-
Medical journals
- Career
Reconstruction of the Hand in Apert Syndrome: Two Case Reports and a Literature Review of Updated Strategies for Diagnosis and Management
Authors: Z. Roje 1; Ž. Roje 2; M. Ninković 3; S. Dokuzović 4; J. Varvodić 5
Authors‘ workplace: Division of Plastic Surgery and Burns, Department of Surgery, University Hospital Center Split School of Medicine, Split, Croatia 1; Department of Surgery, University Hospital Dubrava, University of Zagreb School of Medicine, Zagreb, Croatia 2; Department of Plastic, Reconstructive and Aesthetic Surgery, Bogenhause, Munich, Germany 3; Department of Orthopaedic Surgery, University Hospital Dubrava, Zagreb, Croatia, and 4; Department of Surgery, University Hospital Dubrava, Zagreb, Croatia 5
Published in: ACTA CHIRURGIAE PLASTICAE, 54, 1, 2012, pp. 13-18
INTRODUCTION
Apert syndrome, or acrocephalosyndactyly, is a congenital syndrome with bicoronal synostosis and limb malformations. The skull is typically brachicephalic, with the presence of a flat facies with hypertelorism, strabismus, ocular muscle palsies, short zygomatic arches, and maxillary hypoplasia. The fontanelles may be large and late in closing. The palate is narrow and either has a median groove or is cleft with a bifid uvula. This syndrome usually includes the upper and lower limbs, which display bony syndactyly and complete fusion of the four fingers, leaving the thumb free. The terminal phalanx of the thumb is short and often broad with radial clinodactily. All bones are totally deformed, with symphalangism, conjoined finger nails and synostoses between metacarpals and carpal bones. Soft tissue anomalies involve the intrinsic muscles of the hands, the extrinsic tendon insertions and the neurovascular bundles. Cutaneous syndactyly of all toes may be either of the simplex or complex types (6).
The incidence of Apert syndrome is reported to be from 1 : 100,000 to 1 : 160,000 births. Although the occurrence is sporadic, transmission is autosomal dominant as a new mutation with normal karyotype (17). New data suggests that different mutations in the fibroblast growth factor receptor 2 (FGFR-2) genes are most responsible for the appearance of this syndrome (3).
In 1981 Swanson et al. introduced the embryological classification of Apert hand as a failure of differentiation of the mesenchymal elements of the limb-bud between the fifth and the eighth week of embryonic life (16). Anatomically it may be classified according to the degree of failure of differentiation into complete and incomplete, or into complex or simple, depending upon whether elements other than skin are common to both digits or not. If only the most distal parts of the digits are fused, it is termed acrosyndactyly. These pathologic anomalies of bone, cartilage and soft tissue have later been sub-classified by Upton (18) as Type I to Type III of increasing clinical severity of the skeletal coalition. Type I or spade hand is the most frequent. The first and fourth web spaces have an incomplete simple syndactyly, with the central mass flat to the palmar plane. Type II, or mitten/spoon hand has a complete simple syndactyly of the first and the fourth web spaces, with central mass curved due to fingertip fusion. Type III or hoof/rosebud hand has the thumb ray incorporated within the central mass with synechia of nails, complete complex syndactyly of the first web space and simplex sindactyly of the fourth web space with metacarpal fusion. Because of the shortness or absence of the first web space, it is impossible to perform a pincer grip. A short radially deviated thumb, complex syndactyly, symphalangism of all 4 digits and a simple syndactyly of the fourth web space are common to all types of Apert hand (16, 18).
The correction of the craniofacial anomalies is usually performed first, but this is not obligatory. An accompanying mental retardation is variously reported in association with Apert syndrome, but it is unclear how much of it is secondary to environmental influences. Certainly, many patients with Apert syndrome attain a high level of mental function (11).
The timing for surgery for correction of the hand abnormalities continues to be controversial (2, 11). These days, correction of hand deformities should start when the child is about 6 to 12 months old. Since it is known that hand function patterns are established between 6 and 24 months of age, the digits should be separated within this time frame (15). Apert hand requires multiple staged procedures and different surgical techniques to obtain the appropriate hand function. Surgery usually starts with the separation of the multiple bilateral syndacitylous digits and thumb, and obviously needs a later correctional osteotomy for radical clinodactily of the thumb. The main principles of treatment are to lengthen and realign the thumb and to separate the border digits first. The central mass (mitten-glove symphalangism) should be released only on one side, but surgical separation “per se” produces relatively little functional improvement. An early start allows these surgeries to be completed before 2 to 4 years of age, and they should definitely be completed before the child starts going to school. A child less than 14 months old with bilateral anomalies will usually tolerate having both hands immobilized due to simultaneous bilateral surgical procedures. After that age, bilateral surgical procedures are less well tolerated. A growing child will attempt to use every available part of a congenitally deficient hand, provided that sensation is adequate; however, when he realizes that an extremity is different from that of other children, the child may hide it in shame and deny its effective usage (12, 8).
MATERIALS AND METHODS
We present a series of seven patients who were admitted to our Division between January 1995 and December 2010 with Apert syndrome with complex hand syndactyly, and lateral ray polydactyl on the feet. There were five neonatal boys and two neonatal girls (Table 1). The average age of the patients was 1.7 years (range from 1.2 to 2.2 years). There was a bicoronal synostosis in the first case report and a combination of bicoronal synostosis and cleft primary and secondary palate in another case report. Neurosurgical treatment was performed at 22 to 26 months of age; the primary palate closed at 8 months and the secondary palate closed at 18 months of age. The concomitant feet syndactylies were usually operated on throughout the school ages. The etiology of these congenital anomalies was unknown (see Table 1). In our series, there was no history of teratogenic agents used by the mothers during intrauterine life. Nevertheless, in one case the mother had a serious urinary infection with Pseudomonas species during her pregnancy. According to the Upton classification, there were five cases of Apert hand Type I, one case of Type II and one case of Type III.
1. Patients’ characteristics and etiology of syndromes 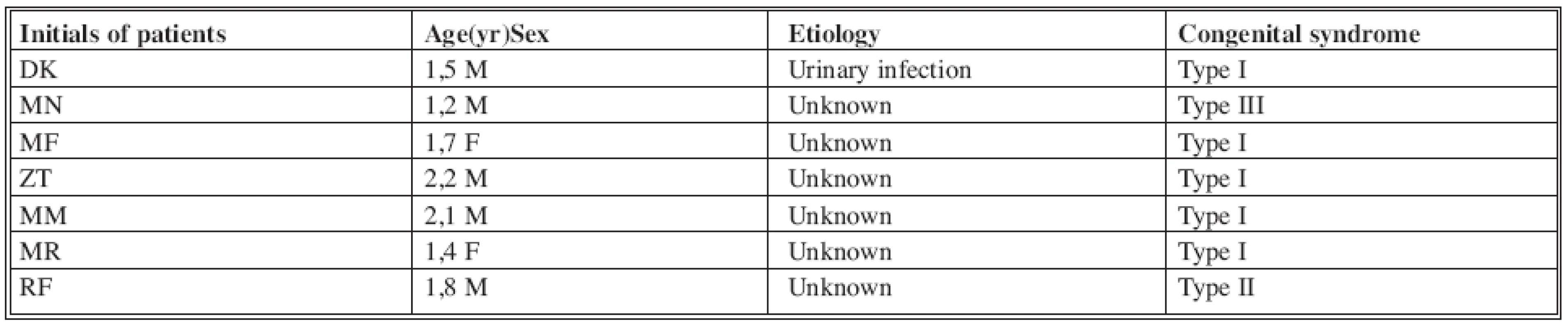
Operative technique
All operations were performed under general anesthesia with tourniquet control and under loupe magnification to allow direct identification of the functional structures of the digits. However, the main targets in our operative strategy were the border digits on both hands, releasing and deepening the first and the fourth web spaces between the ages of 12 and 22 months. With that procedure the concomitant risk of permanent deformity to the adjacent and longer tethered index and ring fingers is minimized (18). In later surgeries, the second and the third web spaces around the middle fingers are sequentially released over the next 26 months (12). These adjacent web spaces should be released separately in a subsequent surgery. An alternative strategy might be to operate on the first and the third web space, and then on the second and the fourth in a subsequent surgery. We performed the thumb osteotomy with bone grafting for clinodactily at 3 to 6 years of age, using internal AO plates and screws or Kirschner wires. Reoperation of the first web space was carried out at around this time as well (12). If necessary, distraction lengthening as a late multi-staged procedure using external fixation and bone grafts could be performed because of a short digit (12). During the adolescent period, we performed one arthroplasty of the carpometacarpal (CMC) joint of the index finger with Swanson’s type of silicon prosthesis. We also performed an “intrinsic muscle” release combined with extensor tendon transfer and corrective osteotomy on a second patient during adolescence, because of prolonged clinodactily of the second digit (9).
The operative reconstruction of 28 fused webs (four webs for each of the seven patients) was achieved by separation of the digits using the inter-digital zig-zag incision and forming web skin flaps based either dorsally or palmarly on the hand. The resulting inter-digital bare areas were covered with full thickness skin grafts (FTSG). The donor site for FTSG was the inguinal or buttock area using a template pattern, and sutured into the defect with absorbable Vicryl-Plus or Polypropylene-Prolene sutures. The hands were postoperatively dressed with tulle gras and cotton gauze or polyurethane sponges and bandaged with crepe bandage or adhesive tape. Digital immobilization was obtained with Kirschner wires placed in the subcutaneous plane of each digit, or we used a “Paris splint” for hand immobilization. The first dressing was applied postoperatively after 2-3 days under sedation or anesthesia. Between 7 to 10 days after surgery the child was released home. The next follow-ups were every 2 days in an outpatient clinic. Further follow-ups were carried out once per year, over a period of three years after the last operation.
RESULTS
We analyzed seven patients with Apert syndrome and complex hand syndactyly. The main aim is to start with the operations as early as possible, which means immediately after first contact with the child and its family. The first operation was performed on the border digits, releasing the first and the fourth web space, and in two particular cases on the first and the third web. In subsequent surgeries, the second and the third web space on either sides of the middle finger were then sequentially released. In the second group of patients this was done on the second and fourth web.
Web spaces were released in twenty three cases, requiring 41 operations. In 5 (21%) cases a web contracture developed and in 4 (17%) cases there were significant flexion contractures of the digits. The influence of the reconstruction methods on the web and flexor contractures is shown in Table 2. All our patients required some kind of later procedures for additional deepening of the acquired web space and flexion contractures. Four different local skin flaps (i.e. dorsal quadrangular, palmar and dorsal triangular, dorsal triangular in a horseshoe shape, and dorsal transposition flap from index finger) have been used for the reconstruction of the web floor after digital separation. In all cases we used FTSG to cover the resultant bare areas of the cleft following closure of the inter-digital zig-zag flaps. The healing process of FTSG over bare areas of bone lasted longer and had a minimal percentage of partial skin lyses. Additional Z or W-plasty with FTSG was used for releasing the concomitant flexion contractures.
2. Comparison of web floor reconstruction methods and their influence on web and flexion contractures 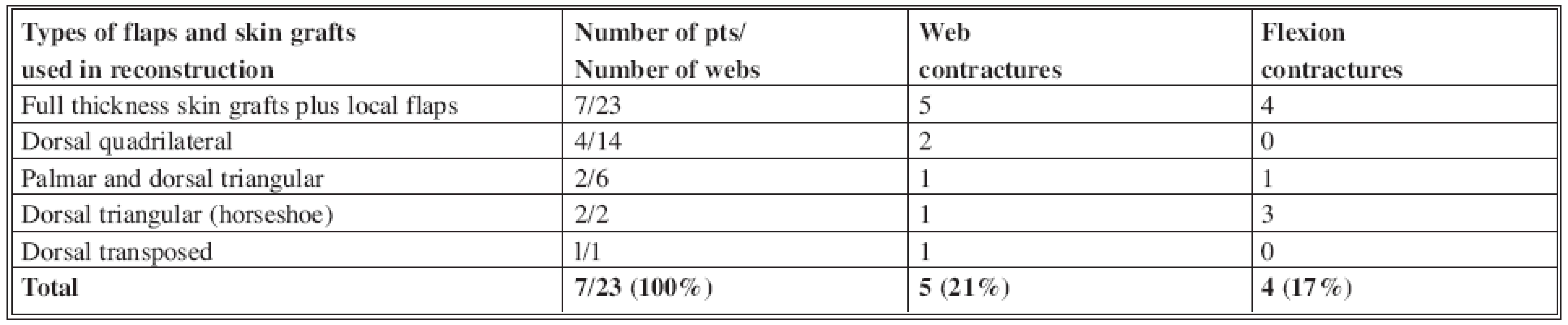
For radial clinodactily of the thumb we predominantly used wedge osteotomies in all patients, and in two cases we combined this with a cancellous bone graft from the iliac crest. We achieved additional lengthening of the short thumb in two cases by performing a distraction lengthening procedure using bilateral external fixation and AO plate and screws with bone grafting from the iliac crest or with Osteovit (a type of bone homograft).
Finally, all of the children had a functional pincer grasp that enabled them to write. However, they all had difficulties in making a firm palmar grip because of a huge symphalangism in the central zone of the hand. To achieve better handwriting and overall function, we performed an additional arthroplasty with Swanson-type silicon prosthesis of a metacarpophalangeal (MCP) joint in one case and an “intrinsic muscle” release with tendon transfer for better extension of the index finger in a second case, during the primary school period. The aesthetic outcome in all cases was satisfying and the family members were also pleased.
Craniofacial anomalies, such as bicoronal synostosis, were operated on in another hospital in two cases. Clefts of the primary and the secondary palates were operated on in our Department. The patients’ mental status after the craniofacial operations was acceptable, and they are attending regular primary school.
Our clinical group has only seven cases, and therefore we cannot conclude that a later operation carries a higher risk of web contracture or flexion contracture recurrence, and insufficient grasp grip or pincer grasp. However, the psychosomatic outcome and quality of life will be better if all operations are performed before 4 years of age – and certainly before children start primary school.
CASE 1
A 12-month-old boy presented with Apert syndrome and complex type III hand syndactyly. The first operation was performed at the age of 14 months with simultaneous bilateral separation of the border digits by releasing the first and the fourth web spaces (Fig. 1). At subsequent surgery at the age of 20 months, the third web space was released on the ulnar side of the middle mass. The digital synostosis between the index and the middle finger was separated later, at 28 months of age, to avoid a permanent deformity of the adjacent longer tethered index finger and to preserve a compromised digit circulation (Fig. 2). A later subsequent surgery with five fingers on the left hand and four fingers on the right side, and plain film radiographs, was carried out at 38 months of age (see Fig. 2). The thumb wedge osteotomy with bone grafting from the proximal ulna for radial clinodactyly was performed at 4 years of the age, in separate procedures on each hand. The next operation was an additional lengthening of the short thumb on the right hand by using the distraction osteogenesis with external fixation and bone grafting from the proximal ulna. Both hands have been in use prior to school time. The last operation was an MCP arthroplasty with Swanson silastic prosthesis (Mitek) at 12 years of age, for a better range of motion in the small MCP joint of the index finger. During the three year follow-up period after the last operation, we tested the flexion and extension of the fingers, pinching, grasping, range of motion in the small joints and 2 point discrimination test (2 PD) on both hands for functional outcome. The Apert acrocephalosyndactyly was surgically corrected in another clinic at 25 months of age (Table 3).
Fig. 1: Case 1 – a 14-month-old male: Type III Apert hand with corresponding X-ray film 
Fig. 2. Case 1 – a 38-month-old male: later surgery with five fingers on the left hand and four fingers on the right hand, and corresponding X-ray film 
3. Follow up testing and question-form 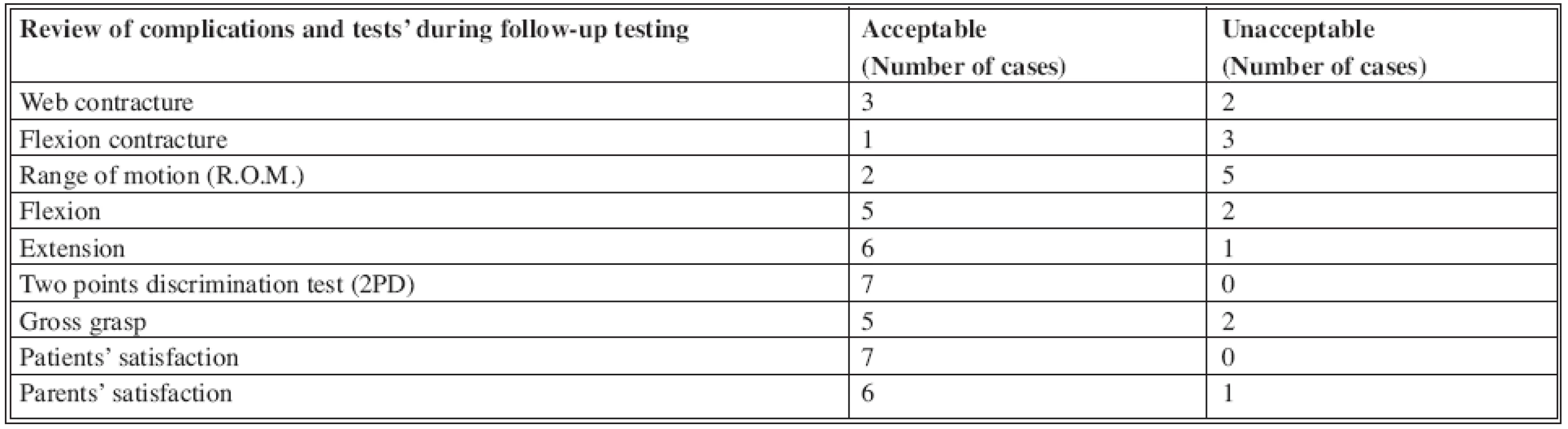
CASE 2
A 17-month-old girl presenting with a type II Apert hand and had her first operation at 19 months of the age, when the webs of the border digits on both hand were simultaneously released. The next operation for the second and the third webs was performed at 3 years of age. The thumb wedge osteotomy with bone grafting for radial clinodactyly was done prior to the start of the primary school. The “intrinsic muscle” release and extensor tendon transfer for better extension on the index finger was carried out at 13 years of age. The follow-up testing for the function of both hands was done during the school age period. The Apert acrocephalosyndactyly was surgically corrected in another clinic at 2 years of age, cleft of the primary palate at 8 months of age and secondary palate at 18 months in our clinic.
DISCUSSION
Dr. Apert described the acrocephalosyndactyly syndrome that bears his name at the beginning of the past century (8). It occurs in more than 1 : 100,000 live births. Apert syndrome is a result of a mutation of the fibroblast growth factor receptor type 2 genes, on chromosome 10q, and inheritance is autosomal dominant (3). Both hands usually have the following deformities: short radially deviated thumb, deficient first web space, complete and complex syndactyly and symphalagism involving the central three rays, and simple, complete syndactyly between the ring and fifth rays. The most comprehensive clinical and radiographic analysis is provided by Upton (18). These pathologic bone, cartilage, and soft tissue anomalies occur in the three predominant clinical patterns classified as Type I to Type III according to increasing clinical severity. Accompanying anomalies of the neurovascular bundles in the involved hand are very common as well.
Correction of the craniofacial deformities is usually performed first (17). Unfortunately, the timing of the surgery for the correction of Apert hand syndactyly is still controversial (15, 18). Today correction of hand deformities is usually recommended when the patient is approximately 1 year old (2). Patterns of the hand function are known to be established between 6 and 24 months of age, so the digits must be separated within this time frame. Surgery is usually not recommended before the age of 6 months because of the increased risk of anesthesia, although Raus reported simple syndactyly repair in two newborns less than 72 hours old (14). On the other hand, Flatt (5) holds off all surgery until a minimum age of 18 months. In cases of complex syndrome syndactyly, Barot et al (2) perform the first surgery at 7 months of age unless there is thumb involvement, in which case the first subsequent release of the web space between the middle and ring finger is carried out between 3 and 6 months of age. All surgery is usually completed by 2 to 3 years of age. Based on our series, we agree that the timing of operations appears to be a very important predictor of success, especially when we compare cases of different complexities, although in simple cases the time of surgery did not appear to be the main factor for a good final outcome. We support the suggestion that digits of disparate length should be separated early to avoid deformities produced by the shorter digit restricting the growth of the longer digit. In light of this, our early and simplified approach for the treatment of the complex hand malformation syndrome of Apert acrocephalosyndactyly (in the first case we started at 12 months of age) has been successful in achieving a timely separation of digits and web spaces with a low revision rate and a satisfying functional outcome of hand function.
Surgical considerations focus on the complete release of the syndactyly, the creation of an adequate web space and the correction of the skin deficiency. The order of separation of digits depends on their functional importance, and their release is usually performed first (19). The most current techniques involve zig-zag incision and small triangular flaps designed to interdigitate in the side of the fingers. Additional skin flaps are necessary whenever structures such as vessels, nerves or tendons are involved, or bone or joints are exposed. A limited number of local flap typess (i.e. dorsal quadrilateral, palmar and dorsal triangular and dorsal triangular-horseshoe) can be used depending on the location and size of the defect (13). The use of dorsal metacarpal island flaps or the application of tissue expanders, in both complex and simple syndactyly, may reduce the need for a second surgery (13). Ashmead reported revisions in 35% of cases when he used expanders, and he suggested that tissue expansion is not so useful for treating Apert hand (1, 4). However, presently, FTSG primarily harvested from the inguinal region are still commonly used skin grafts in everyday practice. Meticulous microsurgical technique and good postoperative dressing with additional subcutaneous Kirschner wires for digital immobilization are essential measures for a good healing of FTSG and skin flaps. We used polyurethane sponges to additionally splint skin grafts. This dressing applies firm pressure to the digits and also reduces maceration of grafts. The donor site morbidity was acceptable in all of our cases. Additional undergrowth or hypoplasia may affect a part or an entire digit. The phalanges are quite thin in children and if there is any distraction we must be very careful during daily manipulation (10). A cooperative child and family are essential for the success of this procedure.
The correction of the thumb deformity before 2 to 3 years of age is the first important step to allow its growth and the development of its function. The reconstruction of an adequate first web space is also the first priority. It is best to deepen with W-plasty or with dorsal skin flap from the first web and index finger (2). In some particular cases, inguinal or lateral arm flaps as free micro-vascular transfers may be used, but the final result with a free flap on the web space is usually unacceptable (15). The sequential release of the skin and fascia, “intrinsic muscle”, lengthening, and capsulotomy of the MCP joints allow the thumb ray to be positioned in 45 degrees of abduction. The thumb clinodactyly can be corrected with osteotomy of the proximal phalanx, but in our case of short thumb we used wedge osteotomy and bone grafting.
During the first operation we treated the first and fourth web spaces. In all of our cases we used local flaps with FTSG for closure of defects. Other web spaces were treated separately, one web space per operation, in order to minimize the morbidity from complications (i.e. infection and lesions of the neurovascular bundles). We performed revision of other webs in 5 (21%) cases and revision of flexion contractures in 4 (17%) of the cases, which differs little from the results of Chang et all - 13% (10) for both types of revisions, and Barot and Caplan - 16% (2) for both types of revisions. Clinodactyly on another digit may be radial or ulnar as a result of phalangeal dystrophy. Splinting is usually ineffective, and the correction demands a bone wedge osteotomy, that may have to be repeated as the child grows. The separation of the fifth finger syndactyly is an additional important issue to avoid alignment deformities during growth. This operation should be performed as early as possible. Concomitant symphalangism regularly affects the ulnar side of both hands. Function may be improved by osteotomy and fusion in a functional position, or various types of arthroplasty can be used (5). Metacarpal synostosis is also a rare concomitant malformation based on the length of the synostosis. The main problem is a frequent divergence of the digits, and during surgical correction we can perform separation, lengthening, or amputation of the digit if necessary. Additional surgery to mobilize the small finger by releasing the ring finger and little finger metacarpal synostosis may be required if the little finger is functional (7). If there is significant carpometacarpal stiffness (a rarity), then MCP arthtoplasty, corrective osteotomy, additional distraction lengthening with or without bone grafting, “intrinsic muscle” release and extensor tendon transfers may be required at 7 years of age or later. Further revision may be necessary during adolescence (19).
CONCLUSIONS
There is no simple algorithm for most congenital hand anomalies and complex syndromes (i.e. Apert syndrome), and straightforward guiding principles should be followed. The first operation should be performed as soon as possible, usually at 1 year of age. The associated anomalies of other organ systems should always be borne in mind during surgical planning. The timing of the operation as well as the sequence of multi-staged procedures plays an important role in the final function of the hand. It is not always possible to achieve both a satisfactorily powerful grasp and precision handling. Standard methods for syndactyly correction still carry a significant failure rate and post-surgery complications. Although we had only seven cases in our retrograde trial analyses, our opinion is that our functional results after surgeries for Apert hands are satisfactory and similar to those from the literature. By using a complex surgical approach, coupled with early released webs, osteotomies, skin flaps and FTSG for immediate reconstruction, we can achieve a low revision rate with an acceptable functional and aesthetic outcome. Gross grasp and pinch, appropriate flexion and extension tests, range of motions in small joints, test of 2PD and parent and patient satisfaction are the main outcome parameters of hand function in treated Apert hand.
Address for correspondence:
Zdravko Roje, M.D., PhD
Division of Plastic Surgery and Burns, Department of Surgery, University Hospital Center Split, School of Medicine
Soltanska 1
21000 Split
Croatia
E - mail:zdroje@kbsplit.hr
Sources
1. Ashemead D, Smith PJ. Tissue expansion for Apert’s syndrome. J. Hand Surg. Br., 20B, 1995, p. 327–330.
2. Barot LR, Caplan HS. Early surgical intervention in Apert syndactyly. Plast. Reconstr. Surg., 77, 1986, p. 282–285.
3. Britto JA, Chan JCT, Evans RD, Hayward RD, Jones BM. Different expression of fibroblast growth factor receptors in human digital development suggests common pathogenesis in complex acrosyndactyly and craniosynostosis. Plast. Reconstr. Surg., 107(6), 1999, p. 1331–1345.
4. Coombs CJ, Mutimer KL. Tissue expansion for the treatment of complete syndactyly of the first web. J. Hand Surg. Am., 19A, 1994, p. 968–972.
5. Flatt AE. Practical factors in the treatment of syndactyly. In: Litter JW, Cramer LM, Smith JW (Eds), Symposium on reconstructive hand surgery. Saint Louis: CV Mosby, Vol. 9; Ch 14, 1974, p. 144–156.
6. Flood J, Hobar C. Craniofacial anomalies II: Syndromes and surgery. Selected Read. Plast. Surg., 8(25), 1992, p. 1–57.
7. Foucher G, Navarr R, Medina J, Knouri RK. Metacarpal synostosys: A simple classification and a new treatment technique. Plast. Reconstr. Surg., 108(5), 2001, p. 1225–1234.
8. Hooven GH, Flatt AE, Weiss MW. The hand and Apert’s syndrome. J. Bone Joint Surg. Am., 52, 1970, p. 878–895.
9. Kozin SH. Upper extremity congenital anomalies. J. Bone Joint Surg. Am., 85A (8), 2003, p. 1564–1576.
10. Netscher DT. Applications of distraction osteogenesis. Clin. Plast. Surg., 25(4), 1998, p. 561–566.
11. Netscher DT. Congenital hand problems: Terminology, etiology, and management. Clin. Plast. Surg., 25(4), 1998, p. 537–552.
12. Netscher DT. Treatment of congenital upper extremity problems. Plast Reconst Surg., 119(5), 2007, p. 101e–129e.
13. Percival NJ, Sykes PJ. Syndactyly: A review of the factors which influence surgical treatment. J. Hand Surg., 14B, 1989, p. 196–200.
14. Raus EE. Repair of simple syndactyly in healthy neo-newborn. Orthoped. Rev., 13, 1984, p. 494–498.
15. Salazard B, Galinier P, Samson P, Casanova D. Hand abnormalities in Apert’s syndrome: Surgical management. Eur. J. Plast. Surg., 30, 2007, p. 107–112.
16. Swanson AB, Swanson GD, Tada K. A classification for congenital limb malformation. J. Hand Surg. Am., 8(5 Pt 2), 1983, p. 693–702.
17. Tessier P. Apert’s syndrome: Acrocephalosyndactyly type I. In: Caronni EP, (Eds). Craniofacial surgery. Boston: Little Brown, 1965, p. 280–303.
18. Upton J. Zuker RM. Apert syndrome. Classification and pathologic anatomy of limb anomalies. Clin. Plast. Surg., 18(2), 1991, p. 298–355.
19. Van Heest AE, House JH, Recling WC. Two-stage reconstruction of Apert acrosyndactyly. J. Hand Surg .Am., 22, 1997, p. 315–322.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2012 Issue 1-
All articles in this issue
- Reconstruction of the Hand in Apert Syndrome: Two Case Reports and a Literature Review of Updated Strategies for Diagnosis and Management
- Successful Replantation of a Completely Amputated Ear on a Child
- Middle Phalangeal Distal Condylar Fracture Remodelling in Children: A Case Report
- Comparison of Otoplasty Results Using Different Types of Suturing Techniques
- Breast Hypertrophy and Asymetry: A Retrospective Study on a Sample of 344 Consecutive Patients
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Comparison of Otoplasty Results Using Different Types of Suturing Techniques
- Breast Hypertrophy and Asymetry: A Retrospective Study on a Sample of 344 Consecutive Patients
- Reconstruction of the Hand in Apert Syndrome: Two Case Reports and a Literature Review of Updated Strategies for Diagnosis and Management
- Middle Phalangeal Distal Condylar Fracture Remodelling in Children: A Case Report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

