-
Medical journals
- Career
Axillary artery injury in low-energy shoulder injury
Authors: Zuzana Mannová; Martin Křivohlávek; Jaroslav Šrám
Authors‘ workplace: Traumatologicko-ortopedické centrum, Krajská nemocnice Liberec a. s.
Published in: Úraz chir. 27., 2020, č.2
Overview
In the presented case reports, the author describes a rare complication in the dislocation and fracture of the proximal humerus. Both with the occurrence of a low-energy injury (simple fall). In the subsequent discussion, he deals with possible aetiology and mechanisms of a. axillaris injuries and its therapies.
Keywords:
Injury/lesion of a. axillaris – fracture of proximal humerus – shoulder dislocation
Introduction
Injuries of the proximal humerus are a typical injury of elderly patients. High-energy injuries are typically accompanied by vascular injuries. We must not forget that even a low-energy mechanism of injury can lead to vascular complications.
Dislocation of humerus accounts for up to 80 % of all dislocations. Anterior dislocation is the most common one, making up 90–95% [11]. Cumulative incidence (up to 70 years of age) of acute shoulder joint dislocation in the population is around 0.7 % in men and around 0.3 % in women [17].
Proximal humeral fractures represent 4–5 % of all fractures [13]. 75 % of these patients are women whose incidence is significantly higher and rises sharply with age over 60 [5]. The average age at the time of injury is 67 years [1].
Limb vascular traumas account for up to 80 % of all vascular injuries [19]. Lesions of the armpit artery account for about 6 % of all arterial injuries [18]. Incidence of injury of a. axillaris is approximately 5 % for proximal humerus fractures and 1–2 % for shoulder joint luxuries [2, 7].
Possible associated complications are nerve damage resulting from the anatomical course of the artery and nerves mentioned below. In the case of low-energy injuries, it is usually a reversible damage of the so-called neurapraxia without interrupting the continuity of the nerve from pressure or bruising.
Neurovascular complications are more frequent after high-energy injuries in younger patients, in low-energy injuries, the incidence of these complications is rarer and occurs in elderly patients [6, 12].
Incidence of an injury of a. axillaris (0.09 %) in fr. proximal humerus is less frequent than the injury of brachial plexus (0.14 %), i.e. A complicating neural injury is more frequent than a vascular one [14].
Factors associated with a higher risk of injury of a. axillaris with the fracture of proximal humerus include the male sex, atherosclerosis, open fracture, and the presence of concomitant injuries such as shoulder dislocation or brachial plexus injury [14].
Arteria axillaris is a continuation of a. subclavia from the outer edge of the 1st rib through the axilla to the inside of the collum chirurgicum humeri (to the lower edge of the m. pectoralis major tendril). According to the course, the artery is divided into three sections – medial from m. pectoralis minor, for m. pectoralis minor and from the outside from m. pectoralis minor, where there is a nerve fork in front of the artery, from which the n. medianus connects. Plexus brachialis runs in parallel with the artery, at first dorsocranially, gradually laying its bundles to the artery [4]. Distal section of a. axillaris, which lies externally from m. pectoralis minor (not sufficiently covered), is affected most frequently, in more than 90 % [16].
Case report 1
74-year old female patient, was brought in by the rescue service after falling from a ladder while hanging curtains, with pain in her right arm. At first sight a clear defiguration of the shoulder with a palpable empty hole of the shoulder joint. Another serious symptom was numbness from the elbow up to the periphery and restriction of active movement with vaguely palpable pulsation. Due to clear clinical signs of shoulder dislocation and neurological deficiency, an urgent reduction according to Arlt was performed. On the subsequent X-ray scan, the head of the humerus is reinserted (Fig. 1). It was the first dislocation, without glenoid fracture (Fig. 2). Immediately after the reduction, the neurological deficit subsided, sensitivity and movement were restored, paresthesia persisted temporarily (tingling in the fingers). The patient was relieved and pains subdued. However, when checking the periphery, there was a poorly palpable pulse on a. radialis, slightly cooler fingers, and a slowed capillary return. Therefore, duplex ultrasonography of the right upper limb was performed with the conclusion: flows in a. brachialis were undifferentiated. Subsequently, an SCT angiography examination was performed with the finding of a. axillaris and a. brachialis on the right, in the axilla with a noticeable blunt stump of the artery, further on, only fine collaterals are filled. Truncus brachiocephalicus and a. subclavia are free (Fig. 3).
1. Humeral head is in glenoid cavity after reduction 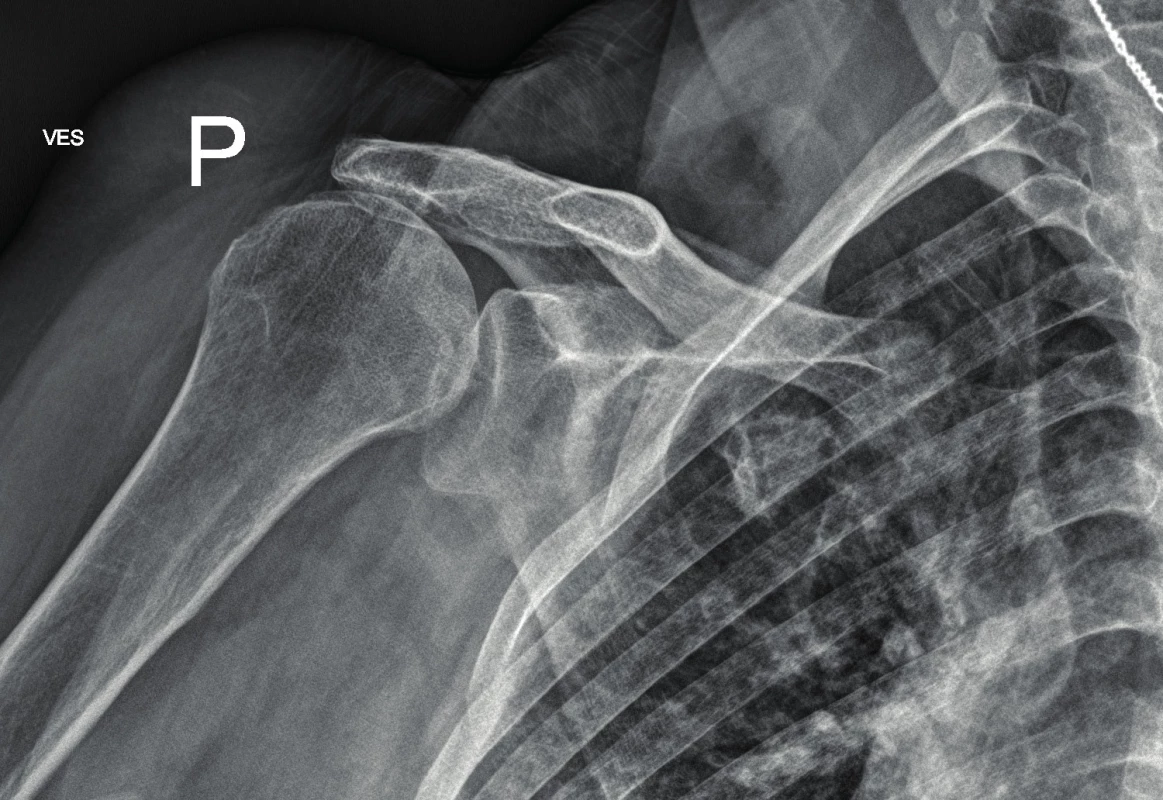
2. Without glenoid fracture on CT imaging 
3. SCT angiography procedure finds closure of right axillary and brachial artery 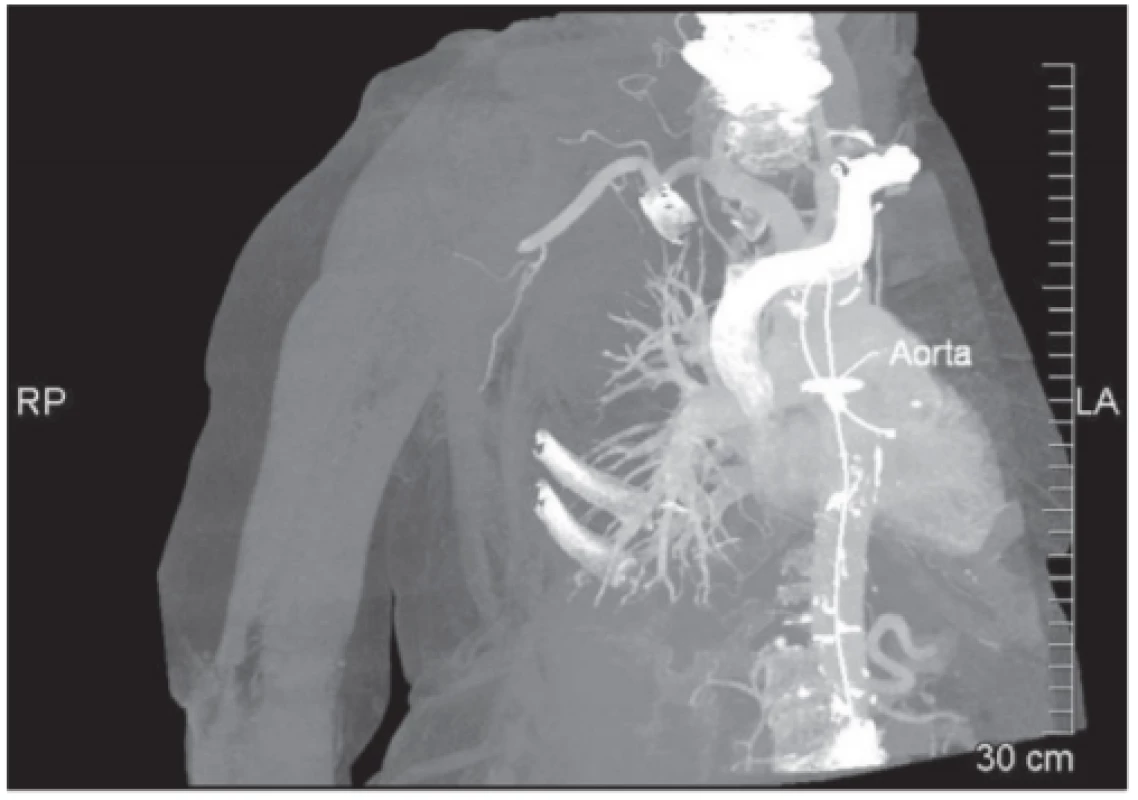
Heparin 10 was administered still in the ambulance. The patient was admitted to hospital and prepared for surgery. We expected a lesion of intima with an onsetting thrombus, so the plan was to perform a thrombectomy in the operating room with the introduction of a stent. An alternative to this procedure was to perform the bypass surgery. The patient did not have significant comorbidities in her medical history affecting the course of injury or treatment. In the operating room, an attempt for thrombectomy was performed first under local anesthesia from a cut in cubita; however, the catheter was introduced only up to 25 cm, it was impossible to proceed further centrally. We were not able to introduce the catheter over the site of the suspected injury. After an unsuccessful thrombectomy, we proceeded to convert to an open reduction under general anesthesia. A cut was made high in the axilla with a revision of the brachial plexus, vein and axillary artery, which was pathologically wound (kinking) and lacerated with acute arterial closure. Therefore, venous axillo-axillary bypass with graft from v. cephalica was performed. After the operation, the patient was observed in the ICU and administered Agapurin in continuous infusion for 24 hours. The total hospitalization was 6 days. The postoperative period was without complications, with an early subsiding of pain. Clexane was administered as a prophylaxis, and Anopyrin was administered as a prevention of bypass closure (Anopyrin is indicated to be taken permanently). The patient was given a shoulder brace and she was able to perform exercises from the elbow to the periphery. After a month, the patient wore a brace only for the night and began exercising her shoulder in terms of an intensive outpatient rehabilitation. After 2 months, the patient was able to elevate the shoulder up to 160 degrees; she had fully functional peripheries l and subjectively was completely untroubled; the wounds healed per primam intention. Arthrotic changes were visible on the X-ray scans and the higher position of the head persisted. As a sign of damage to the rotator cuff without the need for further solution, due to the age and good range of movements of the patient‘s shoulder (Fig. 4). Vascular surgeon‘s check-ups after bypass surgery took place in 1 month, 3 months, and in 1 year with duplex USG examination without pathology.
4. Arthrosis and cranial translation of humeral head on X-ray image 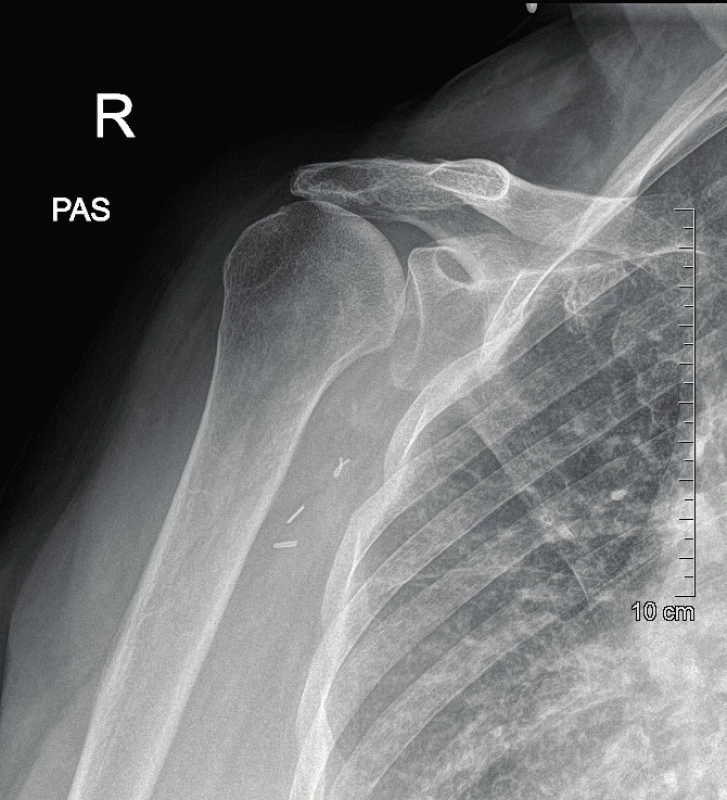
Case report 2
74-year old female patient, was pulled to the ground by a dog and subsequently brought in by the rescue service. On the X-ray scan there was a comminuted fracture of the greater tuberosity with dislocation of the left shoulder. During the reduction in sedation, there was an iatrogenic injury with the occurrence of fracture of proximal humeral metaphysis (Fig. 5). The patient was hospitalized and made ready for the surgery that was performed on the following day. We performed an open reduction from the deltoideopectoral approach, and then splint osteosynthesis (Philos); the procedure took place without complications. During the first postoperative day, a progressing disorder of the finger movement and sensitivity of the left upper limb developed. During the clinical examination, there were no palpable pulsations in the periphery; a CT-angio (graphy) examination was therefore subsequently performed with the finding of a closure on the interface of a. subclavia and a. axillaris (Fig. 6). Based on agreement with the vascular surgeon and intervention radiologist, percutaneous transluminal angioplasty was performed by the way of joint femoral artery on the right with administration of 2,000u of Heparin i.a. with successful recanalization (Fig. 7, 8).
5. Comminutive tuberosity fracture with humeral head dislocation and metaphyseal fracture on X-ray image 
6. CT-angio (graphy) investigation finds closure of interface between subclavian artery and axillary artery 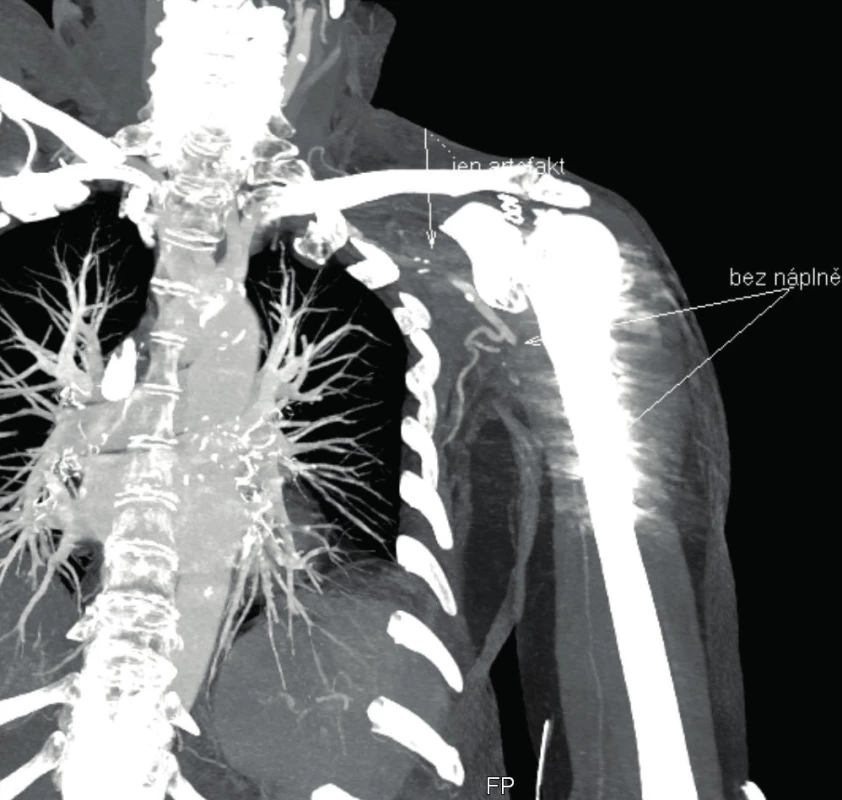
7. PTA of axillary artery closure with recanalization via common femoral artery 
8. PTA of axillary artery closure with recanalization via common femoral artery 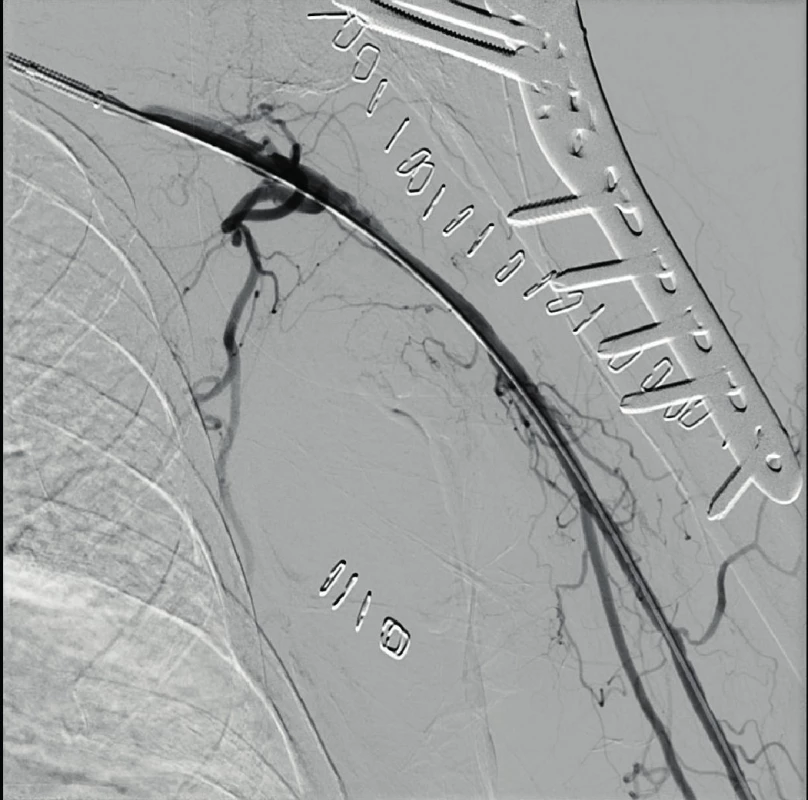
Clexane was administered in a therapeutic dose. Then the difficulties subsided. For the next three days, there were nonpalpable pulsations on the limb again. Duplex ultrasonography revealed indirect signs of a closure of a. axillaris; the artery itself was not noticeable for edema in B-mode; more distally, a. brachialis was filled through collaterals. During the clinical examination, the periphery was slightly colder, without neurological deficiency. Based on agreement with a vascular surgeon and an intervention radiologist due to favourable clinical condition, the conservative approach was chosen. Apparently, there was on onsetting thrombosis with the lesion of intima. Due to the functional collateral bloodstream, the patient was informed that the operational solution would only be used in case of difficulties when carrying out normal daily activities. The patient was discharged into home care with a shoulder orthosis, with the recommendation to do exercises from the elbow to the periphery. Acetylsalicylic acid was permanently deployed. The overall hospitalization lasted 21 days due to repeated closure and complications with the development of stress ulcer.
Discussion
That which guides us to suspect vascular injury is particularly the clinical examination. Symptoms are divided into „hard signs“ (active bleeding, limb ischemia, non-palpable pulsation, enlarged or pulsating haematoma) and „soft signs“ (subjectively reduced pulse, non-pulsating haematoma, typical bone or neurological injuries, history of bleeding) [15]. The limb tends to be pale and cold, capillary return may be reduced. The patient experiences pains from severe to unbearable, which persist even after e.g. reduction of dislocation, up to mild paresthesia. Arteries are capable of vasoconstriction, especially those with smaller lumen can completely stop the bleeding and prematurely reassure the attending physician that the injury is not a serious one. One should keep in mind that the presence of peripheral pulsation does not exclude vascular injury yet. In up to 14 %, pulsation is reduced only, and in 11% of patients, peripheral pulsation may be present even in a proven vascular lesion [9]. There is a risk of delayed onset of symptoms of an onsetting thrombosis. The pulse on the limb is palpable provided that the systolic pressure exceeds at least 60 mmHg [15].
In addition to a thorough clinical examination, we will use the Doppler USG imaging techniques, and particularly CT-angio (graphy). CT angiography will allow for early detection of an arterial injury, and in a situation where this examination is available, it can be performed without prior USG examination, thus avoiding unnecessary delay of the final treatment. At the same time, it will help to determine the method of therapy, either in radio-intervention or surgery form.
The undeniable advantage of the low-energy injury is that the patient is conscious and his/her circulation is stable. Therefore, there is no obscuration of clinical symptoms and initial overlooking of the injury. In contrast, in high-energy trauma (polytrauma), a consciousness disorder is often present, the patient is unable to communicate subjective difficulties, and active movement cannot be examined. Performed CT AG (whole body in polytrauma mode) will help to detect a vascular lesion more often, but is not able to diagnose potential nerve injuries.
Injuries of a. axillaris as such can be subdivided from several points of view.
Depending on the extent of damage to the artery wall. It can only affect the outer layer (tangential injury) only, penetrate up to the lumen (puncture), or interrupt it completely (dilation, avulsion).
According to communication with the external environment. These may be open or closed injuries.
According to the direction of injury violence. It can be direct or indirect.
In the indirect mechanism, the artery traction results from dislocation of a joint or major dislocation of a fracture or by unsparing handling during reduction.
Depending on the type of injury. The direct mechanism can be further subdivided into sharp and blunt injuries.
Sharp injuries can be subdivided to perforating or penetrating ones (stabbing, cutting, slash wounds, injuries caused by bone fragment in a dislocated fracture, gunshot) and iatrogenic ones (e.g. Injuries caused by nail or screws during surgery or by catheter during catheterization).
Blunt injuries caused by compression (impact, hit, compression against bone, haematoma, long-term use of armpit crutches). Blunt injuries pose a high risk of overseeing. In most cases, only the inner part of the artery (tunica intima), is damaged, so called. intimal lesion. This causes the closure by self-obstruction or subsequent onsetting thrombosis.
M. pectoralis minor can operate as a support point, the artery is strained by abduction and it is subsequently damaged by cutting forces of the outer rotation of the arm [6, 10].
Condition of the patient‘s vascular system can be a certain predisposition to an arterial injury, e.g. kinking of the artery, where the risk of wrapping of a long vessel and easier injury, or the effect of comorbidities in terms of atherosclerosis or peripheral vascular disease, when reduced elasticity may result in increased vulnerability of the vessel.
In elderly patients, the distal part of a. axillaris is relatively free, which makes it more prone to injury in patients with atherosclerotic changes [12].
Injuries affecting only the outer wall of the artery usually heal spontaneously. They usually do not result in bleeding or interruption of the blood flow; sometimes a later rupture or pseudoaneurysm [8] may occur.
Puncture injury usually also heals spontaneously, but it may result in persisting communication between the artery and the blood sprain and formation of so-called pulsating haematoma, which can become encapsulated, and thus develop an pseudoaneurysm. With simultaneous injury to the accompanying vein, similar mechanism may result in create an arteriovenous fistula [8].
In the open trauma therapy, bleeding needs to be stopped first. This is mostly followed by surgical intervention in the form of a revision of the wound with a mapping of the injury to the blood vessel. Vascular injury with acute ischemia should be reconstructed within 6 – 8 hours from the trauma. If the artery is without tension after the mobilization, it can be stitched end-to-end directly or, in a puncture, with a simple suture. In the event of an extensive injury, suture with venous patch or venous graft bypass is recommended (from v. basilica or cephalica; if it is not possible from the previous ones, it is recommended from v. saphena magna on the leg), or prosthetic replacement (higher risk of infection due to foreign material, rather in high-flow arteries). In blunt traumas, the injury of intima is assumed. The surface becomes highly thrombogenic; therefore it is not possible to perform simple thrombectomy and suture of the artery. It is advisable to perform resection and replacement, or to introduce a stentgraft from endovascular approach. In the event of a fracture with dislocation, we perform reduction and osteosynthesis with the ensuing vascular reconstruction procedure first. If irreversible damage from ischemia due to delay threatens, the reconstruction surgery can be performed prior to osteosynthesis with the risk of damage to anastomosis or development of thrombosis. Or to apply bridging using of a fixed catheter and thereby restore the flow to the tissues for the necessary time.
Anticoagulant therapy with vasodilation therapy is usually recommended after the operation [loosely according to 8, 15]. Pentoxifylline is used for vasodilation therapy in an infusion in a daily dose of 400 mg. For the prevention of periprocedural acute thrombosis, unfractionated heparin is administered during the procedure. For the prevention of early thrombosis after percutaneous transluminal angioplasty, it is recommended to administer heparin for 2 days after the procedure. Mini heparinization (prophylactic heparinization) is recommended. Unfractionated heparin may be administered 2–3 times in a dose of 2500-5000 units subcutaneously or low molecular weight heparin may be administered 1–2 times daily (dosing is based on the patient‘s weight). After implantation of stentgraft into peripheral arteries, it is recommended to administer dual antiplatelet therapy (e.g. ASA 100 mg/d + clopidogrel 75 mg/d) for 1–3 months after the procedure and consider its long-term administration as a prevention of restenoses and reclosures [3]. Acetylsalicylic acid is used to prevent and treat arterial closure also after vascular reconstructions.
Conclusion
At the end of this presentation we would like to point out that vascular complications of low-energy shoulder injury, i.e. fracture of the proximal humerus or humeroscapular dislocations are rare, but all the more serious. It is of crucial importance to conduct an examination of the upper limb periphery, i.e. movement, sensitivity and blood circulation, before and after reduction. Further, to thoroughly educate and check the patient even after a time interval due to the risk of late onset of certain types of vascular injury, particularly lesions of intima with the development of late thrombosis. In the event of suspected vascular lesion, we will perform CT angiography, which will allow us to detect early injury of the artery, while helping to determine the therapeutic method, either in a form of radio intervention, or surgery.
Sources
- BARTONÍČEK, J., DŽUPA, V., FRIČ, V. et al. Epidemiologie a ekonomie zlomenin proximálního femuru, proximálního humeru, distálního radia a luxačních zlomenin hlezna. Rozhledy v chirurgii. Praha : Česká lékařská společnost J.E. Purkyně. 2008, 87, 213–219. ISSN 0035-9351.
- BROWNER, B., JUPITER, J., KRETTEK, C. et al. Skeletal Trauma : Basic Science, Management, and Reconstruction. 6th ed. Amsterdam : Elsevier Health Sciences, 2019. 3032 s. ISBN 978-03-2361-114-5.
- ČERNÁ, M., ROČEK, M., PEREGRIN, JH et al. Doporučení České společnosti intervenční radiologie ČLS JEP pro periprocedurální medikaci u endovaskulárních výkonů. Česká radiologie [online]. Praha : Česká lékařská společnost J. E. Purkyně. 2018, 2, 71–75 [cit. 26.02.2020]. ISSN 1210-7883. Dostupné z: http://www.cesradiol.cz/vydanacisla.php
- ČIHÁK, R., DRUGA, R., GRIM, M. Anatomie 3: Druhé, upravené a doplněné vydání. 2. vyd. Praha : Grada, 2004. s. 10 ISBN 80-247-1132-X.
- EDELMANN, K., DVOŘÁK, J., KOPP, L. et al. Fraktura proximálního humeru komplikovaná lézí arteria axillaris - kazuistika. Rozhledy v chirurgii. Praha : Česká lékařská společnost J.E. Purkyně, 2010, 9, 473–476. ISSN 0035-9351.
- EDELMANN, K., HOUSER, J., ŠTĚPÁNOVÁ, E. et al. Přední luxace humeru komplikovaná trombózou arteria axillaris – kazuistika. Rozhledy v chirurgii. Praha : Česká lékařská společnost J. E. Purkyně. 2007, 11, 611–613. ISSN 0035-9351.
- EYLER, Y., Yilmaz, T., Turgut, A. et al. Axillary artery laceration after anterior shoulder dislocation reduction. Turkish Journal of Emergency Medicine [online]. Amsterdam : Elsevier B. V., 2019, 19, 87–89 [cit. 27.02.2020]. ISSN 2452-2473. Dostupné z: http://www.sciencedirect.com/science/article/pii/S2452247318302607
- FIRT, P., HEJNAL, J., VANĚK, I. Cévní chirurgie. 2. vyd. Praha: Karolinum, 2006, 323 s. ISBN 80-246-1251-8.
- HOFMAN, M., GROMMES, J., KROMBACH, GA. et al. Vascular Injury Accompanying Displaced Proximal Humeral Fractures: Two Cases and a Review of the Literature. Emergency Medicine International [online]. London : Hindawi, 2011, [cit. 26.02.2020]. ISSN: 2090–2840 Dostupné z: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3200234/
- CHEHATA, A., MORGAN, FH., BONATO, L. Axillary artery injury after an anterior shoulder fracture dislocation and „periosteal sleeve avulsion of the rotator cuff“ (SARC). Case report and review of the literature. Trauma Case Reports [online]. Oxford : Elsevier Ltd., 2017, 8, 5–10, [cit. 27.02.2020]. ISSN 2352-6440. Dostupné z: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5883186/
- KŘIVOHLÁVEK, M. Poranění ramenního kloubu. In: WENDSCHE, P., VESELÝ, R. Traumatologie. Praha : Galén, 2015, 344 s. ISBN 978-80-7492-211-4.
- KŘIVOHLÁVEK, M. Operační léčba tří a čtyřúlomkových zlomenin proximálního humeru [online]. Olomouc, 2013. Dizertační práce. Univerzita Palackého v Olomouci, Lékařská fakulta. [cit. 20.09.2019]. Dostupné z: https://theses.cz/id/gsefus/
- KŘIVOHLÁVEK, M., LUKÁŠ, R., TALLER, S., ŠRÁM, J. Použití úhlově stabilních implantátů při ošetření zlomenin proximálního humeru - prospektivní studie. Acta chirurgiae orthopaedicae et traumatologiae čechoslovaca. Praha : Galén, 2008, 75, 212–220. ISSN 0001-5415.
- MENENDEZ, ME, Ring, D., Heng, M. Proximal humerus fracture with injury to the axillary artery: A population-based study. Injury. Amsterdam : Elsevier BV., 2015, 46, 1367–1371. ISSN 0020-1383.
- MOLÁČEK, J., TŘEŠKA, V., BAXA, J.et al. Poranění cévního systému. Plzeň : Nava, 2016, 136 s. ISBN 978-80-7211-491-7.
- MOUZOPOULOS, G., LASSANIANOS, N., MOUZOPOULOS, D. et al. Axillary artery injury associated with proximal humerus fractures. Vasa. Bern : Hogrefe A.G., 2008, 37, 274–277. ISSN 0301-1526.
- NEORAL, P. Analýza důvodů selhání stabilizačních výkonů u ramenního kloubu [online]. Olomouc, 2014. Dizertační práce. Univerzita Palackého v Olomouci, Lékařská fakulta. [cit. 28.09.2019]. Dostupné z: https://theses.cz/id/74skgf/
- ROCKWOOD, CA. et al. The shoulder. 3rd ed. Philadelphia : Saunders, 2004, 653 p. ISBN 0-7216-0148-0.
- RUTHERFORD, RB. Vascular surgery (Volume 2). 6th ed..Philadelphia : Elsevier Saunders, 2005, 2736 p. ISBN 978-99-9762-676-9.
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2020 Issue 2
Most read in this issue- Supracondylar Fractures of Distal Humerus in Children – Results of Operative Treatment
- Splint rib osteosynthesis: our experience
- Axillary artery injury in low-energy shoulder injury
- Nekrolog Doc. MUDr. František Vyhnánek, CSc.
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

