-
Medical journals
- Career
Pathomorphology of inflammatory response following traumatic brain injury, serum values of interleukins, and gene polymorphisms
Authors: David Vajtr 1,2; Drahomira Springer 3; Libor Staněk 4; Oldrich Benada 5; Filip Samal 6; Michal Beran 7; Premysl Strejc 1; Richard Prusa 2; Tomas Zima 3
Authors‘ workplace: Department of forensic medicine and toxicology, Charles University 1st Medical Faculty and General teaching hospital, Prague Czech Republic 1; Department of medical biochemistry and pathobiochemistry, Charles University 2nd Medical Faculty and University hospital Motol, Prague, Czech Republic 2; Department of clinical biochemistry and laboratory diagnostics, Charles University 1st Medical Faculty and General teaching hospital Prague, Czech Republic 3; Department of pathology, Charles University 1st Medical Faculty and General teaching hospital, Prague, Czech Republic 4; Laboratory of molecular structure characterization, Institute of microbiology, Academy of sciences of the Czech Republic, Prague Czech Republic 5; Department of neurosurgery, KNTB Zlin, Czech Republic 6; Department of forensic medicine, Charles University, 2nd Medical Faculty and Hospital Na Bulovce, Prague, Czech Republic 7
Published in: Soud Lék., 59, 2014, No. 4, p. 40-47
Category: Original Article
Overview
Our present study was aimed to investigate time-profile kinetics of interleukins, vascular endothelial growth factor (VEGF) in acute inflammatory response following traumatic brain injury, and the influence of activated microglial cells in patients who developed severe space occupying lesion (SOL) of secondary traumatic brain injury. Interleukins IL-6, monocyte chemo attractant protein (MCP-1), and VEGF had a significant different time-profile kinetics (p<0.05) in patient with, and without expansive traumatic brain contusions (SOL). The serum VEGF was significantly higher in trauma patients with uncomplicated brain contusions, and lower in patients with SOL. The patients with septic complications developed the sudden increase of TNF alpha and IL-8 within the first 72 hours. Our data suggested PSGL and CD68 immunopositivity of microglial cells in both focal and diffuse TBI, predominantly in perivascular space correlated with telolysosome formation in cytoplasma. Polymorphism of PAI-1, MTHFR, eNOS, VEGF, and Apo E genes in TBI were in patients with SOL were bound to show up leucocyte plugging in capillaries.
Keywords:
traumatic brain injury – acute inflammatory response – microglial cells – interleukins – vascular endothelial growth factor – monocyte chemoattractant protein – gene polymorphisms
Acute traumatic brain injury (TBI) is characterised by two injury phases, primary and secondary caused by an interaction between ischaemic, inflammatory and cytotoxic processes. TBI triggers a series of inflammatory reactions following traumatic brain injury involving blood brain barrier (BBB) impairment, manifested by astroglial or endothelial failure. Cytokines and growth factor VEGF play a role in neuroinflammation, promoting angiogenesis and vascular stability after traumatic brain injury. Lenzlinger et al. (1) summarised brain damage following traumatic injury as a result of direct (immediate mechanical disruption of brain tissue, or primary injury) and indirect (secondary or delayed) mechanisms comprising the initiation of an acute inflammatory response, including breakdown of BBB, edema formation and swelling, infiltration of peripheral blood cells and activation of resident immunocompetent cells, release of numerous interleukins and chemotactic factors. Published data suggested that TBI is associated with disruption of the blood–brain barrier (2,3,4,5) and access of proinflammatory cells to brain parenchyma (6). TBI is associated with up-regulation of interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor–α. Winter et al. (7) have reported that elevated levels of IL-6 are associated with improved outcome 6 months after TBI. The increase of levels of IL-6 was significantly (p < 0.05) correlated with increasing volumes of brain lesion and was also significantly associated with poor functional and neurological outcome (8). MCP-1 (monocyte chemoattractant protein-1) play a role for blood monocyte recruitment. Semple et al. (9) reported maximal levels of MCP-1 protein in the brain by 4 h post-injury. VEGF plays an important role in aspects of astroglial scar formation after TBI. Endogenous VEGF up regulation by astrocytes induces angiogenesis, and increases astrocyte proliferation (10). Grad et al. (11) reported significantly higher increases of serum VEGF in patients with uncomplicated healing, than patients who developed severe complications during the post-traumatic course, such as sepsis, adult respiratory distress syndrome or multiple organ failure (p < 0.05). Genetically determined individual differences of polymorphism of gene APO E, Angiotensin-converting enzyme, NO synthase, PAI-1 (plasminogen activator inhibitor), and MTHFR (methylenetetrahydrofolate reductase) are important factors of outcome after TBI and components of the response following neurotrauma leading to secondary TBI (12). The APOE gene is located on chromosome 19, and three major APOE alleles (ε2, ε3, and ε4) code for 3 Apo E isoforms. Apo E play a role in lipid transport in the brain, and recovery after a brain injury. Apo E-ε4 is a risk factor for chronic traumatic encephalopathy (13), and worse functional and cognitive outcomes after severe traumatic brain injury (14), and it may modify the type and severity of brain damage from a severe traumatic brain injury (15). Angiotensin-converting enzyme (ACE) plays a central role in the regulation of blood pressure through the conversion of angiotensin I to angiotensin II. The ACE gene is located on chromosome 17, and insertion/deletion mutation in intron 16 may be associated with greater levels of circulating ACE (16). According to Ariza et al (17), there was the association with D allele with poorer outcome in a 73 patients with moderate and severe TBI, the increased ACE activity associated with the D allele may be associated with the risk of vasospasm and cerebral blood flow impairment after TBI-related injury.
MATERIAL AND METHODS
Group of patients
The enrolled patients with traumatic brain injury (TBI, n=22) were divided into group I of space-occupying lesion (SOL) patients showing progressive expansive cortical contusion submitted to neurosurgery (n=8). In group I enrolled patients with multiple traumas there were 7 cases of predominant injury to the head, and one case with predominant injury of head and another thoracic or abdominal organ. Patients submitted to neurosurgery due to SOL were diagnosed with midline shifts more than 10 mm, mydriasis, and an intracranial pressure (ICP) elevation more than 10 torr. Within the first 10 days of hospitalisation, 3 patients in group I died (GOS 1, poor outcome). Patients of group II without expansive process (non-space-occupying lesion, n=14) did not exhibited the CT scan signs of space-occupying lesion. In group II enrolled patients with multiple traumas there were 9 cases of predominant injury to the head, and 5 cases with predominant injury to another thoracic or abdominal organ. Within the first 10 days of the study there was none patients with outcome GOS 1 in the group II.
Autopsies of DAI cases
Samples (n=7) from autopsy of patients with diagnose of diffuse axonal injury (DAI) were obtained with agreement of Department of Forensic Medicine. The patients with diffuse axonal injuries were diagnosed with signs of DAI using nuclear magnetic resonance (NMR) performed 2-3 weeks after injury. Formalin-fixed brain autopsies of deceased DAI patients were cut coronally in a way as to make paraffin-embedded sections.
Electron microscopy
Cortical biopsies were carried out in 8 patients with craniocerebral trauma submitted to surgery for expansive lesion (SOL). The tissue samples from the pericontusional zone on the border line of necrotic contusion tissue were fixed in 3% glutaraldehyde in cacodylate buffer and postfixed with 2% osmium tetroxide. After dehydration in alcohol series, the samples were embedded into Epon resin in accordance with standard procedure. The stained ultrathin sections were examined in Philips CM100 electron microscope (FEI, formerly Philips EO, the Netherlands) and selected areas were digitally recorded using MegaViewII slow-scan camera. The digital images were processed in Analysis 3.2 Pro software.
Immunohistochemistry
Formalin-fixed cortical biopsies and also tissues obtained during autopsies of patients who died and patients submitted to neurosurgery were cut coronally in a way as to make paraffin-embedded sections, which were labelled with anti-VEGF, anti-CD68, anti-beta amyloid precursor protein (beta-APP), and anti-P-selectin glycoprotein ligand antibodies (Chemicon). The colour was developed using a chromogenic substrate di-amino-benzidine (DAB). Positive tissues for immunohistochemistry were used as positive controls (ihcworld.com/_technical_tips/positive_control_tissue_list.htm).
Biochemical investigation
Blood samples were collected each day for the first 3 days after admission to the hospital. Serum cytokines and growth factors concentrations were measured by the Evidence Investigator™ Biochip Array technology. The core technology is the Randox Biochip, a solid-state device containing an array of discrete test regions of immobilised specific antibodies. A sandwich chemiluminescent immunoassay is employed for the cytokine array. The specific antibodies are labelled with horseradish peroxidase (HRP) and the chemiluminescent signal is emitted and is detected using digital imaging technology. The Evidence Investigator™ Cytokine High-Sensitivity Array tests quantitatively for IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, VEGF, IFNγ, EGF, MCP-1 and TNFα simultaneously.
Genetic investigation
Capillary electrophoresis: Genomic DNA was extracted from peripheral blood leukocytes using the commercial QIAamp DNA Blood Mini Kit (QIAGEN, Germany). Patients were genotyped for mutations in the Factor V Leiden (R506Q), Prothrombin (Faktor II 20210A) and MTHFR (C677T) gene using commercial Elucigene TRP-F kit and analysis by capillary electrophoresis.
ARMS PCR: Genomic DNA was extracted from peripheral blood leukocytes using the commercial QIAamp DNA Blood Mini Kit (QIAGEN, Germany). DNA was mixed with ELUCIGENE TRP-F PCR amplification mix. The Elucigene kit uses ARMS™ allele specific amplification technology to detect mutations in the human genes. Fluorescent analysis was performed using capillary electrophoresis ABI 3131xl. Genotyping of the 4G/5G polymorphism in the PAl-1 promoter region was performed by PCR using the following oligonucleotides: 5´-CACAGAGAGAGTCTGGCCACGT-3´ (forvard); 5´-CCAACAGAGGACTCTTGGTCT-3´ (reverse). Genotyping of A1298C polymorphism in methylenetetrahydrofolate reductase gene was performed by PCR using the following oligonucleotides: 5´ - ATGTGGGGGGAGGAGCTGAC-3´ (F); 5´-GTCTCCCAA CTTACCCTTCTCCC-3´ (R). Reactions were performed in volumes of 25 µL with 0.1 mol of each oligonucleotide, 1 U of Taq DNA polymerase, 2 mmol of MgCl2 and 0.2 mmol of each dNTP. (Fermentas, USA). Amplification products (20 µL) were subjected to digestion of the specific restriction enzyme BsI I (Fermentas, USA) at 55°C (PAI-1) and MboII (Fermentas, USA) at 37°C (MTHFR). The DNA fragments were separated by electrophoresis in 3% agarose gels (Amresco, USA) for 70 minutes and visualized using GelRed (Biotium, USA).
qRT-PCR: RNA was isolated from paraffin block using isolation kit RNeasy Mini Kit (QIAGEN), barrels method. Reverse transcription (RT-PCR) carried kit RevertAid H Minus First Strend cDNA Synthesis Kit (Fermentas). cDNA was subsequently quantified for VEGF gene using absolute qRT-PCR using the kit, Real-Time PCR Using RT2 qPCR Primer Assays VEGF (QIAGEN) in Light Cycler LC480 II (Roche).
StripAssay: Genomic DNA was isolated using QIAamp DNA Mini Kit (QIAGEN), followed by amplification and hybridization of the strips using a kit CVD StripAssay A (Pentagen, VienaLab) was used robotic hybridisation Bee20 (BeeRobotics) and evaluation performed Software (Pentagen).
Informed consent
The ethics committee at each institution approved this study, and written informed consent was obtained from surviving patients.
Statistical methods
Data were expressed as mean ± standard deviation (SD). Differences in serum protein concentrations between groups were tested by the unpaired t-test with Welsh correction, and by Deming model of linear regression. Differences at p< 0.05 were considered statistically significant.
RESULTS
The Biochemical kinetics of VEGF, IL-6, and MCP-1 in TBI
The Serum values of VEGF, IL-6, and MCP over first 3 days of sampling are summarized in Table 1. In terms of all data of growth factor serum level ranging between 1 up to 3 day, the highest values of VEGF (303.0±55 vs. 155.4±33 ng/l, p<0.03) were found in group II as compared to group I (SOL). The peak value of VEGF 1339.4 ng/l was found in patient with diffuse axonal injury. The time-dependent profile of serum VEGF revealed a significant increase in group II (138.1±38 vs. 358.8±95 ng/l, p<0.05) from 1st day up to 2nd-3rd day. We found non-significant development of VEGF serum values in group of SOL patients from 1st day up to 2nd-3rd day, although the relevant decrease of VEGF values was revealed in 2 patients who died. In terms of IL-6 and MCP-1 serum values, the significant increase of IL-6 values (133.5±42 vs. 359.2±85 ng/l, p<0.04) was found in group I (SOL) from 1st day up to 2nd-3rd day. We found non-significant development of IL-6 serum values in group II of patients with non-space occupying brain contusions from 1st day up to 2nd-3rd day. In terms of comparison of IL-6 values between group I and II, there were significantly higher value of IL-6 in group I patient submitted to neurosurgery during the 48-72 hours (359.2±85 vs. 85.57±25 ng/l, p<0.05). We found non-significant development of MCP-1 serum values in group of SOL patients with non-space occupying brain contusions from 1st day up to 2nd-3rd day. The significant decrease of MCP-1 values (853.3±155 vs. 334.5±83 ng/l, p<0.01) was found in group II from 1st day up to 2nd-3rd day. In terms of comparison of MCP-1 values between group I and II, there were significantly higher value of MCP-1 in group I pacient submitted to neurosurgery during the first day (853.3±155 vs. 387.3±117 ng/l, p<0.05). With respect of all data, there was a correlation between IL-6 and MCP-1 serum values (proved by Deming model of linear regression, p <0.05).
1. Biochemical data of either group with respect to time-profile during 3 days after admission. Square (□) indicates differences between both groups of patients diagnosed as SOL, and without SOL (p < 0.05). Triangle (▲) indicates differences in one group of patients with respect to time-profile during 3 days after admission (p < 0.05). 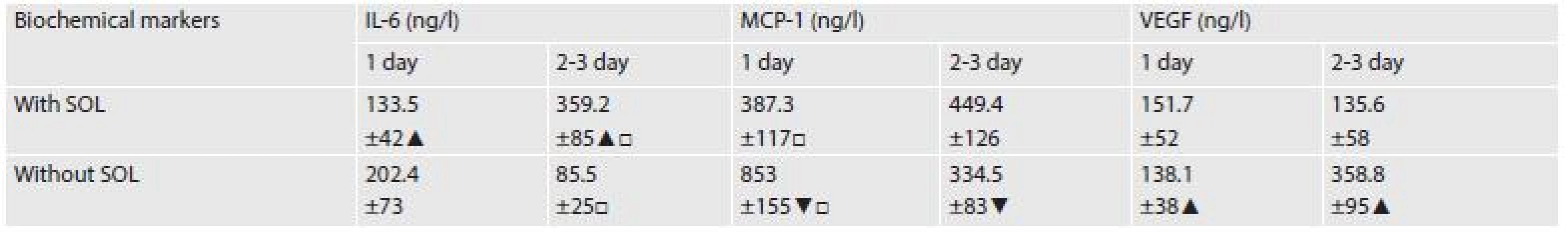
The Biochemical kinetics of IL-2, 8, 10, and TNF alpha in TBI
The serum values of IL-2, 8, 10, and TNF alpha during first 3 days of sampling are summarized in Table 2. We found non-significant development of IL-2, 8, 10, and TNF alpha serum values in group I of SOL patients from 1st day up to 2nd-3rd day, and non-significant development of IL-2, 8, 10, and TNF alpha serum values in group II without SOL. In terms of all data of IL-2, 8, 10, and TNF alpha serum level, there were none significant changes of serum values in group I as compared to group II. Cases of higher values of TNF alpha: In a SOL cases of group I with contusions areas constituting from significant intraparenchymal haemorrhages rather than component of capillary microhaemorhages, and with bigger leucocyte recruitment and transmigration, and lower immunoreactivity of CD68(+), and PSGL(+) positive microglial cells there were 3 cases of patients developing the sudden increase of TNF alpha and IL-8 within the first 72 hours. The values of TNF alpha range from 5.10 ng/l up to 45.5 ng/l, and the values of IL-8 alpha range from 26.3 up to 302.7 ng/l within the first 72 hours.
2. Data of either group with respect to time-profile during 3 days after admission. Square indicates differences between both groups of patients diagnosed as SOL, and without SOL (p < 0.05). Triangle indicates differences in group of patients with respect to time-profile during 3 days after admission (p < 0.05). 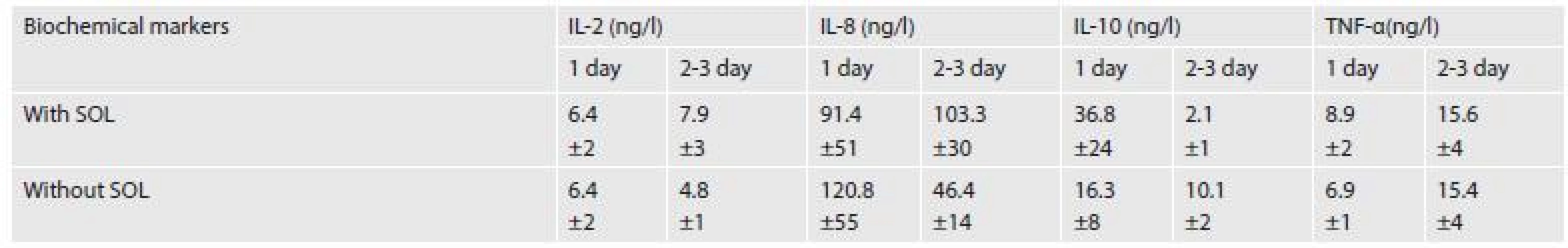
Immunohistochemistry of P-selectin glycoprotein ligand, and CD68 in focal TBI
In our study we have been performing investigation of P-selectin glycoprotein ligand (PSGL), and CD68 immunopositivity of microglial cells in samples of cortical biopsies of patients undergoing neurosurgery due to SOL contusion. We identified attenuated leucocyte recruitment in SOL with component of contusions areas with predominantly capillary microhaemorhages rather than contusions areas constituing from intraparenchymal haemorrhages. There were bigger immunoreactivity of CD68(+), and PSGL(+) immunopositive microglial cells. Scattered local immunoreactivity with anti-PSGL, and anti-CD68 has been detected in grey and white matter. CD68-related local immunoreactivity demonstrated fagocytic activity of microglial cells in injured patient with SOL. We proved strong CD68(+) immunopositivity of microglial cells surrounding capillaries in patients with SOL. We identified PSGL immunopositivity of perivascular ramified microglial cells (Fig. 1) in a case of 74 years old pedestrian knocked down during trafic accident who suffered brain contusions. In other case there were juxtavascular PSGL immunopositive microglial cells inside brain neurophil demonstrating the ramification and branching of microglial projections in 51 year old women (Fig. 2) cycling over the railway crossing who was knocked down by a lorry. She sustained a base skull fracture, and lost consciousness, GCS 3. There were SDH, midline shift by over 5 mm, SOL contusions in the left front and the left temporal lobes. She underwent neurosurgery due to SOL. The state of consciousness improved in one week up to GCS 15. In a SOL cases with contusions areas constituting predominantly from significant intraparenchymal haemorrhages there were bigger leucocyte recruitment and transmigration, and lower immunoreactivity of CD68(+), and PSGL(+) positive microglial cells. VEGF protein was expressed in astroglial cells in all patients with SOL.
1. A case of 74 years old pedestrian knocked down during trafic accident who suffered brain contusions. MC – microglial cell. Arrowhead indicates PSGL immunopositivity of perivascular ramified MC (see in detail). 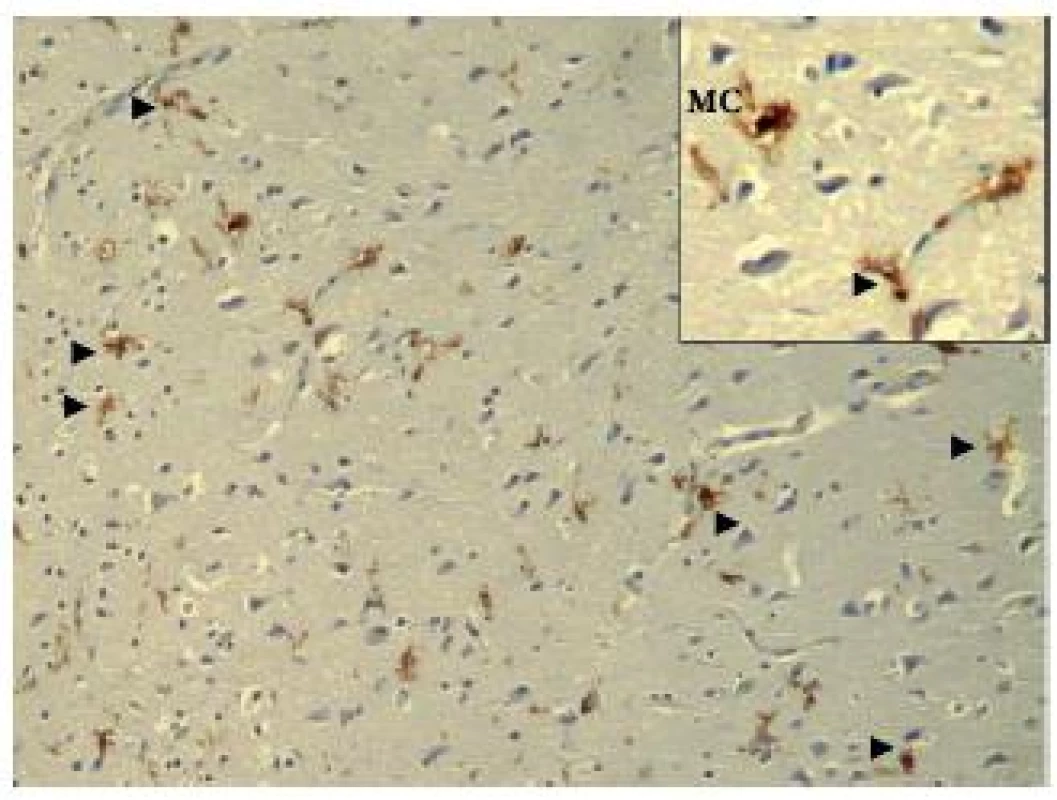
2. A 51 years old women cycling over the railway crossing who was knocked down by a lorry. Arrowhead indicates juxtavascular PSGL immunopositive microglial cells. Ramification and branching of microglial projections inside brain neurophil. MC – microglial cell. PSGL immunopositivity of MC (see in detail). Square indicates pericellular oedema. 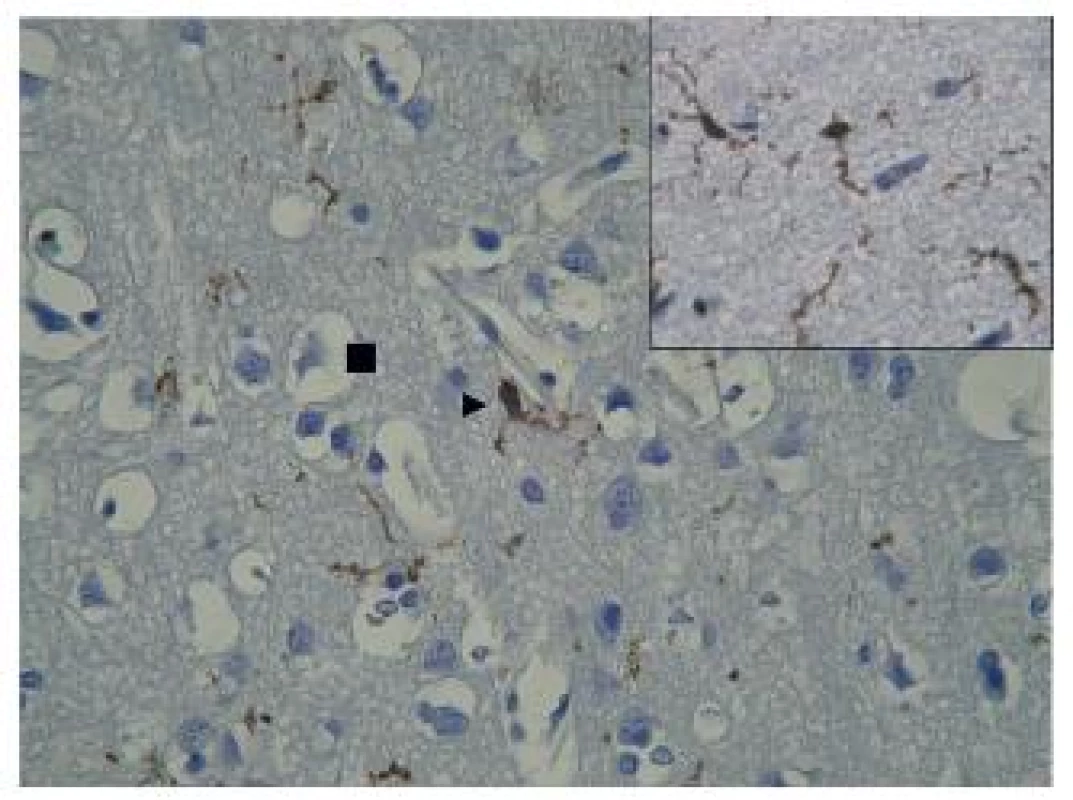
Immunohistochemistry of VEGF expression in focal and diffuse TBI, and qantification of VEGFA expression
The immunohistochemistry demonstrated a moderate labelling of anti-VEGF antibodies in astroglial and endothelial cells (Fig. 3). However, in these patients, we identified low values of serum VEGF. The lowest values were proved in three patients with GOS 1 (poor outcome): the man suffering a fall from height; a man falling down to the ground striking his head; a woman knocked down by a lorry while cycling. VEGF immunopositivity was identified inside cytoplasma of neurons, astroglial cells, and in perivascular spaces. Perivascular and pericellular oedema was revealed in contusions area. Patchy disperse immunopositivity of VEGFA have been identified in astroglial cells of patients diagnosed as DAI. The real-time polymerase chain reaction (qRT-PCR) for the quantification of VEGF-A mRNA in brain tissues proved higher gene expression in patients with expansive contusions in comparison with patients diagnosed as DAI (Fig. 4). The highest gene expression of VEGF-A mRNA in plasma was identified in patients with expansive contusions (SOL).
3. A 75 years old man falling down to the ground striking his head. VEGF immunopositivity was identified inside cytoplasm of neurons, astroglial cells, and in perivascular spaces. Perivascular and pericellular oedema was revealed in contusions area. 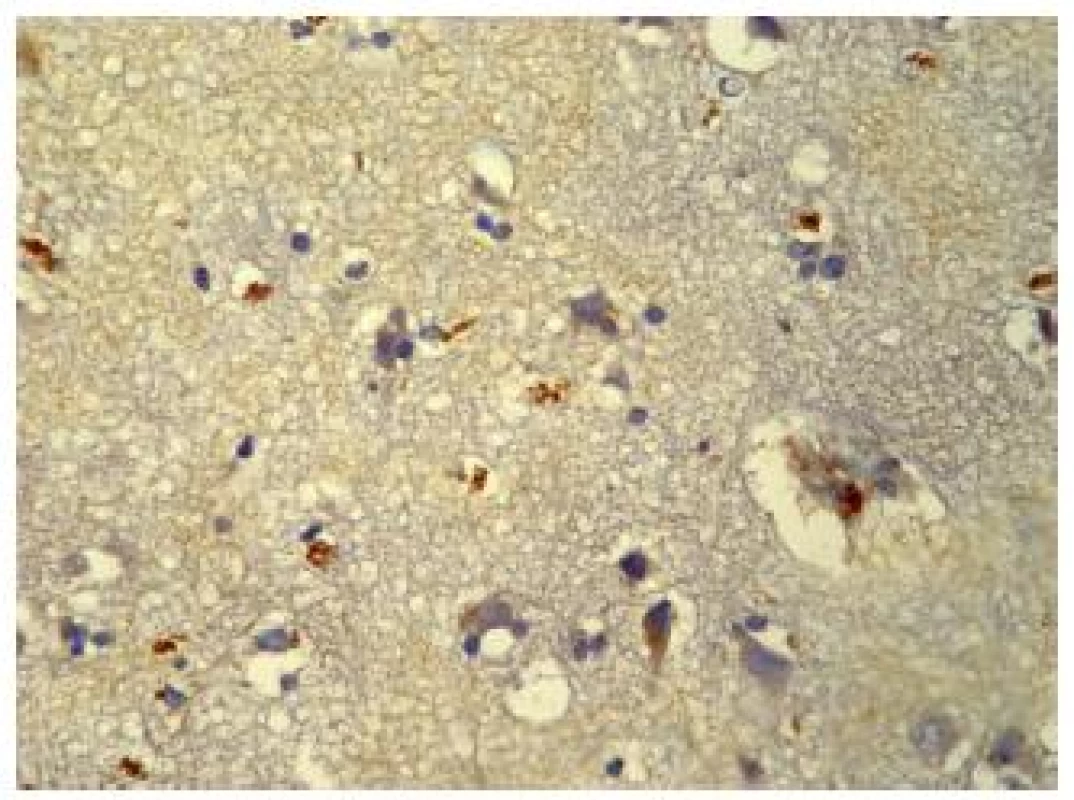
4. Panel A demonstrated the results of strip assay using a kit CVD StripAssay. B: Panel B demonstrated amplification plots of VEGF gene using the kit Assays VEGF in Light Cycler LC480 II. C: In patients with SOL was identified plugging of leucocytes in capillaries. Curved line 1 demonstrates standard sample, concentration of cDNA 1.00 μg/μl. Curved line 2 demonstrates sample of contused brain tissue, concentration of cDNA 7.84 μg/μl. Curved line 3 demonstrates sample of diffuse axonal injuried brain tissue, concentration of cDNA 1.92 μg/μl. 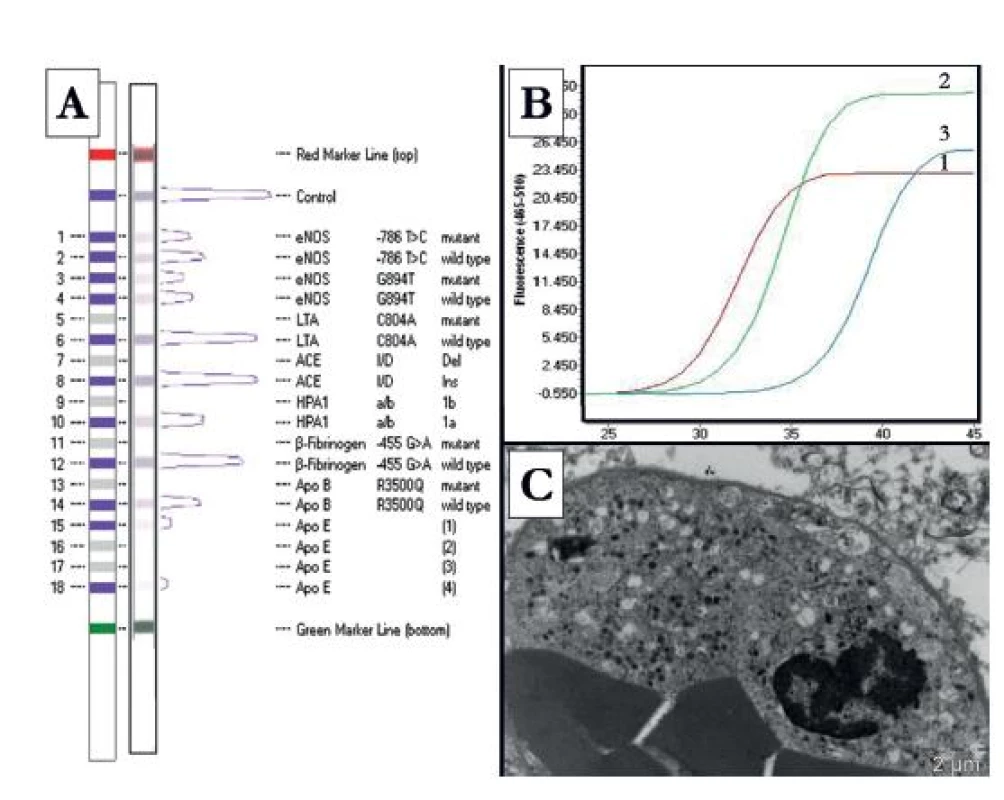
Ultrastructural findings in focal TBI
Ultrastructural signs of early inflammatory response following TBI were studied by electron microscopy in patients submitted to neurosurgery due to SOL (expansive contusion). In the early stages (patients submitted to neurosurgery up to 24–48 hours after admission due to SOL with component of contusions areas characterised by predominant capillary microhaemorhages rather than contusions areas constituting from intraparenchymal haemorrhages) an ultrastructural investigation of perivascular microglial cells revealed digestion and breakdown of the foreign proteins. Perivascular microglial cells exhibited telolysosome with hydrophilic and hydrophobic component. There was correlation between numerous telolysosomes inside cytoplasma of cells and local immunoreaction with anti-CD68 antibody. Microglial cell had been activated, nucleus appeared to be indented, there were identified vacuoles, and telolysosomes in cytoplasma (Fig. 5). Axonal swelling was accompanied by the formation of axolemmal blebs. Axons and myelin sheath were broken up into small fragment. There were identified mitochondrial like vacuoles in axoplasma. In a SOL cases with contusions areas constituting from significant intraparenchymal haemorrhages there were bigger leucocyte recruitment and transmigration (Fig. 6). We observed neutrophil rolling and tethering on to endothelial cells, transmigration into extravascular tissue, and signs of neuronophagia in which a dying neuron is surrounded by lymphocyte and neurotrophil cells. We observed extravasation of red blood cells passing through capillary lumen, and proteinaceous fibrillary material in oedematous tissue. There were revealed plugging of polymorphonuclear neutrophiles (Fig. 4C) and red blood cells in capillaries. We found degranulation of neutrophils, and lysis of erythrocytes in contusion zone, and there were identified macrophages bearing dense lysosome like organelles, and forming vesicles. There were identified mitochondrial like vacuoles in swollen axoplasma. Axonal swelling was accompanied by the formation of axolemmal blebs. Axons and myelin sheath were broken up into small fragment phagocytes by microglial cells. There were identified phagocytosis and lysis of red blood cells, degranulation of polymorphonuclears, formation of phagolysosomes, and in cytoplasm there were a large granules, and rod–shaped granules in a 43 years old man who suffered TBI as a car driver.
5. Microglial cells exhibited telolysosome with hydrophilic and hydrophobic component. Activated microglial cell, nucleus appeared to be indented (arrowhead). Vacuoles, and telolysosomes in cytoplasm (square). Asterisk indicates nucleolus (see in detail). 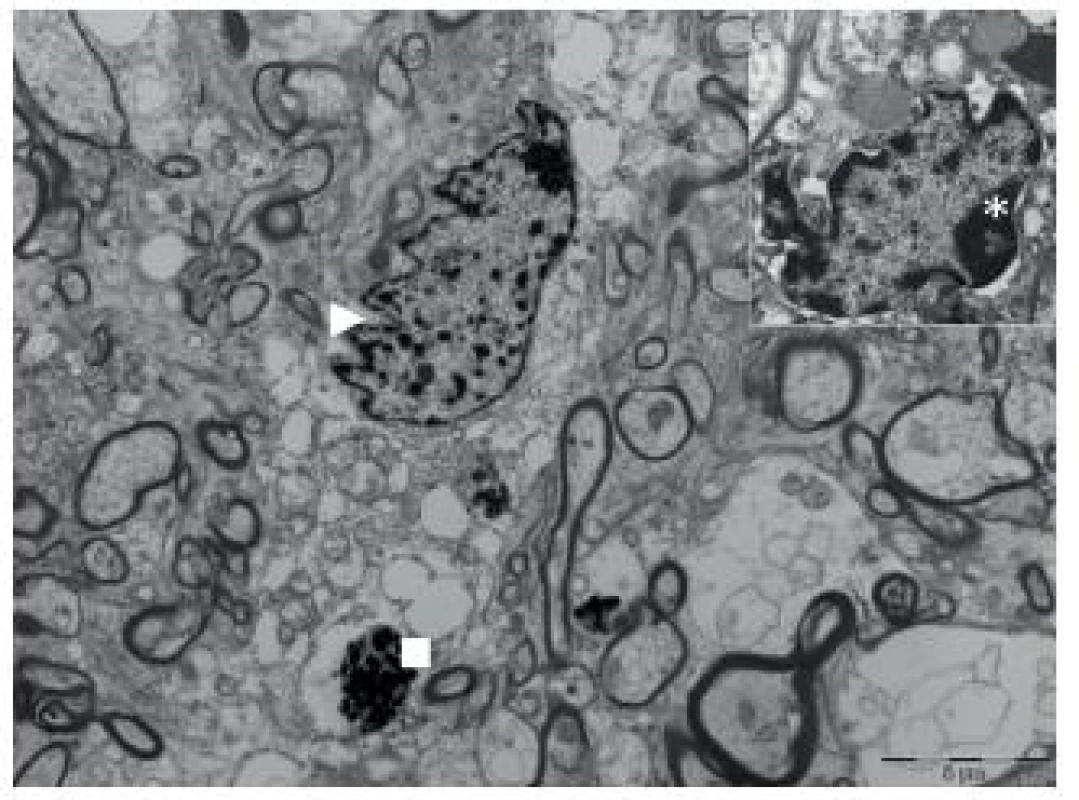
6. 43 years old man who suffered TBI as a car driver. A,B: Extravasation of red blood cells (RC). Oedematous brain tissue. Phagocytosis and lysis of red blood cells, and degranulation of polymorphonuclears. Degranulation of neutrophiles. Lysis of erythrocytes in contusion zone (arrowhead). C: Phagolysosomes, and in cytoplasma there were a large granules, and rod shaped granules (asterisk). D: Signs of neuronophagia. Necrotic neuron surrounded by neurotrophil cells (square). 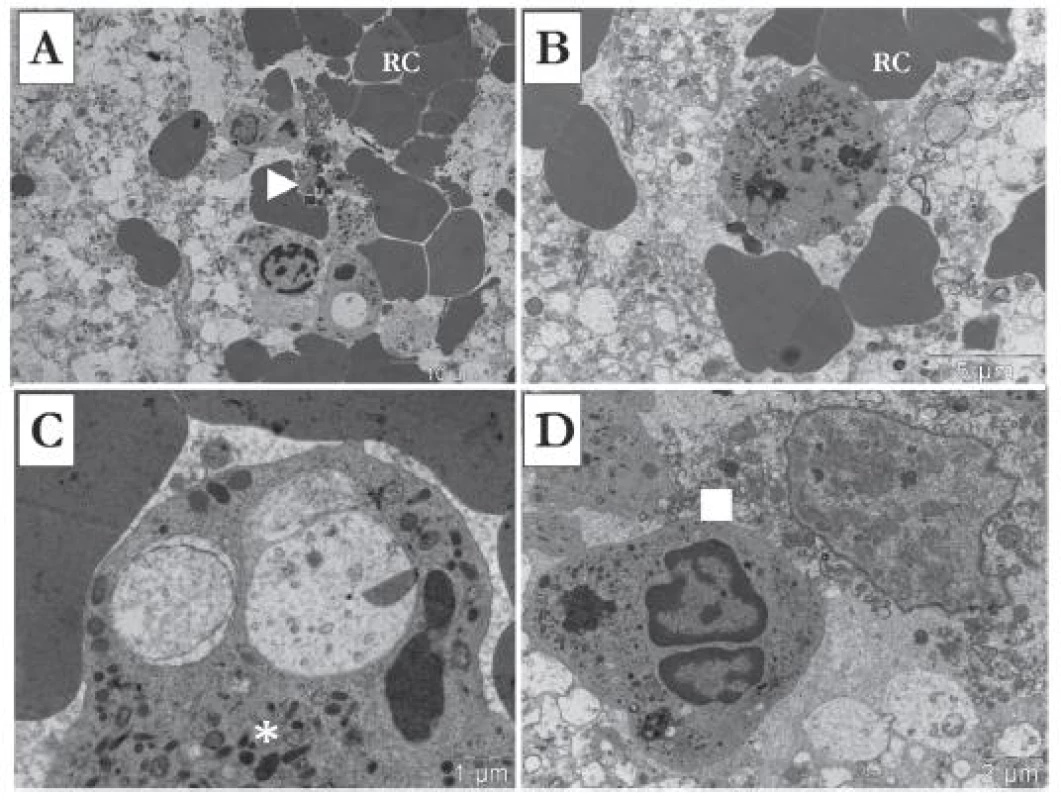
Immunohistochemistry of P-selectin glycoprotein ligand, CD68, and beta-APP in diffuse TBI
In patients diagnosed with DAI were not identified torn of stretch axons. There were proved wave-like and varicose axons with granular beta-APP immunopositivity inside axoplasma (Fig. 7). Many axons have been appeared swollen and formed a bulb like retraction ball. There were perivascular CD68(+) immunopositive microglial cells, juxtavascular rod-like CD68(+) immunopositive microglial cells, and ramified resting PSGL(+) immunopositive microglial cells in cortical and subcortical grey matter. Patchy disperse immunopositivity of VEGF have been identified in astroglial cells.
7. Wave-like and varicose axons (asterisk) with granular beta- amyloid precursor protein (β-APP) immunopositivity inside axoplasma. Axons have been appeared swollen and formed a bulblike retraction ball (arrowhead, see in detail). 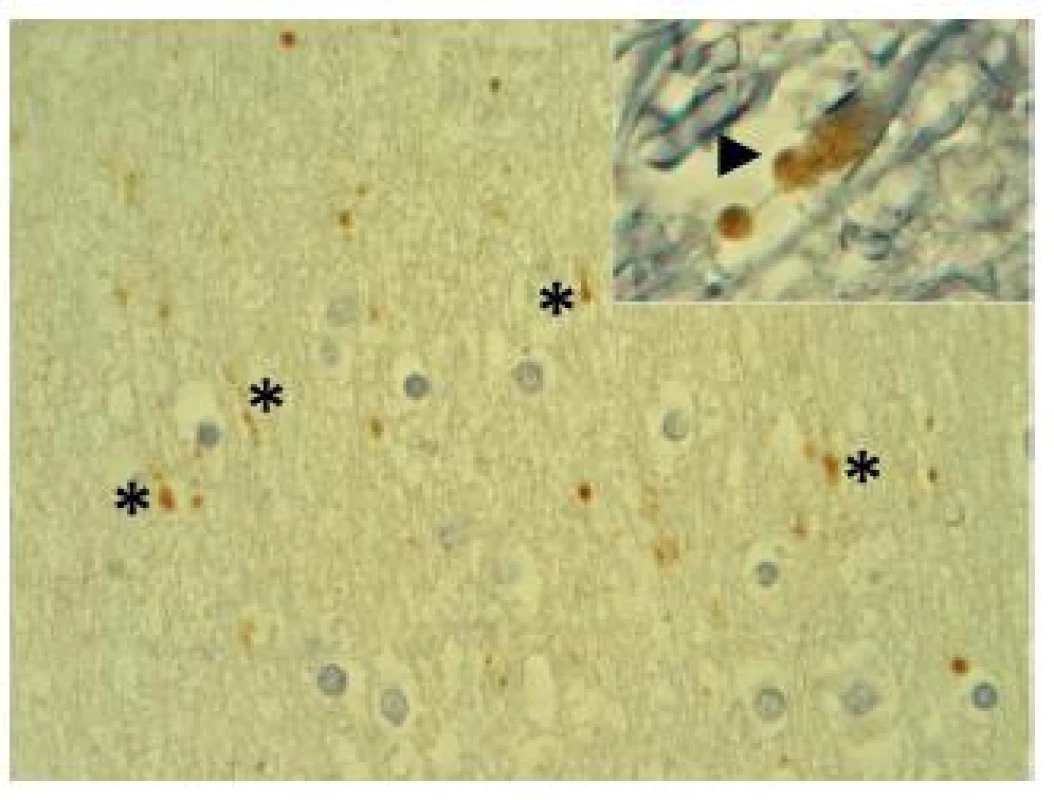
Polymorphism of PAI-1, MTHFR, eNOS, ACE, and Apo E genes in TBI
PAI-1 gene restriction fragment lenght polymorphism investigation of 4G/5G in the promoter region demonstrated in two patients the 5G/5G less transcriptionally active allele, and in one patient transcriptionally active 4G/5G allele. Genetic variation of DNA single nucleotide polymorphisms (SNP) of gene methylenetetrahydrofolate reductase revealed two of the most investigated polymorphisms C677T and A1298C in two patients. The 677T allele encoding a thermolabile enzyme with reduced activity was identified in one patient, and 1298C allele was too identified in one patient. Presence of a T-786C mutation producing a significant reduction in the NOS3 gene promoter activity, in the endothelial NOS (Nitric Oxide Synthase) gene was proved in 3 patients (fig. 4A). In terms of the polymorphism in exon 7 of the NOS3 gene, we detected the Glu298Asp polymorphism (G894T) in eNOS in 3 patients. We performed investigation of three major APOE alleles (ε2, ε3, and ε4) coding 3 Apo E isoforms. Strip assay investigation suggested the presence of the Apo E-ε4 allele in 3 patients. We studied angiotensin converting enzyme polymorphism (the absence (deletion, D) or presence (insertion, I) of a 287 base-pair DNA fragment inside intron 16). The one patient was diagnosed as DI heterozygotes, and two patients were diagnosed as I/I wild genotype. None patient in our group was diagnosed for mutations in the Factor V Leiden (R506Q), or Prothrombin (Factor II 20210A) by capillary electrophoresis.
DISCUSSION
The importance of infiltration and accumulation of polymorphonuclear leukocytes (PMNs) into brain parenchyma in TBI have been documented (18,19). Infiltration occured in the acute post-traumatic period reached a peak by 24 h post-injury. Zhuang et al. (20) have suggested a relationship between cortical PMN accumulation and secondary brain injury, including lowered cerebral blood flow (CBF), increased edema, and elevated ICP. Microthrombosis in the cerebral microcirculation caused immediate post-traumatic decrease in peri-contusional blood flow (21). Contusions are commonly associated with hemodynamic changes including focal reductions in cerebral blood flow (22), and TBI is often associated with abnormalities in coagulation parameters (23). In our study we confirmed the importance of identification of accumulated polymorphonuclear leukocytes, and activated microglial cells in SOL, and the measurement of interleukin levels. Activated microglia have been characterised as being the predominant source of interleukins (24). In terms of comparison of MCP-1 and IL-6 values between groups I and II inour study, there were significantly higher value of MCP-1 and IL-6 in group I patients submitted to neurosurgery during the first day. According our previous references, the BBB breakdown, elevated ICP, and oedema were diagnosed in cases of SOL patients (4,5). The activation and proliferation of resident glia were typical of inflammatory events in both focal and diffuse TBI. Our data suggested PSGL and CD68 immunopositivity of microglial cells in both focal and diffuse TBI (25). According a different study, the serum VEGF is significantly higher in trauma patients with uncomplicated healing (11). In our study, the highest values of VEGF (303.0±55 vs. 155.4±33 ng/l, p < 0.03) were found in group II (without SOL) as compared to group I (SOL). The time-dependent profile of serum VEGF revealed a significant increase in group II (138.1±38 vs. 358.8±95 ng/l, p < 0.05) from 1st day up to 2nd-3rd day. Grad et al. (11) suggested no significant correlation between the peak of serum VEGF and initial Injury Severity Score of mechanical injury. In the subgroup of trauma patients with uncomplicated healing the authors showed significantly higher increases of serum VEGF than the subgroup who developed severe complications during the post-traumatic course, such as sepsis, adult respiratory distress syndrome or multiple organ failure (p < 0.05). In our study, there were 3 cases of group I with septic complications, who developed the sudden increase of TNF alpha and IL-8 within the first 72 hours. The values of TNF alpha ranged from 5.1 ng/l up to 45.5 ng/l, and the values of IL-8 alpha ranged from 26.3 up to 302.7 ng/l within the first 72 hours. We revealed the correlation of proinflammatory cytokines IL-6 and MCP-1 with space occupying lesion after primary TBI. We demonstrated the significant increase of IL-6 values (133.5±42 vs. 359.2±85 ng/l, p < 0.04) in group I (SOL) from 1st day up to 2nd-3rd day, and significantly higher value of MCP-1 in group I patient submitted to neurosurgery during the first day (853.3±155 vs. 387.3±117 ng/l, p < 0.05). There was a correlation between IL-6 and MCP-1 serum values (proved by Deming model of linear regression, p <0.05). Ho L et al. (26) reported the correlation between blood concentration of MCP-1 and the severity of TBI and the index of compromised axonal fibre integrity in the frontal cortex. The increase of levels of cytokine IL-6 was significantly (p < 0.05) correlated with increasing volumes of brain lesion and was significantly associated with poor functional and neurological outcome (8). In the retrospective study, Woiciechowsky et al. (27) demonstrated that severe brain injury (GCS score and mortality on day 7) was associated with high plasma levels of proinflammatory cytokines within 2 to 6 hours after the acute event. Authors reported, that all patients who died or developed infectious complications within the first week showed plasma IL-6 levels more than 100 ng/l on day 1. In our study, we found concentration of IL-6 higher than 100 ng/l on day 1 in both groups SOL and without SOL. The genetic polymorphism of gene APO E, Angiotensin-converting enzyme, NO synthase, PAI-1 (plasminogen activator inhibitor), and MTHFR in (TBI) may contribute to variability in outcome of TBI patients (12). In our study we confirmed PAI-1 gene restriction fragment length polymorphism in one patient with transcriptionally active 4G/5G allele, DNA single nucleotide polymorphisms (SNP) of gene MTHFR C677T and A1298C in two patients, presence of a T-786C mutation in the NOS3 gene promoter (Nitric Oxide Synthase) in 3 patients, and the Glu298Asp polymorphism (G894T) in 3 patients, the presence of the Apo E-ε4 allele in 3 patients, and D/I polymorphism of a 287 base-pair DNA fragment inside intron 16 of angiotensin converting enzyme. All gene polymorphisms were detected in patients diagnosed as SOL, and electron microscopic investigation suggested plugging of polymorphonuclear leucocytes in capillaries. Gene polymorphism could worse endothelial dysfunction in thrombophilic mutation of gene PAI-1 and MTHFR. In patients with polymorphism of PAI-1, MTHFR, eNOS, and Apo E genes were identified plugging of leucocytes in capillaries.
CONCLUSION
Interleukins IL-6, MCP-1, and VEGF has a different time-profile kinetics in patient with, and without expansive traumatic brain contusions (SOL). The serum VEGF was significantly higher in trauma patients with uncomplicated brain contusions, and lower in patients with SOL, and in patients with SOL were higher expression of VEGFA mRNA. The patients with septic complications developed the sudden increase of TNF alpha and IL-8 within the first 72 hours. Polymorphism of PAI-1, MTHFR, eNOS, and Apo E genes in TBI were in patients with SOL were bound to show up leucocyte plugging in capillaries.
ACKNOWLEDGEMENTS
Our work was supported by Reserch Project of The Ministry of Health RVO-VFN64165, and by Institutional Research Concept (AV0Z50200510).
✉ Correspondence address:
MUDr. David Vajtr, Ph.D.
Department of Forensic medicine and toxicology
Charles University, 1 st Medical Faculty
Studnickova 4, Praha 2, 120 00
email: vajtr777@seznam.cz
tel: +420 603961347
fax: +420 224435320
Sources
1. Lenzlinger PM, Morganti-Kossmann MC, Laurer HL, McIntosh TK. The duality of the inflammatory response to traumatic brain injury. Molecular Neurobiology 2001; 24 : 169–181.
2. Quan N, Herkenham M. Connecting cytokines and brain: A review of current issues. Histol Histopathol 2002; 17 : 273–288.
3. Kukacka J, Vajtr D, Huska D, et al. Blood metallothionein, neuron specific enolase, and protein S100B in patients with traumatic brain injury. Neuro Endocrinol Lett 2006; 27 : 116–120.
4. Vajtr D, Benada O, Kukacka J, et al. Correlation of ultrastructural changes of endothelial cells and astrocytes occuring during blood brain barrier damage after traumatic brain injury with biochemical markers of BBB leakage and inflammatory response. Physiol Res 2009; 58(2): 263–268.
5. Vajtr D, Filip M, Benada O, et al. Immunohistochemistry And Serum Values Of S-100B, Glial Fibrillary Acidic Protein, And Hyperphosphorylated Neurofilaments In Brain Injuries. Soud Lek 2012; 57(1): 7–12.
6. Holmin S, Soderlund J, Biberfeld P, Mathiesen T. Intracerebral inflammation after human brain contusion. Neurosurgery 1998; 42 : 291–298.
7. Winter CD, Pringle AK, Clough GF, Church MK. Raised parenchymal interleukin-6 levels correlate with improved outcome after traumatic brain injury. Brain 2004; 127 : 315–320.
8. Fassbender K, Rossol S, Kammer T, Daffertshofer M, Wirth S, Dollman M. Proinflammatory cytokines in serum of patients with acute cerebral ischemia: kinetics of secretion and relation to the extent of brain damage and outcome of dinase. J Neurol Sci 1994; 122 : 135–139.
9. Semple BD, Bye N, Rancan M, Ziebell JM, Morganti-Kossmann MC. Role of CCL2 (MCP-1) in traumatic brain injury (TBI): evidence from severe TBI patients and CCL2−/ − mice. J Cereb Blood Flow Metab 2010; 30(4): 769–782.
10. Krum JM, Mani N, Rosenstein JM. Roles of the endogenous VEGF receptors flt-1 and flk-1 in astroglial and vascular remodeling after brain injury. Exp Neurol 2008; 212 : 108–117.
11. Grad S, Ertel W, Keel M, Infanger M, Vonderschmitt DJ, Maly FE. Strongly enhanced serum levels of vascular endothelial growth factor (VEGF) after polytrauma and burn. Clinical Chemistry and Laboratory Medicine 1998; 36(6): 379–383.
12. Veenith T, Goon SH, Burnstein RM. Molecular mechanisms of traumatic brain injury: the missing link in management. World J Emerg Surg 2009; 4 : 7.
13. Jordan B, Relkin N, Ravdin L. Apolipoprotein E-[Epsilon]4 associated with chronic traumatic brain injury in boxing. JAMA 1997; 278 : 136–140.
14. Friedman G, Froom P, Sazbon L, et al. Apolipoprotein E-epsilon4 genotype predicts a poor outcome in survivors of traumatic brain injury. Neurology 1999; 52 : 244–248.
15. Teasdale GM, Nicoll JA, Murray G, Fiddes M. Association of apolipoprotein E polymorphism with outcome after head injury. Lancet 1997; 350 : 1069–1071.
16. Tiret L, Rigat B, Visvikis S. Evidence, from combined segregation and linkage analysis, that a variant of the angiotensin I-converting enzyme (ACE) gene controls plasma ACE levels. Am J Hum Genet 1992; 51 : 197–205.
17. Ariza M, Matarin M, Jungue C. Influence of the angiotensin-converting enzyme polymorphism on neuropsychological subacute performance in moderate and severe traumatic brain injury. J Neuropsychiatry Clin Neurosci 2006; 18 : 39–44.
18. Soares HD, Hicks RR, Smith D, McIntosh TK. Inflammatory leukocytic recruitment and diffuse neuronal degeneration are separate pathological processes resulting from traumatic brain injury. J Neurosci 1995; 15 : 8223–8233.
19. Stahel PF, Shohami E, Younis FM, Kariya K, Otto VI, Lenzlinger PM. Experimental closed head injury: analysis of neurological outcome, blood-brain barrier dysfunction, intracranial neutrophil infiltration, and neuronal cell death in mice deficient in genes for pro-inflammatory cytokines. J Cereb Blood Flow Metab 2000; 20 : 369–380.
20. Zhuang J, Shackford SR, Schmoker JD, Anderson ML. The association of leukocytes with secondary brain injury. J Trauma 1993; 35 : 415–422.
21. Schwarzmaier SM, Kim SW, Trabold R, Plesnila N. Temporal profile of thrombogenesis in the cerebral microcirculation after traumatic brain injury in mice. Journal of Neurotrauma 2010; 27(1): 121–130.
22. Von Oettingen G, Bergholt B, Gyldensted C, Astrup J. Blood flow and ischemia within traumatic cerebral contusions. Neurosurgery 2002; 50 : 781−790.
23. Laroche M, Kutcher ME, Huang MC, Cohen MJ, Manley GT. Coagulopathy After Traumatic Brain Injury. Neurosurgery 2012; 70(6): 1334–1345.
24. Nakajima K, Kohsaka S. Microglia: neuroprotective and neurotrophic cells in the central nervous system. Curr Drug Targets Cardiovasc Haematol Disord 2004; 4(1): 65–84.
25. Morganti-Kossmann MC, Rancan M, Stahel PF, Kossmann T. Inflammatory response in acute traumatic brain injury: a double-edged sword. Curr Opin Crit Care 2002; 8(2): 101–105.
26. Ho L, Zhao W, Dams-O‘Connor K, et al. Elevated Plasma MCP-1 Concentration Following Traumatic Brain Injury as a Potential “Predisposition” Factor Associated with an Increased Risk for Subsequent Development of Alzheimer‘s Disease. Journal of Alzheimers disease 2012; 31(2): 301–313.
27. Woiciechowsky Ch, Schöning B, Cobanov J, Lanksch WR, Volk HD, Döcke WD. Early IL-6 Plasma Concentrations Correlate with Severity of Brain Injury and Pneumonia in Brain-Injured Patients. Journal of Trauma-Injury Infection & Critical Care 2002; 52(2): 339–345.
Labels
Anatomical pathology Forensic medical examiner Toxicology
Article was published inForensic Medicine

2014 Issue 4-
All articles in this issue
- Possibilities of molecular genetic determination of age of an individual from biological traces
- Pathomorphology of inflammatory response following traumatic brain injury, serum values of interleukins, and gene polymorphisms
- Ethanol-induced ketoacidosis as a possible neglected cause of sudden death in chronic alcohol consumers
- Causes of death and heart pathology in pacemaker or implantable cardioverter-def ibrillator patients who died in hospital
- Forensic Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Causes of death and heart pathology in pacemaker or implantable cardioverter-def ibrillator patients who died in hospital
- Ethanol-induced ketoacidosis as a possible neglected cause of sudden death in chronic alcohol consumers
- Possibilities of molecular genetic determination of age of an individual from biological traces
- Pathomorphology of inflammatory response following traumatic brain injury, serum values of interleukins, and gene polymorphisms
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

