-
Medical journals
- Career
HISTOLOGICAL EXAMINATION OF THE LINGUAL FRENULUM IN PATIENTS WITH ANKYLOGLOSSIA
Authors: S. Hilbertová 1; T. Dostálová 1; J. Michálek 2; P. Hliňáková 1
Authors‘ workplace: Stomatologická klinika dětí a dospělých, 2. lékařská fakulta Univerzity Karlovy a Fakultní nemocnice Motol, Praha 1; Ústav klinické a molekulární patologie, Lékařská fakulta Univerzity Palackého a Fakultní nemocnice, Olomouc 2
Published in: Česká stomatologie / Praktické zubní lékařství, ročník 122, 2022, 1, s. 4-10
Category: Original articles
doi: https://doi.org/10.51479/cspzl.2022.001Original article – clinical study
Overview
Introduction and aim: Tongue-tie or ankyloglossia is a congenital anomaly characterized by a short lingual frenulum which can be defined as restriction of tongue movement and thus impact on function. The exact cause of ankyloglossia is unknown. Prevalence varies in 7% of men and 4% of women. Tongue-tie is reported to be the cause of breastfeeding difficulties. It also causes speech and articulation problems, can be one of the causes of poor oral hygiene and often does not allow the patient to play wind instruments. The aim of the study was to assess in the clinical, anatomical and histological image, the indication for the surgical procedure, and the possible invasiveness with respect to the following rehabilitation of tongue movement.
Material and methods: The group included 13 generally healthy patients with ankyloglossia – seven girls, and six boys – with mean age at the time of surgery of 8.3 years. An informed consent to participate in our study was signed in accordance with the Declaration of Helsinki. The anonymity of the data obtained was strictly observed. Approval for the study was obtained from the Ethics Committee of the 2nd Medical Faculty of Charles University and the Motol University Hospital. Tongue frenulectomy using a scalpel was always used for the procedure itself. Patients and parents were instructed on the type and nature of surgery in order to achieve the greatest possible cooperation. Local anesthesia was applied, 1–2 ml of Supracain. The sublingual frenulum was then cut with a scalpel to release the tip of the tongue. Soft tissues around the sublingual bridle were loosened and mobilized, and tongue mobility was checked. After wound revision and toilet, suturing was performed with absorbable material.
Results: Histological evaluation was performed using an optical microscope Olympus CH30. The type of superficial covering epithelium, its thickness (magnification 100×), the proportion of fibrosis, vascular and nerve structures, inflammatory elements and especially the presence of striated muscle were evaluated and calculated.
Conclusion: In the study it was clinically proven that the main indication for treatment were speech and articulation difficulties of older children. Tongue frenulectomy using a scalpel was clinically and histologically a very gentle method, the preschool age of the child was optimal, which already allowed easy rehabilitation of the fibrous scar. As we have shown, the optimum is early surgery, followed by functional rehabilitation of the tongue and then by speech therapy. During the histological examination of a lingual frenulum we proved a presence of the squamous epithelium which can be also parakeratotic, fibrous tissue, striated muscle, nerves and blood vessels.
Keywords:
Anatomy – Dentistry – treatment – histology – tongue-tie – ankyloglossia
INTRODUCTION
The lingual frenulum is the fold of the mucosa – the lining of the mucosa that connects the base of the mouth to the midline of the lower part of the tongue [1] and thus helps to stabilize the base of the tongue with its tip [2]. Tongue-tie (ankyloglossia) is a condition in which this mucous membrane is attached near the tip of the tongue and can be either too short or unusually firm and strong, causing limited tongue movement [3]. The exact cause of ankyloglossia is unknown. The prevalence based on 15 studies with 24536 patients was 7% in men and 4% in women [4]. These data are also confirmed by data from our literature, where the incidence varies from 0.02 to 4.8% and the occurrence tongue-tie is observed 3 times more often in boys than in girls [5]. The exact etiopathogenesis is unclear, the role of the GPCR (G protein-coupled receptor) has been suggested [6] and genetics may also play a role here [7]. Other studies suggest that alterations of the lingual frenulum may be caused by mutations in the T-box gene, inherited as an autosomal dominant trait with incomplete penetration. The vast majority occur independently, rarely as part of some syndromes (Smith-Lemli-Opitz syndrome, Beckwith-Wiedemann syndrome, Simpson-Golabi-Behmel syndrome, acrofacial dysostosis, cleft palate bound to the X chromosome) [8].
Ankyloglossia is reported to be the cause of breastfeeding difficulties. A baby is unable to adhere to the mother's breast, which is related to failure to thrive in infancy and may lead to the termination of breastfeeding [9]. It also causes speech and articulation problems [5]. Tongue-tie can be one of the causes of poor oral hygiene and often does not allow the patient to play wind instruments [1].
DEVELOPMENT AND ANATOMY OF THE TONGUE AND FRENULUM
Tongue is a dynamic organ that affects breathing, speech, breastfeeding and swallowing, and thus plays a vital role in facial development. Intrauterinely the growth of the tongue is directed forward by a lingual frenulum attached to the base of the oral cavity and to the ventral surface of the tongue. During fetal development, the lingual frenulum thus creates a balance between the tongue, lip muscles, and growing facial bones. The tongue is short at birth and the tip is not fully developed, as it lengthens and narrows towards the apex, the ligament of frenulum often retreats to a lower position. They form during the 4th week of gestation in two parts that move medially to join the tuberculum impar and form the anterior two-thirds of the tongue.
The frenulum can have different shapes – it can be long, short, thin or thick. Recent studies suggest that anatomical variations in the lingual frenulum may be due to the persistence of sublingual tissue that has not undergone apoptosis (“programmed embryonic cell death” to eliminate unnecessary or damaged cells) during embryonic development and may limit tongue movement. The lingual frenulum is usually extended at birth and reaches the apex. Then it recedes due to growth during the first six months and this process continues until the age of six [11].
HISTOLOGICAL PICTURE
From an anatomical and physiological point of view, the sublingual frenulum is a dynamic structure formed by a fold of the midline in the fascia layer, which is inserted in the inner arch of the mandible and forms a membrane-like oral structure. Histologically, it was examined in the form of microdissection of the lingual frenulum and base of the mouth at necropsy of 9 adults [10]. It has been proven that the connective tissues of the sublingual frenulum are predominantly formed by the fascia layer; less often the central mucosa. A squamous epithelium covering the frenulum has been described, which extends directly into the epithelium of the base of the oral cavity and the ventral surface of the tongue. The connective tissue fibres passed diagonally to the longitudinal axis and formed a scaffold-like skeleton. In 2014, Martinelli et al. [12] analysed samples of frenulums excised during surgery in seven children under four years of age. Muscle fibres were also identified in some samples. Type I collagen fibres predominated in all samples. Collagen fibres of type III were usually located near the epithelium and around blood vessels. Variability in the abundance and location of elastic fibres has also been noted. The location, size and orientation of the biopsy specimens were not stated and therefore no conclusions could be drawn regarding the structure or morphology of the frenulum. According to another study [13], the ankyloglossia frenulum had a significant amount of transverse skeletal muscle fibres. This may be due to the involvement of collagen and elastic mucosal fibres with genioglossus muscle fibres. High levels of type I collagen have been detected in all types of lingual frenulum. Because type I collagen is resistant to tension, tongue rehabilitation may not be effective in lengthening the tongue frenulum [12].
CLINICAL PICTURE
Ankyloglossia can be asymptomatic or cause restriction of tongue movement. Patients affected by this congenital malformation are not able to perform sideways movements with their tongues, stick out their tongues, they cannot lick their upper lip or palate. We consider eating disorders during breastfeeding and the associated failure to thrive in infancy to be one of the most serious complications of too tight tongue connection. We also include speech and articulation difficulties and deformities of the lower incisors, gingival recessions and malocclusions were also described. The defect does not cause delayed speech development, but causes problems with the pronounciation of some phones, especially T, D, Z, S, H, N, L. Altered chewing and swallowing patterns in individuals with a short sublingual frenulum may further affect the coordination of masticatory muscles during speech and leads to the development of habits such as mouth breathing, aerophagy and anterior tongue position [5]. Hood et al. [14] describe two dental anomalies as a consequence of ankyloglossia – i.e. open bite and mandibular prognathism. The inability to touch the palate with the tongue further promotes an infantile way of swallowing, which leads to the development of an open bite. Lack of free movement of the tongue up and back can result in excessive pushing of the tongue against the body of the mandible and cause the development of mandibular prognathism.
THERAPY OPTIONS
There are currently two basic types of procedures – frenulotomy (mere intersection of the frenulum) and frenulectomy (excision of the frenulum). Frenulotomy is performed in infants without anesthesia or under mucosal local anesthesia using scissors, an electrocautery or a laser [15]. All methods are effective and safe, however the most common is conventional frenulotomy using scissors or a scalpel [16]. The procedure is easy and inexpensive, but a third of patients at this age require reoperation. Immediate breastfeeding after exercise is recommended. In 96% of infants, breastfeeding improved within 48 hours after frenulotomy [1]. Frenulectomy is recommended for children older than two years. In younger children it is performed under general anesthesia, in older children under local anesthesia. Rehabilitation of the tongue after the operation is necessary to prevent scarring. It is important to keep in mind that the postoperative scar may cause a worse clinical picture than the initial one. Proper management of ankyloglossia involves timely and appropriate surgery, followed by speech therapy, which produces the desired results [5, 12].
The appropriate age of therapy is widely discussed. In neonates, it is performed immediately if there are difficulties with breastfeeding or then at the age when the child is able to rehabilitate the tongue. The procedure is improperly performed around one or two years age of the patient, who is without subjective problems only with clinical signs of ankyloglossia, which were detected during preventive examinations of a general dentist or pediatrician. The diversity of views on the types of therapy and the appropriate age for surgery may be due to a lack of common parameters for evaluation and diagnosis and a lack of in-depth knowledge of the sublingual frenulum [13].
Ankyloglossia may be asymptomatic or, conversely, cause limited movement of the tongue, so the aim of the study was to assess it in a clinical, anatomical and histological picture.
MATERIAL AND METHODOLOGY
Clinical group
Our group included 13 generally healthy patients with ankyloglossia – seven girls and six boys with an average age of 8.3 years at the time of surgery. These were patients of the pediatric department of the Department of Dentistry, University Hospital Olomouc and the Department of Dentistry for Children and Adults, 2nd Medical Faculty, Charles University and University Hospital Motol. Patients' legal representatives signed an informed consent to participate in our study in accordance with the Declaration of Helsinki. The anonymity of the data obtained was strictly observed. Approval for the study was obtained from the Ethics Committee of the 2nd Faculty of Medicine, Charles University and the Motol University Hospital (EK-973IGA 1.12 / 11). Clinical data of patients included in the group are summarized in Table 1. Two clinical samples were not histologically processed for tissue inhomogeneity and were excluded from clinical and histological results.
1. Clinical data of patients with ankyloglossia who underwent surgical excision of the sublingual frenulum 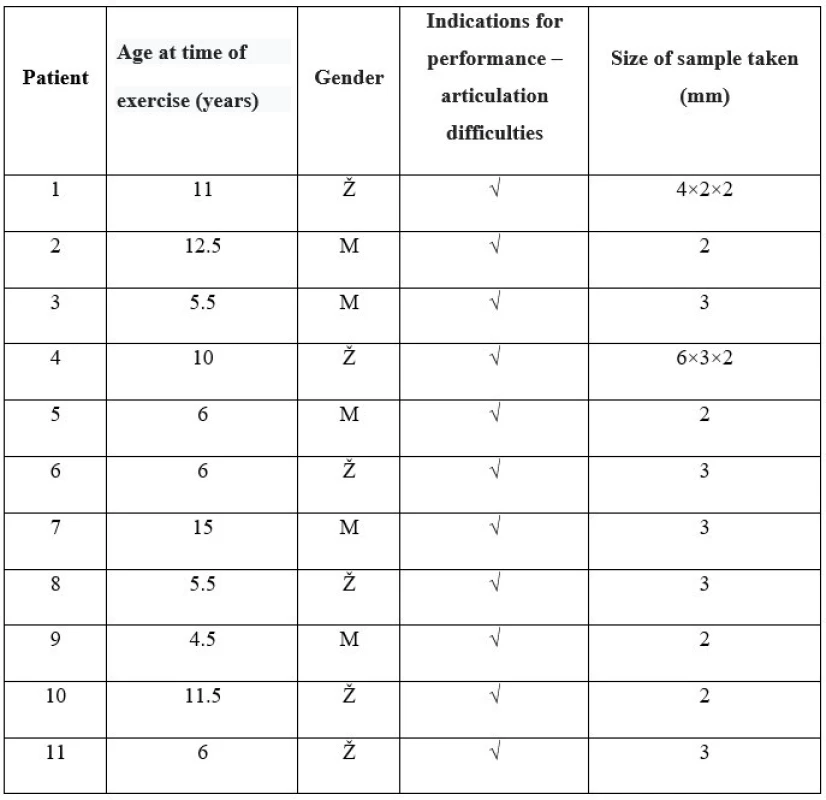
Therapy
Tongue frenulectomy was always used for the procedure itself. First, we instructed the patient and parents about the type and nature of the surgery in order to achieve the greatest possible cooperation. We also applied local anesthesia, 1–2 ml of 4% Supracain. We then cut the sublingual frenulum with a scalpel to release the tip of the tongue. We also loosened and mobilized the soft tissues around the sublingual frenulum and checked that the tongue was free to move. After revision and wound toilet, suture was performed with absorbable material Resorba 5/0. The surgical procedure is shown in Figure 1.
Fig. 1 Frenulectomy in healthy 15-year-old boy: 
A – initial state of tongue protrusion, heart shape,
B – application of local anesthesia Supracain 1 ml,
C – surgical excision using a scalpel,
D – excised frenulum,
E – release and mobilization of surrounding tissues,
F – wound suture with absorbable material Resorba 5/0,
G – protrusion of tongue immediately after surgery
Sampling and its transport and histological processing
We placed the sample in a closable bottle with 10% formalin and transported it to the Institute of Clinical and Molecular Pathology, Olomouc University Hospital. In the laboratory, the samples were processed into tissue blocks and embedded in paraffin in the following steps:
- Dehydration – dewatering of fixed samples with ascending ethanol (50%, 70%, 90%, 96%, 100%), each bath of alcohol lasted two to six hours.
- Clarification – displacement of alcohol by xylene.
- Saturation – with dissolved paraffin (melting point 56 °C); carried out in a thermostat: paraffin bath - 3×6 hours.
- Pouring – dissolved paraffin is poured into the chambers and tissue samples are placed in it.
The chambers were rapidly cooled by immersion in cold water. After removal from the chambers, the paraffin blocks were stripped of excess paraffin and prepared for microtome slicing.
Tissue sections on slides were subsequently stained with basic hematoxylin-eosin (HE) staining, which consists of the following steps:
- Deparaffinization and watering: sections were deparaffinized before staining in aqueous solutions with xylene and rehydrated with a descending alcohol series.
- Self-staining: dewaxed and irrigated sections were stained first with hematoxylin solution for 3–10 minutes. This was followed by rinsing in water, so-called differentiation in acidic ethanol, washing in running water for 5 minutes. Eosin staining was then performed for 1–3 minutes and rinsing in distilled water.
- Drainage and clarification were performed with an ascending xylene alcohol series (96% to 100%).
- Assembly of painted sections: the assembly medium was a transparent Solakryl fabric with a high refractive index (Solakryl BMK, manufactured by Lučební závody Draslovka, a.s., Kolín, Czech Republic). A drop of mounting medium was dropped on the slide on a slide, and a coverslip was placed on it. The finished preparation was placed in a thermostat (37 °C), where it dried in the mounting medium.
This was followed by a histopathological examination by a pathologist with an assessment of selected monitored parameters. Histological evaluation was performed under an Olympus CH30 optical microscope (manufactured by Olympus Optical CO., LTD, 2-43-2, Hatagaya, Shibuya, Tokyo, Japan). The type of superficial covering epithelium, its thickness (using an ocular scale at 100x magnification), the presence of fibrosis, vascular and nerve structures, inflammatory elements and especially the presence of striated muscle were evaluated, where in its presence its percentage of the whole sample muscle / whole sample size × 100; evaluated at 100× magnification).
RESULTS
Two clinical samples were not histologically processed due to tissue inhomogeneity and were excluded from histological results. The histological composition of the individual samples is summarized in Table 2. The structures of the sublingual frenulum are shown and described in Figures 2 and 3.
Fig. 2 Part of sublingual frenulum (stained with HE, magnified 100×) showing squamous epithelium, fibrous and muscle tissue, blood vessel 
Fig. 3 Part of sublingual frenulum (stained with HE, magnified 100×) showing striated muscle, nerve and fibrous tissue 
2. Histological composition of taken samples 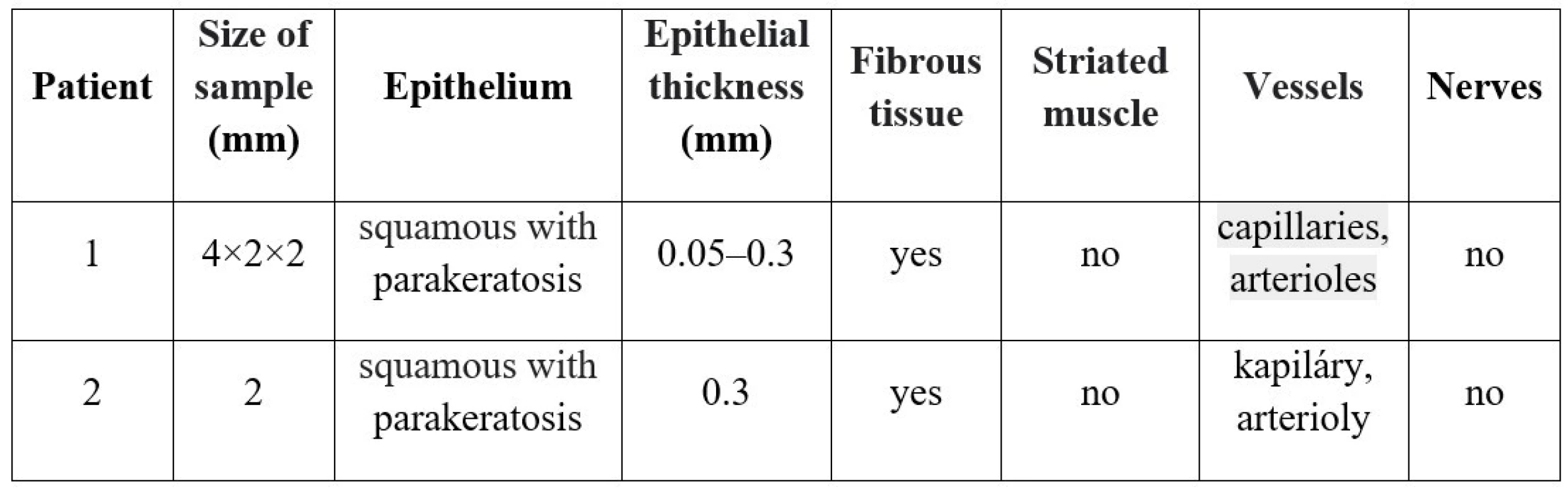
DISCUSSION AND CONCLUSION
It is known that a short sublingual frenulum can be asymptomatic, but if it restricts the movements of the tongue, it can already cause eating disorders in the newborn during breastfeeding and the associated failure to thrive in infancy [9]. In later life, it can cause speech and articulation problems, orthodontic defects, gingival recessions and malocclusion. The defect is also associated with impaired pronounciation of individual phones, such as T, D, Z, S, etc. Limitation of chewing and swallowing often leads to mouth breathing, problems with swallowing and the development of an open bite or mandibular prognathism [5, 14].
Diagnosis and treatment of short sublingual frenulums remain an open problem [5, 17]. It is uncertain whether ankyloglossia is a congenital oral anomaly requiring treatment or only a variation in the shape and position of the sublingual frenulum. Ninety percent of pediatricians and seventy percent of otolaryngologists believe that limited language movement never or rarely causes a feeding problem [17]. The American Academy of Pediatrics recognizes that ankyloglossia is a major clinical entity that should be treated [1].
In our study, we clinically demonstrated that the main indication for surgical treatment in older children was articulation difficulties. According to the clinical and histological picture, lingual frenulectomy using a scalpel was a very gentle method. The preschool age of the child was optimal, which already allowed easy rehabilitation of the fibrous scar. Thus, early surgery is most appropriate, followed by functional rehabilitation of the tongue, followed by speech therapy. Histological examination of the sublingual frenulum showed the presence of squamous epithelium with or without superficial parakeratosis, fibrous tissue, striated muscle, nerves and blood vessels.
Supported by the project of the Ministry of Health, conceptual development of the research organization 00064203 FN MOTOL.
MDDr. Sandra Hilbertová
Stomatologická klinika dětí a dospělých, 2. LF UK a FN Motol
V Úvalu 84
150 06 Praha 5
e-mail: sandra.hilbert@seznam.cz
Sources
- O'Shea JE, Foster JP, O'Donnell CP, Breathnach D, Jacobs SE, Todd DA, Davis PG. Frenotomy for tongue-tie in newborn infants. Review. Cochrane Database Syst Rev. 2017; 3(3): CD011065.
- Marchesan IQ. Lingual frenulum: quantitative evaluation proposal. Int J Orofacial Myology. 2005; 31 : 39–48.
- Jackson R. Improving breastfeeding outcomes: the impact of tongue-tie. Community Pract. 2012; 85(6): 42–44.
- Hill RR, Lee CS, Pados BF. The prevalence of ankyloglossia in children aged <1 year: a systematic review and meta-analysis. Pediatr Res. 2020; 13. doi: 10.1038/s41390-020-01239-y. Epub ahead of print
- Seydlová M. Pedostomatologie. Praha: Mladá fronta; 2015.
- Edmunds J, Miles SC, Fulbrook P. Tongue-tie and breastfeeding: a review of the literature. Breastfeed Rev. 2011; 19(1): 19–26.
- Walsh J, McKenna Benoit M. Ankyloglossia and other oral ties. Otolaryngol Clin North Am. 2019; 52(5): 795–811.
- Lopes de Castro Martinelli R, Marchesan IQ, Gusmão RJ, de Castro Rodrigues A, Berretin-Felix G. Histological characteristics of altered human lingual frenulum Int J Ped Child Health. 2014; 2 : 5–9.
- Hogan M, Westcott C, Griffiths M. Randomized, controlled trial of division of tongue-tie in infants with feeding problems. J Paediatr Child Health. 2005; 41(5–6): 246–250.
- Mills N, Pransky SM, Geddes DT, Mirjalili SA. What is a tongue tie? Defining the anatomy of the in-situ lingual frenulum. Clin Anat. 2019; 32(6): 749–761.
- Mills N, Geddes DT, Amirapu S, Mirjalili SA. Understanding the lingual frenulum: histological structure, tissue composition, and implications for tongue tie surgery. Int J Otolaryngol. 2020; 8 : 1820978.
- Martinelli R, Marchesan I, Gusmão R, Rodrigues A, Berretin-Felix G. Histological characteristics of altered human lingual frenulum. Int J Pediatr Child Health. 2014; 2 : 5–9.
- Bakutra G, Vishnoi S, Desai J, Soni V. Management of ankyloglossia (tongue-tie) – review and report of two cases. J Pierre Fauchard Academy (India Sect.) 2017; 31 : 2–4.
- Hooda A, Rathee M, Yadav S, Gulia J. Ankyloglossia: A review of current status. Int J Otorhinolaryng. 2009; 12(2): 1–7.
- Yoon A, Zaghi S, Weitzman R, Ha S, Law CS, Guilleminault C, Liu SYC. Toward a functional definition of ankyloglossia: validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017; 21(3): 767–775.
- Ruffoli R, Giambelluca MA, Scavuzzo MC, Bonfigli D, Cristofani R, Gabriele M, Giuca MR, Giannessi F. Ankyloglossia: a morphofunctional investigation in children. Oral Dis. 2005; 11(3): 170–174.
- Messner AH, Lalakea ML. Ankyloglossia: controversies in management. Int J Pediatric Otorhinolaryng. 2000; 54(2–3):123–131.
Labels
Maxillofacial surgery Orthodontics Dental medicine
Article was published inCzech Dental Journal

2022 Issue 1-
All articles in this issue
- ZIRCONIA CERAMICS: PROPERTIES AND CLASSIFICATION
- Editorial
- EROSIVE EFFECT OF ACIDIC BEVERAGES ON THE SURFACE OF FILLING MATERIALS
- Změna na postu šéfredaktora časopisu Česká stomatologie a praktické zubní lékařství
- IN MEMORIAM DOC. MUDr. IVO DŘÍZHAL, CSc.
- HISTOLOGICAL EXAMINATION OF THE LINGUAL FRENULUM IN PATIENTS WITH ANKYLOGLOSSIA
- Czech Dental Journal
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- ZIRCONIA CERAMICS: PROPERTIES AND CLASSIFICATION
- HISTOLOGICAL EXAMINATION OF THE LINGUAL FRENULUM IN PATIENTS WITH ANKYLOGLOSSIA
- EROSIVE EFFECT OF ACIDIC BEVERAGES ON THE SURFACE OF FILLING MATERIALS
- IN MEMORIAM DOC. MUDr. IVO DŘÍZHAL, CSc.
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career



