-
Medical journals
- Career
Natural healing process after partial glans excision while using novel haemostatic „VerisetTM patch“: description of the technique and initial surgeon’s perspective
Authors: Peter Weibl 1,2; Ghazal Ameli 1; Andrea Holzer 3; Wilhelm Huebner 1
Authors‘ workplace: Department of Urology, Teaching Hospital – Landesklinikum Korneuburg, Austria 1; Uroclinic, s. r. o., Bratislava, Slovak republic 2; Department of Pathology, Landesklinikum Mistelbach, Austria 3
Published in: Ces Urol 2020; 24(2): 105-112
Category: Original Articles
Overview
To describe the initial surgeon’s perspective and results of partial glans excision, while using VerisetTM as a haemostatic patch for excised benign and pre‑malignant penile lesions. Five patients (mean age 61 years) underwent a total of 6 procedures. The defect was covered with the novel patch – VerisetTM.
The mean lesion size was 14 mm (range 8–22 mm). Lesions affected less than 1/3 of the whole glans surface. The mean follow‑up was 9 weeks (range 8–12 weeks). All patients except for one were free of primary local disease. In one case of well differentiated intraepithelial neoplasia (PeIN), the final histology confirmed (PeIN) crossing into squamous cell carcinoma (G1R+,3 mm). The patient underwent a second glans‑preserving procedure. For the remaining cases the histology confirmed chronic balanoposthitis (2 pts) and verruca vulgaris (2 pts). Within a time frame of 6–8 weeks the excised glans area was completely epithelialized, all patients were satisfied with the final appearance andfully recovered their sexual activities. There was no serious complication or sequelae requiring any kind of intervention. Our initial experience should encourage urologists to conduct a well designed study to prove the efficacy and safety of this surgical principle.
Keywords:
Penis – carcinoma – glans resurfacing – tissue sealant – verisetTM
INTRODUCTION
Over the last decade glans resurfacing with split thickness skin grafting (STSG) has been well standardized and proven as a safe procedure with oncologically comparable outcomes to those after traditional partial penectomy in the setting of superficial penile cancer population (1). STSG procedures demostrated excellent cosmetic outcomes and patients could regain their self confidence in sexual intercourse (2, 3). However, for the smaller benign and premalignat lesions in the glans area, STSG may pose some dillemas with regard to the complexity of the procedure.
In addition STSG technique may carry higher morbidity risk, when compared to less inasive approach. The smaller defects can be managed with simple sutures. On the other hand, surgeons should avoid and minimize the alterations of the basic anatomy and shape of the glans.
The aim of our preliminary report is to describe the initial surgeon’s perspective and results of partial glans excision, while using VerisetTM as a „graft“ coverage for excised benign and pre‑malignant penile lesions. VerisetTM is a ready to use topical hemostatic patch composed of absorbable oxidized cellulose and hydrogel components (Medtronic‑Austria). The material is free from any human or animal derived components and therefore unlikely to induce unwanted immune response or trasmit viruses. So far, Veriset™ has been approved for use on solid organs and in soft tissue procedures in order to stop and control the bleeding within few minutes (4, 5, 6).
MATERIAL AND METHODS
In lieu of a formal approval of our institutional review board, the principles of the Helsinki Declaration were followed. All patients were informed about the surgical procedure and realistic expectations were discussed with all the participants. Perioperative and postoperative risks, as well as potential complications of the procedure were discussed before the surgery. Written informed consent was obtained from all the patients. Patients were fully informed about our further scientific and publishing intentions, and gave us written informed consent. Surgery was performed by one surgeon (PW). None of the patients had any graft‑related issues, increased risk of bleeding or any other heath problems compromising the use of STSG. Each patient was fully informed and educated about all current trends in partial glans resurfacing surgery. The realistic expectations were discussed as a part of the informed consent. Each patient made an independent decision, and opted for a less invasive approach regardless the paucity of data on Veriset use. We think that the encouraging moment was, the knowledge, that the surgeon can still perform redo sugery while using STSG.
In total we performed 6 procedures in 5 patients who underwent partial glans excision of the epithelium and subepithelium followed by coverage with novel haemostatic material – VerisetTM.
After adequate general anesthesia induction, the patient was placed in a normal supine position. A tourniquet was placed around the base of the penis. The plane was developed to undermine the suspicious area with approximately 5 mm healthy margin and only few millimeters for benign and premalignat lesions respectively. Sharp dissection between the subepithelial layer and the corpus spongiosum was performed.
After complete excision, the defect was covered with novel tissue sealant VerisetTM. Mild compression on the wet sponge for a minimum of 1–2 minutes was applicated, before releasing the tourniquet. Afterwards, a mild compressive bandage with fat gauze and Baneocin cream (combined antibacterial drug for topical application, which contains two antibiotics with bactericidal effect, neomycin and bacitracin) was applied after Foley catheter insertion (Ch 12). The catheter was removed after 3/5 days and patients were discharged on the third postoperative day.
On the very first day after the surgery, we had removed the bandage and after careful inspection of the glans applied a new bandage with a little bit less compression. On the excision site with the remaining parts of the Veriset material we applied a fat gauze with Baneocin. Consequently the Veriset material was completetly resorbed and fell off within 3–5 days. Each patient was followed on weekly intervals thereafter and carefully advised how to proceed with local wound management (application of vaseline mixed with Baneocin 3× daily, after local hygiene with aqua). Within a time frame of 6–8 weeks the excised glans area was completely epithelialized presumably from the healthy margins (Fig. 1, 2). In light of this, once the healing process was completed, there was no further wound care required.
1. A) Low grade penile intraepithelial neoplasia PeN; B) The lesion measured approx. 20 mm and involved less than 1/3 of the glans area; C) Sharp excision of the epithelium and subepithelial layer; D) Application of the VerisetTM patch, which was fixed with few resorbable 5.00 sutures; E) Fat gauze was positioned over the Veriset patch; F) 1st. postoperative day, fragments of the patch are still in situ; G) 3rd postoperative day – the base is already partially granulated; H) 1 week after the procedure; I) 4 weeks after; J) after 8 weeks the wound was completely epithelialized and exhibited satisfactory cosmetic appearance.
Obr. 1. A) Penilní intraepitelová neoplazie nízkého stupně; B) léze měřila přibližně 20 mm a postihovala méně než 1/3 povrchu glandu; C) ostrá excize epitelu a subepitelové vrstvy; D) aplikace náplasti VerisetTM, která byla připevněna několika vstřebatelnými stehy 5/00; E) mastná gáza umístěna přes náplast Veriset; F) první pooperační den, fragmenty náplasti jsou stále in situ; G) třetí pooperační den – spodina je již částečně granulovaná; H) jeden týden po zákroku; I) čtyři týdny po zákroku; J) po osmi týdnech byla rána kompletně epitelizovaná a vykazovala uspokojivý estetický vzhled.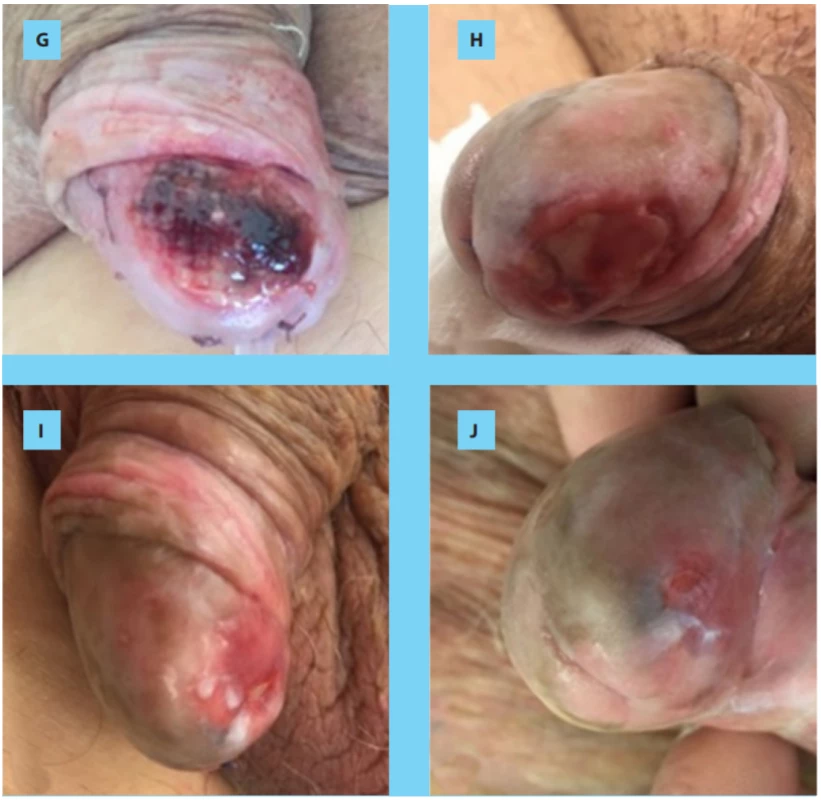
2. . A) 9 weeks after the primary excision; B) demarcation of the glans area; C) re-excision of the glans; D) coverage with the Veriset, which was fixed with a few 4.0 resorbable sutures; E) 3rd postoperative day, F) 7 days after the procedure; G) local wound care with vaseline mixed with baneocin cream; H) final appearance of the glans (week number 8).
Obr. 2. A) Devět týdnů po primární excizi; B) vymezení oblasti glandu; C) reexcize glandu; D) překrytí náplastí Veriset, která byla připevněna několika vstřebatelnými stehy 4/0; E) třetí pooperační den; F) sedm dnů po zákroku; G) lokální péče o ránu za použití vazelíny smíchané s mastí baneocin; H) konečný vzhled glandu (8. týden)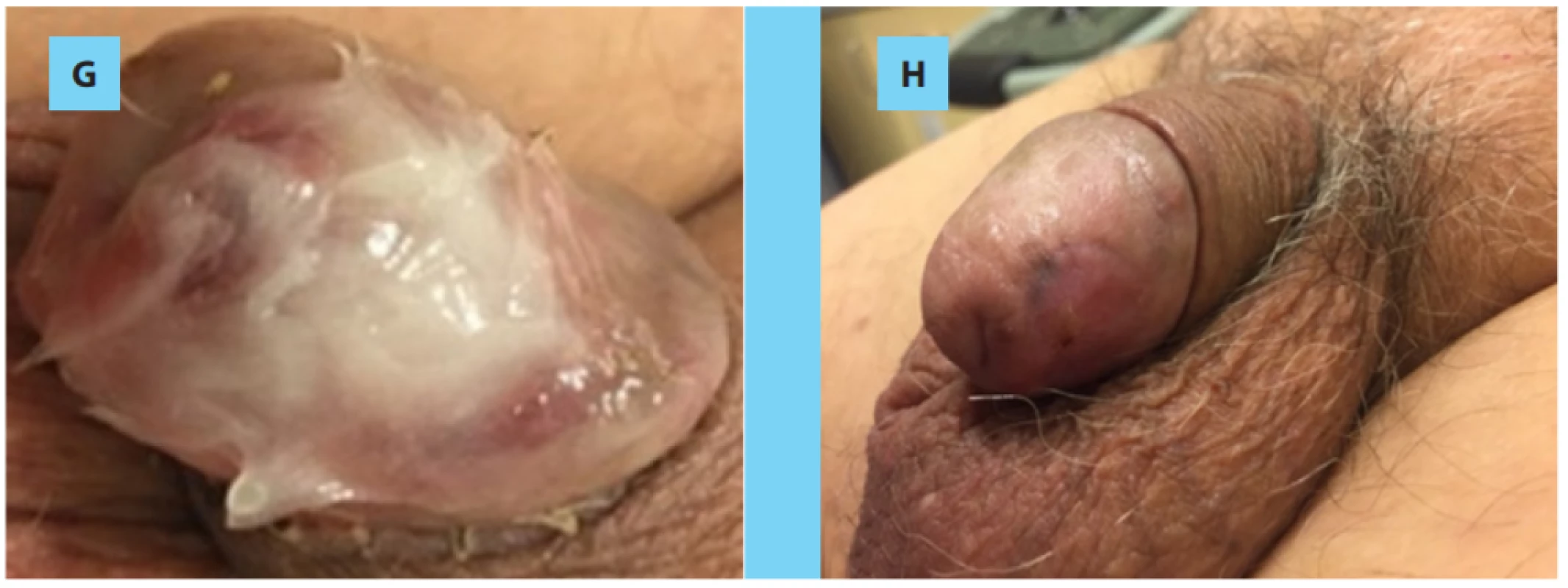
RESULTS
The mean lesion size 14 mm (range 8–22 mm). All the lesions affected less than 1/3 of the whole glans surface. The mean follow-up was 10 weeks (range 8–24 weeks). All patients except one were free of primary local disease. In one case of well differentiated intraepithelial neoplasia (PeIN), the final histology confirmed (PeIN) crossing into squamous cell carcinoma (G1R+,3 mm). The patient underwent a second glans-preserving procedure followed with Veriset application. The frozen section as well as final histology demonstrated no evidence of PeIN nor SCC.
For the remaining cases the histology confirmed chronic balanoposthitis (2 pts) and verruca vulgaris (penile horn, 2 pts), what was in correlation with the primary preoperative biopsy result. In both patients with PeIN and one balanoposthitis case we performed circumcision in the same setting. All benign lesions were treated with various topical regimens previously, however without any success.
Patients were satisfied with the appearance of the glans and fully recovered their sexual activities. The sensitivity was sligthly reduced in the area of excision in 2 patients. However this was not a matter of dissatisfaction. There were no serious complication sequellae requiring any kind of postoperative intervention.
DISCUSSION
In the current paper, we aimed to gather initial evidence for the potential safety and effectiveness of Veriset™ hemostatic patch in soft tissue bleeding during partial glans excision and „natural spontaneous resurfacing“. It is a novel biomaterial made of a polyethelene glycol-coated collagen pad.
To our knowledge this is the very first report on the use of Veriset in the field of open andrological – reconstructive surgery. We have to admit that the term „reconstructive“ is bit overestimated.
When Veriset™ hemostatic patch was used, hemostasis occurred within 1–2 minutes. No device‑related serious adverse events were recorded during the 30 days after surgery, and no reoperations for device-related complications were performed during the follow up period after surgery.
Surgeon experience, careful patient selection, patient preference and the type/size of penile lesion will affect the choice of graft to be used. The use of standardized STSG, vascularized penile skin graft, tunica vaginalis graft increases the complexity of the procedure as well as the time and potential morbidity (2, 3, 7). Therefore, for smaller lesions so called off-shelf /ready to use graft material seems to be more convenient and attractive. The ideal graft should not prolong operative time, be readily available, resistant to infection, should not contract, should induce haemostasis, and be cost-effective. However, such a graft has not yet been developed.
In general, major advantages of VerisetTM is its coating with fibrin glue, resulting in no need for fixation. For our first three cases with concomitatnt circumcision we placed a few resorbable sutures for safety reasons. It seems that, the novel sealant material acts as a scaffold allowing glans epithelium regeneration immediately after inducing sufficient hemostasis. According to our preliminary data Veriset had shown satisfactory haemostatic properties and potential to restore normal superficial glans tissue anatomy. The final cosmesis was regarded highly satisfactory from the surgeon‘s point of view as well as the patient’s perspective, although not measured with standard tools.
The crucial factors for final cosmetic success werepostoperative local wound care management and patients’strict adherence to follow up, which \are actually required for all reconstructive procedures.
Topical cutaneous application of vaseline/ baneocin cream was indicated for each case. Every patient was fully informed and fully advised about postoperative wound care management. The local application was performed at least 3 times per day in order to induce a relatively wet environment and thus induce continuous healing and regeneration.
Some clinicians may argue, because the process of complete epithelialization took 6–8 weeks, while with an STSG it takes 7–10 days. The STSG technique has proven oncological safety over time and demon ‑ strated superior cosmetic outcomes (2, 3, 7). To our opinion, the extended recovery is relative, because our patients did not suffer from any quality of life reduction, apart from restriction of sexual activity.
We can assume once the healing process has been completed, it seems fair to state that we would not expect any wound related complications. Certainly the oncological safety has to stand the test of time, although we used well standardized partial glans excision technique (2, 3).
Our report has several limitations worth noting: a) small subset of patients, b) limited follow up, and c) we did not quantify the satisfactory and sexual outcome according to the appropriate measurements and validated questionnaires. Having said so, we are fully aware that the statement – „the procedure is safe and effective“ is in the meantime preliminary. With respect to our results, the described procedure has promising potential especially in the setting of partial glans resurfacing for smaller lesions involving less than a half surface of the glans. At this time there was no comparison with the „standard of care“ control group analysed. The patch itself, does not help to recreate the initial anatomy of the glans. However, according to our previous observations, the natural healing process of the glans tissues after succesful hemostasis only, has the potential to rebuild the comparable and satisfactory appearance, without any further reconstructive principles (8). This initial report should encourage urologists to conduct a well designed study to prove the efficacy of this surgical principle.
Last but not least, it is of utmost importance to indicate such a technique in a well selected compliant and motivated patient population.
Abbreviations: PeIN – penile intraepithelial neoplasia; SCC – squamous cell carcinoma; STSG – split‑thickness skin graft
Acknowledgements: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board committee. Informed consents including the procedure and possible complications were taken from all patients.
Conflict of interest: Authors have no conflict of interest or any other competing financial interests in relation to the work described.
Došlo: 9. 1. 2020
Přijato: 19. 2. 2020
Kontaktní adresa:
doc. MUDr. Peter Weibl, PhD.
Department of Urology, Teaching Hospital – Landesklinikum Korneuburg,
Wiener Ring 3–5, Korneuburg, Austria
e‑mail: pweibl@yahoo.com
Sources
1. Kelly F, Lonergan P, Lundon D, et al. A Prospective Study of Total Glans Resurfacing for Localized Penile Cancer to Maximize Oncologic and Functional Outcomes in a Tertiary Referral Network. J Urol. 2017; 197(5): 1258–1263.
2. Shabbir M, Muneer A, Kalsi J, et al. Glans resurfacing for the treatment of carcinoma in situ of the penis: surgical technique and outcomes. Eur Urol. 2011; 59(1): 142–147.
3. Hadway P, Corbishley CM, Watkin NA. Total glans resurfacing for premalignant lesions of the penis: initial outcome data. BJU Int. 2006; 98(3): 532–536.
4. Öllinger R, Mihaljevic AL, Schuhmacher C, et al. A multicentre, randomized clinical trial comparing the Veriset™ haemostatic patch with fibrin sealant for the management of bleeding during hepatic surgery. HPB (Oxford) 2013; 15(7): 548–558.
5. Howk K, Fortier J, Poston R. A Novel Hemostatic Patch That Stops Bleeding in Cardiovascular and Peripheral Vascular Procedures. Ann Vasc Surg. 2016; 31 : 186–195.
6. Schuhmacher C, Pratschke J, Weiss S, et al. Safety and effectiveness of a synthetic hemostatic patch for intraoperative soft tissue bleeding. Med Devices (Auckl). 2015 Mar 31; 8 : 167–174.
7. Weibl P, Plank C, Hoelzel R, et al. Neo‑glans reconstruction for penile cancer: Description of the primary technique using autologous testicular tunica vaginalis graft. Arab J Urol. 2018; 16(2): 218–223.
8. Weibl P, Herwig R. Superficial penile cancer treated with complete excision of the glans epithelium and coverage with a tissue sealant matrix (TachoSil®). Cent European J Urol. 2019; 72(2): 204–208.
Labels
Paediatric urologist Nephrology Urology
Article was published inCzech Urology
2020 Issue 2-
All articles in this issue
- Editorial
- Bulbar urethral reconstruction after extensive inflammatory abscess‑forming process in the perineal region due to an underlying foreign body
- Komentář k práci Drlík P, Čermák M. Rekonstrukce bulbární uretry po rozsáhlém zánětlivém abscedujícím procesu v oblasti hráze na podkladě cizího tělesa (video) Ces Urol 2020; 24(2): 90–93
- Hand‑assisted laparoscopic adrenalectomy for large adrenal tumours
- Examination of circulating tumor cells in renal carcinoma
- Renal tumor biopsy – indications, technique, results
- Our approach to diagnosing and treating impalpable testis
- Brachyterapie s vysokým dávkovým příkonem jako orgán šetřící léčba u časného karcinomu penisu
- Pancreatic injury associated with urologic surgery and the options of pancreatic fistula management
- Conversion of the continent diversion to a conduit by retubularization of a neobladder wall
- Objemný cystický lymfangiom levé nadledviny – diferenciálně diagnostický omyl
- Pandemii navzdory – Komplexní novinky v onkourologii 2020
- Natural healing process after partial glans excision while using novel haemostatic „VerisetTM patch“: description of the technique and initial surgeon’s perspective
- Czech Urology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Renal tumor biopsy – indications, technique, results
- Examination of circulating tumor cells in renal carcinoma
- Natural healing process after partial glans excision while using novel haemostatic „VerisetTM patch“: description of the technique and initial surgeon’s perspective
- Objemný cystický lymfangiom levé nadledviny – diferenciálně diagnostický omyl
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career



