-
Medical journals
- Career
EPILEPTICS AND BURNS
Authors: P. Bukovčan; J. Koller
Authors‘ workplace: Department of Burns and Reconstructive Surgery, University Hospital Bratislava, Ružinov Hospital, Bratislava, Slovak Republic
Published in: ACTA CHIRURGIAE PLASTICAE, 55, 2, 2013, pp. 49-50
INTRODUCTION
Epilepsy patients whose seizures are not adequately controlled are at increased risk of injuries. The patient with an epileptic seizure who is close to the source of heat can sustain a burn injury, which is deep and serious. That is why this group of patients requires careful attention. The aim of this paper is to ascertain the number of patients with burn injury sustained during an epileptic seizure treated in our facility, to identify the characteristics of these types of injuries and to suggest preventive measures which could reduce the frequency and morbidity of such injuries.
PATIENTS AND METHODS
We performed a retrospective review of our burn centre registry data, identifying all the patients admitted with burns within the six-year period from January 2005 to December 2011. From all of the hospitalized patients with burns treated in this period only patients who experienced their burns during epileptic seizures were included. The collected data were compared with the results and findings of similar studies and were evaluated. The study was approved by the Ethics Committee of Ružinov Hospital in which it was performed.
RESULTS
Totally 7 women with average age of 45 years (range 27–53) were included into this retrospective study. This group of seven patients accounted 1% of adult admissions (695 patients) during the study period. The average BSAB was 2.4% (range 0,5–6). The burns were predominantly deep and affected mostly the upper part of the body – hands (5 patients) and upper/lower arms (3 patients). One patient sustained superficial and one sustained deep burn of the face, respectively. All burns occurred in a domestic setting during household activities (cooking, ironing). Thermal injury included contact burn (6 patients with deep burns), followed by scald (one patient with superficial burns). Six out of 7 patients (85%) required excision of deep burns and skin grafting procedure; one patient with burn on dominant hand required also amputation of the distal phalanx of the thumb. One case required two-stage operation, including skin xenografts for temporary coverage of excised wound in the first stage. Skin xenografts as a temporary biological skin substitute was used because take of the skin graft was questionable. In the second stage, skin xenografts were removed and well vascularized wound bed was covered by skin autografts. Only one patient (15%) sustained superficial burns, which could be treated conservatively. The duration of hospital stay was 13 days in average (range 8–24). The data and results obtained are shown in the Table 1.
1. Patients included in the study 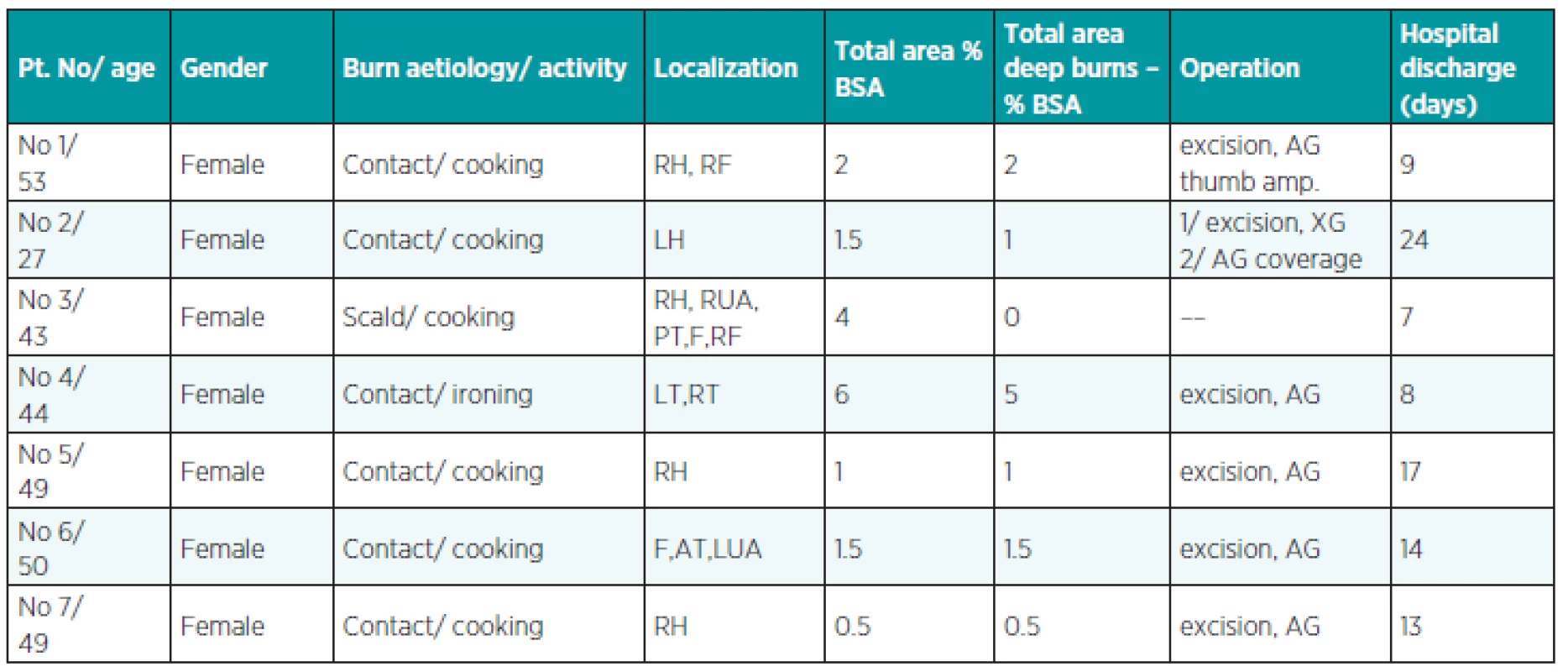
Abbreviations: RH, LH: right, left hand; RF: right forearm; RUA, LUA: right, left upper arm; F: face; AT, PT: anterior, posterior trunk; LT, RT: left, right thigh; BSA: body surface area; AG: autograft; XG: xenograft; thumb amp.: partial amputation of the thumb DISCUSSION
The frequency of burns associated with epilepsy was 1%, which is similar with the results reported by Ansari (1) (1.1%) and comparable with the results reported by Josty (4) (1.6%). According to the gender, all of our patients who were included in this study were women performing their household activities, mostly cooking. Female predominance in this type of injury was observed also in other studies (1, 3). Higher risk of burns among women with epileptic seizures could be explained by their greater household activity. Despite the small extent (mean BSAB 2.4%), the burns were predominantly deep and serious. The majority of burned patients (85%) included in our study required operative treatment, which was also reported by Karacaoĝlan (5), Spitz (6), Aust (2) and Josty (4). Predominance of deep burns among these patients is probably due to the longer exposure time to the source of heat during an epileptic seizure.
The majority of these types of injuries are preventable. The knowledge of the burn aetiology is very helpful in aiming the preventive measures to reduce the incidence of burn injuries during epileptic seizures. Most patients in our study sustained burns during cooking. That is why the preventive measures should be focused on the risk of burns in an epileptic patient while performing this type of activity. It should be recommended to the patients to minimize staying in the kitchen alone during cooking. Patients should use microwave oven, which is likely to be much safer than a stove-top.
One of our patients sustained burns during ironing. This activity should be minimized or should not be performed without the presence of a healthy adult person.
However, other studies (2, 3, 7) reported a higher incidence of scalds caused by showering or bathing in a tub. It would be reasonable to inform the patients also about this potential threat with an advice to install safety devices to their water heaters that limit maximum water temperature.
Only one patient in our study was treated for seizures before burn injury. The other patients in our study were using anticonvulsive drugs for at least five years before burn injury. Therefore the proper dosage of anticonvulsant medication and also the willingness of the patients to take part in the outpatient appointments to adjust the doses of medication and to obtain better seizure control is of paramount importance.
Association of burns and epilepsy has been demonstrated before. Therefore patients with epilepsy should be informed about all potential threats at the time of neurological diagnosis including also the risk of serious burn injury, which should be emphasized.
Conflict of interest statement: The authors have neither conflict of interest nor funding support for publishing this paper.
Address for correspondence:
Peter Bukovčan, M.D., PhD.
Department of Burns and Reconstructive Surgery
University Hospital Bratislava
Ružinov Hospital
Ružinovská 6, 826 06 Bratislava
Slovak Republic
E mail: bukovcanmed@hotmail.com
Sources
1. Ansari Z., Brown K., Carson N. Association of epilepsy and burns – a case control study. Aust. Fam. Physician, 37, 2008, p. 584–589.
2. Aust M., Guggenheim M., Gohritz A., Künzi W., Handschin A., Vogt P., Giovanoli, P. Thermal trauma sustained during epileptic seizures – analysis of 33 cases. Handchir. Mikrochir. Plast. Chir., 40(6), 2008, p. 372–376.
3. Jang YC., Lee JW., Han KW., Han TH. Burns in epilepsy: seven years of experience from the Hallym Burn Center in Korea. J. Burn Care Res., 27(6), 2006, p. 877–881.
4. Josty IC., Narayanan V., Dickson WA. Burns in patients with epilepsy: changes in epidemiology and implications for burn treatment and prevention. Epilepsia, 41(4), 2000, p. 453–456.
5. Karacaoĝlan N., Uysal A. Deep burns following epileptic seizures. Burns, 21, 1995, p. 546–549.
6. Spitz MC. Severe burns as a consequence of seizures in patients with epilepsy. Epilepsia, 33, 1992, p. 103–107.
7. Unglaub F., Woodruff S., Demir E., Pallua N. Patients with epilepsy: a high-risk population prone to severe burns as a consequence of seizures while showering. J. Burn Care Rehabil., 26(6), 2005, p. 526–528; discussion 525.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2013 Issue 2-
All articles in this issue
- Index Acta Chir. Plast. Vol. 55, 2013
- Contens Acta Chir. Plast. Vol. 55, 2013
- PENIS AUGMENTATION BY APPLICATION OF SILICONE MATERIAL: COMPLICATIONS AND SURGICAL TREATMENT
- LIPOMODELLING: AN IMPORTANT ADVANCE IN BREAST SURGERY
- THE INTERPOLATION NASOLABIAL FLAP: THE ADVANTAGEOUS SOLUTION FOR NASAL TIP RECONSTRUCTION IN ELDERLY AND POLYMORBID PATIENTS
- EPILEPTICS AND BURNS
- RECONSTRUCTION OF A NASAL TIP DEFECT USING A V-Y ISLAND DORSAL NASAL FLAP WITH UNILATERAL VASCULAR SUPPLY. A CASE REPORT
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- PENIS AUGMENTATION BY APPLICATION OF SILICONE MATERIAL: COMPLICATIONS AND SURGICAL TREATMENT
- THE INTERPOLATION NASOLABIAL FLAP: THE ADVANTAGEOUS SOLUTION FOR NASAL TIP RECONSTRUCTION IN ELDERLY AND POLYMORBID PATIENTS
- LIPOMODELLING: AN IMPORTANT ADVANCE IN BREAST SURGERY
- RECONSTRUCTION OF A NASAL TIP DEFECT USING A V-Y ISLAND DORSAL NASAL FLAP WITH UNILATERAL VASCULAR SUPPLY. A CASE REPORT
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

