-
Medical journals
- Career
Reconstruction of deep head burn with a free flap - a case study
Authors: P. Šín 1,2; A. Hokynková 1,2; Pavel Rotschein 1,2; Y. Kaloudová 1; B. Lipový 1,2,3
Authors‘ workplace: University Hospital Brno, Department of Burns and Plastic Surgery, Brno, Czech Republic 1; Masaryk University, Faculty of Medicine, Brno, Czech Republic 2; Brno University of Technology, CEITEC – Central European Institute of Technology, Brno, Czech Republic 3
Published in: ACTA CHIRURGIAE PLASTICAE, 61, 1-4, 2019, pp. 32-35
INTRODUCTION
The reconstruction of lost tissue on the head caused by third degree burn trauma represents a great challenge in plastic surgery. The choice of correct method for closure of the defect is essential while bearing in mind the functional and aesthetic outcome1. The reconstructive options are aggravated by the general hyper-coagulation state in burn patients, high risk of wound infection and fragility of tissues surrounding the burn defect2,3. The decision of choosing the correct method starts with the easiest options and the reconstructive ladder should be followed1. In third degree burns where there is an exposed bone, vessel, nerve or tendon with no tendency of healing, a microsurgical intervention using free flap transfer surgery needs to be considered4. The condition of the surrounding tissue is crucial for choosing between a locoregional and free flap surgery.
CASE REPORT
We present a case of a 62-year-old woman who suffered severe thermal burns on the head, neck and chest from a house fire in June 2015. The patient was intubated at the site and transported to the University Hospital Brno to the Department of Burns and Plastic Surgery. The primary evaluation and treatment of burns was done at the OR (Operating Room). The depth of the burns reached from second degree burns on the chest and neck to third degree burns on the head. The total of 26% TBSA (Total Body Surface Area) was affected. The inhalation injury and ocular burn injury were associated with the burn trauma. She was hospitalized at the ICU (Intensive Care Unit), where the focus was concentrated on the prevention of burn shock, monitoring of vital functions and fiberoptic bronchoscopy with bronchoalveolar lavage for microbiological examination. She was extubated 15 days after admission. During the next three months she underwent 31 surgical interventions consisting of chemical and surgical necrectomy, autologous split-thickness skin graft (STSG) transplantation and reconstructive blepharoplasty surgery. The deepest burn defect was localized on patient’s forehead and reached behind the hairline. It showed no signs of healing after three months of standard surgical treatment including trephination of the bone. The defect was T shaped, approximately 100 x 80 mm wide with exposed bone at the bottom with no pericranium (Figure 1). We decided to use a free flap transfer as a method of primary closure of the burn defect (Figure 2, 3). Considering the size and a flat profile of the defect, the serratus anterior muscle flap was chosen with the temporal superficial vessels as the recipients (Figure 4). The surgery was done 96 days after the injury. Since the size discrepancy between the vessels was less than 2 : 1, end to end anastomosis was performed. The flap surface was temporarily covered with synthetic wound dressing and one week after the transfer it was definitely covered with autologous STSG. The patient was discharged from the hospital 118 days after the injury and 22 days after the free flap transfer. Long-term follow-up was established (Figure 5, 6).
1. The deep burn defect on the head before reconstruction 
2. Marking the size of the serratus anterior muscle 
3. Dissection of the serratus anterior muscle 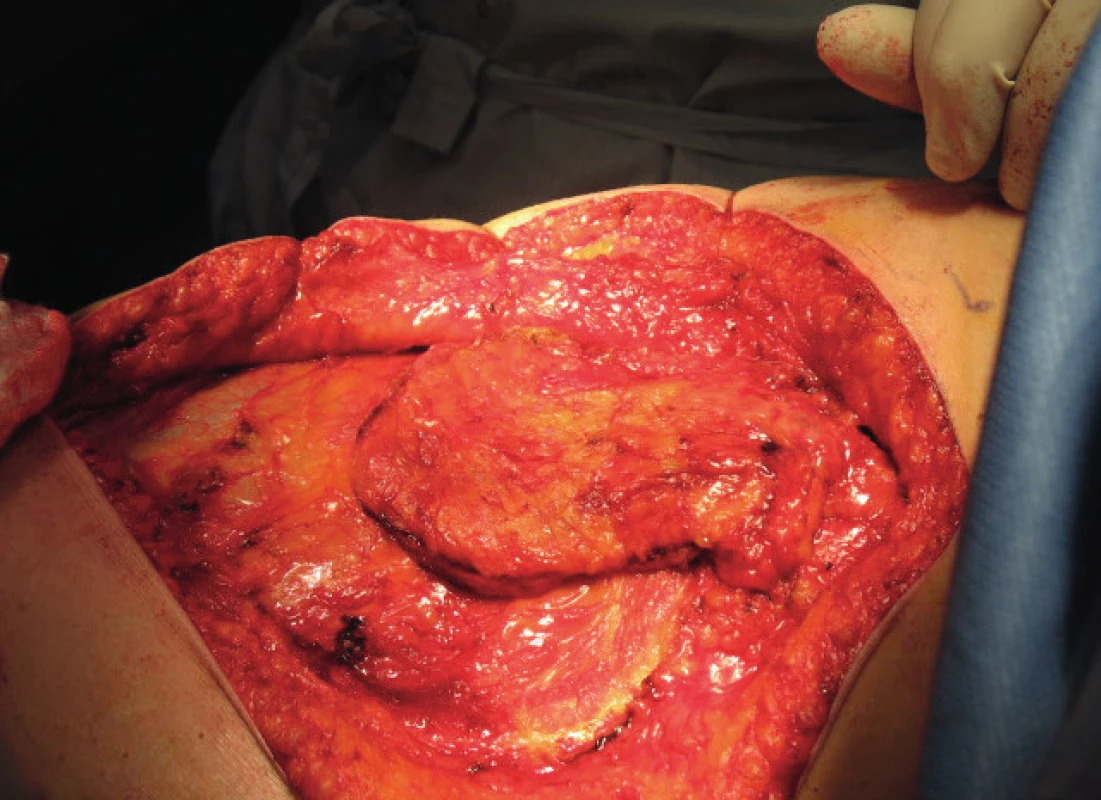
4. Closure of the defect with free flap transfer using the serratus anterior muscle 
5. One year after the surgery – side view 
6. One year after the surgery – front view 
DISCUSSION
Primary closure of deep defects of the face and scalp represent a big challenge for plastic surgeons. The reconstructive ladder needs to be followed using the easiest methods first1. However, the reconstruction of scalp defects with exposed bone may be complicated due to the lack of granulation tissue and by the state of surrounding tissue2. In burn patients, the exposed bone is also a predisposition for burn-related infection5. In our case, chemical necrectomy using benzoic acid6 removed burn tissues while leaving exposed bone. The absence of granulation tissue on the bone even after trephination excluded the autologous STSG transplantation. The next option in the reconstructive ladder were locoregional flaps, which were widely used before microsurgery was introduced in 1960s7. The use of locoregional flaps depends on the state of the surrounding tissue. In our case the surrounding tissues were scarred after the thermal injury and partially covered by autologous STSG, which excluded this method. Following the reconstructive ladder, we chose to cover the defect with a free flap transfer4. We had several options of a free flap transfer. The fasciocutaneous free flaps in reconstruction of this kind of defects can be used, but due to predisposition to site infection and possible microbial colonization of the defect we decided to use a muscular free flap transfer. The muscular flap provided well vascularized tissue reaching to all borders of the reconstructed defect. In our unit we usually use the musculus latissimus dorsi flap for reconstruction of large defects thanks to its long pedicle, minimal morbidity of the donor site and acceptable deficit of its absent function. However, considering the aesthetic outcome and the flat profile of the defect localized on patient’s forehead, we assumed there would be abundant tissue in the vertical axis of the head if we have chosen the musculus latissimus dorsi flap. Other flaps such as bipedicled deep inferior epigastric perforator flap have been ruled out because of previous surgeries of the abdomen. The size of the defect was also too wide for flaps such as the gracilis muscle flap. For these reasons, we decided to choose the serratus anterior muscle flap for the closure of the defect. Its main advantages were its thin profile and pliability of the muscle mass. When choosing the recipient vessels, we had to respect the area of burn trauma, since it was reaching to the parietal and temporal regions on both sides. The left temporal region was primary a third degree burn and after surgical treatment it was covered with autologous STSG. The right temporal region was primarily a second degree burn treated conservatively, which allowed us to choose the superficial temporal vessels as the recipients with end to end anastomosis. The surgery was done with standard microsurgical procedure without any complications. The flap was temporarily covered with a synthetic wound dressing, which was permeable from the inside and not from the outside. It also allowed to examine the pulsation of microanastomosis by Doppler ultrasound probe every hour. After one week the flap was covered by autologous STSG with graft meshing in a ratio of 1 : 1.5.
In general, the closure of the defects with free flap transfer is endangered by vascular thrombosis8. Burn patients have an increased risk of thrombosis due to their hyper-coagulation state, fragility of vessels and inclination to vessel spasms3. We chose the superficial temporal vessels as in the recipients with the risk that their inner layer intima may have been harmed by the second degree burn of the skin. However, in our case we did not observe any complications in the microanastomosis after the surgery. The donor site required surgical intervention for bleeding from the residual muscle mass.
We did not observe any complication in the flap site such as local infection, dehiscence of the wound or possible infectious complications such as sinusitis or meningitis. We also did not observe any other complications during the subsequent one year of follow up, which included observation for scar contracture, spontaneous de-epithelialization of autologous STSG on the flap surface, fistulas or any other complication in the flap site or in the donor site.
The reconstruction of deep burn defects on the head with exposed skull is problematic and interdisciplinary approach is crucial. The primary intensive care is needed for stabilization of the burn shock including targeted antibiotics therapy and correction of the nutritional status of the patient. When standard surgical techniques cannot be used for closing the defect, the reconstructive microsurgery is considered with choosing the correct method of closure. After successful closure of the defect, a long-term follow-up with surveillance for possible complications and evaluation of the maturation and quality of the scars is needed.
CONCLUSION
An extensive head burn trauma represents a big challenge for plastic surgeons. A patient with a large defect on the head with exposed bone is in a great threat of wound infection despite targeted antibiotic therapy. An early closure of the defect is indicated. Usually the burn treatment involves necrectomy and reconstruction with STSG even at the cost of scars. The free flap transfer is not a method of choice and it is rarely used in burn surgery for primary closure. It can be used when all the methods listed in the reconstructive ladder cannot be implemented either due to the size of the defect or due to the condition of the surrounding tissues. Muscular free flap provides well vascularized and pliable tissue. In our case the free flap transfer was used for primary closure of the burn defect after the standard burn therapy has failed. The closure was performed in about three months from the injury, which can be considered as an early surgery since the patient underwent many surgical interventions and suffered from an inhalation injury. Interdisciplinary approach in this kind of trauma is essential with a long-term follow-up of the patient.
Conflict of interest: The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
Ethical requirements: The authors declare that the study was conducted in accordance with Helsinki Declaration.
Alica Hokynková, MD
Department of Burns and Plastic Surgery
University Hospital Brno
Jihlavská 20
625 00 Brno
Czech Republic
E-mail: hokynkova.alica@fnbrno.cz
Sources
1. Sokoya M, Inman J, Ducic Y. Scalp and Forehead Reconstruction. Semin Plast Surg. 2018, 32 : 90–4.
2. Bizhko IP, Slesarenko SV. Operative treatment of deep burns of the scalp and skull. Burns. 1992, 18 : 220–3.
3. Herndon D. Total burn care. 5th ed. Edinburgh: Elsevier; 2018. Chapter 22, Hematology, Hemostasis, Thromboprophylaxis, and Transfusion Medicine in Burn Patients; p. 236–47.
4. Lorenzi F, Hulst R, Boeckx W. Free flaps in burn reconstruction. Burns. 2001, 27 : 603–612.
5. Jeyakumar P, Hussain AT, Ahamed AR. Reconstruction of Extensive Post-Electric Burn Scalp Defects With Exposed Bones – A Study of 12 Cases. Ann Plast Surg. 2018, 81 :39–44.
6. Jelínková Z, Řihová H et al. Our experience with the use of 40% benzoic acid for necrectomy in deep burns. Acta chirurgiae plasticae. 2017, 59 : 5–10.
7. Susumu T. History of microsurgery. Plast Reconstr Surg. 2009, 124 : 282–94.
8. Seo MH, Kim SM, Huan F. et al. Analysis of Microvascular Free Flap Failure Focusing on the Microscopic Findings of the Anastomosed Vessels. J Craniofac Surg. 2015, 26 : 2047–51.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2019 Issue 1-4-
All articles in this issue
- České souhrny
- Bilobed flap in facial reconstruction
- Free-flap monitoring: review and clinical approach
- Giant basal carcinoma on the forehead and why should prevent them - case report
- Use of medial femoral condyle flap and anterolateral thigh free flap in proxymal tibial posttraumatic non-union with multiple anastomosis - case report
- The impact of aesthetic plastic surgery on body image, body satifaction and self-esteem
- Reconstruction of deep head burn with a free flap - a case study
- Acknowledgemets to reviewers
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- The impact of aesthetic plastic surgery on body image, body satifaction and self-esteem
- Free-flap monitoring: review and clinical approach
- Bilobed flap in facial reconstruction
- Use of medial femoral condyle flap and anterolateral thigh free flap in proxymal tibial posttraumatic non-union with multiple anastomosis - case report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

