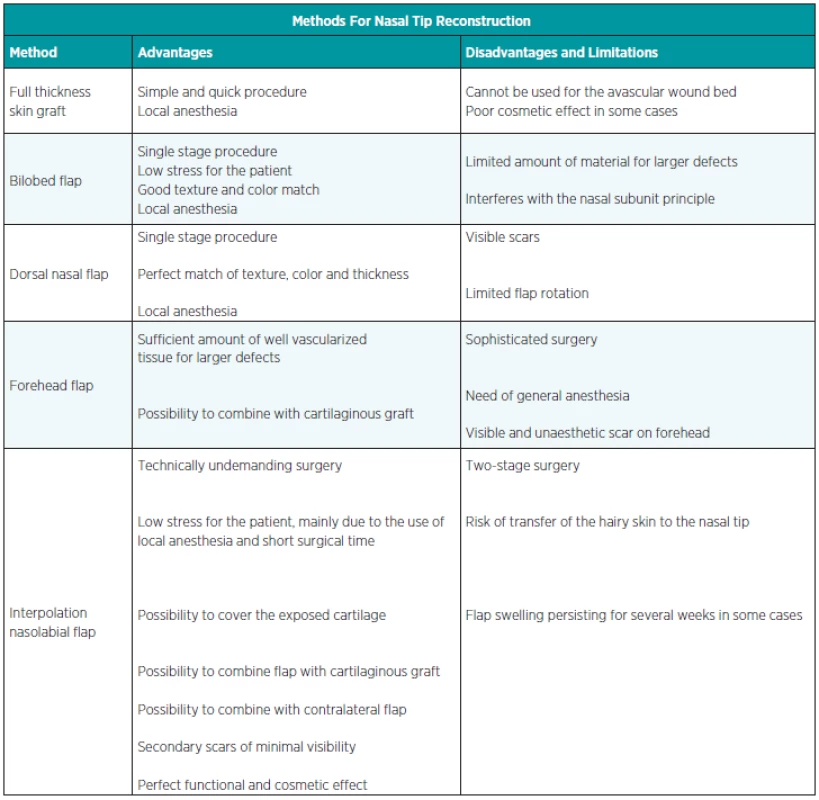
CONCLUSION
The interpolation nasolabial flap is an easy and effective approach for reconstruction of smaller and middle-sized defects of the nasal tip. The flap perfectly matches the requirements of complex reconstruction including the possibility to combine it with cartilage graft. It produces a good functional and aesthetic outcome with minimal stress for the patient. Despite the fact that it is a two-stage surgery, it is suitable for patients with higher expectations even in cases when they are rather old and suffer from a lot of severe comorbidities.
All co-authors have seen and agree with the contents of the manuscript and there is no financial interest to report.
Address for correspondence:
Jiri Bayer, MD
Department of Plastic Surgery
3rd Faculty of Medicine, Charles University and Faculty Hospital Královské Vinohrady,
Šrobárova 50, 100 34 Prague 10
Czech Republic
E-mail: bayer01@seznam.cz; duskova@fnkv.cz
Sources
1. Mazzola RF., Marcus S. History of total nasal reconstruction with particular emphasis on the folded forehead flap technique. Plastic and Reconstructive Surgery 72, 1983, p. 408–414.
2. McGregor A., McGregor I. Fundamental techniques of plastic surgery and their surgical applications. 10th ed. Edinburg: Churchil Livingstone, 2000, p. 178–179.
3. Hisashi O., Nobuyuki S., Takashi A. Clinical experience with nasolabial flaps. Annals of Plastic Surgery, 6, 1981, p. 207–212.
4. Rohrich RJ., Conrad MH. The superiorly based nasolabial flap for
simultaneous alar and cheek reconstruction. Plastic and Reconstructive Surgery, 108, 2001, p. 1727–1730.
5. Rose EH. One-stage arterialized nasolabial island flap for floor of mouth reconstruction. Annals of Plastic Surgery, 6, 1981, p. 71–75.
6. Rudkin GH., Carlsen BT., Miller TA. Nasolabial flap reconstruction of large defects of the lower lip. Plastic and Reconstructive Surgery, 111, 2003, p. 810–817.
7. Thorne CH. Grabb and Smith Plastic Surgery. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 1997, p. 392.
8. Thornton JF., Griffin JR., Constantine FC. Nasal reconstruction: An overview and nuances. Seminars in Plastic Surgery, 22, 2008, p. 257–268.
9. Thornton JF., Weathers WM. Nasolabial flap for nasal tip reconstruction. Plastic and Reconstructive Surgery, 122, 2008, p. 775–781.
10. Turan A., Kul Z., Türkaslan T., Özyigit T., Ozsoy Z. Reconstruction of lower half defects of the nose with the lateral nasal artery pedicle nasolabial island flap. Plastic and Reconstructive Surgery, 119, 2007, p. 1767–1772.
11. Uchinuma E., Matsui K., Shimakura Y., Murashita K., Shioya N. Evaluation of the median forehead flap and the nasolabial flap in the nasal reconstruction. Aesthetic Plastic Surgery, 21, 1997, p. 86–89.
12. Weerda H. Reconstructive facial plastic surgery. Stuttgart: Georg Thieme Verlag; 2001, p. 36–46, 62.
13. Yanai A., Nagata S., Tanaka H. Reconstruction of the columella with bilateral nasolabial flaps. Plastic and Reconstructive Surgery, 77, 1986, p. 129–132.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2013 Issue 2-
All articles in this issue
- Index Acta Chir. Plast. Vol. 55, 2013
- Contens Acta Chir. Plast. Vol. 55, 2013
- PENIS AUGMENTATION BY APPLICATION OF SILICONE MATERIAL: COMPLICATIONS AND SURGICAL TREATMENT
- LIPOMODELLING: AN IMPORTANT ADVANCE IN BREAST SURGERY
- THE INTERPOLATION NASOLABIAL FLAP: THE ADVANTAGEOUS SOLUTION FOR NASAL TIP RECONSTRUCTION IN ELDERLY AND POLYMORBID PATIENTS
- EPILEPTICS AND BURNS
- RECONSTRUCTION OF A NASAL TIP DEFECT USING A V-Y ISLAND DORSAL NASAL FLAP WITH UNILATERAL VASCULAR SUPPLY. A CASE REPORT
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- PENIS AUGMENTATION BY APPLICATION OF SILICONE MATERIAL: COMPLICATIONS AND SURGICAL TREATMENT
- THE INTERPOLATION NASOLABIAL FLAP: THE ADVANTAGEOUS SOLUTION FOR NASAL TIP RECONSTRUCTION IN ELDERLY AND POLYMORBID PATIENTS
- LIPOMODELLING: AN IMPORTANT ADVANCE IN BREAST SURGERY
- RECONSTRUCTION OF A NASAL TIP DEFECT USING A V-Y ISLAND DORSAL NASAL FLAP WITH UNILATERAL VASCULAR SUPPLY. A CASE REPORT
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career