-
Medical journals
- Career
Evaluation of retinal light scattering, visual acuity, refraction and subjective satisfaction in patients after Acrysof IQ PanOptix intraocular lens implantation
Authors: M. Středová 1; T. Řeháková 1; V. Veliká 1; P. Rozsíval 1; L. Hejsek 2; N. Jirásková 1
Authors‘ workplace: Oční klinika LFUK a FN Hradec Králové, Sokolská 581, Hradec Králové, 500 05, Přednostka: prof. MUDr. Naďa Jirásková, Ph. D., FEBO 1; VISUS, s. r. o., 17. listopadu 291, Police nad Metují, 549 54, Primář: doc. MUDr. Jan Studnička, Ph. D. 2
Published in: Čes. a slov. Oftal., 75, 2019, No. 6, p. 316-322
Category: Original Article
doi: https://doi.org/10.31348/2019/6/4Overview
Aim: To evaluate the retinal light scattering, visual acuity, refraction and subjective satisfaction in patients after implantation of Acrysof IQ PanOptix intraocular lens.
Methods: Our group included 32 eyes of 21 patients who underwent cataract surgery or refractive lensectomy with Acrysof IQ PanOptix multifocal intraocular lens implantation at the Ophthalmology Clinic of Faculty Hospital Hradec Králové during the time from September 2015 to December 2017. The observed parameters were visual acuity, subjective refraction, retinal light scattering and patient‘ subjective satisfaction. Preoperative refractive values and visual acuity values were compared with results obtained on day 1, 1 month and at an average of 27 months postoperatively. Subjective satisfaction and degree of light scattering on the retina were evaluated at the end of the follow-up period.
Results: Preoperative, uncorrected distant visual acuity improved from an average of 0,51 ± 0,29 (expressed in decimal values) to 0,94 ± 0,10 at the end of the follow-up period. Preoperative best-corrected distance visual acuity improved from an average of 0,95 ± 0,19 to 1,00 ± 0,09 at the end of the follow-up period. The mean value of preoperative uncorrected near visual acuity was 8,29 ± 4,93 of Jaeger charts, the mean value of uncorrected near visual acuity at the end of the follow-up period was 1,00 ± 0 of Jaeger charts. Subjective satisfaction was assessed using a standardized VF-14 questionnaire at least 1 year after surgery (mean follow-up of 27 months). Retinal light scattering was examined using an Oculus C-Quant instrument. The retinal light scattering value in our sample was 1,12 ± 0,19. In only 6 eyes of 4 patients, the resulting value was outside the physiological range used for eyes with lens crystallina
Conclusion: The value of light scattering on the retina is a factor affecting the degree of sensitivity to glare after implantation of multifocal intraocular lenses. In our group, we observed a deviation from the physiological range of retinal light scattering in only 6 eyes of 4 patients, but this did not lead to a deterioration in subjective postoperative satisfaction.
Keywords:
multifocal intraocular lens – retinal light scattering – Acrysof IQ PanOptix – C-Quant
INTRODUCTION
The aim of current refractive surgery is not only to attain the best possible objective refractive result, but above all a high degree of postoperative subjective patient satisfaction [7]. A decrease of the quality of the retinal image and a subsequent deterioration of visual functions, with the occurrence of adverse “secondary optic phenomena” following refractive surgery may take place due to the influence of increased intraocular light scattering [6]. In particular, after the performance of refractive lensectomy (or alternatively cataract surgery) with implantation of a multifocal intraocular lens, dysphotopssia may markedly influence postoperative quality of vision. Despite the fact that this concerns a significant factor, at the present time it is still a relatively complex matter to quantify. In regular practice, subjective questionnaires are used to determine and evaluate the presence of disruptive secondary optic phenomena [1].
We are informed of the distribution of brightness on the retina at the moment when the eye fixes on a new point source by the point of spread function (PSF) curve, which thus defines the quality of the retinal image. The PSF curve is of a Guassian shape. The peak of the curve is determined by visual acuity, its outer parts by light dispersion [5]. Evidence on the outer part of the curve is provided by measurement using the instrument Oculus C-Quant (Oculus GmbH, Germany) [6]. The aim of our study was to evaluate subjective satisfaction, visual acuity, refraction and light scattering on the retina following the implantation of the multifocal intraocular lens AcrySof IQ PanOptix (Alcon Laboratories, Inc., Fort Worth, TX, USA).
Cohort of patients
The cohort incorporates patients in whom an AcrySof IQ PanOptix artificial multifocal intraocular lens [17] was implanted at the Department of Ophthalmology at the University Hospital in Hradec Králové within a time frame from September 2015 to October 2017. The study included 32 eyes of 21 patients, of whom 33% were women and 67% men. The average age of the patients was 56 ± 8.7 years (range 42 to 75 years). In 59% of eyes the implantation of the PanOptix lens was performed within the framework of refractive lensectomy, in the remaining 41% within the framework of cataract surgery. Preoperative refractive values and values of visual acuity were compared with the results obtained on the 1st day, 1 month and with an interval of an average of 27 months after surgery (minimum 13, maximum 38). The parameters of subjective satisfaction and the degree of light scattering on the retina were evaluated only at the end of the observation period. The preoperative data is presented in table 1
1. Preoperative patient data 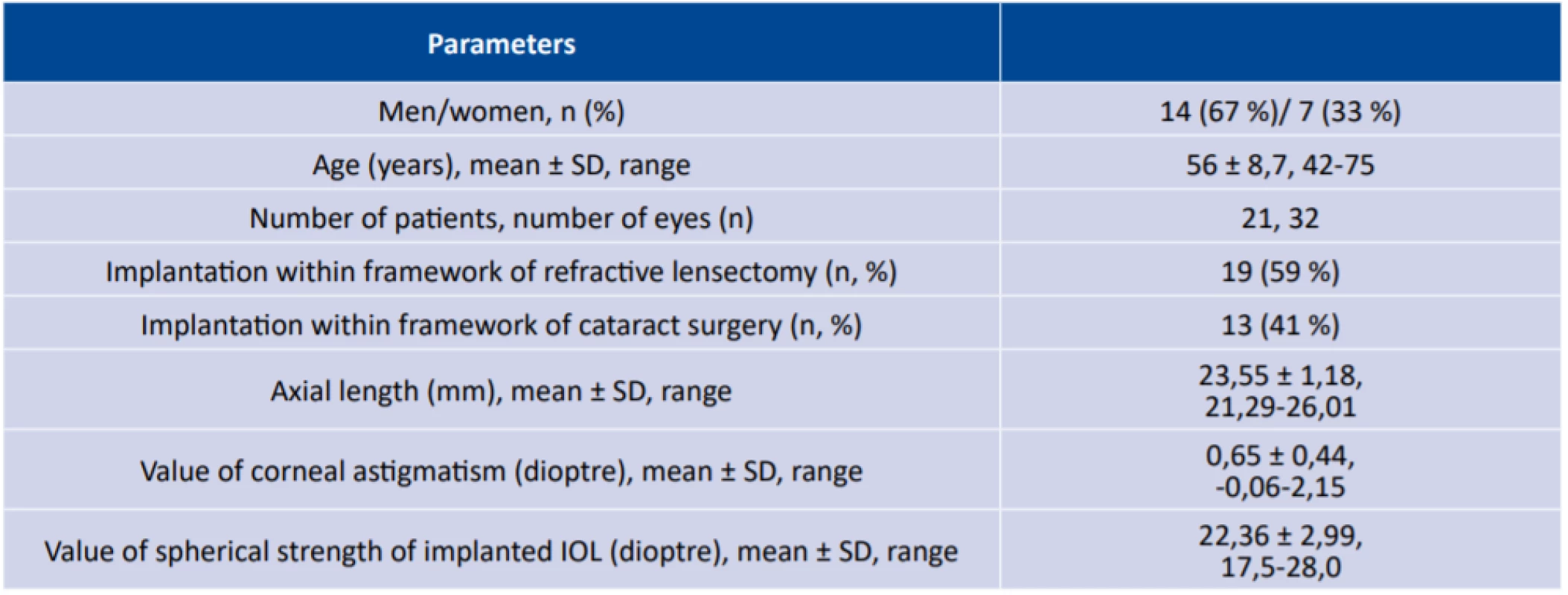
n (number of patients), mm (millimetre), SD (standard deviation), IOL (artificial intraocular lens) METHOD
All the patients underwent a preoperative examination, which covered: recording of personal medical history, examination of uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) for distance and near vision, examination of dominance, measurement of intraocular pressure (non-contact tonometer, NIDEK NT-530), performance of biometry (IOLMaster, Carl Zeiss Meditec AG), corneal topography (Pentacam, Oculus, Inc.) and examination of the anterior segment. In conclusion an examination of the ocular fundus was performed, and in the case of absence of a foveal reflex also examination of the macula by optical coherence tomography (OCT) (CIRRUS HD-OCT, Zeiss).
The exclusion criteria for implantation of a multifocal intraocular lens incorporated: retinal pathology (disease of macula, diabetic retinopathy, condition following retinal detachment), pathology of the optic nerve and cornea (irregular astigmatism, endothelial dystrophy), dry eye syndrome, loose suspensory apparatus of lens, uveitis, glaucoma and condition following ocular trauma. In our cohort there were no patients who had undergone a prior laser corneal refractive procedure. Patients with markedly unrealistic expectations and patients who did not accept the possibility of the occurrence of secondary optic phenomena following the implant of a multifocal intraocular lens (MF IOL) were excluded from the indication. Informed consent was obtained from each patient.
Observed parameters:
UVA – uncorrected visual acuity, BCVA – best corrected visual acuity, subjective refraction, retinal light scattering, subjective satisfaction.
Evaluation of retinal light scattering
We examined retinal light scattering with the aid of the instrument Oculus C-Quant (Oculus GmbH, Germany) at an interval of 27 months after surgery. The C-Quant instrument uses the compensatory comparative method [4]. Each patient was examined monocularly. During the course of the examination, a field is presented to the patient with a number of concentric rings, inside which is a central circle divided into two halves. The left testing field corresponds to the intensity of the scattered light, while the compensatory light is projected into the right testing field. During the examination a circular source of glare is switched on and off at a frequency of 8 Hz (peripheral ring), and the examined patient fixes with the fovea on the centre of the illuminated surface (central ring). Upon activation of the source of glare, a part of the light is scattered by means of passage through the optic media (here primarily through the MF IOL) and thus deflected from the fovea. Subsequently this part of the light is projected onto a point onto which the central testing field (area of the fovea) is also projected. Upon switching off the source of glare, the scattered light is not present in the eye, and therefore only light that is present in the centre of the illuminated surface falls upon the fovea. The patient has the task of indicating with the press of a button which half of the central circle is flashing more pronouncedly. Light scattered inside the eye is measured by log units. Higher values mean a greater scattering of light in the eye [10].
Subjective satisfaction questionnaire
Subjective patient satisfaction was evaluated with the aid of the standardised questionnaire Visual Functioning Index (VF-14), completed at a time of 1 year or more after the performance of the surgery. The questions are targeted at subjective complaints upon the performance of regular daily activities, under both photopic and mesopic conditions. The questions are answered by the patient with a score of zero to four points (4 – no difficulties in performing activity, 1 – large difficulties, 0 – activity not performed due to poor vision), an arithmetical average is subsequently calculated from the individual responses, and the result is multiplied by 25. The resulting value is always located within the range of 0 to 100, the higher the value, the less subjective complaints the patient has [16]. We included in our study only questionnaires from patients in whom the reliability parameters of examination by the C-Quant instrument were met.
Statistical analysis
Quantitative data is expressed by the mean, standard deviation (SD) and range. Values of UCVA and BCVA were evaluated by means of a Wilcoxon test. Statistical significance was defined as p < 0.05.
RESULTS
We evaluated sensitivity to glare, which was examined monocularly at a follow-up examination with an interval of 12 months and longer following the implantation of the artificial intraocular lens PanOptix with the aid of the C-Quant instrument. The study included only patients who attained such values of Esd parameters (standard deviation of individual points of measurement < 0.08) and Q parameter (reliability coefficient > 1), in order for the results to be considered credible [5]. At the same time, patients with a finding of secondary cataract were excluded from the study due to potential distortion of the results. The average length of duration of the examination using the C-Quant instrument was 99 ± 17 seconds. The average level of light scattering (log(s)), thus the ratio between undesirable light scattering and desirable light scattering was 1.12 ± 0.19. The Esd value was 0.06 ± 0.01 and the mean Q parameter was 1.66 ± 0.26. The evaluation of retinal light scattering is recorded in graph 5, 81% of eyes corresponded to the physiological range. The resulting value was outside of the physiological range in only 6 eyes (19%) of 4 patients. The results are recorded in graph 6.
In our cohort the mean resulting value following processing of the questionnaires was 98.02 ± 3.54 (100 maximum satisfaction, 0 – dissatisfaction). Patients stated the greatest problems during delicate manual tasks (knitting, sewing) and night driving of motor vehicles, the point average in these questions was 3.64 and 3.7. The questionnaire, with the resulting mean point evaluation, is presented in table 2.
2. Questionnaire VF-14 (Visual Functioning Index 14) for evaluation of satisfaction with postoperative visual functions 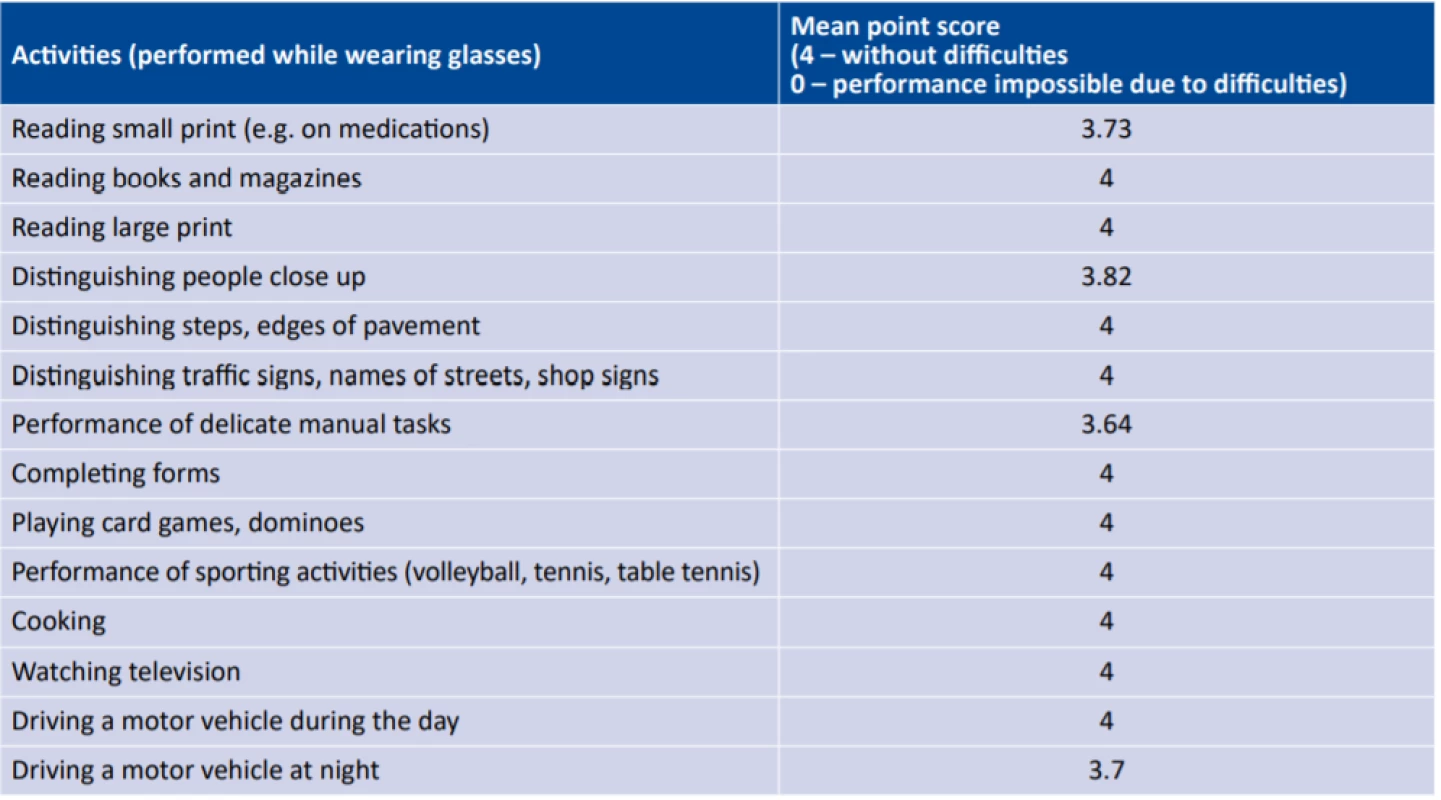
We also evaluated uncorrected (UCVA) and best corrected (BCVA) in the patients for near and distance vision. In UCVA we recorded a statistically significant improvement during the observation period. For distance vision mean preoperative uncorrected visual acuity (UCVA) was 0.51 (decimal value) ± 0.29, mean best corrected visual acuity (BCVA) was 0.95 ± 0.19. On the first day after surgery, mean UCVA for distance vision was 0.83 ± 0.16, mean BCVA was 0.94 ± 0.08. At a follow-up examination at an interval of 1 month after surgery, mean UCVA was 0.9 ± 0.13, mean BCVA was 0.99 ± 0.08. At a follow-up examination at an interval of 1 year or longer after surgery (on average 27 months), mean UCVA was 0.94 ± 0.10 and average BCVA 1.00 ± 0.09.
For near vision, mean preoperative UCVA was Jaeger (J.) no. 8.29 ± 4.93, mean BCVA was J. no. 1.34 ± 1.26. On the first day after surgery mean UCVA was J. no. 2.61 ± 2.13, mean BCVA was J. no. 1.19 ± 0.90. At a follow-up examination at an interval of 1 year or longer after surgery (on average 27 months), mean BCVA was J. no. 1.00 ± 0, mean BCVA was J. no. 1.00 ± 0.00 and UCVA binocularly to centre was 0.96 ± 0.19. We recorded a statistically significant improvement of uncorrected visual acuity for near and distance vision in comparison with the preoperative values at a time of 1 day (p < 0.0001) and 1 month (p < 0.0001) after surgery, after which the finding was stationary. The development of UCVA and BCVA at both distances is presented in graphs 1 and 2. At the time of 1 month after surgery, 100% of eyes attained monocular UCVA for distance vision of 0.7 (decimal value), and for near vision of J. no. 5 (Graphs 3 and 4).
1. Mean subjective distance visual acuity during the course of observation of UCVA (uncorrected visual acuity), BCVA (best corrected visual acuity, *on average 27 months (range 1 year or longer) 
2. Mean subjective near visual acuity during the course of observation of UCVA (uncorrected visual acuity), BCVA (best corrected visual acuity, *on average 27 months (range 1 year or longer) 
3. Cumulative distance UCVA (uncorrected visual acuity) 1 month after surgery 
4. Cumulative distance UCVA (uncorrected visual acuity) 1 month after surgery 
Preoperatively the value of subjective refraction for distance vision was +0.79 sph (D) ± 1.89 (within the range of -5 to +4) and -0.36 cyl (D) ± 0.41 (within the range of -1.5 to 0). At a follow-up examination at an interval of 1 year or more after surgery, the value of subjective refraction for distance vision was +0.24 sph (D) ± 0.41 (within the range of 0 to +1.25) and -0.16 cyl (D) ± 0.34 (within the range of -1 to 0). The value of subjective refraction for near vision was preoperatively +2.27 sph (D) ± 1.89 (within the range of -3.5 to +5.5) and -0.19 cyl (D) ± 0.40 (within the range of -1.25 to 0). At a follow-up examination at an interval of 1 year after surgery, the value of subjective refraction for near vision was 0.00 sph (D) ± 0 and 0 cyl (D) ± 0. The SE value at the time of 1 month after surgery was within the range of -0.5 to +0.5 D (Graph 5).
5. Intervals of SE for distance vision and percentage representation of eyes at the time of 1 month after surgery. SE (spherical equivalent), D (dioptre) 
6. Dependency of intraocular scattering on age 
DISCUSSION
The aim of the refractive operation PRELEX (presbyopic lens exchange) is to attain independence of glasses correction. Within the framework of implantation of multifocal intraocular lenses, however, adverse optic side effects may occur: the onset of positive and negative dysphotopsias (halo, glare or shadow in the temporal periphery of the visual field), reduction of contrast sensitivity and increased retinal light scattering, which may be one of the causes of occurrence of restricting glare [13]. In our study we focused on an evaluation of retinal light scattering following the implantation of the MF IOL PanOptix (Alcon Laboratories, Inc., Fort Worth, TX, USA).
The distribution of brightness on the retina at the moment when the eye is fixing on a point source is described by the point of spread function (PSF curve), and thus defines the quality of the retinal image. The central part of the curve is determined by visual acuity and the outer parts by retinal light scattering [18]. The point of spread function of the human eye therefore incorporates very different domains: a domain with high intensity and a small angle, referred to as the “PSF core”, and a domain with a wide angle and low intensity, usually referred to as “straylight”. The first domain can be evaluated with the aid of optical techniques. For the second domain psycho-physical techniques have been developed, in particular a comparative method which is available with the aid of measurement on a C-Quant instrument [14]. Intraocular scattering is influenced by several factors. It increases with the age of the patient, it is higher in patients with corneal edema or in contact lens wearers, and additionally in the case of presence of opacities of the lens or its posterior capsule and in glaucoma patients. It is also connected with pigmentation of the eye – in retinitis pigmentosa and Fuchs’ heterochromic iridocyclitis there is also greater light scattering [4]. At present retinal light scattering is being studied in connection with implantation of intraocular lenses within the framework of cataract surgery or refractive lensectomy. Light scattering following its passage through the optics of the intraocular lens may occur either through the influence of diffractive transitions in the case of diffractive intraocular lenses, or on the edge of the optics in the case of all intraocular lenses, including monofocal. Glistening also may be the cause of greater retinal light scattering [12].
Studies focusing on a comparison of retinal light scattering in the case of implantation of hydrophilic and hydrophobic intraocular lenses have produced interesting findings. Tang et al. recorded a significantly larger amount of dispersed light in the case of hydrophobic lenses [12]. The authors Guo et al. also conducted a comparison of hydrophobic and hydrophilic material. Similarly as in the previous study, in the case of hydrophilic artificial intraocular lenses, a significantly lower degree of light scattering was demonstrated than in the case of hydrophobic lenses [6].
The same issue was also the subject of research by Łabuz et al., who focused on a comparison of both materials in the case of multifocal intraocular lenses, and published an overview of the influence of multifocal intraocular lenses on postoperative intraocular scattering. It incorporated 10 studies, which stated the values of scattering obtained with the aid of a C-Quant instrument following uncomplicated implantation of 9 types of MF IOL. Hydrophilic MF IOLs manifested less intraocular scattering than hydrophobic IOLs by 0.08 log (s) (p = 0.001). IOLs with a filter of the blue part of the light spectrum showed lower values of intraocular scattering than standard MF IOLs by 0.04 log (s), which was not statistically significant (p = 0.32) [8]. Further studies have focused on the influence of the type of multifocal optics (diffractive, refractive) on values of intraocular scattering and on the occurrence of secondary optic phenomena (halo) obtained with the aid of halometry (Aston Halometer). In this study the authors evaluated the intraocular lenses Tecnis ZM900 (Advanced Medical Optics, Inc.), Lentis Mplus MF30 (Oculentis GmbH and Topcon Europe BV) and Softec-1 (Lenstec, Inc.). The authors did not record a significant difference in the value of retinal light scattering between the individual intraocular lenses by measurement with the aid of straylightmetry (C-Quant), nevertheless halometry identified clear differences in the values through the influence of different multifocal technologies of the optic parts of the intraocular lenses. The value of retinal light scattering therefore need not necessarily directly attest to the occurrence of secondary optic phenomena [1].
A comparison of intraocular scattering in multifocal and monofocal intraocular lenses was presented in a study by the authors de Vries et al. The average value of intraocular scattering at the time of 6 months after surgery was higher in patients with an AcrySof ReSTOR SA60D3 IOL than in patients with a monofocal AcoSof SA60AT IOL. The study produced the interesting finding that the values of intraocular scattering were significantly lower in eyes following implantation of both types of intraocular lenses than in subjects of a corresponding age from the normal population [15]. The study by Peng et al. also confirms higher intraocular dispersion following the implantation of a multifocal diffractive intraocular lens in comparison with a monofocal lens [11]. However, studies are available which do not demonstrate a statistically significant difference in the values of intraocular scattering in the case of a comparison of multifocal and monofocal intraocular lenses [2]. A comparison of different types of multifocal introacular lenses was presented in a study by the authors Ehmer et al., which also focused on a correlation between measurement of retinal light scattering with the aid of the C-Quant instrument (Oculus, Germany) and the results of subjective satisfaction. The authors compared three different multifocal intraocular lenses: AMO ReZoom (refractive design, n = 10), AMO ZM900 (diffractive design, n = 10) and Oculentis Mplus (rotationally-asymmetric design, n = 10). The functional results were evaluated at least 3 months after surgery, followed by measurement of light scattering and a subjective questionnaire. The authors did not demonstrate a correlation between the values of retinal light scattering and subjective photopic phenomena. Patients with the refractive type of optics of MF IOL recorded the highest percentage of occurrence of positive dysphotopsias (halo) [3]. Mueller-Schotte et al. in their study used the questionnaire NEI-VFQ-25 (National Eye Institute Visual Functioning Questionnaire, 25 questions) for evaluating subjective patient satisfaction, while the degree of intraocular scattering was measured in the same manner as in our study, using the instrument Oculus C-Quant. The authors did not find any correlation between quality of life and the degree of intraocular scattering [10]. This conclusion is supported also by the authors Michael et al. in their study from 2009 [9].
It is also stated in the literature that light scattering depends on the diameter of the pupil. The authors Tang et al. demonstrated greater light scattering in their cohort in the case of pupils in artificial mydriasis, although on a C-Quant instrument, with respect to the calculation of light scattering (proportion of dispersed and non-dispersed light, in which there is an increase in both types of light following dilation of the pupil), the values should be independent of pupil diameter. It is assumed that the increase in light scattering is due to exposure of the edge of the IOL, capsular opacities or also corneal edema [12].
CONCLUSION
Subjective patient satisfaction following implantation of multifocal intraocular lenses depends on the correct selection of the patient (patient motivation), correct choice of the type of intraocular lens, precise calculation, precise operation and if applicable also subsequent psychological support after surgery. Evaluation of retinal light scattering following the implantation of multifocal intraocular lenses is significant at the present time due to the construction of new designs of the optical parts of these implants. In our cohort we recorded a high degree of postoperative patient satisfaction in connection with independence of glasses correction together with a high degree of predictability and stability of the refractive result. In 82% of eyes the value of retinal light scattering was within the range of physiological values. We recorded a resulting value of retinal light dispersion outside of a physiological value in 6 eyes of 4 patients. An interesting finding was that in three patients from this group, even despite higher values of intraocular scattering, 100% subjective satisfaction with the postoperative result was recorded. Further studies will be required in order to clarify the relationships between retinal light scattering, the degree of occurrence of secondary optic phenomena, increased sensitivity to glare and subjective satisfaction following implants of multifocal intraocular lenses.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Markéta Středová
Oční klinika
Fakultní nemocnice Hradec Králové
Sokolská 581
50005 Hradec Králové
Received: 30. 9. 2019
Accepted: 21. 11. 2019
Available on-line: 20. 5. 2020
Sources
1. Buckhurst PJ., Naroo SA., Davies LN. et al.: Assessment of dysphotopsia in pseudophakic subjects with multifocal intraocular lenses. BMJ Open Ophth, 2017 : 1–7.
2. Cerviño A., Hosking SL., Montés-Micó R. et al.: Retinal straylight in patients with monofocal and multifocal intraocular lenses. J Cataract Refract Surg, 34; 2008 : 441–6.
3. Ehmer A., Rabsilber TM., Mannsfeld A. et al.: Influence of different multifocal intraocular lens concepts on retinal stray light parameters. Ophthalmologe, 108; 2011 : 952–6.
4. Franssen L., Coppens JE., van den Berg TJ. et al.: Compensation Comparison Method for assessment of Retinal Straylight. Investigative ophthalmology and Visual Science, 47; 2006 : 768–776.
5. Guo Y., Li J., Song H. et al.: Comparison of the Retinal Straylight in Pseudophakic Eyes with PMMA, Hydrophobic Acrylic and Hydrophilic Acrylic Spherical Intraocular Lens. Journal of Ophthalmology, 2014 : 1–6.
6. Iijima A., Shimizu K., Yamagishi M. et al.: Assessment of subjective intraocular forvard scattering and duality of vision after posterior chamer phakic intraocular lens with a central hole (Hole ICL) implantation. Acta Ophthalmol, 94; 2016: e716–e720.
7. Kyprianou G., Macháčková M., Feuermannová A. et al.: Subjektivní zrakové vnímání po laserové operaci myopie provedené na dvou typech laserů. Cesk Slov Oftalmol, 66; 2010 : 213–219
8. Łabuz G., Reus NJ., van den Berg TJ. et al.: Comparison of ocular straylight after implantation of multifocal intraocular lenses. J Cataract Refract Surg, 42; 2016 : 618–25.
9. Michael R., van Rijn LJ., van den Berg TJ. et al.: Assosiation of lens opacities, intraocular straylight, contrast sensitivity and visual acuity in European drivers. Acta Ophthalmologica, 87; 2009 : 666–671.
10. Mueller-Schotte S., van der Schouw YT., Schuurmans MJ.: Ocular Straylight: A determinant of Quality of Life in the Elderly? Gerontology and Geriatric Medicine, 2015 : 1–10.
11. Peng C., Zhao J., Ma L. et al.: Optical performance after bilateral implantation of apodized aspheric diffractive multifocal intraocular lenses with +3.00-D addition power. Acta Ophthalmol, 90; 2012: e586–e593.
12. Tang Y., Song H., Chen J. et al.: Comparison of pseudophakic retinal straylight in spherical/aspherical and hydrophobic/hydrophilic intraocular lens. Int J Ophthalmol, 8; 2015 : 1146–1150.
13. Van den Berg TJ.: On the relation between glare and straylight. Doc Ophthalmol, 78; 1991 : 177–81.
14. Van den Berg TJ., Franssen L., Coppens JE.: Straylight in the human eye: testing objectivity and optical character of the psychophysical measurement. Ophthalmic Physiol Opt, 29; 2009 : 345–50.
15. de Vries NE., Franssen L., Webers CA. et al.: Intraocular straylight after implantation of the multifocal AcrySof ReSTOR SA60D3 diffractive intraocular lens. J Cataract Refract Surg, 34; 2008 : 957–62.
16. Tajchmanová E.: Změna kontrastní citlivosti po operaci šedého zákalu, dostupné z URL: https://is.muni.cz/th/ixl1a/Zmena_kontrastni_citlivosti_po_operaci_sedeho_zakalu.txt
17. Vyjádření firmy Alcon stran pooperačních zrakových funkcí po implantaci čočky Acrysof IQ PanOptix, dostupné z URL: https://www.novartis.com/news/media-releases/novartis-international-ag-alcon-acrysofr-iq-panoptixr-trifocal-intraocular-lens-shows-superior-visual-performance-head-head-trial-post-cataract-surgery
18. Trendy v oční optice 2018, dostupné z URL: http://www.s-presspublishing.cz/archiv/201802_trendy.pdf
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2019 Issue 6-
All articles in this issue
- 100 let od narození prof. MUDr. Heleny Lomíčkové, DrSc. 40 let oční kliniky dětí a dospělých v Motole
- OCENĚNÍ ČLS JEP
- CENA PREZIDENTA ČLK
- Innovative strategies for treating retinal diseases
- Assessment of the efficacy of photodynamic therapy in patients with chronic central serous chorioretinopathy
- Sensitivity and specificity in methods for examination of the eye astigmatism
- Evaluation of retinal light scattering, visual acuity, refraction and subjective satisfaction in patients after Acrysof IQ PanOptix intraocular lens implantation
- Eyelid edema as a first sign of lymphoma
- Ocular Symptoms of Rosacea
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ocular Symptoms of Rosacea
- Eyelid edema as a first sign of lymphoma
- Assessment of the efficacy of photodynamic therapy in patients with chronic central serous chorioretinopathy
- Innovative strategies for treating retinal diseases
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

