-
Medical journals
- Career
Examples of use of outpatient negative pressure therapy in chronic wound healing – a set of case reports
Authors: Miloš Prcúch 1; Lubomír Kopp 1,2; Karel Edelmann 1
Authors‘ workplace: Krajská zdravotní, a. s., Masarykova nemocnice v Ústí nad Labem, o. z., Klinika úrazové chirurgie UJEP 1; Ústav anatomie, 2. LF UK, Praha 2
Published in: Úraz chir. 26., 2018, č.3
Overview
INTRODUCTION: Negative pressure wound therapy (NPWT) belongs to standardized treatment methods in many departments. Local controlled negative pressure affects all phases of healing of chronic wounds. Several different therapy systems using same principles are available, the difference lies mainly in their size and ability to absorb wound secretion. Aim of the report is to present benefits of outpatient NPWT compared to standardized NPWT used in departments with regards to social and labor demands of patients.
MATERIAL AND RESULTS: Outpatient NPWT should be small in size, which means systems not using collecting containers. Two systems available in our market are PICO® from manufacturer Smith & Nephew and newer AVELLE® from manufacturer ConvaTec. Besides benefits, there are existing risks connected mainly to monitoring output of the wound secretion. Three NPWT case reports present benefits of the therapy concerning efficacy of the method and minimal limitations of the social and labor demands of patients. Outpatient NPWT protects wound from contamination, alleviates pain and lowers the number of wound redressing. Compliance of patient is needed in situations with higher output of secretion fluid.
CONCLUSION: NPWT systems do reach in correct indication the same efficacy in treatment of chronic wounds compared to systems with collecting container and higher efficacy compared to modern wound dressing materials. Main disadvantage is thus limited absorption of wound secretion and compliance of patients.
Keywords:
Chronic wounds – outpatient negative pressure wound therapy – wound necrosis
INTRODUCTION
The principle of the effect of local negative pressure on the reatment of chronic wounds is described in many studies. Local Negative Pressure Wound Therapy (NPWT), acts on all stages of healing of a chronic wound: it increases blood supply to the wound base, thereby increasing O2 partial pressure and nutrient availability, leading to support for autolytic débridement and faster demarcation of necroses. By extracting exudate and tissue fluid it effectively reduces bacterial and toxic burden on the wound base, while also preventing wound contamination from the outside environment, thereby positively affecting the cleansing (inflammatory) healing phase. It also significantly reduces the risk of nosocomial infections [4]. The mere removal of interstitial fluid rich in pro-inflammatory mediators in the early stage of healing can lead to a faster tissue repair [7]. Labler showed a higher concentration of interleukin 8 (IL-8) and vascular endothelial growth factor (VEGF - angiogenesis initiating factor) in early exudate in the treatment of 32 patients with soft tissue injuries under negative pressure compared to wounds treated with conventional means [7]. Decreasing concentration of pro-inflammatory factors induces formation of granulation tissue as these inhibit its formation [7]. An important factor is the rate, length and branching of the interstitial fluid flow that positively affect vascular neoformation and VEGF activity. This effect is noticeable up to a flow rate of 50 mm/min., but its maximum is achieved at a flow rate between 10 and 20 mm/min. [1]. Another strong stimulus for the formation of granulation tissue is the micro-deformation of the wound base, which is caused by pressure forces at the contact points of the wound base with the filling material (polyurethane foam) and traction forces at its pores [3]. In addition to the term microdeformation, which induces changes at the subcellular level, the term macrodeformation has also taken place. This is associated with a change in the size of the wound based on the contraction of the filling material after the application of the vacuum, the size of which is influenced in particular by the physical properties of the wound base and filler material and the vacuum level [7].
Active contraction of wound margins, along with support for epithelial migration from wound margins, leads to faster epithelialization. Another important feature of negative pressure is the reduction of wound edema around the wound. Krass et al. reports a significantly shorter treatment time in a group of 25 patients with compartment limb syndrome treated with negative pressure from day one after fasciotomy and in most patients with wound closure by linear suture without plastic surgery [2].
MATERIAL
The systems for negative pressure therapy are divided according to different aspects. From the point of view of the method of removal of early secretion, the systems can be divided into those with a collecting container and those without it. In the first group, the portable pump develops a negative pressure that is transferred to the wound bottom by a hose drainage system. This one is in contact with the suction device by means of a specific covering most often formed by polyurethane (PU) foam. Early secretions are collected in a collecting container outside the wound using a multi-tube hose drainage system. In addition to the open-pored hydrophobic polyurethane foam, which is suitable for removal of secretion from the wound and for stimulating granulation tissue formation (microdeformation), polyvinyl alcohol foam dressing is often used, which is hydrophilic and does not adhere to the wound base. Its use is advantageous where progression of granulation tissue formation is no longer preferred or in patients undergoing granulation tissue penetration into black PU foam. Different therapy parameters, such as vacuum level (most commonly in the range of 20 to 200 mm Hg), or the method of treatment, can be set on these instruments. Continuous mode creates negative pressure in the wound continuously for all the time. It is recommended in the first 48 hours for all types of wounds. In the following days, it is indicated in patients who have experienced severe pain, cover leakage, a condition of high wound waste, need to strengthen the affected area or prevent skin transplantation during intermittent therapy [8]. For intermittent mode, 5 minutes of active suction and 2 minutes of therapy interruption are most often used. It contributes to faster granulation tissue formation, wound closure, approximates fistula walls [8]. Newer devices allow the practitioners to record total therapy time, display brightness for day and night mode. Hartmann‘s Vivano®Tec System Pro of the latest generation used also in our workplace features a well-arranged history of events including a filter function for easy therapy analysis. A certain disadvantage of these systems is the need for trained operators, in addition to the relatively large dimensions and weight.
In the second group of devices, the wound exudate is drained from the wound by aspirating it into the absorptive layer of the wound cover pad, from which a significant part of the exudate evaporates due to the high vapour permeable layer. The absence of a collecting container and the small size of the devices predestine these systems in particular for outpatient use. Therefore, they are often referred to as outpatient negative pressure systems and are intended for single use only. One-touch button operation is very simple.
We use systems such as PICO® by Smith & Nephew or newer AVELLE® by ConvaTec. Both instruments operate at a continuous negative pressure of 80 mm Hg. A significant disadvantage is their limited efficiency, after which the device is programmed to be self-destructed with no further possibility of use and a higher price. In the case of the PICO® system, the amount is CZK 4,860, which the patient pays in full, as the system is not covered by the health insurance company, the price of the Avelle® system is CZK 7,800. This system is covered by health insurance in hospitalized patients. The functionality of the PICO® system is 7 days, Avelle® works for 4 weeks. In foreign literature they are referred to as Singleuse NPWT.
RESULTS
Three examples of outpatient negative pressure wound healing systems are used to hereby present the benefits of this therapy, both in terms of the effectiveness of the method itself and in terms of minimizing the socio-occupational needs of patients and disadvantage in case of reduced patient´s compliance.
Case report 1
A 68year-old patient was sent to the Clinic of Traumatic Surgery in Ústí nad Labem in October 2015 from a district hospital with chronic ankle and foot swelling due to an overlooked fracture of the calcaneus of August 2015. Multiplanar corrective osteotomy and plate osteosynthesis of the fracture were accompanied by a cutaneous incision and suprafascial release of the lobe to relieve tension in the surgical wound. The incision was originally covered with a Vivano® negative pressure system and closed with a free skin graft 2 weeks later. Despite the skin lobe release, the first signs of necrosis at the wound angle occurred as early as a few days after surgery (Fig. 1).
1. Relaxing incision on the metatarsus, with the already healed skin graft. Development of necrosis and defects in the surgical wound 
Defect progression was stopped by applying the Vivano® negative pressure system during 28-day hospitalization. However, as a result of the daily loss of several thousand Czech Crowns due to his absence during the peaking period of maximum work on the farm and in orchards, the patient-farmer insisted on release into outpatient care despite the risk of limb amputation in case of a deep skin defect (Fig. 2).
2. Defect progression in the surgical wound. Situation at the beginning of the outpatient negative pressure therapy using the PICO® system, before discharging the patient 
That is why he was offered an application of the PICO® outpatient NPWT system, which he agreed to despite full payment of its price. He was released on the 27th day after the corrective intervention. Already during the first outpatient check, the patient reported a reduction in pain and swelling, no need for home redressing and, in particular, the possibility of active work in orchards as well as in the stables of horses and pigsheds, which was allowed by the hermetically closed vacuum system. For a clear defect regression and subjective patient satisfaction, the system was applied repeatedly for 6 weeks, with a total of 6 applications. After this time the defect was completely cleared and granulated almost to the level of the surrounding tissue (Fig. 3).
3. Situation after 6-week outpatient administration of negative pressure 
In this healing phase, the negative pressure treatment was stopped and the healing of the defect was performed using other modern dressing materials. Indication of this change in treatment is questionable because of the subsequent stagnation of healing practically immediately after discontinuation of the negative pressure. The next image (Fig. 4) shows the wound condition 4 weeks after the end of the negative pressure therapy and dressings using gels, alginates and silver-containing foams.
4. Situation after 4 weeks from the termination of outpatient negative pressure therapy, after changes of dressings using standard dressings, without any signs of healing progression 
Hyperkeratoses and parakeratoses in the defect, possibly caused by secondary infection, developed in the following course. Neither malignancy nor specific inflammation has been proven histologically (Fig. 5). The patient was transferred to another specialized outpatient clinic for further relapses of progressive parakeratosis, but it was not fully healed even after 3 years (Fig. 6).
5. Hyperkeratosis and parakeratosis in the defect, 35 weeks after surgery 
6. Local condition, 3 years after treatment 
Case report 2
A 58-year-old patient suffered an open bruised wound in the calf caused by the fall of a metal gate in August 2016. A suture of the wound upon revision was performed, however, with subsequent necrosis of the lobe and an origination of a defect, which was later dressed by the VIVANO® negative pressure system during hospitalization. After cleaning and granulation of the defect, the Thiersch skin sculpture was performed 3 weeks after the injury, but due to the superinfection it was later separated and the defect was restored. Further hospitalization with the intended skin graft re-plasty after defect cleansing was refused by the patient, justifying that by the need to reopen her professional outpatient practice and preference of further treatment in the form of outpatient dressings. These were initially carried out with greasy tulle with Betadine, after two weeks with foamed silver cover, which, despite the beneficial effect on healing, was perceived by the patient as unsatisfactory due to the need for repeated replacement of the secondary dressing cover in the course of day due to significant secretion from the defect, which significantly reduced her performance in outpatient practice (Fig. 7, 8).
7. , 8.: Situation after 3 weeks of outpatient changes of dressings, using Betadine Ointment and Mepilex® Ag 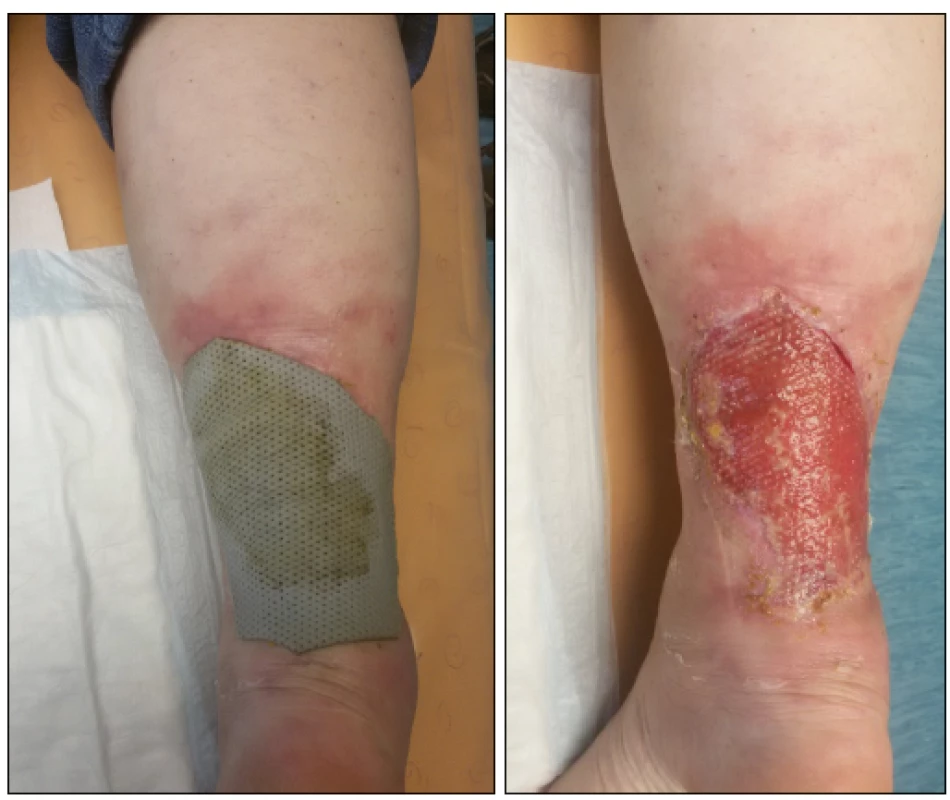
Therefore, after three weeks of outpatient re-dressing, the PICO® system was applied, which was perceived very positively by the patient. Its application resulted in a significant reduction in pain, reduction of calf swelling and prolongation of the re-dressing interval to twice weekly, which the patient reported as the major benefit in the exercise of her profession. After discontinuation of PICO®, the patient perceived a switch back to Mepilex® Ag dressings as a significant discomfort due to aggravation of pain, increased swelling, the need for more frequent redressing and, in particular, worse adhesion of the dressing to the defect. For this reason, the PICO® system was deployed twice more on the 8th and 13th week after the accident. After completion of the negative pressure therapy, the residual defect of 5 x 1.5 cm (Fig. 9) was completely healed with Mepilex® Ag and Ialugen® in December 2016, i.e. the 19th week after the injury.
Fig. 9.: Condition at the termination of negative pressure therapy 
Case report 3
An 83-year-old patient with persistent cardiac pacing for atrial fibrillation, warfarinized, suffered a bulky subcutaneous hematoma on the lateral side of the thigh on 12/12/2017. During the initial treatment, two days after the injury, a bulky subcutaneous hematoma with fluctuation, ischemic skin and bulla was present in the centre of the arch. For imminent skin necrosis, a spot incision was made under local anesthesia and evacuation of a portion of the hematoma to release skin tension. The final evacuation was performed after the adjustment of the coagulation parameters on 13/12/2018. The patient was released on 18/12/2017 in home care. Already a week after release, a large fluctuation occurred at the site of the original hematoma, which was drained after suture removal and the opening of the original incision. Erysipelas were diagnosed on the crus of the affected limb, antibiotic therapy was initiated. For the subsequent development of fascia necrosis at the bottom of the cavity, a radical debridement of a 30 x 10 cm cavity was performed on 30 December 2017 in the course of rehospitalization. During outpatient dressings, a the incision was healed by fistula from which abundant serous secretion persisted, greatly limiting the patient with the necessary wound redressing several times during the day. As the patient managed the operation of modern equipment without difficulty, treatment with outpatient negative pressure appeared to be the optimal choice. When applying the Avelle® outpatient system, the patient was instructed to strictly prevent the wound secretion flowing through the tubing to the device. The next check was scheduled in five days, in the event of any difficulties even earlier. He came for examination on schedule, saying that some three days after the machine had been loaded, some liquid flowed out of it and stopped working the next day. The function has not been restored, the device was wasted (Fig. 10).
Fig.10.: Devaluation of the instrument with instillation of early secretion into the instrument. The arrow points to the secretion in the suction tube 
The wound with subcutaneous cavity was then regularly redressed with dry gauze and healed over the next ten weeks.
DISCUSSION
Due to the similar principle of the function of negative pressure systems with and without a collecting container, the indication criteria are similar too. The basic factors we take into account when selecting a suitable system are the general condition of the patient, the extent of injury and the amount of exudate produced. If the overall condition and extent of injury allow for outpatient treatment, we choose systems without a collecting container. However, these are not suitable for wounds with abundant secretion, as they may irritate the surroundings of the defect caused by accumulated secretion in the cover pad. A more serious complication may be the aspiration of the secretion into the device, which will destroy it, as demonstrated by case report no. 3.
The different vacuum levels of the individual systems (in the case of systems with collecting container, mostly 125 mm Hg and in systems without the container 80 mm Hg) have no influence on the selection decision since the latest published results of the clinical studies show that the efficiency of the NPWT is not limited by the use of a specific material that fills the wound, nor does it bind to a specific vacuum level. Possible determination of its truly optimal value will be a matter of further clinical studies [6]. This statement is in some contradiction with the unpublished results of Walch et al., suggesting that the chemical composition of the foam used affects the extent of activation of inflammatory processes [7].
A number of papers describing the beneficial effect of outpatient negative pressure therapy to prevent dehiscence and acute healing complications when applied to fresh surgical wounds are available in the literature. However, there less of them on the use of outpatient negative pressure for chronic defects [5]. In our outpatient department, we apply negative pressure only to chronic defects with complicated healing. In all cases, a different degree of progression of healing was apparent already after the first week of application. Despite these facts, defects were healed with other modern dressing materials. This is due to the financial limits for patients acquiring systems not covered by health insurance companies within outpatient care. Due to our good experience and with regard to price, it seems to us to be one of the appropriate indications for applying these systems to stagnating chronic wounds to “trigger” the healing process.
The effectiveness of negative pressure therapy is comparable to the use of modern antiseptic silver dressings and significantly higher than conventional antiseptic topical therapies [6].
CONCLUSION
Outpatient Negative Pressure Therapy Systems appear to be comparatively effective as collecting container systems and more efficient than modern bandage materials in the correct indication for wounds with mild to moderate secretion in various stages of the healing process. The main advantage of the outpatient negative pressure therapy systems is their small size and ease of use, which significantly affect the patients´ mobility and in some cases also allow for their return to work even during treatment, thereby at least partially compensating the higher cost of the vacuum system. The disadvantage is the limited absorption of early secretion.
MUDr. Miloš Prcúch
Sources
- Hernández, VR., Genové, E., Alvarez, L. et al. Interstitial fluid flow intensity modulates endothelial sprouting in restricated Srcactivated cell clusters during capillary morphogenesis, Tissue Eng Part A. 2009, 15, 175–185. ISSN 2152-4947
- Krass, V., Procházka, V. et al. Kompartment syndrom v traumatologii končetin. Úraz chir. 2014, 21, 38–43. ISSN 1211-7080
- Murphey, GC., Macias, BR., Hargens, AR. Depht of penetration of negative pressure wound therapy into underlying tissues. Wound Repair And Regen. 2009, 17, 113–117. ISSN 1067-1927
- Pometlová, J., Pleva, L. et al. Využití podtlakové terapie rány při léčbě otevřených zlomenin III. stupně na Traumatologickém centru FN Ostrava. Úraz chir. 2014, 22, 9–18. ISSN 1211-7080
- Schwartz, JA., Goss, SG., Facchin, F. et al. Single-use negative pressure wound therapy for the treatment of chronic lower leg wounds. Journal of Wound Care. 2015, 24, 4-9. ISSN 0969-0700
- Stryja, J. Repetitorium hojení ran 2. 2.vyd. Semily : GEUM, 2016. 377 s. ISBN 978-80-87969-18-2
- Šimek, M., Bém, R. Podtlaková léčba
ran. 1.vyd. Praha: Maxdorf, 2013. 231 s. ISBN 978-80-7345-352-7 - V.A.C. Therapy-Clinical Guidelines [online], ©2015 KCI Licensing [cit. 2018-09-10]. Anglická verze. Dostupná z WWW: https://www.acelity.com/-/media/Project/Acelity/Acelity-Base-Sites/shared/PDF/2-b-128-emea-enb-emea-guidelines-en.pdf
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2018 Issue 3-
All articles in this issue
- Current approach to the management of forearm and elbow dislocation in children
- Medial malleolar fractures
- Examples of use of outpatient negative pressure therapy in chronic wound healing – a set of case reports
- Forefoot Navicular Bone Fractures - Short Communication and Case Report
- Assessment of the injuring effect of loose objects in a vehicle in a traffic accident
- Effect of earlier load on healing of calcaneus fractures after stable osteosynthesis
- Trauma Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Current approach to the management of forearm and elbow dislocation in children
- Forefoot Navicular Bone Fractures - Short Communication and Case Report
- Effect of earlier load on healing of calcaneus fractures after stable osteosynthesis
- Examples of use of outpatient negative pressure therapy in chronic wound healing – a set of case reports
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

