-
Medical journals
- Career
Key factors for the development of pressure ulcers in surgical practice
Authors: L. Veverková 1; M. Reška 1; P. Vlček 1; I. Čapov 1; J. Habr 1; J. Konečný 1; P. Doležal 2
Authors‘ workplace: Ist Surgical Department, Medical Faculty of Masaryk University and St. Anne University Hospital of Brno, Czech Republic 1; Consulting s. r. o., Czech Republic 2
Published in: Cesk Slov Neurol N 2019; 82(Supplementum 1): 60-65
Category: Original Paper
doi: https://doi.org/10.14735/amcsnn2019S60Overview
Aim: Pressure ulcers represent a major postoperative complication. We retrospectively analyse data and identify risk factors for the development of pressure ulcers in patients undergoing surgery at the 1st Surgical Clinic of St. Anne’s Hospital in Brno between 2017 and 2018.
Methods: We used data from the hospital’s information system and a purpose-built electronic database (I-hojeni.cz). Statistical analysis was performed using Pearson‘s chi-square at a significance level of 0.05, the variables used included: age, Body Mass Index (BMI), number and grade of pressure ulcers and comorbidities (history of cardiovascular diseases, diabetes mellitus, chronic renal failure, neurological and oncological diseases).
Results: 5,851 inpatients underwent surgery (91.15% of the total of 6,419) between 2017 and 2018. Pressure ulcers newly developed in 86 patients (1.46%), 40 men and 46 women. The patients’ average age was 79.85, age was confirmed as a predictive factor for pressure ulcer formation. The average BMI value was 24.13, the relationship between BMI and development of pressure ulcers was not statistically significant. The average pressure ulcer grade was 2.04 and the average number per patient 1.5. Pressure ulcers mostly developed on the heels, buttocks and sacrum. On average the period between a patient’s admission and operation was 2.79 days (0–16 days), it did not prove to be a factor. 56 patients (65.11%) had a history of neurological disorder – a predictive factor – the correlation was not statistically significant, similarly to oncological diseases 30 (24.41%), 19 patients (22.09%) with pressure ulcers died.
Conclusion: Our study is unique in expanding our understanding of multiple risk factors for the development of pressure ulcers, it suggests that age and a history of neurological disorder in particular are key risk factors while other risk factors generally considered to be significant (mobility, nutritional factors) did not prove so.
Keywords:
incidence – surgical patient – pressure ulcer – pressure sore – age – gender
Introduction
Annually on a global scale some inpatients develop post-operative complications, including pressure ulcers. These can develop in the post-operative period, including in the immediate one [1] and have significant social, medical and economic consequences [2–5]. Risk reduction and the limitation of complications remain major challenges when population ageing and more frequent multimorbidity result in increasing numbers and complexity of surgical interventions. The factors that are the primary cause of pressure ulcers are generally known, a systematic review identified three primary risk factors: mobility/ activity, perfusion (including diabetes) and skin / pressure ulcer status [6]. Our study aims to clarify which patients are at risk of developing pressure ulcers and which risk factors play a key role.
Although many patients are exposed to factors that are the primary causes of pressure ulcers, not all develop them. This is due to the complex and multi-factorial causality and pathophysiology of pressure ulcers [7], it is well known that any of the widely recognized risk factors increases the probability of the development of pressure ulcers if pressure and friction are also present. It is, however, limited mobility that is most important in exposing the individual to constant pressure and friction [8,9]. Although the evaluation of risks forms a key part of clinical practice, it is a demanding task due to the variety of risk assessment tools in use and to their insufficient validity and reliability [10]. Our study retrospectively analyses data and identifies risk factors for the development of pressure ulcers in patients hospitalized and undergoing surgery at the 1st Surgical Clinic of St. Anne’s Hospital in Brno between 2017 and 2018.
Methods
We analysed the records of inpatients who developed pressure ulcers while undergoing surgery in the Clinic between 1. 1. 2017 and 31. 12. 2018. We first identified whether the patient underwent surgery or not – as this is the main factor for the development of pressure ulcers – this was the case for 5,851 inpatients i.e. 91,15% of the total of 6,419 inpatients. The variables that we included in the analysis were: age, Body Mass Index (BMI), number and grade of pressure ulcers and incidence of comorbidities, namely histories of cardiovascular diseases, diabetes mellitus, chronic renal failure, neurological and oncological diseases. We used data from the hospital’s information system as well as data from a purpose-built database (I-hojeni.cz). Statistical analysis was performed using Pearson‘s chi-square at a significance level of 0.05.
Results
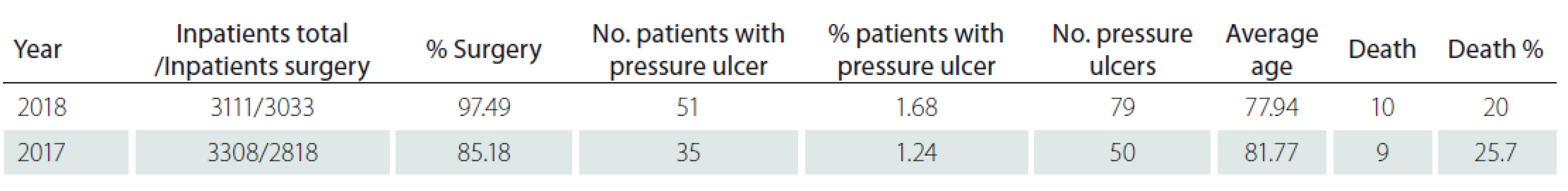
Between 1. 1. 2017 and 31. 12. 2018 the Clinic had a total of 6,419 inpatients, the large majority of whom (5,851 [91.15%]) underwent surgery (Tab. 1).
We evaluated patients with newly developed pressure ulcers, i.e. these developed during hospitalization in the Clinic. We had 86 such cases, i.e. 1.46% of all inpatients. The average age of patients with pressure ulcers was 79.85 (33–101 years) and they were mostly women, 46 women and 40 men (Fig. 1).
1. Number of cases by age and gender.
Obr. 1. Počet pacientů s dekubity rozdělený dle věku a pohlaví.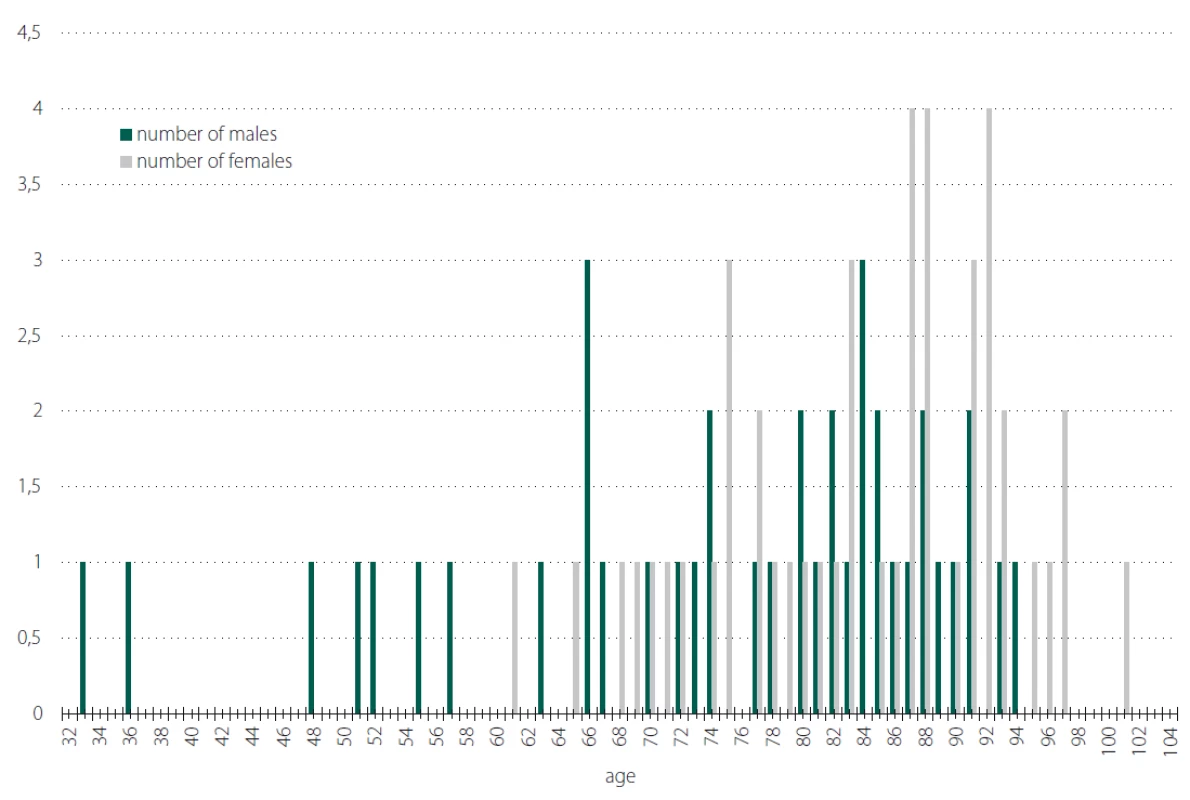
The average BMI value was 24.13, with the extreme values of 13.6 and 40.6. In our sample the BMI value was not a predictive factor for pressure ulcer development as we did not find a statistically significant relationship between the BMI value and the development of pressure ulcers (P > 0.05). The average pressure ulcer grade was 2.04 and the average number of pressure ulcers per patient was 1.5. Most typically pressure ulcers developed on the heels, buttocks and sacrum (Fig. 2).
2. Pressure ulcer location by patient‘s age.
Obr. 2. Počet pacientů s dekubity dle věku a lokalizace.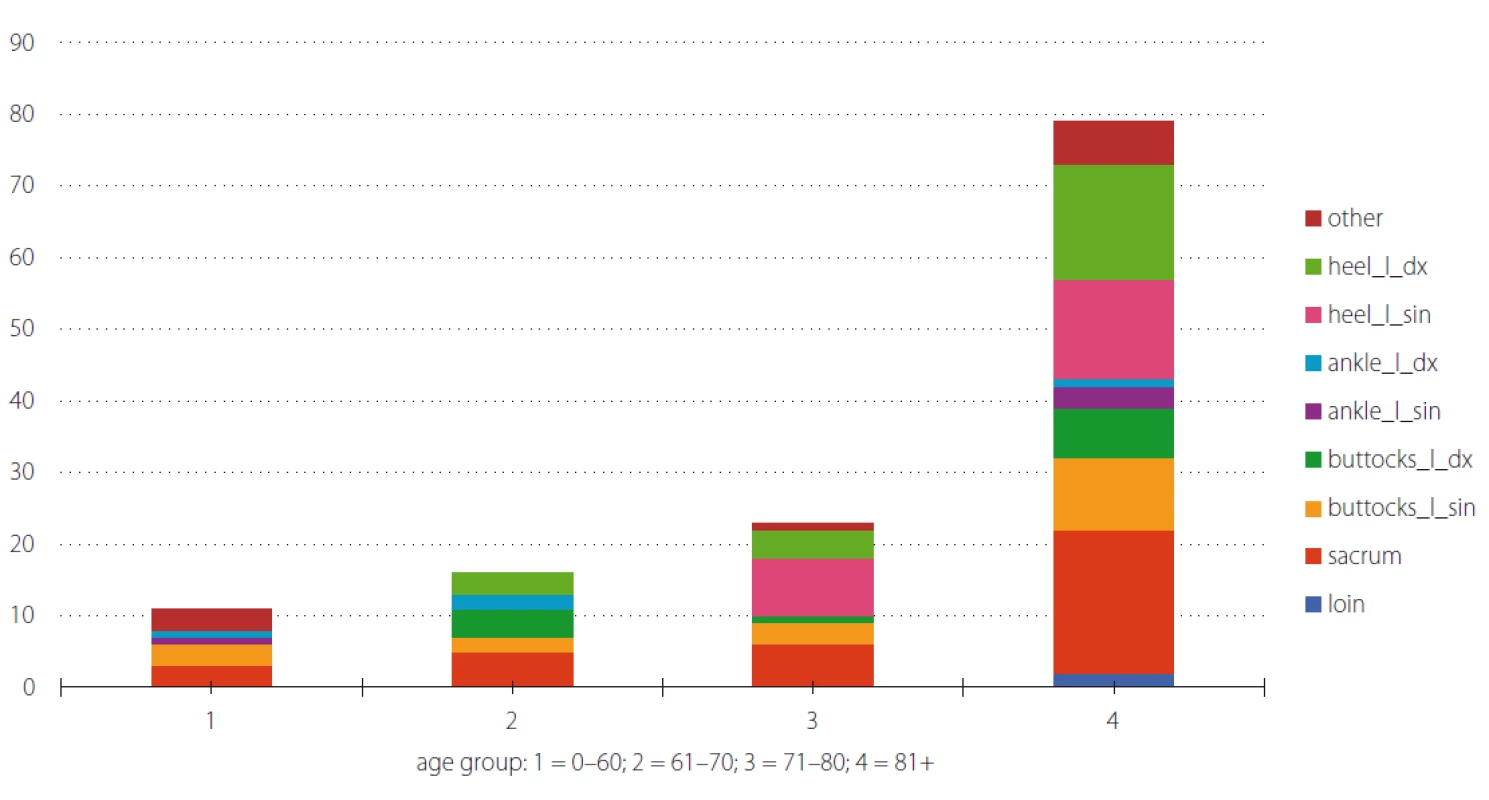
On average the period between a patient’s admission and operation was 2.79 days (0–16 days). Although literature [11–13] refers to the time factor as key for the development of pressure ulcers, it did not apply to our sample. 56 patients (65.11%) had a history of neurological disorder which is considered to be a predictive factor [6,14] but we did not find it statistically significant (Tab. 2–5 and Fig. 3, 4).
2. Patients with pressure ulcer by neurological disorder. 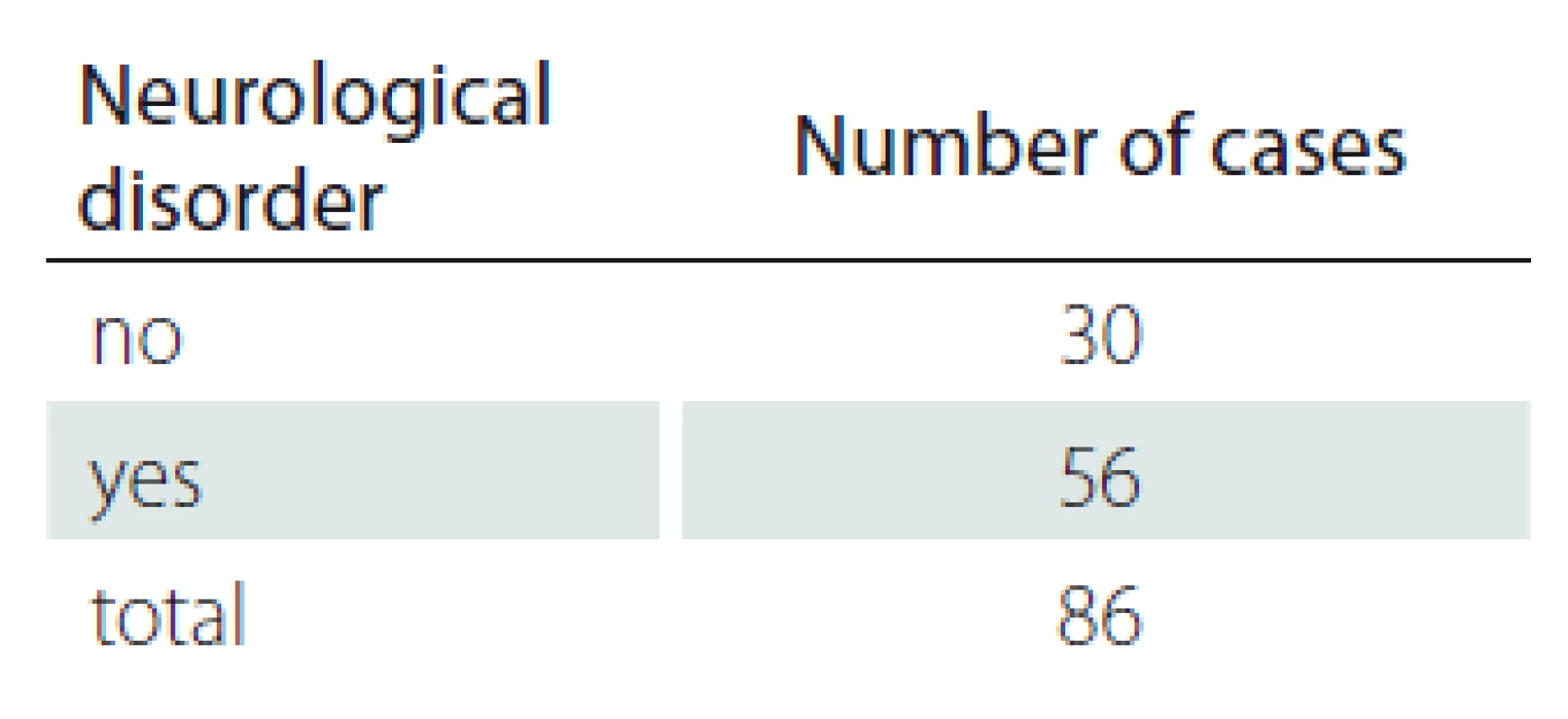
3. Neurological disorders and location of pressure ulcer.
Obr. 3. Typy neurologických onemocnění a lokalizace dekubitů.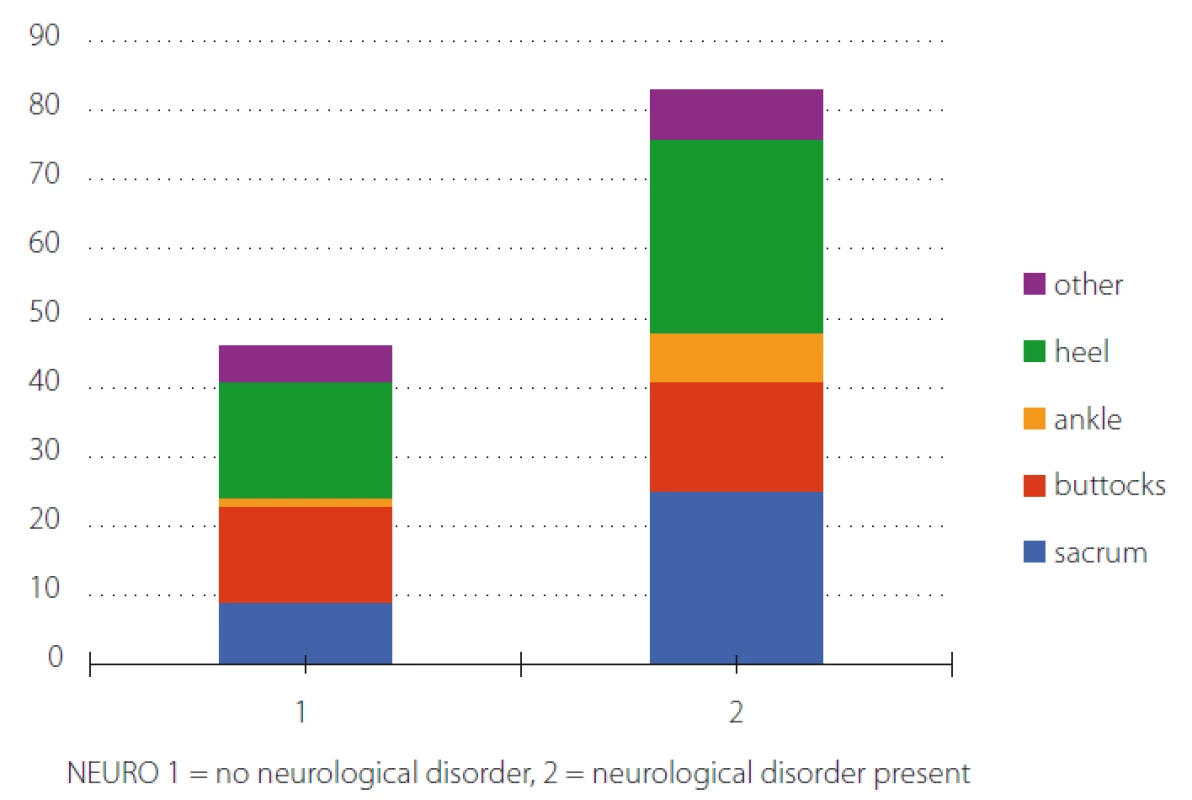
3. Neurological disorder type. 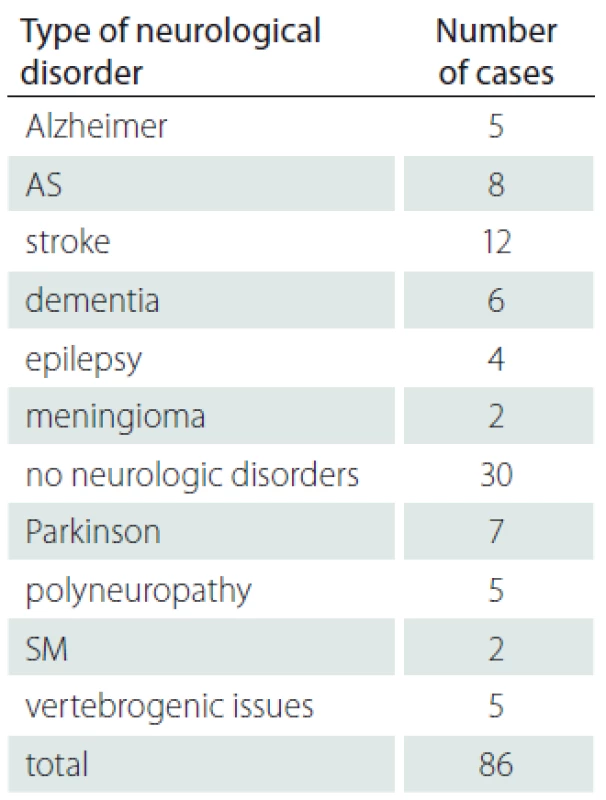
AS – arteriosclerosis; SM – sclerosis multiplex 4. Neurological disorders and localisation of pressure ulcer.
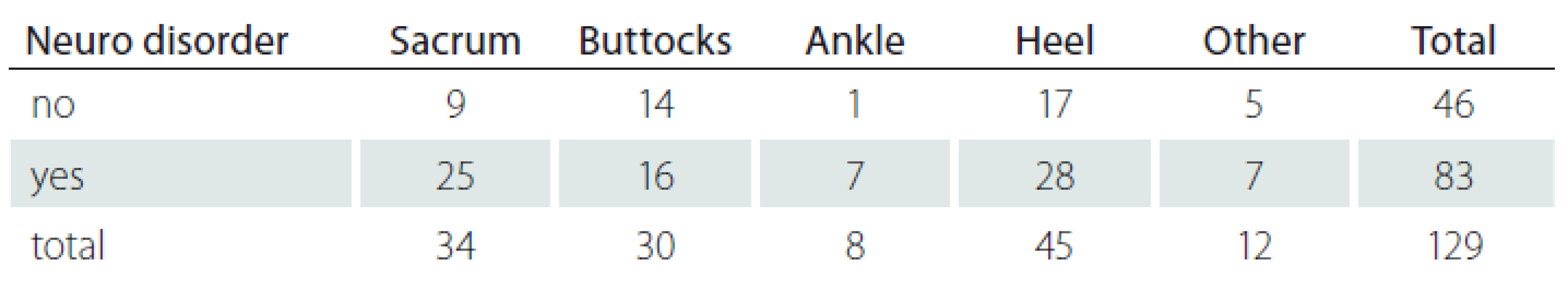
5. Presence of neurological disorder. 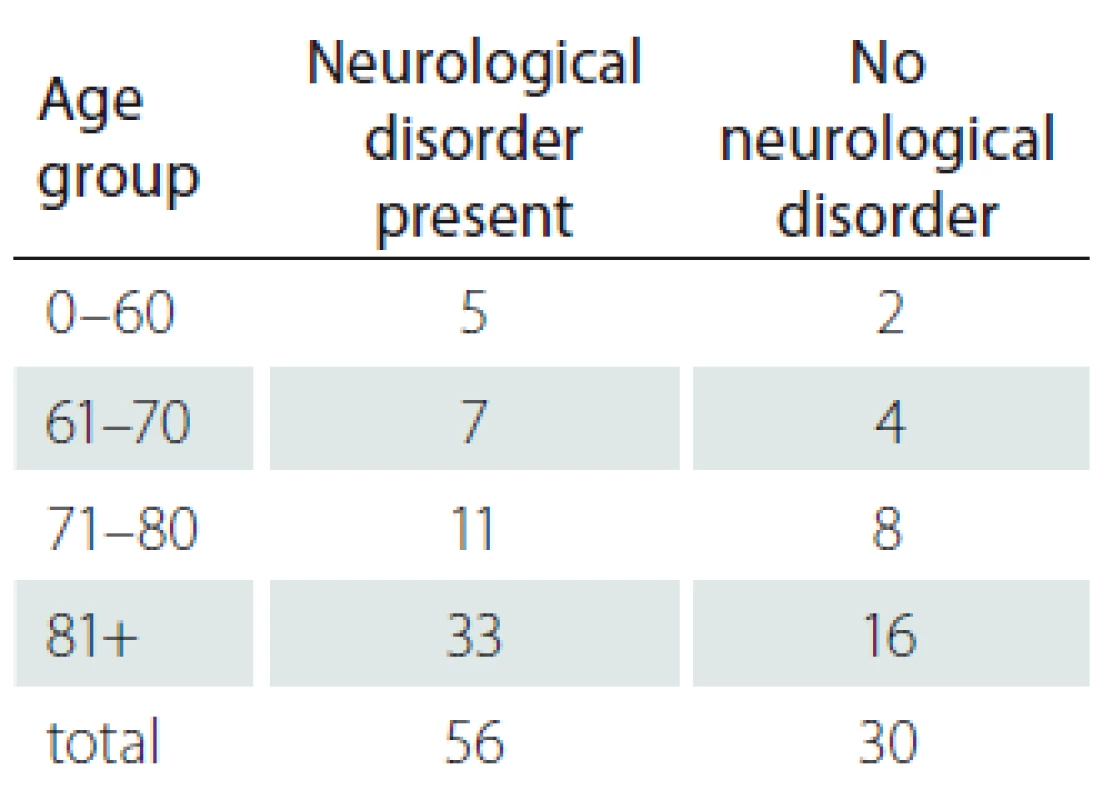
4. Neurological disorder and age distribution.
Obr. 4. Věkové rozložení nemocných s neurologickým onemocněním.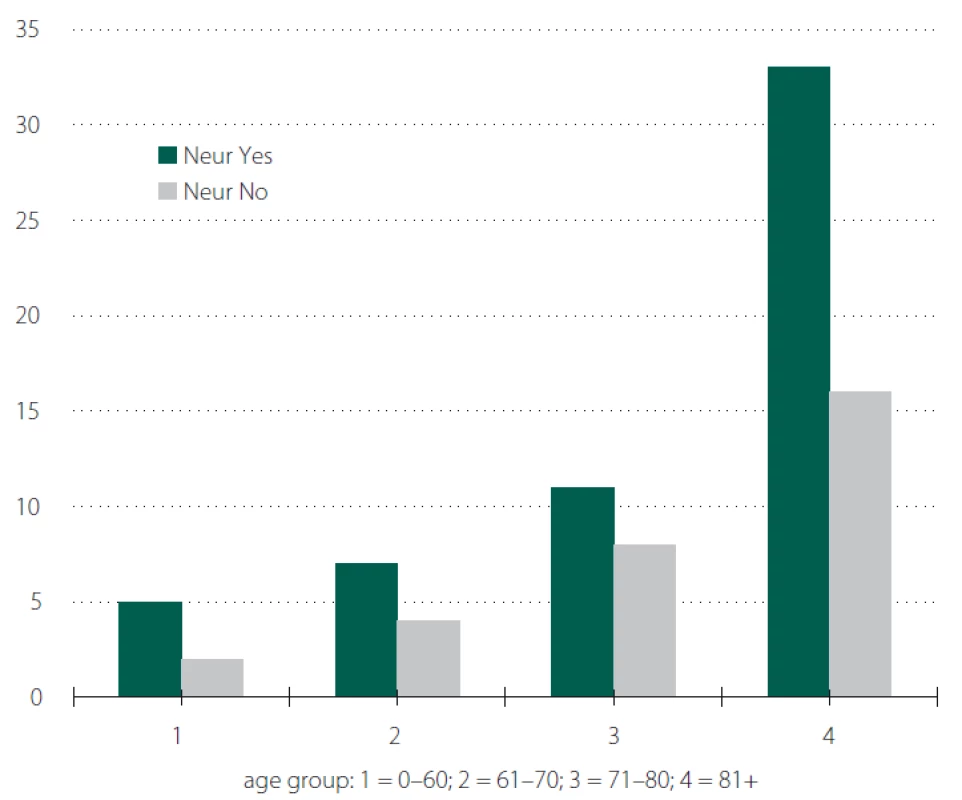
5. Patients‘ age distribution by neoplasms.
Obr. 5. Věkové rozložení nemocných pacientů s dekubity a výskytem nádorů.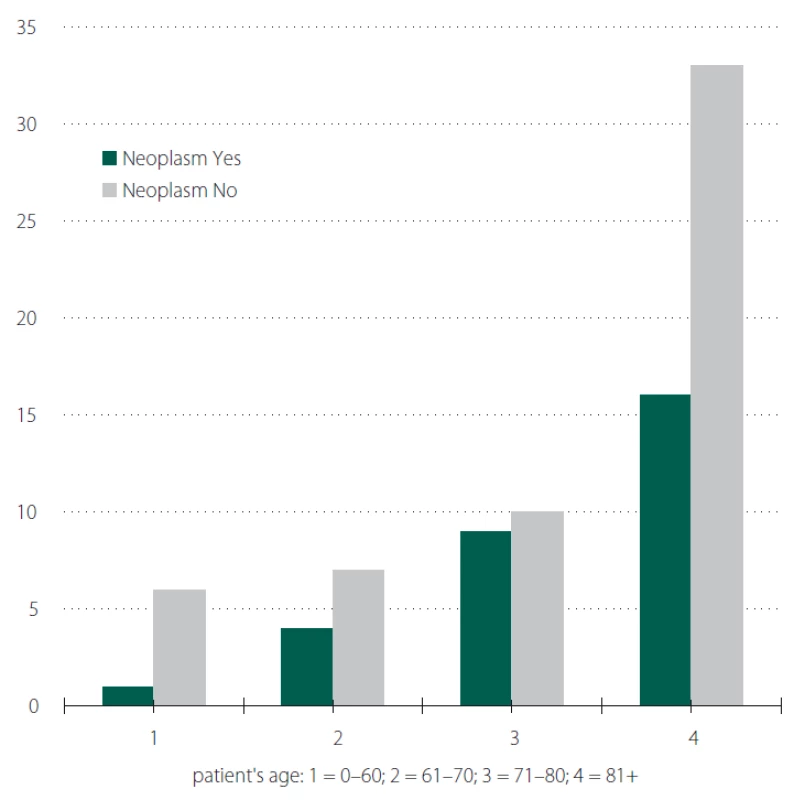
This is similar to the history of oncological illness in 34.9% of patients, we did not find it to be statistically significant (Tab. 6, 7 and Fig. 5, 6).
6. Age distribution by neoplasms. 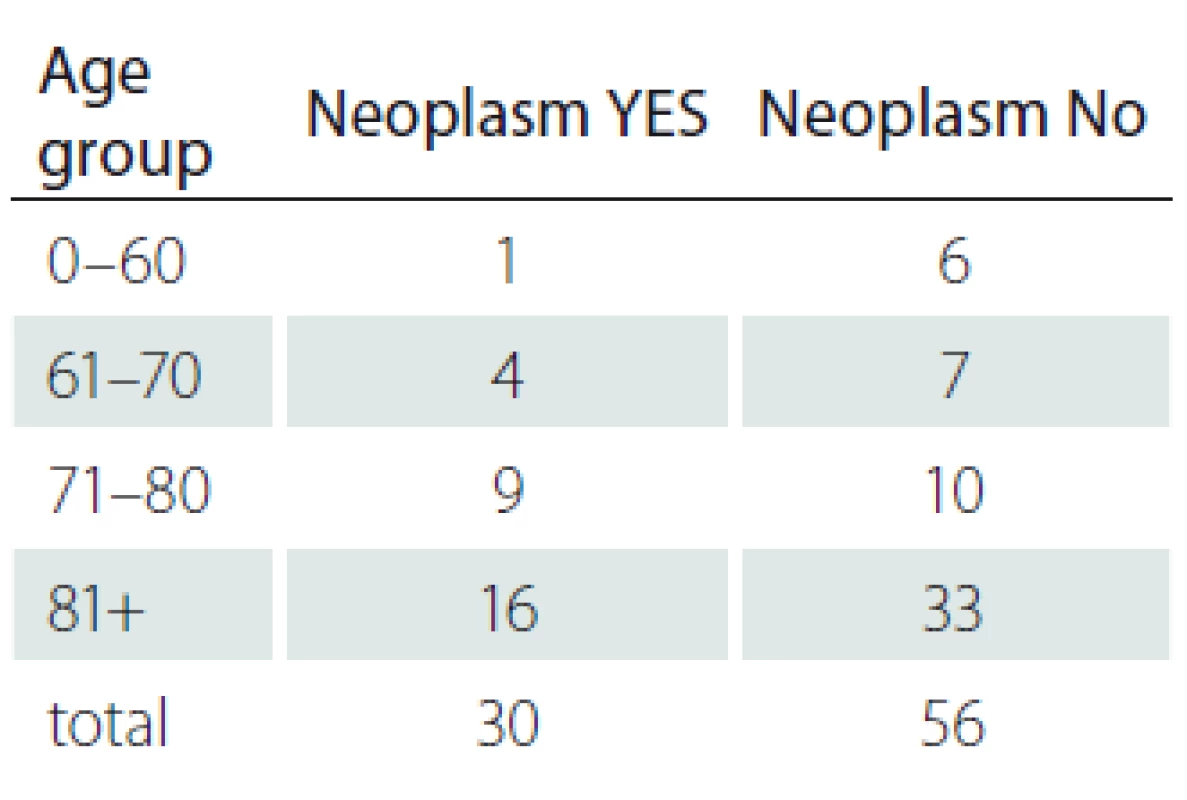
7. Neurological disorder and neoplasm. 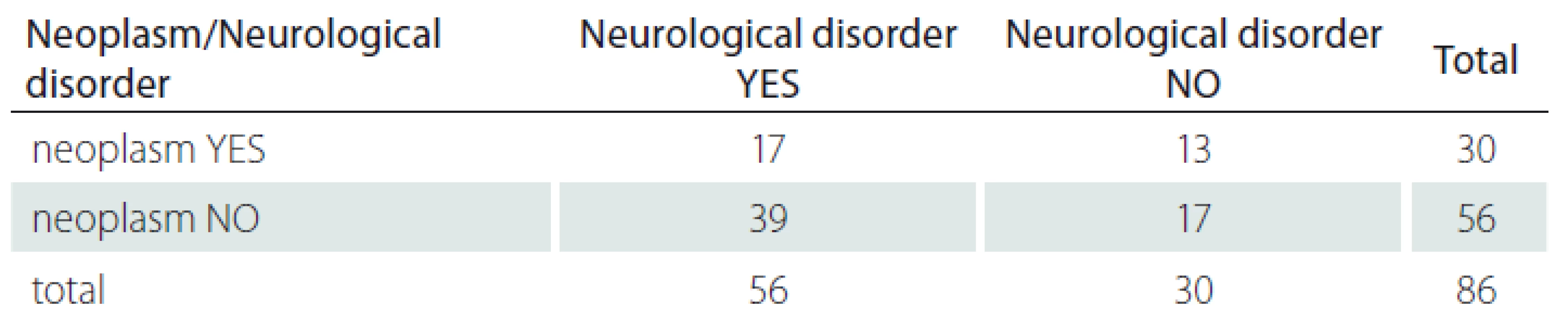
6. Neurological disorder and neoplasm.
Obr. 6. Počet pacientů s dekubity s neurologickým onemocněním a výskytu nádorů.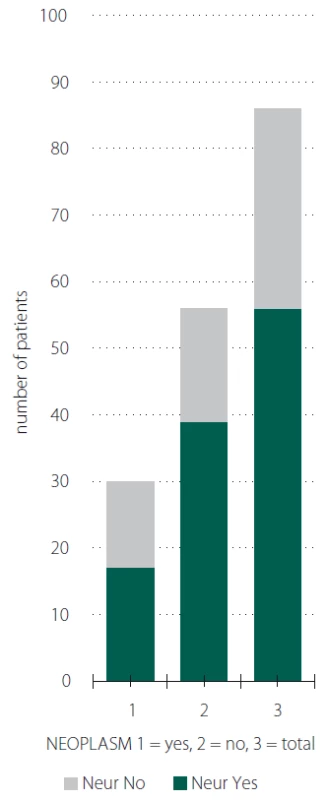
The American Society of Anesthesiologists (ASA) developed the physical status classification system for a simple categorization of a patient’s physiological status when assessing risk. In our sample this factor was 3.17. 19 patients (22.09%) with pressure ulcers died. In our sample the patient with a high risk of pressure ulcer is a man aged 71–80+ after surgery with a history of neoplasm followed by a man or woman aged 80+ after trauma surgery. In Tab. 8 below the group of patients most at risk is highlighted in red, it is a total of 13 patients.
8. Risk of pressure ulcer. 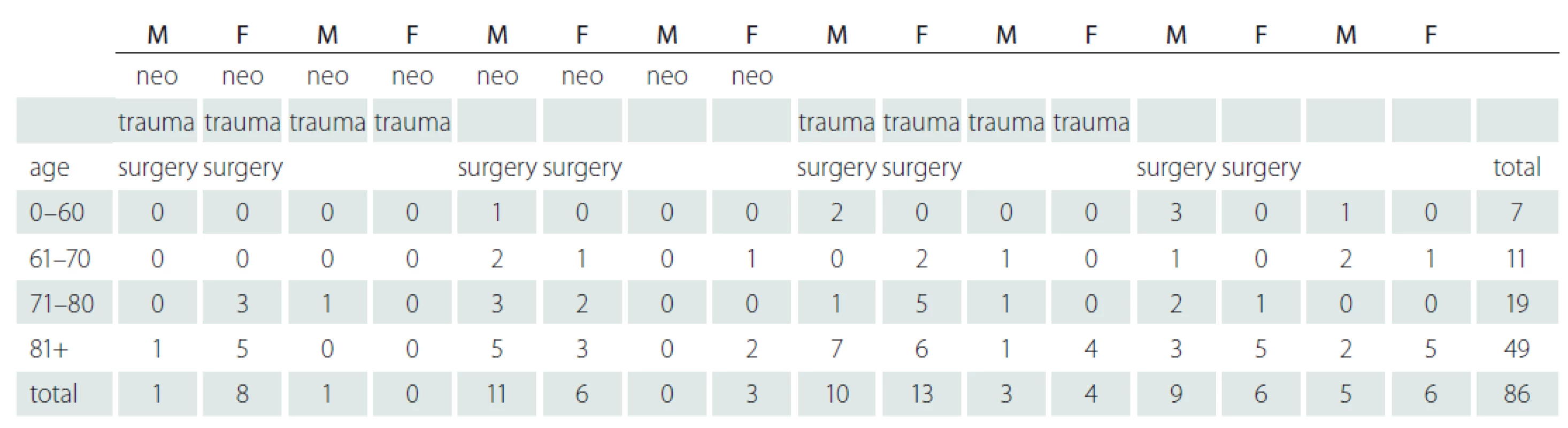
F – female; M – male Discussion
The occurrence of pressure ulcers is increasingly understood as a quality indicator in medical care. In the USA and Europe it has been on the radar of legal professionals and there is a growth in legal actions against healthcare providers. Patients or their families can consider the development of pressure ulcers a failure of the healthcare provider and a threat to patients. When an adequate explanation is not available, patients or their families seek legal action or financial compensation [15]. The worst cases are often reported in the media as proof of a failure in the provision of healthcare, insufficient training or lack of staff are often blamed. Based on media accounts, the public can be under the impression that all pressure ulcers can be prevented.
The incidence rate of pressure ulcers in patients undergoing surgery is variable, for intraoperatively acquired pressure ulcers it ranges from 12 to 66% and the average prevalence rate of pressure ulcers is 3.5–29% [16]. In our study we attempted to identify critical factors that can increase the risk of the occurrence of pressure ulcers on a surgical ward. A surgical patient arrives in a ward for an elective operation or (more often) with an acute problem. The occurrence of pressure ulcers on surgical wards is relatively lower than on other wards [17]. This is due to the spectrum of inpatients and mainly to the short period of hospitalization. In addition nowadays patients live longer and thanks to accessible high quality healthcare they are also undergoing surgeries at a higher age. This increases the risk of complications [18] related to the surgery itself but also due to multiple co-existent conditions as patients’ comorbidity increases enormously with age [19].
In recommendations on the prevention of pressure ulcers the key criteria are a patient’s immobility, nutritional predictors and age. The occurrence of comorbidities in a patient’s history, as well as the ASA risk factors, are not overlooked but normally they are not emphasised as much as the former ones.
In our sample 86 out of a total of 6,419 inpatients (1.46%) developed pressure ulcers in the course of 2 years. The average period of hospitalization was 5.56 days, the surgery occurred on average in 2.79 days since admission (the span was 0–16 days). The time period is identified as a key factor for the development of pressure ulcers, it did not prove so in our sample [6]. We have confirmed the fact that patients live longer and are also undergoing surgery at a higher age, the average age of a patient with pressure ulcers was 79.85 years, they were 17 years older than the average age of all patients treated in our Clinic which is 61.25 years. Fig. 1 shows that there were slightly more women in the sample and that the group at risk is those over 75. It is clear that a patient’s age is a determining factor for the development of pressure ulcers [6]. In our sample another of the main predictive factors proved to be a history of neurological disorder [6,14]. This applied to almost 65% of patients with pressure ulcers in the 2-year period, we believe that this is very significant and we identified this factor as key. Nutritional predictors [20,21] did not prove to be a significant factor for the development of pressure ulcers in our sample. Although Czechs are considered to be an obese nation, the average BMI value was normal in our sample, we only had five malnourished or obese patients in the sample. We also evaluated the risk of developing pressure ulcers by the type of operation [11] but there was no correlation and we also took the history of oncological disease into account [22,23].
Conclusion
We analyzed risk factors for the development of pressure ulcers on a surgical ward during a 2-year period. Our analysis identified patient’s age and a history of neurological disorder as main factors for the development of pressure ulcers. Other factors that are identified as key in literature – such as nutritional predictors – were not statistically significant for our sample. We worked with a small sample of patients which has its limitations and we acknowledge that it is desirable to study larger numbers of patients in order to comply with criteria for evidence-based medicine.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 4. 7. 2019
Accepted for print: 5. 8. 2019
Assoc. Prof. Lenka Veverková, PhD
Ist Surgical Clinic
Medical Faculty of Masaryk University
and St. Anne University Hospital of Brno
Pekařská 53
602 00 Brno
Czech Republic
e-mail: lvever @med.muni.cz
Sources
1. Nixon J, Brown J, McElvenny D et al. Prognostic factors associated with pressure sore development in the immediate post-operative period. Int J Nurs Stud 2000; 37(4): 279–289. doi: 10.1016/ S0020-7489(99)00059-0.
2. Vonlanthen R, Slankamenac K, Breitenstein S et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1,200 patients. Ann Surg 2011; 254(6): 907–913. doi: 10.1097/ SLA.0b013e31821d4a43.
3. Archer S, Pinto A, Vuik S et al. Surgery, complications, and quality of life: a longitudinal cohort study exploring the role of psychosocial factors. Ann Surg 2019; 270(1): 95–101. doi: 10.1097/ SLA.0000000000002745.
4. Pinto A, Faiz O, Davis R et al. Surgical complications and their impact on patients’ psychosocial well-being: a systematic review and meta-analysis. BMJ Open 2016; 6(2): e007224. doi: 10.1136/ bmjopen-2014 - 007224.
5. Padula WV, Mishra MK, Makic MB et al. Improving the quality of pressure ulcer care with prevention: a cost-effectiveness analysis. Med Care 2011; 49(4): 385–392. doi: 10.1097/ MLR.0b013e31820292b3.
6. Coleman S, Gorecki C, Nelson EA et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud 2013; 50(7): 974–1003. doi: 10.1016/ j.ijnurstu.2012.11.019.
7. Moda Vitoriano Budri A, Moore Z. The relationship between risk factors, risk assessment, and the pathology of pressure ulcer development. Cesk Slov Neurol N 2017; 80/ 113 (Suppl 1): 25–28. doi: 10.14735/ amcsnn2017S25.
8. Boyko TV, Longaker MT, Yang GP. Review of the current management of pressure ulcers. Adv Wound Care (New Rochelle) 2018; 7(2): 57–67. doi: 10.1089/ wound.2016.0697.
9. Lindgren M, Unosson M, Fredrikson M et al. Immobility – a major risk factor for development of pressure ulcers among adult hospitalized patients: a prospective study. Scan J Caring Sci 2004; 18(1): 57–64. doi: 10.1046/ j.0283-9318.2003.00250.x.
10. Romanelli M, Clark M, Gefen A (eds). Science and practice of pressure ulcer management. London: Springer-Verlag 2018.
11. Lumbley JL, Ali SA, Tchokouani LS. Retrospective review of predisposing factors for intraoperative pressure ulcer development. J Clin Anesth 2014; 26(5): 368–374. doi: 10.1016/ j.jclinane.2014.01.012.
12. Aronovitch AS. Intraoperatively acquired pres-sure ulcer prevalence: a national study. J Wound OstomyContinence Nurs 1999; 26(3): 130–136. doi: 10.13140/ RG.2.1.4253.5765.
13. Allman RM, Goode PS, Patrick MM et al. Pressure ulcer risk factors among hospitalized patients with activity limitation. JAMA 1995; 273(11): 865–870. doi: 10.1001/ jama.1995.03520350047027.
14. Perneger TV, Rae AC, Gaspoz JM et al. Screening for pressure ulcer risk in an acute care hospital: development of a brief bedside scale. J Clin Epidemiol 2002; 55(5): 498–504. doi: 10.1016/ S0895-4356(01)00514-5.
15. Lockhart DG. The legal implications of pressure ulcers in acute care. Critical Care Nursing Quarterly 2002; 25(1): 63–68.
16. Primiano M, Friend M, McClure C et al. Pressure ulcer prevalence and risk factors during prolonged surgical procedures. AORN J 2011; 94(6): 555–566. doi: 10.1016/ j.aorn.2011.03.014.
17. Lahmann NA, Kottner J, Dassen T et al. Higher pressure ulcer risk on intensive care? Comparison between general wards and intensive care units. J Clin Nurs 2012; 21(3–4): 354–361. doi: 10.1111/ j.1365-2702.2010.03550.x.
18. Sukharamwala P, Thoens J, Szuchmacher M et al. Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HPB (Oxford) 2012; 14(10): 649–657. doi: 10.1111/ j.1477-2574.2012.00506.x.
19. Divo MJ, Martinez CH, Mannino DM. Ageing and the epidemiology of multimorbidity. Eur Respir J 2014; 44(4): 1055–1068. doi: 10.1183/ 09031936.00059814.
20. Kennedy S, Batchelor-Murphy M, Yap T. Clinical insights: understanding the link between nutrition and pressure ulcer prevention. Geriatr Nurs 2015; 36(6): 477–481. doi: 10.1016/ j.gerinurse.2015.10.007.
21. Siang Choo T, Hayter M, Watson R. The effectiveness of nutritional intervention(s) and the treatment of pressure ulcers – a systematic literature review. Int J Nurs Pract 2013; 19 (Suppl 1): 19–27. doi: 10.1111/ ijn.12019.
22. Veverkova L, Krejsova K, Reska M et al. Pressure ulcers represents a constant nightmare for me. Cesk Slov Neurol N 2017; 80/ 113 (Suppl 1): 61–64. doi: 10.14735/ amcsnn2017S61.
23. Sternal D, Wilczyński K, Szewieczek J. Pressure ulcers in palliative ward patients: hyponatremia and low blood pressure as indicators of risk. Clin Interv Ageing 2017; 12 : 37–44. doi: 10.2147/ CIA.S122464.
Labels
Paediatric neurology Neurosurgery Neurology
Article was published inCzech and Slovak Neurology and Neurosurgery

2019 Issue Supplementum 1-
All articles in this issue
- The knowledge and practises of nurses in the prevention of medical devices related injuries in intensive care – questionnaire survey
- Effectiveness of comprehensive pain management in hard-to heal ulcers – a protocol of systematic review
- Negative wound pressure therapy in treatment of a pressure ulcer in paraplegics
- The use of negative pressure wound therapy for wound complication management after vascular procedures
- Mapping of pressure ulcers and non-healing wounds in medical curriculum
- Quality of life in patient with non-healing wounds
- Pain assessment of surgical wounds after angio-surgical interventions
- Effectiveness of hyperbaric oxygen therapy in non-healing ulcerations – meta-review
- Hyperbaric oxygen therapy in non-healing ulcerations – mechanisms of action, current european recommendations and case report
- Reconstruction of recurrent ischiadic pressure ulcer using turnover hamstring muscle flap
- Oxidative stress in wound healing – current knowledge
- Multidisciplinary approach in surgical pressure ulcer therapy after spinal cord injury
- Key factors for the development of pressure ulcers in surgical practice
- Pilot analysis of pressure ulcers – nationwide data from central adverse event reporting system
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Quality of life in patient with non-healing wounds
- The knowledge and practises of nurses in the prevention of medical devices related injuries in intensive care – questionnaire survey
- The use of negative pressure wound therapy for wound complication management after vascular procedures
- Negative wound pressure therapy in treatment of a pressure ulcer in paraplegics
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career