-
Medical journals
- Career
TRIDIMENSIONAL DOPPLER ASSESSMENT: A RELIABLE, NON-INVASIVE AND COST-EFFECTIVE METHOD FOR PREOPERATIVE PERFORATOR ASSESSMENT IN DIEP FLAP
Authors: L. Dražan 1; Lombardo G. A.g 2
Authors‘ workplace: Clinic of Plastic and Aesthetic Surgery, St. Anne’s University Brno, Czech Republic 1; Breast Unit, Cannizzaro Hospital, Catania, Italy 2
Published in: ACTA CHIRURGIAE PLASTICAE, 58, 2, 2016, pp. 60-63
INTRODUCTION
The deep inferior epigastric artery perforator (DIEAp) flap has become an increasingly popular choice since its introduction in 1989 1 and its use for breast reconstruction.2 It is one of the most commonly used perforator flaps for breast reconstruction, becoming the gold standard in few decades. The preoperative perforator mapping is an important step in autologous breast reconstruction, making the flap raising safer, more predictable and time-saving. In these past years, several advanced diagnostic tools have become available, such as Magnetic Resonance Imaging, Computed Tomography Angiography, Digital Subtraction Angiography and Colour Doppler Sonography (Duplex).3
These techniques have proven to be accurate in detecting perforator vessels. They are however time consuming, they cannot be performed during operation and most of these techniques are invasive and expensive. Contrariwise, the hand held Doppler (HHD) examination, despite being a less modern device, is practical, hand portable, inexpensive, easy to perform and to interpret.9
However there are some limitations with HHD. The sensitivity may actually be too high (false positives), as vessels can be overlooked or, vice versa, they can be missed because of the background noise from larger vessels in the proximity 5.
The literature is poor in reports concerning how to technically perform a Doppler exam, especially for the preoperative study of the DIEAp flap. The authors have used this simple device for 15 years in preoperative mapping of the perforators in breast reconstruction. The aim of this paper is to share some advices on how to perform a Doppler exam in preoperative evaluation of a DIEAp flap, increasing its reliability in location of the perforators.
MATERIALS AND METHOD
A Huntleigh Dopplex D900 (Cardiff, UK) with a 5 MHz – 8 MHz – 10 MHz probe and an ultrasound transmission gel were used. The choice of the Doppler probe is based on the thickness of the periumbilical skin evaluated preoperatively by a calliper. Based on our experience the 10 MHz probe is optimal for very thin patients (skin thickness < 3.5 cm), the 8 MHz probe was used for normal weight patients (skin thickness 3.5–5.5 cm) while the 5 MHz Probe’s signal runs deeper when the panniculus adiposus is thicker (skin thickness > 5.5 cm). The study was carried-out preoperatively in 26 consecutive patients for a total of 52 semi-abdomens. All the preoperative measurements were performed by a single surgeon (L.D.)
The detection method to map the perforators preoperatively is a four-step process and it is summarized in Fig. 1. All of the preoperative perforators detected were marked on the skin with a marker pen. The flap was then dissected in the usual manner identifying the suitable perforators. The penetration point of a perforating vessel through the fascia was then projected onto the surface of the skin and marked.
Fig. 1. The preoperative Mapping Method. Each sound signal was marked on the skin in all of the four steps. We incline the probe slightly (≈ 75°). The location with the higher density of marked dots was assigned as the perforator. By this way a preoperative map was created 
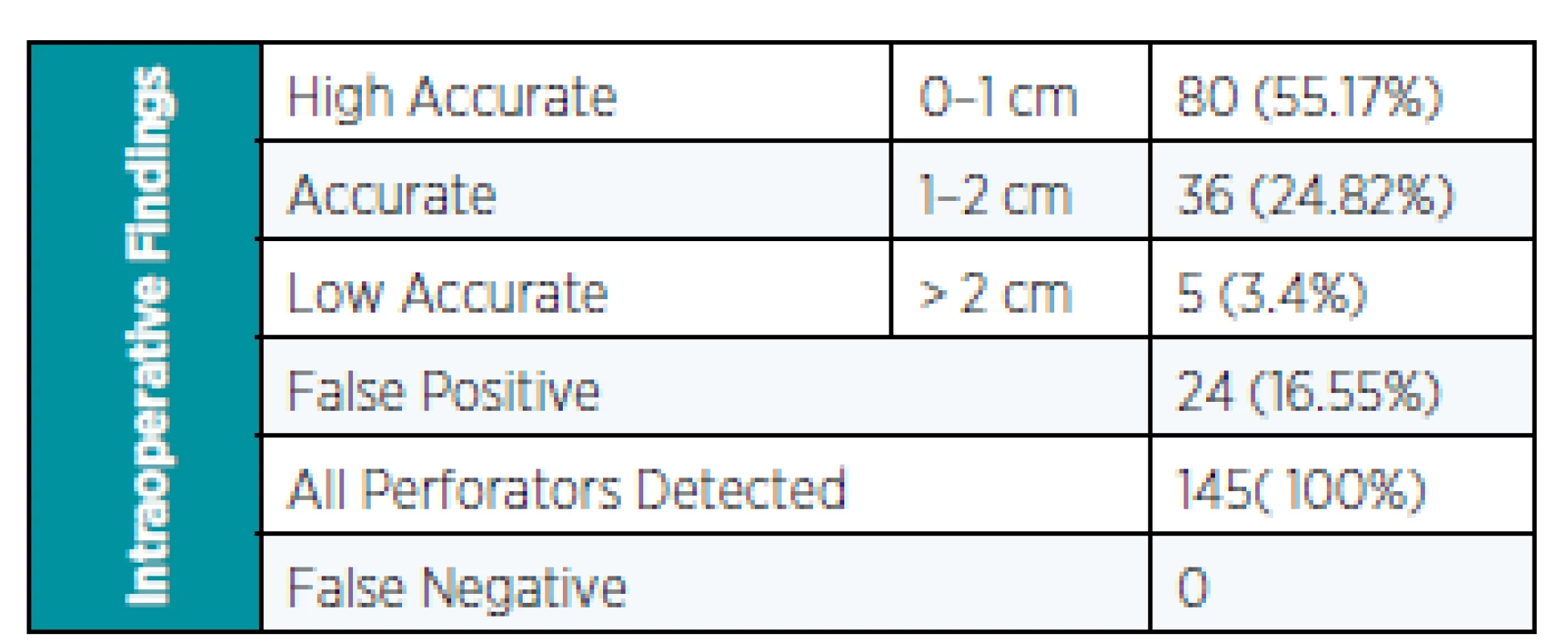
For the evaluation of the matching between Doppler Dot and the operative finding was used a Cartesian coordinate system. We compared Preoperative and Postoperative map measuring the distance in cm and using the umbilicus as the origin of the coordinate system, marked as “0” point. We divided the results in three categories as high accurate (0–1 cm), accurate (1–2 cm) and low accurate (>2 cm).
RESULTS
The results are summarized in Table 1. We have marked preoperatively 145 perforators, in 26 patients for a total of 52 semi-abdomens. An average of 5.6 vessels per patient were marked. Of these, 80 (55.17%) were found between 0–1 cm, 36 (24.82%) between 1–2 cm and 5 (3.4%) of these more than 2 cm from each other. We had 24 (16.55%) false positives in which there was no correspondence between the signal and the intraoperative finding. All of the dissected perforators were detected preoperatively so we did not have false negatives in our series.
DISCUSSION
Although the Doppler exam has proven to be less accurate in locating perforators compared with colour duplex sonography 1,3 and computed tomography angiography 4–7, it will probably remain of importance in clinical practice. This is because the device is portable and the examination inexpensive, not invasive and relatively easy to perform and to interpret.
Klasson et al. found in a recent randomized prospective study that there is no significant difference in surgery time and complication rate when Doppler exam is used for preoperative mapping of perforators in comparison with CTA.8
Although the device is widely available, only few papers are present in literature on how to perform a Doppler exam in preoperative evaluation of DIEAp surgery.4,9 They advise to direct it perpendicularly to each perforator being assessed.
The criticism to perform the Doppler exam in this manner is that a tridimensional structure like the skin is commutated in a flat geometric figure like a square. The single direction probe application can be valid only in few cases, where the vessel is exactly perpendicular to the surface of the skin, but in many cases the direction of the vessel is not straight. So if we put the probe in a single direction, there is a high chance to get a signal (high sensibility), but it is possible that the signal is picked up by a vessel without a perpendicular course.
For this reason, during the dissection there will be no correspondence with the dot marked preoperatively and the point where the vessel perforates the fascia (false positive). With our method we create a dense tridimensional network of signals with different angles (Fig. 2). In this manner if we detect the perforator in more than one direction, the possibility of matching the perforator location during intraoperative assessment is higher (false positives).
Fig. 2. The tridimensional network of Doppler signals. The tridimensional network of signals crossing the skin is simply explained. We create a dense web of signals with different angles. We know from geometry that a unique straight line passes through two distinct points. This simple axiom could explain the downfall of the false positives in our series (The figures are of our own creation) 
For this reason we could explain the downfall of the false positives in our series (16.16%) compared with Giunta’s et al. report, where there was a high percentage of false positives (48.4%). 9 Blondeel et al. also quit the preoperative Doppler exam converting to the colour Duplex scanning because of a high number of false positives. 10
Besides, in our series there were no false negatives found; this is clinically commutated in less risk to injure accidentally the perforator for a failure in preoperatively identification.
The group 0–1 cm was the most represented with 80 cases (55.17 %) while the 1–2 cm was found in 36 cases (24.82%). Clinically these classes could be linked in a unique class because the take-home preoperative finding is that we must dissect slowly in proximity of the dot.
Based on our results, the preoperative Doppler exam gives us basic information about the location of the perforators allowing us to perform a safer, more predictable and time-saving dissection.
Although the Doppler exam may not provide the same anatomic details as the other newer modalities, such as CTA and MRA, the HHD remains a very useful and important tool for autologous reconstruction. We recommend performing this exam as a standardized and reproducible method to improve reliability.
Declaration of interest: The authors report no conflict of interest. The authors alone are responsible for the content and writing of this article.
Corresponding author:
Lombardo Giuseppe A.G.
Cannizzaro Hospital
Via Messina 829 Catania IT 95129
Italy
E-mail: giuseppelombardouni@gmail.com
Sources
1. Koshima I, Soeda S. Inferior epigastric artery skin flap without rectus abdominis muscle. Br J Plast Surg. 1989;42(6):645–8.
2. Allen, RJ, Treece, P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32 : 32.
3. Smit JM, Klein S, Werker PM. An overview of methods for vascular mapping in the planning of free flaps. J Plast Reconstr Aesthet Surg. 2010;63:e674–82.
4. Nahabedian M, Patel K. Maximizing the use of the handheld Doppler in autologous breast reconstruction. Clinics in Plastic Surgery 2011;38 : 213–8.
5. Hallock G. Acoustic Doppler Sonography, Color Duplex Ultrasound, and Laser Doppler Flowmetry as tools for successful autologous breast reconstruction. Clinics in Plastic Surgery 2011;38 : 203–11.
6. Masia J, Clavero JA, Larranaga JR et al. Multidetector-row computed tomography in the planning of abdominal perforator flaps. J Plast Reconstr Aesthet Surg. 2006;59 : 594e9
7. Alonso-Burgos A, Garcia-Tutor E, Bastarrika G et al. Preoperative planning of deep inferior epigastric artery perforator flap reconstruction with multislice-CT angiography: imaging findings and initial experience. J Plast Reconstr Aesthet Surg. 2006;59 : 585e93.
8. Klasson S, Svensson H, Malm K, Wassélius J, Velander P. Preoperative CT angiography versus Doppler ultrasound mapping of abdominal perforator in DIEP breast reconstructions: A randomized prospective study. J. Plast. Reconstr. Aesthet. Surg. 2015. doi:10.1016/j.bjps.2015.02.002
9. Giunta RE, Geisweid A, Feller AM. The value of preoperative Doppler sonography for planning free perforator flaps. Plast Reconstr Surg. 2000;105 : 2381e6.
10. Blondeel P et al. Doppler flowmetry in the planning of perforator flaps. Br J Plast Surg. 1998;51,202–9.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2016 Issue 2-
All articles in this issue
- Editorial
- TRIDIMENSIONAL DOPPLER ASSESSMENT: A RELIABLE, NON-INVASIVE AND COST-EFFECTIVE METHOD FOR PREOPERATIVE PERFORATOR ASSESSMENT IN DIEP FLAP
- OUR PRELIMINARY EXPERIENCE WITH A NEW METHOD OF DIEAp FLAP DISSECTION
- Lipomodelling – advanced technique for the correction of Congenital hypoplastic breast malformations and deformities
- Reconstruction of large facial and orbital defects by combining free flap transfer with craniofacial prosthesis
- UPPER EYELID INJURY WITH PARTIAL LOSS. CASE REPORT
-
ISAPS Visiting Professor Program
Hluboká nad Vltavou, Czech Republic
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Lipomodelling – advanced technique for the correction of Congenital hypoplastic breast malformations and deformities
- Reconstruction of large facial and orbital defects by combining free flap transfer with craniofacial prosthesis
- TRIDIMENSIONAL DOPPLER ASSESSMENT: A RELIABLE, NON-INVASIVE AND COST-EFFECTIVE METHOD FOR PREOPERATIVE PERFORATOR ASSESSMENT IN DIEP FLAP
- UPPER EYELID INJURY WITH PARTIAL LOSS. CASE REPORT
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career