-
Medical journals
- Career
Comparison of endoscopic mucosal resection and endoscopic submucosal dissection in the treatment of flat neoplastic lesions in the rectum
Authors: O. Urban 1,2,3; Přemysl Falt 1,2,3; P. Fojtík 4; R. Andělová 5
Authors‘ workplace: nd Department of Medicine – Gastroenterology and Geriatrics, Faculty of Medicine and Dentistry, Palacky University and University Hospital Olomouc, Czech Republic 1; Faculty of Medicine at Hradec Kralove, Charles University in Prague, Czech Republic 2; Faculty of Medicine, Ostrava University, Ostrava, Czech Republic 3; Department of Gastroenterology, Vitkovice Hospital, Ostrava, Czech Republic 4; Depatment of Pathology, AGEL laboratories a. s., Novy Jicin, Czech Republic 5
Published in: Gastroent Hepatol 2018; 72(3): 193-198
Category:
doi: https://doi.org/10.14735/amgh2018193Overview
Endoscopic submucosal dissection (ESD) is used for en bloc removal of colorectal lesions > 20 mm. As shown by studies mostly from Japan, ESD is more effective than endoscopic mucosal resection (EMR) in achieving en bloc and R0 resection. Nevertheless, the associated high risk of perforation still prevents the wider use of ESD in the West, including in the Czech Republic. The aim of this study was to compare EMR and ESD for the treatment of rectal superficial neoplastic lesions. Main study outcomes were proportion of en bloc, R0 and curative resections, occurrence of complications, and occurrence of local residual neoplasia. A total of 27 and 30 patients were included in ESD and EMR groups, resp. There were no significant differences in gender, lesion size, and presence of invasive carcinoma between the two groups. En bloc resection was achieved in 21 (78%) vs. 2 (7%; p < 0.005) while perforation not requiring surgery occurred in 3 (11%) vs. 0 (p = 0.099) and local residual neoplasia in 2 (9%) vs. 9 (41%) cases (p = 0,017). No procedure was related to lethality in either group. ESD is a promising method for the treatment of rectal neoplastic lesions.
Key words:
colorectal neoplasia – endoscopic submucosal dissection – local residual neoplasiaIntroduction
Colorectal cancer (CRC) is a major cause of morbidity and mortality in Western countries [1–3]. Screening proved to reduce CRC incidence and mortality [4,5]. The pillars of screening are detection and treatment of precancerous lesions and early cancer [6]. Nowadays, a majority of them can be treated endoscopically. Polypoid lesions represent most prevalent early lesion morphology treated by endoscopic polypectomy as a method of choice. Nevertheless, flat and depressed morphology occur in 40 and 4%, resp. [7]. Flat lesions ≤ 20 mm in diameter can be usually resected en bloc by endoscopic mucosal resection (EMR) technique. For lesions > 20 mm, piecemeal EMR (EPMR) or endoscopic submucosal dissection (ESD) can be used. As shown by studies mostly from Japan, ESD is more effective in achieving en bloc and R0 resection. Nevertheless, associated high risk of perforation still prevents ESD from wider use in the West, the Czech Republic included. Therefore, more studies showing efficacy and safety of colorectal ESD from Western centres are needed. The aim of our study is to compare EMR and ESD in the treatment of rectal superficial neoplastic lesions. Main study outcomes were a proportion of en bloc, R0 and curative resection, occurrence of complication and local residual neoplasia.
Patients and methods
Our study was conducted in a single tertiary referral centre in the Czech Republic. Patients were included prospectively. The study protocol was approved by the local ethics committee at Vitkovice Hospital.
Between January 2013 and December 2014 all consecutive patients treated with ESD were enrolled. Lesions were included if they 1. could be managed endoscopically, 2. required en bloc excision and 3. would require piecemeal removal if treated with EMR. Exclusion criteria were age < 18 years, inability to provide informed consent, signs of deep (≥ SM2–3) submucosal neoplastic invasion, polyposis syndrome, previous treatment of the same lesion and lesion not amenable for ESD with regard to the experience of the attending endoscopist.
Patients treated with EMR between January 2010 and December 2011 served as a control group. In that period of time, rectal ESD was not routinely used in the centre. Patients were enrolled prospectively as a part of another study.
General measures
All endoscopy procedures were provided by a senior endoscopist. To avoid submucosal fibrosis, treatment was carried out without previous biopsy. The coagulation status was examined before each procedure. Rules for management of anticoagulation and antiplatelet agents in patients undergoing high-risk endoscopic procedures were applied. Most of the patients were admitted to the hospital in the morning of the day of the procedure. Colonoscopy was performed after standard split-dose preparation (Fortrans®, Beaufour Ipsen Pharma, Paris, France) using Olympus 180/190 series high definition variable stiffness adult or paediatric colonoscopes (Olympus, Europe SE & Co. KG, Hamburg, Germany). During the procedure, an intravenous sedative such as midazolam or fentanyl was administered in individually adjusted doses. Carbon dioxide was used for colon insufflation. After each procedure, patients were kept under observation at the gastroenterology department. Fluids were allowed orally on the day of the procedure. The physical condition of the patient was monitored, and the blood cell count and C reactive protein (CRP) – the CRP level was evaluated. In the absence of complications, patients were discharged from the hospital on the following day.
Lesion description and staging
The Paris classification was used to describe lesion morphology [7]. Laterally spreading tumours (LSTs) were further classified on the basis of their endoscopic macroscopic appearance into granular (LST-G) and non-granular (LST-NG) types. Moreover, LST-G type was subdivided into homogenous and mixed types, whereas LST-NG type was subdivided into flat elevated pseudo-depressed types [7,8]. The size of each lesion was measured by making a comparison with a diameter of polypectomy snares. The depth of neoplastic invasion was diagnosed using either pit pattern classification and/or high frequency (20 MHz, 30 MHz) ultrasound probe sonography (Olympus UM-DP20-25R or UM-S30-25R). Type Vn pit pattern and significant (> 1/3) narrowing of the third endosonographic layer corresponding to submucosa were considered as signs of deep submucosal invasion.
ESD procedure
Standard ESD procedure starting with semi-circumferential incision followed by submucosal dissection was used. In all cases, Flush knife (Fujifilm Europe GmbH, Düsseldorf, Germany) or Dual-knife (Olympus, Europe SE & Co. KG, Hamburg, Germany) were used. For submucosal injection, 10% hydroxyethylstarch solution (Voluven, Fresenius Kabi, Bad Homburg, Germany) mixed with epinephrine (100,000 : 1) and dyed with methylene blue, was used. Setting of the electrosurgical generator (ESG 100, Olympus, Europe SE & Co. KG, Hamburg, Germany) was Puls Cut Slow 40−60 W for circumferential incision and Forced Coag 10−60 W for submucosal dissection.
EMR procedure
For EMR, the standard “lift and cut” technique was used. For submucosal injection, a saline or 10% hydroxyethyl-starch solution, both mixed with epinephrine (100,000 : 1) and dyed with methylene blue, were used. Elevated lesion was excised using standard polypectomy snare. As a rule, lesions with diameter ≤ 20 mm were treated en bloc while lesions > 20 mm were excised using EPMR.
Specimen evaluation
Retrieved specimens were fixed on a cork plate and placed in a 10% formaldehyde solution. Histological results were report-ed in accordance with the revised Vienna classification of gastrointestinal neoplasia [9]. “R0 resection” was confirmed if both lateral and vertical margins were free of tumour cells. The R0 resection was considered curative when there was no deep (≥ SM2, > 1,000 µm) submucosal invasion, lymphatic invasion, vascular involvement or poorly differentiated component of neoplasia.
Follow-up
Patients with non-curative lesion resect-ions were considered candidates for surgery. In all other cases, patients were advised to undertake a first follow-up colonoscopy after 3 months. During this procedure, post ESD/EMR scar was identified and examined by either narrow band imaging or 0,2% indigo carmine chromoendoscopy. Local residual neoplasia was defined as the histological presence of neoplastic tissue in the biopsy performed on the scar site or from the endoscopically visible lesion.
Statistical analysis
All statistical analyses were carried out using NCSS 2004 and PASS (Number Cruncher Statistical Systems, Kaysville, Utah, USA) with a two-tailed t-test used for parametric continuous variables, Mann-Whitney U test for nonparametric continuous data, and chi-squared test for categorical variables. A p value of < 0.05 was regarded as significant.
Results
The study group consists of 27 patients with 27 lesions (74% males, mean age 68 years) treated with ESD. The basic demographic and clinical data are summarized in Tab. 1. According to size of the lesions they were distributed as follows (range): 10−19 mm in 4 (15%), 20−29 mm in 11 (41%) and ≥ 30 mm in 12 (44%) of cases.
1. Endoscopic submucosal dissection – basic demographic and clinical data.
Tab. 1. Endoskopická submukózní disekce – základní demografické a klinické charakteristiky.
lesion size: 1 (10–19 mm), 2 (20–29 mm) 3 (30+ mm)
AdCa – adenokarcinoma, m – intramucosal, sm – submucosal invasive, NET – neuroendocrine tumour, LFU – lost from follow-up, LRN – local residual neoplasia, M – male, F – female, LST – laterally spreading tumours, GM – granular-nodular mixed, GH – granular-homogenous, NGF – non-granular fl at, NGPD – non-granular pseudodepressed, HGIEN – high-grade intraepithelial neoplasia, LGIEN – low-grade intraepithelial neoplasiaEn bloc and piecemeal resection were achieved in 21 (78%), and 6 (22%) patients, resp. All but one (74%) en bloc resections were R0. Submucosal invasive cancer (SMIC) was diagnosed in 5 (19%) cases. Of these, curative resection was achieved in 4 (80%) while resection of one remaining SMIC was non-curative due to deep (1,583 μm) submucosal neoplastic invasion. There was no procedure-related death. In 3 (11%) patients, intraprocedural perforation occurred which could be successfully closed with endoscopic clips without the need for emergency surgery. Nevertheless, perforation resulted in incomplete resection in 2 (7%) patients who undertook elective surgical rescue treatment. The mean ESD procedure time was 176 (range 55–240) min. The first follow-up colonoscopy was carried out in 23 (85%) patients. Of these, local residual neoplasia was diagnosed in 2 (9%) cases.
The control group consists of 30 patients with 30 lesions (57% males, mean age 66 years) treated with EMR. The basic demographic and clinical data are summarized in Tab. 2. According to the size of lesions they were distributed as follows (range): 10−19 mm in 5 (17%), 20−29 mm in 8 (27%) and ≥ 30 mm in 17 (57%) of cases. En bloc and piecemeal resection was achieved in 2 (7%) and 28 (93%) of patients, resp. Both en bloc resections were R0. SMIC was diagnosed in 2 (7%) cases, both treated piecemeal. There was no procedure-related death and no complicating perforation. Mean EMR procedure time was 32 min. The first follow-up colonoscopy was carried out in 22 (73%) patients. Of these, local residual neoplasia was diagnosed in 9 (41%) of them.
2. Endoscopic mucosal resection – basic demographic and clinical data.
Tab. 2. Endoskopická slizniční resekce – základní demografické a klinické charakteristiky.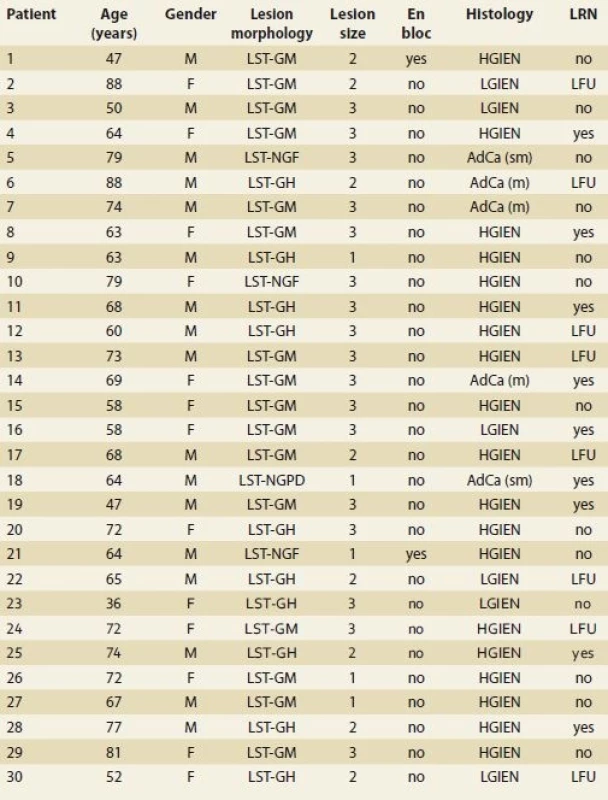
lesion size: 1 (10–19 mm), 2 (20–29 mm), 3 (30+ mm)
AdCa – adenokarcinoma, m – intramucosal, sm – submucosal invasive, LFU – lost from follow-up, LRN – local residual neoplasia, M – male, F – female, LST – laterally spreading tumours, GM – granular-nodular mixed, GH – granular-homogenous, NGF – non-granular fl at, NGPD – non-granular pseudodepressed, HGIEN – high-grade intraepithelial neoplasia, LGIEN – low-grade intraepithelial neoplasiaThere was no significant difference in gender, size of the lesions and presence of SMIC between both groups. The en bloc resection rate was significantly higher (p < 0.005) and the local residual neoplasia rate was significantly lower (p = 0.017) in the ESD group. There was no significant difference in the rate of perforations (p = 0.099) which can be attributed to the low number of cases.
Discussion
In Japan and Korea, ESD is used for en bloc resection of mucosal and superficially invasive cancers both in the upper and lower gastrointestinal tract [10]. While its usage in the oesophagus and stomach has been already adopted in the West, treatment of colorectal lesions is still considered controversial due to high risk of perforation [11–14].
The Czech Republic belongs to the countries with the highest incidence of CRC in the world. Since 2000, a screening programme is organised by the state. Although colorectal ESD is performed in several Czech centres, detailed analysis of treatment results have not been published yet. This study shows that, compared to EMR, ESD provides a significantly higher en bloc resection rate and a significantly lower local residual neoplasia rate. Although higher occurrence of perforation in the ESD group was noted the difference was not statistically significant.
En bloc resection is clinically relevant especially in patients with SMIC [15]. In such lesions, to avoid unnecessary surgery, R0 curative resection must be histologically confirmed, which is generally not possible after piecemeal excision. Since the need for surgery after endoscopic treatment of colorectal neoplasms is the most important outcome criterion, piecemeal resection should be avoided when signs of SMIC are present [16].
In the ESD group, we achieved R0 resection in 5 (100%) patients with SMIC. Of these, curative and non-curative resection occurred in 4 (80%) and 1 (20%) cases, resp. On the other side, in the EMR group, R0 resection was confirmed in none of the 2 SMIC patients who had to be referred to surgery. Our results are in accordance with other studies showing that SMIC was diagnosed more frequently in patients treated with ESD as compared to EPMR (16 vs. 2%) [17].
There is a lot of debate about the safety of ESD in Western centres. In our present study, the rate of ESD related perforation was 11% as compared to 0% after EMR. Although the difference was not statistically significant the trend is obvious. We consider ESD to be a technically more complex procedure. Nevertheless, compared to EMR, our experience with ESD was shorter. In accordance with chronological trends from Japanese series we expect that the risk of ESD related perforation can be decreased to that of EMR. For instance, in a comparison of EMR and ESD of lesions ≥ 40 mm one study from Japan has recently shown perforation in 1.9 and 2.4%, resp. [18]. It has been shown by others that intraprocedural perforation can be closed endoscopically and treated without the need for surgery in most of the cases [19]. Similarly, all three perforations in our series were closed using clips. Nevertheless, perforation did not allow complete endoscopic resection in two of them and they had to undertake elective surgery.
The literature data, including ours, show occurrence of local residual neoplasia after successful ESD in 0−2.8% as compared to 5−54% after EMR [20,21]. In our present study, LRN occurred in 9 and 41% after ESD and EMR, resp. This difference corresponds to the rate of en bloc resection that was achieved in 78% of ESD patients as compared to 9% of EMR patients (p < 0.005).
There are effective surgical alternatives for rectal ESD, namely transanal endoscopic surgery (TEM) and laparoscopically assisted colorectal surgery (LACS). No prospective randomized study comparing these methods is available at the moment. One retrospective study from Asia comparing TEM and ESD shows the same rate of en bloc resection, R0 resection and local residual neoplasia while the time spent in the hospital and operation time were longer in TEM group [22]. On the other side, in a recent meta-analysis, TEM proved higher en bloc and R0 resection rates (99 vs. 88% and 89 vs.75%) while complication rates were similar [23]. In one retrospective study, ESD was compared with LACS in the treatment of early CRC. While both R0 and curative resection rates were higher in LACS group (87% and 87 vs. 100%), the operation time (106 vs. 206 min), length of hospital stay (5 vs. 13 days) and complications (6 vs. 14%) were shorter and less frequent in the ESD group [24]. In another study, outcomes of surgical treatment (open surgery 45, LACS 90, TEM 22) of 175 patients with benign polyps were analysed. Complications occurred in 24%, of these 10 patients had to be re-operated on and 1 patient died [25]. Based on our own experience and literature data, we recommend ESD as a method of choice for the en bloc treatment of rectal lesions. In the Czech medical environment with a widely available endoscopy service, patients with difficult rectal lesion should be referred to an endoscopy centre with experience with endoscopy treatment. Surgery should be reserved for technically difficult lesions, secondary treatment of lesions with non-curative resection and emergency treatment of complications.
There were two patients with neuroendocrine tumours (NETs) in our ESD group. Both lesions had a diameter of 10 mm. Based on histology, ESD was curative in one case while a deep resection margin could not be histologically assessed in one remaining case due to burning artefacts. Never-theless, no residual tumour was endoscopically and histologically found during follow up. Literature evidence shows that NET with diameter ≤ 10 mm should be considered for endoscopic resection, while surgery is a method of choice for lesions ≥ 15 mm. In cases of NET 10−14 mm in size, endoscopy is acceptable as a definite treatment for lesions without muscularis propria invasion, lymphovascular involvement and with mitotic index < 2/10 high power fields [26].
The length of hospital stay in uncomplicated cases in our ESD group of patients was 2 days. Although there is no consensus in the literature we believe that 2−3 days are optimal, since delayed perforation only rarely occurs later.
Our study has several limitations. Firstly, the study is not randomized and selection bias cannot be excluded. Nevertheless, the indication criteria for EMR and ESD differ and randomized study is ethically difficult to organize. Secondly, both groups of patients are relatively small. To compare with West-ern published series, results of treat-ment of 58 patients with rectal lesions from 6 large centres in the USA were published in 2016 [27]. In Europe, a total of 4 studies published between 2012 and 2015 includes 201 mostly rectal lesions [28−31]. Nevertheless, one other European study published in 2017 could recruit as many as 302 patients for rectal ESD [32]. Thirdly, the follow-up of our patients is not long enough to show long term survival without recurrence. Nevertheless, it has been shown by the others that the risk of recurrence after R0 resection is very low. Recently published long-term data showed an endoscopic recurrence rate of 2.9% and cancer recurrence rate of 1.1% [33]. Finally, all ESDs were performed by a single endoscopist which reflects the reality of most Western centres where low number of suitable lesions prohibits the participation of more endoscopists. The strength of the study is its prospective design with low (7%) drop of follow-up.
In conclusion, our study shows that rectal ESD can be safely performed. It is most beneficial for patients with curative resection of cancer with superficial submucosal invasion. Compared to EMR, ESD offers a significantly higher en bloc resection rate and a significantly lower local residual neoplasia rate. Intraprocedural perforation in the ESD arm occurred in 11%, and could always be treated endoscopically. Although our data are promising, more studies are needed to confirm the position of ESD in the therapeutic algorithm of colorectal lesions.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE „uniform requirements“ for biomedical papers.
Submitted: 23. 3. 2018
Accepted: 30. 3. 2018
As soc. Prof. Ondrej Urban, MD, PhD
2nd Department of Medicine
Gastroenterology and Geriatrics
Faculty of Medicine and Dentistry
Palacky University and University
Hospital Olomouc
I. P. Pavlova 185/ 6 779 00 Olomouc Czech Republic
Sources
1. Torre L, Bray F, Siegel RL et al. Global cancer statistics 2012. CA Cancer J Clin 2015; 65 (2): 87–108. doi: 10.3322/caac.21262
2. Ferlay J, Staliarova-Foucher E, Lortet-Tieulent J et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013; 49 (6): 1374–1403. doi: 10.1016/j.ejca.2012.12.027.
3. Ústav zdravotnických informací a statistiky ČR. Národní onkologický registr (NOR). [online]. Dostupné z: http: //www.uzis.cz/registry-nzis/nor.
4. Zauber AG. The impact of screening on colorectal cancer mortality and incidence: has it really made a difference? Dig Dis Sci 2015; 60 (3): 681–691. doi: 10.1007/s10620-015-3600-5.
5. Zavoral M, Suchanek S, Majek O et al. Colorectal cancer screening: 20 years of development and recent progress. World J Gastroenterol 2014; 20 (14): 3825–3834. doi: 10.3748/wjg.v20.i14.3825.
6. Zauber AG, Winawer SJ, O‘Brien MJ et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012; 366 (8): 687–696. doi: 10.1056/NEJMoa1100370.
7. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon. Gastrointest Endosc 2003; 58 (6 Suppl): S3–S43.
8. Kim BC, Chang HJ, Han KS et al. Clinicopathological differences of laterally spreading tumors of the colorectum according to gross appearance. Endoscopy 2011; 43 (2): 100–107. doi: 10.1055/s-0030-1256027.
9. Schlemper RJ, Riddell RH, Kato Y et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut 2000; 47 (2): 251–255.
10. Watanabe T, Itabashi M, Shimada Y et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clinical Oncol 2012; 17 (1): 1–29. doi: 10.1007/s10147-011-0315-2.
11. Arezzo A, Passera R, Marchese N et al. Systematic review and meta-analysis of endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal lesions. United European Gastroenterol J 2016; 4 (1): 18–29. doi: 10.1177/2050640615585470.
12. Bourke MJ, Neuhaus H. Colorectal endoscopic submucosal dissection: when and by whom? Endoscopy 2014; 46 (8): 677–679. doi: 10.1055/s-0034-1377449.
13. Uraoka T, Parra-Blanco A, Yahagi N. Colorectal endoscopic submucosal dissection in Japan and Western countries. Dig Endosc 2012; 24 (Suppl 1): 80–83. doi: 10.1111/j.1443-1661.2012.01279.x.
14. Repici A, Hassan C, De Paula Pessoa D et al. Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy 2012; 44 (2): 137–150. doi: 10.1055/s-0031-1291448.
15. Williams JG, Pullan RD, Hill J et al. Management of the malignant colorectal polyp: ACPGBI position statement. Colorectal Dis 2013; 15 (Suppl 2): 1–38. doi: 10.1111/codi.12262.
16. Rolny P. The need for surgery after endoscopic treatment of colorectal neoplasms is the most important outcome criterion. Endoscopy 2017; 49 (1): 80–82. doi: 10.1055/s-0042-118451.
17. Nakajima T, Saito Y, Tanaka S et. al. Current status of endoscopic resection strategy for large, early colorectal neoplasia in Japan. Surg Endosc 2013; 27 (9): 3262–3270. doi: 10.1007/s00464-013-2903-x.
18. Nakajima T, Tanaka S, Saito Y et al. Prospective multicenter study on endoscopic treatment of large early colorectal neoplasia conducted by Colorectal Endoscopic Resection Standardiazation Implementation Working Group of Japanese Society for Cancer of the Colon and Rectum. Presented at: UEG Week Stockholm 2011. Endoscopy 2011; 43: S1, A1.
19. Paspatis GA, Dumonceau JM, Barthet M et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 2014; 46 (8): 693–711. doi: 10.1055/s-0034-1377531.
20. Belderbos TD, Leenders M, Moons LM et al. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy 2014; 46 (5): 388–402. doi: 10.1055/s-0034-1364970.
21. Urban O, Kijonkova B, Kajzrlikova IM et al. Local residual neoplasia after endoscopic treatment of laterally spreading tumors during 15 months of follow-up. Eur J Gastroenterol Hepatol 2013; 25 (6): 733–738. doi: 10.1097/MEG.0b013e32835eda96.
22. Park SU, Min YW, Shin JU et al. Endoscopic submucosal dissection or transanal endoscopic microsurgery for nonpolypoid rectal high grade dysplasia and submucosa-invading rectal cancer. Endoscopy 2012; 44 (11): 1031–1036. doi: 10.1055/s-0032-1310015.
23. Arezzo A, Passera R, Saito Y et al. Systematic review and meta-analysis of endoscopic submucosal dissection versus transanal endoscopic microsurgery for large noninvasive rectal lesions. Surg Endosc 2014; 28 (2): 427–438. doi: 10.1007/s00464-013-3238-3.
24. Kiriyama S, Saito Y, Yamamoto S et al. Comparison of endoscopic submucosal dissection with laparoscopic-assisted colorectal surgery for early-stage colorectal cancer: a retrospective analysis. Endoscopy 2012; 44 (11): 1024–1030. doi: 10.1055/s-0032-1310259.
25. Le Roy F, Manfredi S, Hamonic S et al. Frequency of and risk factors for the surgical resection of nonmalignant colorectal polyps: a population-based study. Endoscopy 2016; 48 (3): 263–270. doi: 10.1055/s-0034-1392976.
26. De Mestier L, Brixi H, Gincul R et al. Updating the management of patients with rectal neuroendocrine tumors. Endoscopy 2013; 45 (12): 1039–1046. doi: 10.1055/s-0033-1344794.
27. Chapman CHG, Haber GB, Draganov PV. Evaluation of endoscopic submucosal dissection in the United States: the American experience. Presented at: DDW, San Diego, 21–24 May 2016.
28. Rahmi G, Hotayt B, Chaussade S et al. Endoscopic submucosal dissection for superficial rectal tumors: prospective evaluation in France. Endoscopy 2014; 46 (8): 670–676. doi: 10.1055/s-0034-1365810.
29. Repici A, Hassan C, Paggano N et al. High efficacy of endoscopic submucosal dissection for rectal laterally spreading tumors larger than 3 cm. Gastrointest Endosc 2013; 77 (1): 96–101. doi: 10.1016/j.gie.2012.08.036.
30. Probst A, Golger D, Anthuber M et al. Endoscopic submucosal dissection in large sessile lesions of the rectosigmoid: learning curve in a European center. Endoscopy 2012; 44 (7): 660–607. doi: 10.1055/s-0032-1309403.
31. Bialek A, Wiechovska-Kozlowska A, Pertkiewitz J et al. Endoscopic submucosal dissection for the treatment of neoplastic lesions in the gastrointestinal tract. World J Gastroenterol 2013; 19 (12): 1953–1961. doi: 10.3748/wjg.v19.i12.1953.
32. Probst A, Ebigbo A, Märkl B et al. Endoscopic submucosal dissection for early rectal neoplasia: experience from a European center. Endoscopy 2017; 49 (3): 222–232. doi: 10.1055/s-0042-118449.
33.Yamada M, Saito Y, Takamaru H et al. Long term clinical outcomes of endoscopic submucosal dissection for colorectal neoplasms in 423 cases: a retrospective study. Endoscopy 2017; 49 (3): 233–242. doi: 10.1055/s-0042-124366
Labels
Paediatric gastroenterology Gastroenterology and hepatology Surgery
Article was published inGastroenterology and Hepatology

2018 Issue 3-
All articles in this issue
- Editor-in-Chief’s editorial
- Digestive endoscopy
- Cholangiopancreatoscopy – Czech Society of Gastroenterology Guidelines
- Endoscopic full-thickness resection for the treatment of local residual neoplastia in the colon – an analysis of 19 cases
- Case report of melanoma metastasizing to the pancreas
- Successful treatment of bleeding from aortoesophageal fistula with a metallic self-expandable stent
- Migration of a self-expandable metallic stent into a drained pseudocyst after endoscopic pseudocystogastrostomy and its endoscopic extraction
- Brunner’s gland adenoma – a rare cause of gastrointestinal bleeding
- Contribution to the issue of hepatorenal damage and failure
- Experience in the treatment of severe bleeding in Crohn’s disease with anti-TNF therapy
- Is Amanita phalloides poisoning still a problem?
- A tumorous atrioesophageal fistula as an unusual cause of septicemia
- New member of the Editorial Board
- 40th Czech and Slovak Endoscopic Days 19th Endoscopic Day IKEM
- The selection from international journals
- Vistaprep – the standard of bowel preparation before colonoscopy
- Comparison of endoscopic mucosal resection and endoscopic submucosal dissection in the treatment of flat neoplastic lesions in the rectum
- Gastroenterology and Hepatology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Vistaprep – the standard of bowel preparation before colonoscopy
- A tumorous atrioesophageal fistula as an unusual cause of septicemia
- Is Amanita phalloides poisoning still a problem?
- Experience in the treatment of severe bleeding in Crohn’s disease with anti-TNF therapy
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

