-
Medical journals
- Career
Importance of PET/CT examination in patients with malignant uveal melanoma
Authors: M. Marko 1; P. Leško 1; D. Jurenová 1; R. Furda 2; M. Greguš 2
Authors‘ workplace: Klinika oftalmológie, Lekárska fakulta Univerzity Komenského a Univerzitná nemocnica, Nemocnica Ružinov, Bratislava, Prednosta: doc. MUDr. Krásnik Vladimír, Ph. D. 1; Katedra informačných systémov, Fakulta managementu Univerzity Komenského, Bratislava, Vedúci katedry: prof. RNDr. Greguš Michal, Ph. D. 2
Published in: Čes. a slov. Oftal., 76, 2020, No. 1, p. 37-44
Category: Original Article
doi: https://doi.org/10.31348/2020/5Overview
Introduction: Diagnostic and therapeutic management of the patient with malignant uveal melanoma (MMU) is subject to ongoing efforts to innovate. PET/CT (Positron Emission Tomography / Computed Tomography) examination is important in both diagnosis and metastases.
Material and methods: Evaluation of the importance of PET/CT examination in the group of patients diagnosed with MMU in the period 12.1.2016 to 6.12.2018. All patients with a diagnosis of secondary retinal detachment, suspected uveal melanoma, underwent standard examinations to detect possible metastases (liver ultrasound, chest X-ray). Patients for whom a stereotactic radiosurgery solution was planned due to the stage of the disease this examination was to exclude metastasis in the liver or lungs. PET/CT examination is part of the protocol within the exclusion criteria for treatment with stereotactic radiosurgery in one day session surgery.
Results: In the group of 84 patients, 47 women (56 %) and 37 men (44 %) were aged between 26 and 90 years. Their average age was 61.4 years. The median group was 64 years, modus 65 years.
Of 84 patients, 79 (94 % of cases) had a diagnosis of C69.3 (choroidal melanoma) and 5 patients (6 % of cases) had a diagnosis of C69.4 (ciliary body melanoma).
Subsequent PET/CT examination in many patients did not reveal hypermetabolic manifestations that could involve various pathological processes, in others the radiopharmaceutical was captured in the primary tumor area of the uveal tract.
Hypermetabolism in eye globe was only found in melanomas with a volume of more than 0.5 cm3.
PET/CT examinations were 85, with one patient undergoing examination twice.
However, in 25 patients (26 examinations), the radiopharmaceutical was taken up in places that subsequently required closer attention. The initial aim of the examination was to locate possible metastases of MMU. In the others, 3 incidents have been reported: increased metabolism in the lung and liver, thyroid and mediastinal lymph nodes.
Of the 85 examinations, 26 (30.6 %) resulted in a hypermetabolic manifestation of accumulation, which was not located in the eye tract, resp. right in the eye. Two malignancies (prostatic carcinoma and rectosigmal carcinoma) have occurred in two patients. Very important was the discovery of MMU metastasis in the liver, which confirmed the important role of PET/CT examination in the management of MMU patients. The metastasis was discovered after repeated PET/CT examination.
Conclusion: PET/CT examination is a technically demanding examination and is one of the possibilities of imaging intraocular melanoma in tumors with volume more than 0.5 cm3. It is important in determining the grading and staging of the disease before radiosurgical treatment and also in detecting possible metastases after MMU treatment in cases where ultrasound or MRI examinations do not give a definite result.
However, our study confirmed the significance of this examination for randomly detected 2 duplex malignancies (2.4%) and 3 incidentalomas (3.6%) in patients whose ophthalmologist diagnosed uveal melanoma and sent patients for full-body PET/CT examination.
Keywords:
18-FDG PET/CT – uveal melanoma – choroidal melanoma – ciliary body melanoma
INTRODUCTION
Malignant melanoma is the most commonly occurring oncological disorder in patients of adult age [15]. Its symptoms appear suddenly and have a dramatic influence on the life of the patient [13,18].
Diagnostic and therapeutic management of patients with this pathology is continually undergoing attempts at innovation. One of the options for exclusion of the possibility of metastases in the patient is PET/CT (Positron Emission Tomography / Computer Tomography) examination. In recent years, this examination has started to be applied also in ophthalmology, especially in determining the stage of the pathology before primary treatment, as well as in contentious cases, in which it is not possible to exclude the possibility of metastasis by ultrasound examination. It is also significant in the monitoring of patients after treatment for uveal melanoma.
Malignant uveal melanoma (MUM) is an oncological disorder, which originates from melanocytes. It occurs more frequently with advancing age in both sexes, and its initial stages are often without symptoms. In addition to other factors, the most common cause of its appearance is genetic abnormalities. With increasing age, its potential to form metastases increases, especially in the liver and lungs [16].
Today research is focused on seeking the epigenetic mechanisms, in an endeavour to understand the origin and development of the tumour in the early stage and the transition to a metastatic disorder. Some chromosomal anomalies such as deletion of the chromosome 1p, monosomy of chromosome 3 or acquisition of chromosome 8q, correlate very strongly with a poor prognosis for survival of patients with uveal melanoma. The chromosomal aberration monosomy of chromosome 3 occurs most frequently and is found primarily in metastasising tumours [22,29].
A broad range of examinations are used for its diagnosis, while treatment relies especially upon a radiosurgical solution, and in severe cases on enucleation of the eyeball. Management of such patients during diagnosis and therapy includes a PET/CT examination, which following uptake of the radiopharmaceutical 18F-FDG and fusion with CT provides a full-body image on the localisation of the primary MUM pathology and other pathological units in the body of the patient, in which an accumulation of the radiopharmaceutical is displayed. This examination may be used before the indication of the patient for treatment, e.g. in certain centres it is a component of the preoperative protocol before stereotactic radiosurgery [14,17,19,20].
The PET examination has primarily been used for assessing the metabolism of the brain with the aid of determining the blood flow to a certain region, for example for measuring the decrease in through-flow in a certain region in an epileptic patients or for differentiating a tumour from radiation necrosis, which may occur after a therapeutic process. The PET/CT method uses positron radiation, i.e. radionuclides which emit positrons, or positively charged particles. These are generated upon β+ breakdown of a radioactive element, they are the size of an electron, but unlike an electron they have a positive charge. This is then subject to annihilation with an electron, in which two photons are generated, spreading in a 180° angle with substantial energy. These photons are captured on two opposite detectors, which are connected by a coincidental circuit. The detectors on the PET cameras require special scintillators with a higher density and higher atomic number, at present a detector based on gadolinium and lutetium is used. A 3D image is produced by computer processing, and after the CT examination a fusion of these two images takes place. The patient is applied a radioactive isotope of fluorine, the carrier of which is a glucose substance intrinsic to the body (FDG – fludeoxyglucose). The isotope 18F is artificially produced in a cyclotron, it has an advantageous half-life of 110 minutes. Isotopes with a longer half-life place a greater burden on the patient by means of ionising radiation. Tissues with high glucose consumption are capable of absorbing it in a larger quantity. In addition to tumours, inflammatory lesions also typically have an intensive glucose mechanism, although in addition to the glucose carrier they also capture the radioactive substance upon examination. Such lesions can thus be colour-differentiated, and subsequently they can be precisely localised within the body through connection with CT. Without CT it would be possible to see an active lesion, but it would not be possible to determine its precise localisation [28]. Before the examination itself, the patient must adhere to a certain regimen (without any intake of nutrition also intravenously, including intravenous administration of fluids with a content of dextrose, for 6 hours before the examination). It is important to ensure that no competitive inhibition of 18F-FDG intake takes place, in connection with glucose in foodstuffs, and to ensure that the insulin level in serum attains the basic values [31]. The radiopharmaceutical is administered to the patient intravenously. After the elapse of the accumulation phase, i.e. after 60 minutes, recording of images of the patient takes place, lasting for approximately 45 minutes. The 18F-FDG PET method is used in the diagnosis of a wide spectrum of tubercular, as well as not primarily oncological disorders [3-7]. It is highly valuable in the detection of recurrences in patients with increasing values of tumour markers without clinical symptoms, and has been demonstrated to represent a solution in cases in which other display modalities do not demonstrate a clear finding. At the same time, it enables monitoring of response to treatment. Clinical indications include evaluation of the scope of the pathology in known malignancies, detection of recurrence of a tumour in the presence of raised tumour markers, identification of an unknown primary lesion upon presence of metastases, evaluation of reaction to chemotherapy and radiotherapy, differentiation of benign and malignant lesion and selection of suitable location for targeting biopsy [7,9,11,24,26,32].
Reliable methods of staging are of decisive importance for optimal care of patients with orbital and ocular malignancies. The PET/CT method has been demonstrated to be one of the possible reliable staging tools in the field of ophthalmological oncology. In the detection of primary ocular or orbital lesions its significance is comparable with clinical ophthalmological examination and other imaging methods. Its significance consists in the detection of remote metastatic lesions which are not identified by other conventional imaging methods. Whereas in other areas of oncology, the possibilities of use were discovered much earlier, in the field of ophthalmology the use of PET/CT was not applied until later. Today this examination is now being used with increasing frequency as a significant aid in determining staging in cases of orbital tumours, lymphomas, retinoblastomas invading the orbit, and carcinomas. Intensive intake of 18F-FDG has been demonstrated in cases of carcinoma of the Merkel cells, which is typical for its intensive growth and frequent formation of metastases. In cases of MUM, PET/CT examination is capable of detecting metabolic activity of choroidal melanomas, and a positive correlation also exists between the size of the melanoma and its capacity for uptake of the radiopharmaceutical. A significant role is played by PET/CT in the process of identifying remote metastases of MUM [23].
MATERIAL AND COHORT
A retrospective study was conducted on 84 patients, from whose health records data was obtained about the age and sex of the patients, their diagnosis, date of examination and application dose in MBq, and of the result of the examination and subsequent therapy. Each patient had a confirmed growth of MUM by a clinical examination, ultrasound examination and magnetic resonance imaging. All the patients with a diagnosis of secondary retinal detachment and suspected uveal melanoma underwent a standard examination in order to determine potential metastases (ultrasound of liver, X-ray of chest). In patients in whom stereotactic radiosurgery was planned with regard to the stage of the pathology, and in the case that this examination did not confirm metastases, e.g. in the liver or the lungs, a radiosurgical procedure was indicated. A PET/CT examination is a part of the protocol within the framework of the exclusion criteria for stereotactic treatment within the framework of single-dose radiation.
RESULTS
Our cohort comprised 84 patients, numbering 47 women (56 %) and 37 men (44 %) aged from 26 to 90 years, with an average age of 61.4 years, and covered the period from 12.1.2016 to 6.12.2018. The average age of the men was 58.7 years and the women 63.5 years. The oldest patient was a woman aged 90 years, the youngest patients was also a woman, aged 26 years (Graph 1). The median age of the cohort was 64 years, the modus 65 years.
1. Age distribution in cohort of patients 
In 2016 a total of 23 examinations (27 %) were performed, followed by 49 examinations (58 %) in 2017, and 13 examinations (15 %) in 2018. Of 84 patients, 79 (94 % of cases) had a determined diagnosis of C69.3 (malignant tumour of the choroid) and 5 patients (6 % cases) had a diagnosis with code C69.4 (malignant tumour of the ciliary muscle).
Hypermetabolisation in the eyeball was determined only in the case of melanomas with a volume of more than 0.5 cm3 (Fig. 1).
1. PET/CT examination – arrow indicates capturing of radiopharmaceutical in the region of the uveal melanoma 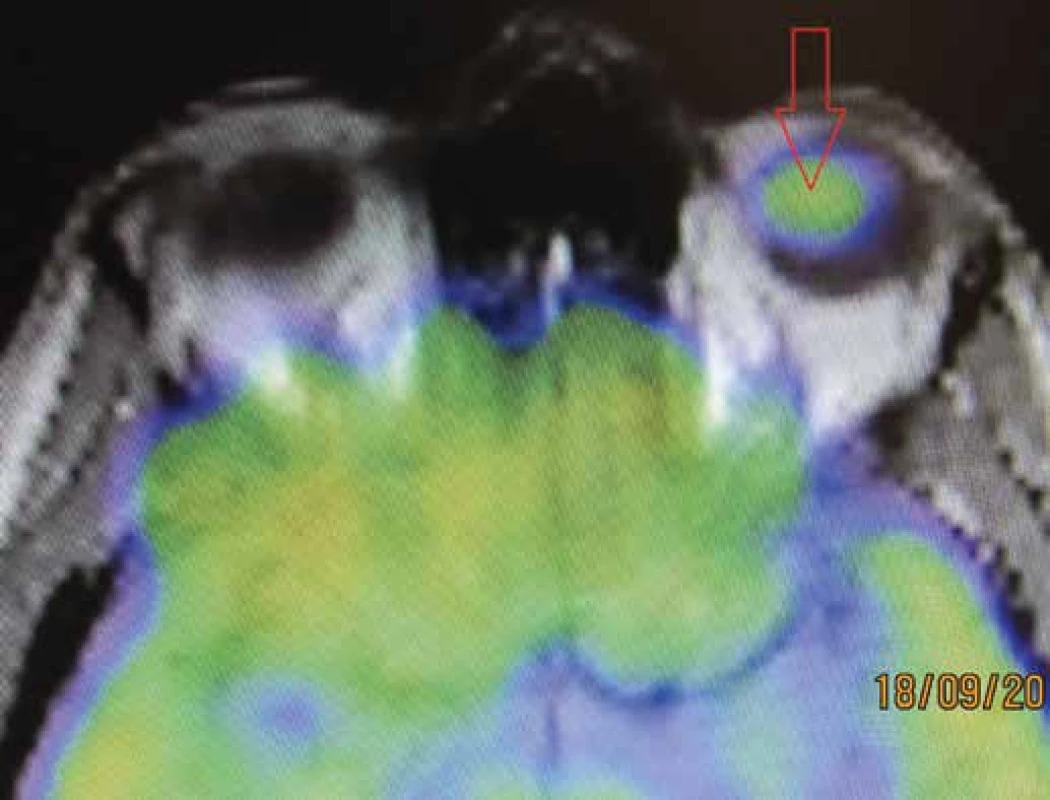
A total of 85 PET/CET examinations were conducted, in which one patient underwent an examination twice for technical reasons.
In 25 patients (26 examinations), however, the radiopharmaceutical was uptaken in places which subsequently demanded closer attention. The original aim of the examination was to localise any applicable metastases of MUM. This succeeded in 1 patient upon repeated PET/CT examination. In the other patients 3 incidentalomas were discovered: increased metabolisation in the region of the lungs and liver, thyroid gland and mediastinal lymph nodes.
Of 85 examinations, 26 (30.6 %) concluded with a hypermetabolic manifestation of accumulation, which was not localised in the ocular tract or directly in the eye (Table 1). This concerned pathological conditions which may have had a direct correlation with the growth of the MUM, but may also have been manifestations of other pathologies, which was subsequently assessed by specialist doctors in the given field. The results of these 26 examinations were not necessarily always concluded with a finding of a specific pathology, but the presence of serious pathologies, of which no symptoms were demonstrated at the time of hte PET/CT examination, was demonstrated by means of subsequent targeted examinations.
1. Overview of further PET/CT findings beyond the primary pathology 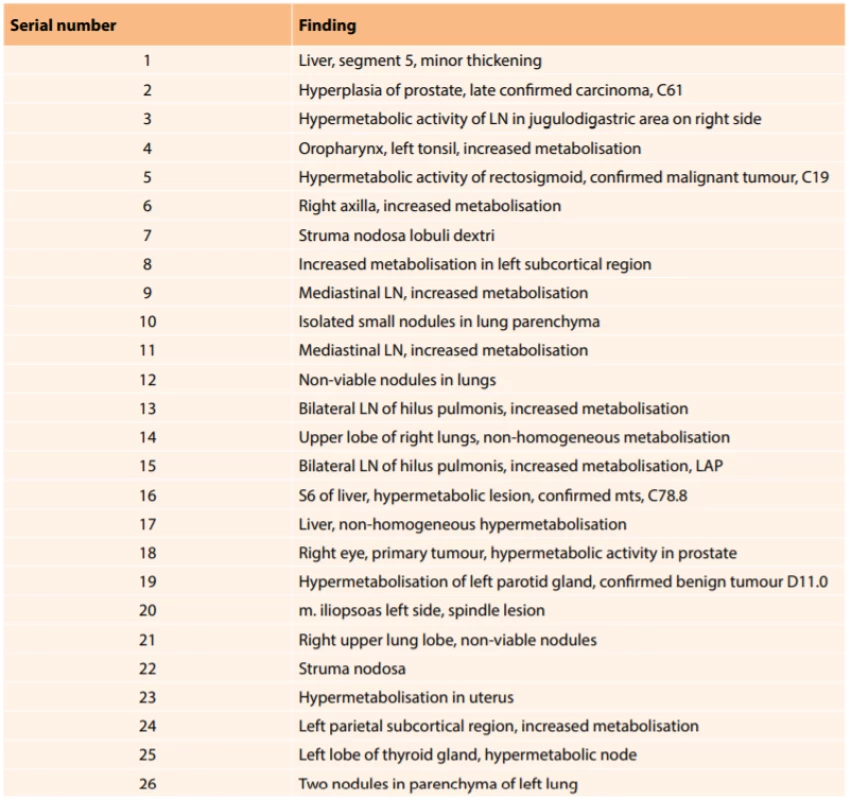
Note: LN – lymph nodes, C61 – malignant tumour of prostate, C19 – malignant tumour of rectosigmoid junction, LAP – lymphadenopathy, C78.8 – secondary malignant tumour of other unspecified digestive organs, S6, segment no. 6, D11.0 – benign tumour of relevant gland In our cohort, however, the significance of this examination was confirmed in a chance finding of 2 duplex malignancies (2.4 %) and 3 incidentalomas (3.6 %) in patients in whom the ophthalmologist diagnosed uveal melanoma and sent the patients for a full-body PET/CT examination.
Some of the findings demonstrated pathological activity which did not represent a risk to the patient’s life, and after subsequent examinations did not require further treatment, but some findings constituted a serious danger to the patient’s life. For example, in addition to the determined pathologies of the thyroid gland and manifestations in the lymph nodes and lungs, we discovered in particular two malignant pathologies of the prostate and rectosigmoid colon, and a benign tumour in the left parotid gland. A very important finding was metastasis of MUM in the liver, which confirmed the important role of PET/CT examination in the management of patients with MUM. Metastasis was determined after a repeated PET/CT examination.
DISCUSSION
A routine evaluation of staging of MUM covers a physical examination, ultrasonography of the orbit and determination of the local extent of the pathology, examination of the values of liver enzymes and X-ray of the chest. Identification of a primary tumour with the aid of a PET/CT examination is limited, and is not routine for this purpose, especially in the case of a tumour in the early stage. According to Murphy, PET/CT is capable of identifying approximately 33 % of tumours in stage T2 and 75 % of T3 uveal melanomas [25].
Timely management of uveal melanocytic lesions is of vital importance, because any delay in the diagnosis and treatment of the early stages of the tumour may lead to substantial growth, disorders of sight and loss of the eye (enucleation), and in the case of formation of metastatic lesions also to the death of the patient. Ultrasonography of the orbit is used to determine the size and shape of the tumour. Imaging with the aid of CT and MR (magnetic resonance) is not usually used during diagnostic processing if other examinations produce convincing results. An experienced ophthalmologist with practice in oncology is capable of diagnosing uveal melanoma also with the aid of examination of the ocular fundus. However, evaluation of staging and selection of a suitable therapeutic method is complex, and delay of the treatment also in cases of malignancies with a size of less than 2 mm increases the risk of formation of metastases. Staging, evaluated according to the American Joint Committee on Cancer (AJCC), therefore requires the use of all the available diagnostic methods. At present the use of basic X-ray imaging of the chest and abdominal cavity in order to exclude systemic metastases is being phased out due to its low sensitivity. To a large degree X-rays are being replaced by MR and PET/CT. The sensitivity of MR is within the range of 67-92 % and is slightly higher than in PET/CT (35-100 %) [34].
It has been demonstrated that haematological tests have both low sensitivity and low specificity. Eskelin et al. stated that functional tests of the liver and abdominal ultrasonography precisely detected liver metastases in only 59 % of asymptomatic patients with metastates in the liver, and X-ray examination of the chest detected lung metastases in only 2 % of patients with this condition. Also with regard to these limitations of routine methods of observation, PET/CT has the potential to provide a significant contribution. Reddy et al. [27] stated that metabolic activity of a choroidal melanoma was determined by PET/CT examination, which was most effective in detection of stage T3 and larger choroidal melanomas. At the same time, however, they came to the conclusion that PET/CT was not superior to the standard clinical protocol in treatment. In addition to this, it was not possible to differentiate small melanomas from suspected choroidal nevi. A positive correlation was determined between SUV (Standardised Uptake Value) and size of choroidal melanoma, as well as between other factors such as age, sex or location of the tumour, although a significant correlation was not confirmed. It was demonstrated that full-body PET/CT plays a significant role in the detection of regional and remote metastases from uveal melanoma. Its contribution is therefore all the more important in cases of patients with normal functional liver tests and metastases which could not be detected by abdominal ultrasonography for various reasons. In the case of extrahepatic metastases, especially in the bones, PET/CT enables differentiation of benign and malignant lesions, whereas CT alone does not have this capacity. In addition to this, PET/CT is used to determine the stage of MUM, and is used as a non-invasive method also for assessing the risk of formation of metastases from the primary lesion.
Finger et al. [12] determined that a positive correlation exists between higher SUV and larger MUM. Since a larger diameter of the tumour ranks among broadly accepted risk factors of formation of metastases, in fact statistically significant, Finger came to the conclusion that PET/CT may be an effective biomarker of the metastatic potential of MUM. Studies exist which cast doubt upon the value of using the PET/CT method in the detection of a primary MUM and metastases in the liver. Strobel et al. stated that in 13 patients with MUM, together with 27 known metastases in the liver, 16 liver metastases were negative on 18F-FDG PET/CT, which is 59 %. This runs contrary to a large number of other studies, which did not demonstrate such negative results. They also determined that SUV for liver metastases from MUM was markedly lower (value of 3.5) than in the case of metastases in the liver from skin melanoma. Strobel defended the results of his study by stating the theory according to which other studies without negative results included only patients with positive findings on PET [30].
Although less than 1 % of patients have a metastatic pathology at the time of the initial diagnosis, metastases subsequently develop in the majority of them over various lengths of time. Monitoring of metastases is therefore of key importance for patients with MUM. The most common location of formation of metastases is the liver, and the prognosis of the patient depends on its treatment. As a result, imaging of metastases in the liver is essential, for which in addition to PET/CT, MR is also used as the most specific modality, with a similar level of sensitivity as CT. The capacity for uptake of a radiopharmaceutical by metastases of MUM is on a similar level as in the case of metastases of skin melanoma. The level of uptake of 18F-FDG by the liver itself, which leads to a poor resulting identification of the target-background ratio, is a problem in detection of small lesions. This is less of a problem in the case of lesions of larger dimensions [2].
On the basis of the predominant formation of metastases in the liver, tests of liver enzymes are the most usual haematological evaluation performed following treatment of a patient with MUM. In 1985, the Collaborative Ocular Melanoma study requested regular medical examinations, including a physical examination, study of liver function, complete blood count and X-ray examination of chest. If the liver enzymes exceed 1.5 times the normal value, a CT examination of the abdomen is necessary [21]. With the introduction of PET/CT into diagnosis, possibilities were discovered of detecting occult metastatic melanoma, an example of which is the case of a female patient published in 2004 in the British Journal of Ophthalmology. The patient, a 77 year old woman, underwent enucleation, evaluated as the appropriate method of treatment. Two years later, increased liver functions and pleural exudate were determined. CT of the abdominal cavity demonstrated several lesions in the liver, which had a consistency similar to metastatic melanoma. After the performance of PET/CT and imaging of the whole body, large metastases were confirmed in the liver, and at the same time enlarged paraaortic lymph nodes and a subcutaneous nodule in the abdominal wall were displayed. The PET part of the image detected multiple bone metastases, which were not observed on CT. In this case PET/CT succeeded in detecting metastases which were not detected by abdominal CT, which led doctors to consider a resection of the liver and directed them toward systemic therapy. This case demonstrated a significant influence of PET/CT in identifying extrahepatic affliction and in the management of patients with metastatic uveal melanoma [12].
Although histology still provides the most precise information, in many cases PET/CT brings about an optimisation of staging of a tubercular pathology. In a retrospective study of 522 patients with bronchial carcinoma who underwent PET/CT with the use of 18F-FDG in the period of 2008 to 2010, Taus et al. evaluated a positive contribution of this examination. Out of 246 patients who underwent PET/CT, a change of staging occurred in 85 cases (34.6 %) following the examination. The treatment was modified in 60 patients (24.4 %), while in 13 patients (5.2 %) thoracotomy was not required [33]. PET/CT examination is applied also in a range of other types of oncological disorders, in the diagnosis of colorectal carcinomas, head and neck tumours, in gynaecology and others. Its sensitivity and specificity varies according to each type of tumour. In addition, each type of tumour manifests a different affinity to the used pharmaceutical. In the diagnosis of skin melanomas, it does not become significant until stages III and IV (according to AJCC), while it manifests 100 % sensitivity to metastases in visceral and abdominal nodes and 100 % precision for metastases of the superficial lymph nodes, but low sensitivity for pulmonary metastases. In the imaging of primary tumours and metastatic lesions in the region of the brain, metabolic activity of the brain tissue is frequently a problem. According to the data, however, it is possible to evaluate that this examination predicts the response of the tumour to therapy, and that the clinical indications for its use will be extended [1,8,10].
In our cohort, however, the significance of this examination was confirmed for 2 duplex malignancies (2.4 %) and 3 incidentalomas (3.5 %) detected by chance in patients in whom the ophthalmologist had detected uveal melanoma and who were commencing therapy. A study by Cohen et al. [10] confirmed that full-body PET/CT and ultrasound of the liver mutually complement one another in determining the staging of uveal melanoma. Some lesions in the liver determined by ultrasound can be evaluated as potential metastases, but may in fact be benign lesions. However, an important factor in PET/CT full-body examination is that it is possible to identify also other symptomless malignancies in patients we sent for full-body PET/CT if an ophthalmologist detects a uveal melanoma. In the cohort in the study by Cohen et al. [10] this was 1 out of 10 cases, in our cohort we determined this in a total of 5 patients (5.9 %) - two carcinomas and three incidentalomas in the first full-body PET/CT, which we indicated as the first examination in patients with uveal melanoma before the commencement of treatment.
CONCLUSION
PET/CT examination is one of the imaging methods for primary pathology of the uveal tract and its secondary manifestations at the time of diagnosis, therapy and subsequent follow-up examinations. In our cohort of 85 patients, 59 had a negative result, thus without hypermetabolic radiopharmaceutical in the patient’s body, or the radiopharmaceutical was metabolised in the area of growth of the primary tumour. As many as 26 examinations demonstrated hypermetabolisation in another region of the patient’s body, which could have been a secondary manifestation of the pathology, or concerned a new, unknown pathology detected during the examination. Other manifestations of hypermetabolisation meant new pathologies discovered by the examination, which included 3 incidentalomas. In addition to these there were disorders of the thyroid gland, nodules in the lungs, inflammatory manifestations in the regions of the lymph nodes and others. In some cases these pathologies did not require closer attention following further examinations, although some had a significant influence on the future life of the patient. Within the framework of ophthalmology, this examination has an immense contribution in determining the grading and staging of MUM.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company. The authors further declare that the study has not been submitted to any other journal or printed elsewhere, with the exception of congress abstracts and recommended procedures.
Sources
1. Almuhaideb, A., Papathanasiou, N., Bomanji, J.: 18F-FDG PET/CT imaging in oncology. Ann Saudi Med, 31 (1); 2011 : 3–13.
2. Balasubramanya, R., Selvarajan, SK., Cox, M. et al.: Imaging of ocular melanoma metastasis. Br J Radiol, 89 (1065); 2016 : 20160092.
3. Balogova, S., Huchet, V., Kerrou, K. et al.: Detection of bronchioloalveolar cancer by means of PET/CT and 18F-fluorocholine, and comparison with 18F-fluorodeoxyglucose. Nucl Med Commun, 31 (5); 2010 : 389–97.
4. Balogova, S., Talbot, J-N., Nataf, V. et al.: 18F-fluorodihydroxyphenylalanine vs other radiopharmaceuticals for imaging neuroendocrine tumours according to their type. Eur J Nucl Med Mol Imaging, 40 (6); 2013 : 943–66.
5. Balogova, S., Zakoun, JB., Michaud, L. et al.: Whole-body 18F-fluorocholine (FCH) PET/CT and MRI of the spine for monitoring patients with castration-resistant prostate cancer metastatic to bone: a pilot study. Clin Nucl Med, 39 (11); 2014 : 951–9.
6. Bozkurt, MF., Virgolini, I., Balogova, S. et al.: Erratum to: Guideline for PET/CT imaging of neuroendocrine neoplasms with 68Ga-DOTA-conjugated somatostatin receptor targeting peptides and 18F-DOPA. Eur J Nucl Med Mol Imaging, 44 (12); 2017 : 2150–1.
7. Bozkurt, MF., Virgolini, I., Balogova, S. et al.: Guideline for PET/CT imaging of neuroendocrine neoplasms with 68Ga-DOTA-conjugated somatostatin receptor targeting peptides and 18F-DOPA. Eur J Nucl Med Mol Imaging, 44 (9); 2017 : 1588–601.
8. Brovkina, AF: [Local treatment of choroidal melanoma: possibilities and limitations]. Vestn Oftalmol, 134 (4); 2018 : 52–60.
9. Cassou-Mounat, T., Balogova, S., Nataf, V. et al.: 18F-fluorocholine versus 18F-fluorodeoxyglucose for PET/CT imaging in patients with suspected relapsing or progressive multiple myeloma: a pilot study. Eur J Nucl Med Mol Imaging, 43 (11); 2016 : 1995–2004.
10. Cohen, VML., Pavlidou, E., DaCosta, J. et al.: Staging Uveal Melanoma with Whole-Body Positron-Emission Tomography/Computed Tomography and Abdominal Ultrasound: Low Incidence of Metastatic Disease, High Incidence of Second Primary Cancers. Middle East Afr J Ophthalmol, 25 (2); 2018 : 91–5.
11. Fartoux, L., Balogova, S., Nataf, V. et al.: A pilot comparison of 18F-fluorodeoxyglucose and 18F-fluorocholine PET/CT to predict early recurrence of unifocal hepatocellular carcinoma after surgical resection. Nucl Med Commun, 33 (7); 2012 : 757–65.
12. Finger, PT., Kurli, M., Wesley, P. et al.: Whole body PET/CT imaging for detection of metastatic choroidal melanoma. Br J Ophthalmol, 88 (8); 2004 : 1095–7.
13. Furdová, A.: Nové trendy v liečbe malígneho melanómu uvey. In: Trendy soudobé oftalmologie. Galén; 2007, s. 15–35.
14. Furdova, A., Horkovicova, K., Justusova, P. et al.: Is it sufficient to repeat LINEAR accelerator stereotactic radiosurgery in choroidal melanoma? Bratisl Lekárske Listy, 117 (8); 2016 : 456–62.
15. Furdová, A., Oláh, Z.: Malígny melanóm v uveálnom trakte. Bratislava: Asklepios; 2002, 175 s.
16. Furdová, A., Oláh, Z.: Nádory oka a okolitých štruktúr. Brno: Akademické nakladatelství CERM; 2010, 152 s.
17. Furdova, A., Slezak, P., Chorvath, M. et al.: No differences in outcome between radical surgical treatment (enucleation) and stereotactic radiosurgery in patients with posterior uveal melanoma. Neoplasma, 57 (4); 2010 : 377–81.
18. Furdova, A., Sramka, M.: Uveal malignant melanoma and stereotactic radiosurgery: Intraocular uveal melanoma and one-day session stereotactic radiosurgery at linear accelerator. Saarbrücken: LAP LAMBERT Academic Publishing; 2014, 188 p.
19. Furdová, A., Šramka, M., Waczulíková, I. et al.: [Stereotactic Rediosurgery for Uveal Melanoma; Postradiation Complications]. Cesk Slov Oftalmol, 71 (3); 2015 : 134–42.
20. Furdova, A., Strmen, P., Waczulikova, I. et al.: One-day session LINAC–based stereotactic radiosurgery of posterior uveal melanoma. Eur J Ophthalmol, 22 (2); 2012 : 226–35.
21. Honavar, SG.: Is Collaborative Ocular Melanoma Study (COMS) still relevant? Indian J Ophthalmol, 66 (10); 2018 : 1385–7.
22. Horkovičová, K., Markus, J., Krčová, I. et al.: [The BRAF mutation and the possibilities of uveal melanoma metastasing prognostic markers identification]. Cesk Slov Oftalmol, 72 (4); 2016 : 149–56.
23. Hui, K-H., Pfeiffer, ML., Esmaeli, B.: Value of positron emission tomography/computed tomography in diagnosis and staging of primary ocular and orbital tumors. Saudi J Ophthalmol Off J Saudi Ophthalmol Soc, 26 (4); 2012 : 365–71.
24. Jorgov, L., Montravers, F., Balogova, S. et al.: Paediatric and adolescent Hodgkin lymphoma: information derived from diffuse organ uptake of 18 F-fluorodeoxyglucose on pre-treatment and on interim PET/CT. Eur J Nucl Med Mol Imaging, 43 (7); 2016 : 1220–30.
25. Murphy, G., Hussey, D., Metser, U.: Non-cutaneous melanoma: is there a role for (18)F-FDG PET-CT? Br J Radiol, 87 (1040); 2014 : 20140324.
26. Périé, S., Hugentobler, A., Susini, B. et al.: Impact of FDG-PET to detect recurrence of head and neck squamous cell carcinoma. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg, 137 (4); 2007 : 647–53.
27. Reddy, S., Kurli, M., Tena, LB. et al.: PET/CT imaging: detection of choroidal melanoma. Br J Ophthalmol, 89 (10); 2005 : 1265–9.
28. Seidl, Z., Burgetová, A., Hoffmannová, E. et al.: Radiologie pro studium i praxi. Praha: Grada Publishing, a.s.; 2012, 372 s.
29. Smolkova, B., Horvathova Kajabova, V., Zmetakova, I. et al.: Role of epigenetic deregulation in hematogenous dissemination of malignant uveal melanoma. Neoplasma, 65 (6); 2018 : 840–54.
30. Strobel, K., Bode, B., Dummer, R. et al.: Limited value of 18F-FDG PET/CT and S-100B tumour marker in the detection of liver metastases from uveal melanoma compared to liver metastases from cutaneous melanoma. Eur J Nucl Med Mol Imaging, 36 (11); 2009 : 1774–82.
31. Surasi, DS., Bhambhvani, P., Baldwin, JA. et al.: 18F-FDG PET and PET/CT patient preparation: a review of the literature. J Nucl Med Technol, 42 (1); 2014 : 5–13.
32. Talbot, J-N., Fartoux, L., Balogova, S. et al.: Detection of hepatocellular carcinoma with PET/CT: a prospective comparison of 18F-fluorocholine and 18F-FDG in patients with cirrhosis or chronic liver disease. J Nucl Med Off Publ Soc Nucl Med, 51 (11); 2010 : 1699–706.
33. Taus, Á., Aguiló, R., Curull, V. et al.: Impact of 18F-FDG PET/CT in the treatment of patients with non-small cell lung cancer. Arch Bronconeumol, 50 (3); 2014 : 99–104.
34. Weis, E., Salopek, TG., McKinnon, JG. et al.: Management of uveal melanoma: a consensus-based provincial clinical practice guideline. Curr Oncol Tor Ont, 23 (1); 2016: e57-64.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2020 Issue 1-
All articles in this issue
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Current use of the automatic retinal oximetry. Review
- Importance of PET/CT examination in patients with malignant uveal melanoma
- Enucleation after Stereotactic Radiosurgery in Patients with Uveal Melanoma
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Importance of PET/CT examination in patients with malignant uveal melanoma
- Our experience with micropulse cyclophotocoagulation in the therapy of glaucoma
- Visual Training in Virtual Reality in Adult Patients with Anisometric Amblyopia
- Transscleral Extraction of an Intraocular Foreign Body from the Posterior Segment of the Eye without Pars Plana Vitrectomy
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

