-
Medical journals
- Career
CONGENITAL HAND DEFORMITIES – A CLINICAL REPORT OF 191 PATIENTS
Authors: A. K. Yesilada; K. Z. Sevim; D. O. Sucu; L. Kilinc
Authors‘ workplace: Sisli Etfal Research and Training Hospital, Department of Plastic and Reconstructive Surgery, Istanbul, Turkey
Published in: ACTA CHIRURGIAE PLASTICAE, 55, 1, 2013, pp. 10-15
INTRODUCTION
Congenital deformities of the hand are rarely seen in approximately 23 of 10.000 total births (1). When this is compared with the incidence of the children born with cleft lip and palate, which is 14, out of 10.000 total births, one may understand the impact of this spectrum of anomalies on people’s lives. In the etiology of congenital deformities of the hand, hereditary factors or exogenic factors (e.g drug consumption during pregnancy) may play a role. For the majority however, the etiology remains unknown. Following antenatal or postnatal diagnosis, it is crucial to carefully plan the reconstruction protocol in such patients, since functional and sensate hands are important in a child’s normal developmental process including feeding, playing, dressing, toilet needs and writing, along with child’s normal psychological development. Bimanual grasp is achieved by the age of 9 months and three-digit pinch is learned between 1 and 2 years of age (2). Ideally, the reconstruction should be completed by school age to allow easier social adjustment. Some operations however, need to be undertaken in the first few months of life, e.g constriction ring syndrome, floating polydactyly of the 5th finger or the thumb, and some forms of syndactyly. It is important that the child is at an age where he/she can tolerate concomittant therapy, stretching and splintage in order to achieve maximal function and cosmesis. The currently used classification of anomalies of the upper extremity is based on that of Swanson, modified by the congenital malformations committee of the International federation of Societies for the Surgery of the Hand (IFSSH) in 1983 (2). However, this classification system has been critisized for its inherent limitations, because it attempts to incorporate etiology into morphologically-based classification and it is difficult to classify complex cases such as cleft hand or symbrachydactyly. Manske and Oberg, as well as Schoonhoven et al., recently proposed several modifications to the classification scheme, based on the clinical experience and developmental biology (3). There are also many classifications of subtypes of the hand anomalies (e.g. Blauth, Wassel, Buck-Gramcko). Such classifications are handy for epidemiology purposes, however they are of little practical value in the routine management of congenital hand malformations. Each case should be analysed by itsself, the combination of malformations described, and treatment planned based on this analysis. In the following study, the manifold entities accounting for congenital deformities of the hand are described synoptically with their clinical characteristics, gender distributions, laterality, associated non-hand anomalies and surgical strategies, in a large hospital over a period of 14 years. The treatment options and complications are briefly discussed. This article intends to emphasize interdisciplinary cooperation of genetic counselling, physiotherapist, hand surgeon with this group of dedicated patient and parent collective.
PATIENTS AND METHOD
We obtained mandatory approval for the study from the regional ethics committe review board. In a retrospective analysis, the clinical database of congenital hand operations were analyzed during a 14 year period (1998–2012). Among 191 patients, 223 congenital deformities were depicted and these patients were classified in the majority of the cases, according to the IFSSH, modified Swanson guidelines. The medical records of 191 patients were collected. For each entity, the time of admission to the hand clinic, presence of associated non-hand anomalies were considered. Along with those, the patient’s age at the time of the operation, surgical modality and frequency of complications and reoperations were also recorded. We decided to exclude conditions such as congenital tumors (including hemangiomas, lymphangiomas, etc.), epidermolysis bullosa, ichtyosis, arthrogryposis multiplex congenita, from the diagnosis list because we were uncertain how to present accurate treatment techniques regarding these diagnosis. Individuals with a bilateral anomaly belonging to the same IFSSH category were counted as one main anomaly.
RESULTS
A total of 191 patients suffering from congenital disorders of the hand were surgically treated during the study period. The age of patients presented to the clinic and the patient’s age at the time of the operation, number of reoperations and mostly seen complications are depicted in Charts 1, 2, 3. Between years 1998 through 2006, the ratio of female/male is found to be 1 : 1.1, however between 2007 through to 2012, the congenital hand anomalies are encountered twice as often in males. The mean value for the timing of the surgical treatment is found to be 5.2 years. The list of associated non-hand anomalies is shown in Table 1.
Chart 1. Distribution of preaxial and postaxial duplication 
Chart 2. Distribution of syndactyly patients 
Chart 3. Frequency of congenital hand anomalies 
1. Frequency of associated non-hand anomalies 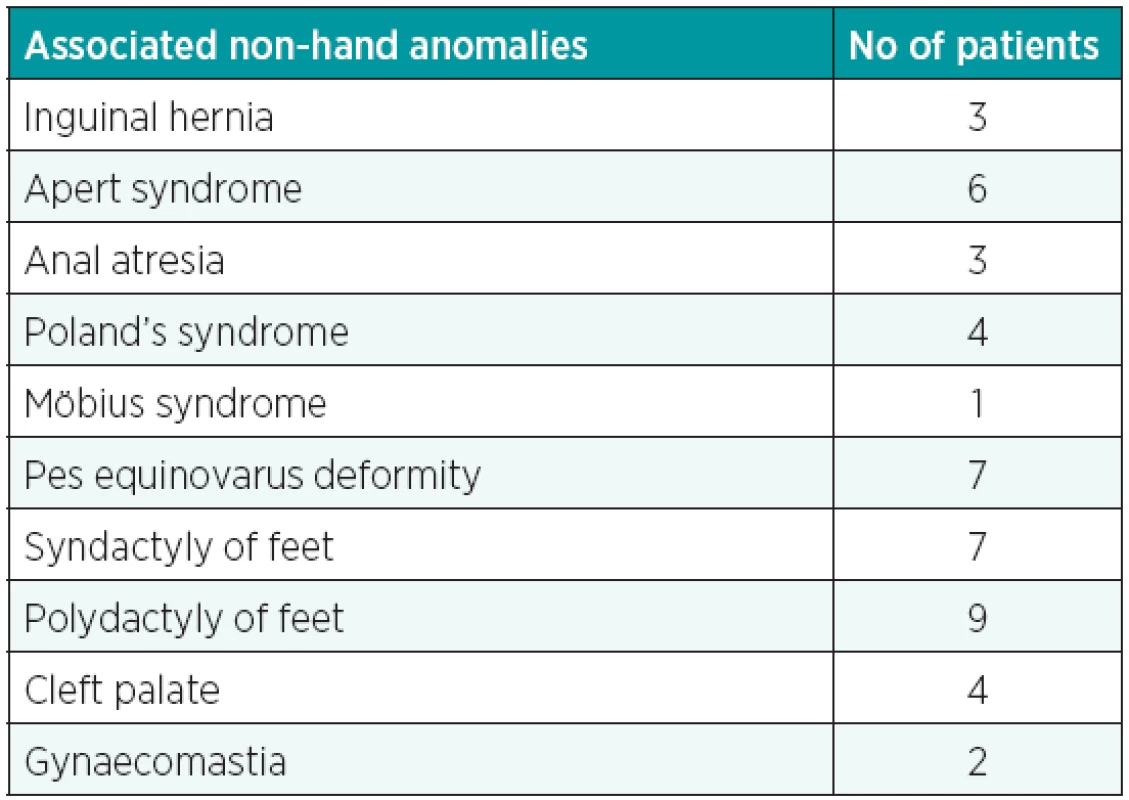
Clinical findings and the choice of treatment methods were as follows for the different entities:
Syndactyly
In all 97 syndactyly patients, 25 patients had bilateral involvement. The gender distribution was 60 male and 27 female patients. The age ranged from 4 months to 25 years (average 4 years). Twenty-one children had associated malformations from other than the hand parts of the musculoskeletal system, as well as from other systems. The most commonly involved web was the third web space. Thirty-three were complete syndactilies, whereas in 18 webs the syndactyly was complex. At the time of surgery, the majority of the patients (75 patients) were in the preschool age (5 years). Ten of the patients were less than 1 year old and the rest were adults when they presented to the clinic. During surgery, we preferred using the dorsal rectangular flap to create the web space and skin grafts in addition to Brunner incisions were used to cover the skin defects after the release of syndactyly. Full thickness skin grafts were always the choice for treatment. In patients where the nail is common, 2 triangular opposed flaps from the common pulp of the involved digit were created and transposed. Keloid formation was observed in 1 patient.
Polydactyly
Diagnosis of polydactyly was made clinically in 66 patients. The extent of bone and soft-tissue involvement was assessed radiologically. Preaxial polydactyly cases including thumb duplications were observed in 41 patients and postaxial polydactyly cases were observed in 25 patients. Thirty patients in the preaxial polydactyly group presented with thumb duplication. Wassel type 4 deformity was the most commonly observed (n=21). In 3 patients, Wassel type 7 (triphalangeal thumb) deformity was observed. Excision of extra phalanx and arthrodesis of IP joint was performed. Six patients were treated with sharing the equal halves (Bilhaut-Cloquet procedure) to reconstruct the thumbs. Reconstruction of the collateral ligaments was performed to provide stability. The operations were eventless and in 2 patients, more than one operation was necessary to sufficiently correct the axis of the finger ray (Fig. 1–5).
Fig. 1. Polysyndactyly in a 4 year old male 
Fig. 2. Preoperative radiography of the polysyndactyly patient 
Fig. 3. Postoperative view of the polysyndactyly patient 
Fig. 4. Thumb duplication Wassel type 4 in a 7 year old male 
Fig. 5. Postoperative view of thumb duplication patient 
Constriction ring syndrome
Seven patients were treated for ring constrictions. Majority of the patients were operated below the age of 1 year. Surgical release was done by planning multiple Z-plasties, which often had to be repeated as the finger grew.
Macrodactyly
Diagnosis of macrodactyly was made clinically in 10 patients. Bone and soft tissue involvement was graded radiologically. Majority of the cases were unilateral and the index finger was the most commonly involved. Three of the macrodactylies were associated with hypertrophy of the median, ulnar or digital nerve, which in one patient presented with symptoms of trigger wrist syndrome and compression neuropathy. Surgical treatment steps included debulking the digit, decompression of the nerves. In 1 patient, amputation at the MCP level had to be performed. Wound infection occurred in 1 patient. In 3 patients, more than one operative intervention was necessary to debulk the digit and to reduce bone and soft tissue masses during the growth of the child.
Camptodactyly
In 8 patients, camptodactyly diagnosis was made clinically. In 2 patients, the cases were bilateral. All of the deformities involved the fifth digit. The average age that patients presented with camptodactyly symptoms was 7 years. Release of any structures (including skin, fascial ligaments or tendons) is combined with dynamic splinting and rigorous physiotherapy in such patients. There were no surgical complications.
Clinodactyly
Five patients were operated because of clinodactyly. All of them involved the fifth digit. The digits showed lateral angulations of the finger rays exceeding more than 40°. Closed wedge osteotomy was performed in all patients and a “delta phalanx” resected in 1 patient. The realignment of the affected digit was supported by K-wiring for 4 weeks. One complication was fund (wound infection). No re-operations were required.
Thumb hypoplasia
In 3 patients with thumb hypoplasia, diagnosis and classification according to Blauth was established clinically. Their deficiencies were Grade 3B and 5, according to Blauth. Phalanx transfer, first web release and opponensplasty were performed in 1 patient with reconstructible thumb hypoplasia and total thumb absence was treated by ablation and pollicization in 2 patients. In these patients, more than one operation had to be performed (Fig. 6–9).
Fig. 6. Grade 3 thumb hypoplasia in a 10 year old male 
Fig. 7. Postoperative view after pollicization 
Fig. 8. Postoperative view of grasping function after pollicization 
Fig. 9. Postoperative view of pinch function after pollicization 
Cleft hand
The diagnosis of cleft hand was established clinically in 5 patients. Two patients were also children, born with Apert’s syndrome and were classified according to the Upton classification. The main goal in cleft hand patients was giving the hand a tripod pinch by separating the digits and thumbs, mobilization of the fifth ray, realignment of the thumb and secondary revisions.
DISCUSSION
About 1 in 600 newborns present with different forms of upper limb abnormality. The hand surgeon’s aim is to achieve the maximum upper limb function possible for each patient. Functional recovery as well as aesthetic appearance following reconstruction of congenital hand differences are almost equally important in a child’s well-being. Children with congenital hand anomalies must be thoroughly assessed since the anomaly may well be part of a wider anomaly. For instance, the VATER association (vertebral, anal, tracheo-oesophageal, radial club hand), Holt-Oram syndrome (cardiac septal defect), TAR syndrome (radial club hand and thrombocytopenia) and Apert’s syndrome (craniofacial anomalies and mitten hand) (6,7). Timing of x-rays and scans are also a topic of controversy. Complicated and complex anomalies concerning the bone, arise the need for earlier surgery, however the high dose of radiation is a major draw-back and special attention must be given to differentiate the proper indication of X-rays. Before starting the treatment of a congenital hand anomaly, one should have a flexible elbow and adequate shoulder motion. A mobile and sensate hand is also paramount. The functional aims are preserving the prehensile ability with an opposable thumb by creating thumb to two finger tripod pinch or key pinch and restoring individual digit function with sideways movement by preserving non-prehensile function (finger grip, elbow movement, palm as sensate paddle with wrist movement). In our clinic, we retrospectively analyzed the 191 patients and classified them with the Swanson classification, modified by IFSSH. Failure of formation of parts, transverse and longitudinal arrest were not treated in this series of patients.
Syndactyly resulting from failure of digital separation is one of the most common congenital hand malformations in our series, which corresponds with 1 : 2000 in literature (8,9). Syndactyly may ocur as an isolated deformity or may be associated with other conditions like acrosyndactyly, camptodactyly, clinodactyly, Apert’s syndrome or Poland’s sequence. There may be a positive family history in as many as 10–40% of the cases. Border digits (thumb/index finger and ring/little finger) are separated earlier than other syndactyly patients (in the first 6 months). Basic principles of our surgical procedure is as follows: One neighbouring web is operated in each session, the web is created by a rectangular or triangular dorsal flap as a rule. In the literature, the incidence of web creep is between 2% and 20% after syndactyly releases. In our patients, 15% were reoperated due to web creep. The less satisfactory results are obtained in our series in complex, complicated syndactyly cases. The main reason is the rotational and angular deformities of the digits after the operation. Correction of the “common nail deformity” in syndactyly is an important problem to be solved in syndactyly. In the past, skin graft from the pulp of the great toe, rectangular or triangular local flaps have been used. We prefer utilizing triangular local flaps to correct the deformity. Syndactylies are sometimes seen together with polydactilies. In complex syndactyly, joint stability or skeletal deformities can ocur. Arthrodesis may be considered to solve the joint instability problem, once the child has reached skeletal maturity.
Clinodactyly or angulation of digits in the radioulnar plane distal to the metacarpophalangeal joint is clinically significant when the inclination is between 10–45°. In correspondence with literature, it was mostly observed in the little finger of individuals. Moderate clinodactyly usually doesn’t require any treatment. In some cases, a trapezoidal bone is intercalated, in the affected ray, which is called the ”delta phalanx”. Realignment of the longitudinal axis may be achieved with osteotomy. We performed wedge osteotomies and fixed the digits with K-wire for 4 weeks. No complications were encountered.
Polydactyly can be located on the radial (preaxial) and ulnar (postaxial) side of the limb. Preaxial polydactyly, in the form of a duplicated thumb is seen 1 in 300 live births. Apart from the triphalangeal thumb, which is associated with autosomal dominat inheritance, the majority of duplicated thumbs are sporadic and unilateral. Wassel classification system is used for classifying thumb duplications and as seen in our series of patients, Wassel type 4 is most commonly encountered. Patients with duplications are mostly operated for cosmetic reasons except triphalangeal thumbs. In triphalangeal thumbs, reconstructing a functional thumb with pinch activity is essential and is performed during the first 2 years of life. In most polydactylies, the digit on the radial side, or the digit that doesn’t have adequate contact surface with the joint is excised. Collateral ligament reconstruction is necessary and the angular deformity of the remaining digit is corrected by wedge osteotomies or releasing the abnormal insertions of the thenar muscles and extrinsic tendons. Bilhaut-Cloquet operation is also commonly preferred, splitting the two thumbs longitudinally.
Hypoplastic thumb can be seen alone or in combination with any radial deficiency. This deformity may be associated with syndromes as mentioned before in the text (10, 11). The goal of treatment for hypoplastic thumb is to reconstruct the thumb, to provide the child with a mobile and stable thumb, adequate to perform the pinch and grip activities. The surgery should be done earlier in this patient group to achieve normal prehensile movements. In the 3 patients that we treated, our preferred method of treatment was phalangeal bone transfer and first web release, along with opponensplasty in 1 patient with a stable CMC joint. Also in 2 patients with unstable CMC joints, index pollicization and opponensplasty procedures were performed. These patients were operated more than once, however functional and aesthetically pleasing results were obtained. For opponensplasty, abductor digiti minimi (Huber procedure) was preferred and pinch power, dexterity and appearance significantly improved.
Macrodactyly is seen in 0.9% of live births and it is sometimes associated with neurofibromatosis. Most cases affect a single digit or a region innervated by a single nerve (12, 13). The patients in our series as in literature, were operated several times because it is difficult to completely correct the deformity in one session. Ray amputation was performed in one patient. Decompression of the nerves (median, ulnar, digital) is sometimes required as we did in 1 patient with severe carpal tunnel syndrome.
Constriction ring syndrome. Also called “amniotic band syndrome”, these deformities are released by multiple Z-plasties, which often have to be repeated as the child grows (14).
Camptodactyly is a painless flexion deformity and corrective surgery is only performed in a digit where more than 40° flexion contracture is seen. The long-term results of correcting this deformity are not very satisfactory, especially in younger children (15).
CONCLUSION
Every parent desires a perfect child and it is extremely important in patients with congenital hand deformities, to make the parents realize the extent of the malformation, the possible pitfalls of the operations and predict the future outcomes from the beginning. In a child with a cleft hand deformity, a hand reconstructed with a normal prehensile ability may seem satisfying for the surgeon, but the parents may be upset by the hand if they are not informed about the limitations of reconstruction. Each patient is unique and the ability of the patient and the parents to adjust the therapies vary among individuals. Our main goal is achieving a functional and somewhat acceptable cosmetic apperance. In this report we tried to summarize our approach to selected cases of congenital hand anomalies seen in our clinics.
Address for correspondence:
Kamuran Zeynep Sevim, M.D.
Sisli Etfal Research and Training Hospital, Department of Plastic and Reconstructive Surgery
Şişli Etfal Hastanesi 7. Kat Plastik Cerrahi Kliniği Şişli
Istanbul, Turkey
E-mail: kzeynep.sevim@gmail.com
Sources
1. Bates SJ., Hansen SL., Jones NF. Reconstruction of Congenital Differences of the Hand. Plast Reconstr. Surg., 124 (Suppl.), 2009, 128e–143e.
2. Swanson AB. A Classification for congenital limb malformation. J. Hand Surg., 1, 1976, p. 8–22.
3. Oberg C., Feenstra JM., Manske PR., Tonkin MA. Developmental biology and classification of congenital anomalies of the hand and upper extremity. J Hand Surg., 35 A, 2010, p. 2066–2076.
4. Gulgonen A., Gudemez E. Toe-to-hand transfers: More than twenty years follow-up of five post-traumatic cases. J. Hand Surg. (Br.), 31, 2005, p. 2–8.
5. Flatt AE. The care of congenital hand anomalies. 2nd ed. St. Louis: Quality Medical Publishing. 1994, p. 366–410.
6. Muzaffar AR., Rafolds F., Masson J., Ezaki M., Carter PR. Keloid formation after syndactyly reconstruction: Associated conditions, prevalance, and preliminary report of a treatment method. J. Hand Surg., 29 A, 2004, p. 201–208.
7. Schmelzer-Schmied N., Jung M., Ludwig K. Radiological and clinical outcome after operations in patients with congenital deficiencies of the wrist and hand. Eur. J. Radiol., 2010, doi: 10.1016/j.ejrad.2010.10.023.
8. Watson S. The principles of management of congenital anomalies of the upper limb. Arch. Dis. Child., 83, 2000, p. 10–17.
9. Green DP., Hotchkiss RN., Pederson WC., eds. Green’s operative hand surgery, Vol. 1, 4th edition. London: Churchill Livingstone, 1999.
10. Riley SA., Burgess RC. Thumb Hypoplasia. J. Hand Surg., 34 A, 2009, p. 1564–1573.
11. Oda T., Pushman AG., Chung KC. Treatment of common congenital hand conditions. Plast. Reconstr. Surg., 126, 2010, p. 121e–133e.
12. Ekblom AG., Laurell T., Arner M. Epidemiology of congenital upper limb anomalies in 562 children born in 1997 to 2007: A total population study from Stockholm, Sweden. J. Hand Surg., 35 A, 2010, p. 1742–1754.
13. Al-Qattan MM., Yang Y., Kozin SH. Embryology of the upper limb. J. Hand Surg., 34 A, 2009, p. 1340–1350.
14. Yuceturk A. Doğumsal el anomalileri. Turkiye Klinikleri J. Surg. Med .Sci., 2(17), 2006, p. 105–113.
15. Buck-Gramcko D. Congenital disorders: Radial and ulnar club hand. In: Berger RA, Weiss A-PC., eds. Hand surgery. 1st ed. Philadelphia: Lippincott Williams & Wilkins; 2004. p. 1453–1464.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2013 Issue 1-
All articles in this issue
- CONGENITAL HAND DEFORMITIES – A CLINICAL REPORT OF 191 PATIENTS
- “DOWNWARD STEPS TECHNIQUE” WITH CO2 ULTRAPULSED LASER FOR THE TREATMENT OF RHINOPHYMA: OUR PROTOCOL
- TREATMENT OF STAGES III−IV OF THE DUPUYTREN’S DISEASE USING A PERSONAL APPROACH: PERCUTANEOUS NEEDLE FASCIOTOMY (PNF) AND MINIMAL INVASIVE SELECTIVE APONEURECTOMY
- COMBINED TRIGGERING AT THE WRIST AND FINGERS AND SEVERE CARPAL TUNNEL SYNDROME CAUSED BY MACRODYSTROPHIA LIPOMATOSA. CASE REPORT AND REVIEW OF LITERATURE
- CHANGES IN DONOR SITE SELECTION IN LOWER LIMB FREE FLAP RECONSTRUCTIONS BY INTEGRATING DUPLEX ULTRASONOGRAPHY IN THE PREOPERATIVE DESIGN
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- TREATMENT OF STAGES III−IV OF THE DUPUYTREN’S DISEASE USING A PERSONAL APPROACH: PERCUTANEOUS NEEDLE FASCIOTOMY (PNF) AND MINIMAL INVASIVE SELECTIVE APONEURECTOMY
- CONGENITAL HAND DEFORMITIES – A CLINICAL REPORT OF 191 PATIENTS
- “DOWNWARD STEPS TECHNIQUE” WITH CO2 ULTRAPULSED LASER FOR THE TREATMENT OF RHINOPHYMA: OUR PROTOCOL
- COMBINED TRIGGERING AT THE WRIST AND FINGERS AND SEVERE CARPAL TUNNEL SYNDROME CAUSED BY MACRODYSTROPHIA LIPOMATOSA. CASE REPORT AND REVIEW OF LITERATURE
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career
