-
Medical journals
- Career
Acute elevation of intraocular pressure in patient with hyperlipidemic myeloma
Authors: O. Dušek 1; M. Fichtl 1; L. Rezková 1; Z. Dubská 1; prof. MUDr. Jarmila Heissigerová, Ph.D., MBA 1; E. Růžičková 1; M. Vráblík 2; I. Špička 3; P. Svozílková 1
Authors‘ workplace: Oční klinika, 1. lékařská fakulta, Univerzita Karlova a Všeobecná fakultní nemocnice v Praze, Česká republika, U nemocnice 499/2, 128 08, Praha 2. 1; III. interní klinika, 1. lékařská fakulta, Univerzita Karlova a Všeobecná fakultní nemocnice v Praze, Česká republika, Česká republika, U nemocnice 2094/1, 128 08, Praha 2. 2; I. interní klinika, 1. lékařská fakulta, Univerzita Karlova a Všeobecná fakultní nemocnice v Praze, Česká republika, U nemocnice 499/2, 128 08, Praha 2. 3
Published in: Čes. a slov. Oftal., 76, 2020, No. 4, p. 172-180
Category: Case Report
doi: https://doi.org/10.31348/2020/27Overview
Purpose: To introduce a rare case of patient with hyperlipidemic myeloma and ocular manifestation in form of masquerade syndrome with acute elevation of intraocular pressure (IOP) and hyperviscous retinopathy.
Results: 55-year-old man with newly diagnosed hyperlipidemic myeloma and hyperviscous syndrome was acutely referred to our glaucoma outpatient clinic due to problems with his left eye: sudden pain, blurred vision, redness of the eye and IOP of 44 mm Hg. We excluded attack of angle closure glaucoma and found presence of whitish material in the anterior chamber and blood obstructing the iridocorneal angle. Glaucoma therapy was initiated and lavage of the anterior chamber of the left eye with sampling of the aqueous humour for biochemical and cytological examination was performed. Identification of trace amount of cryoprotein in the samples of humour proved diagnosis of masquerade syndrome. Finding of the hyperviscous retinopathy and nonperfusion of wide peripheral areas of retina in both eyes was indicated to laser coagulation of these areas. The patient underwent in the meantime three times plasmapheresis, four cycles of biological therapy and autologous stem cell transplantation reaching complete remission of the myeloma. Local and systemic therapy led to significant clinical finding improvement on the anterior segment and fundus of both eyes.
Conclusions: Masquerade syndrome can be complicated by acute elevation of IOP. Diagnostic lavage of the anterior chamber, local therapy, systemic therapy and close interdisciplinary cooperation contributed to right diagnosis, IOP normalisation, ocular and general condition improvement.
Keywords:
glaucoma – hyperlipidemia – myeloma – hyperviscous syndrome – masquerade syndrome
INTRODUCTION
In acute conditions linked with unilateral pronounced elevation of intraocular pressure (IOP), in differential diagnostics it is necessary to mention in first place acute angle-closure glaucoma (glaucoma attack). However, unilateral elevation of IOP may also appear in various forms of secondary glaucoma.
Multiple myeloma with hyperlipidemia is a rare variant of multiple myeloma [1,2]. According to the World Health Organization, multiple myeloma is characterised as uncontrolled clonal proliferation of plasma cells in bone marrow, leading to the formation of non-functional immunoglobulins and their chains (paraproteins) [3]. Worldwide it represents 1 % of all malignancies and 10-15 % of haematological malignancies. The diagnostic criteria of symptomatic melanoma include the presence of 10 % or more of malignant cells in bone marrow or myeloma confirmed by biopsy, extramedullary manifestations or CRAB (C = calcium elevated, R = renal failure, A = anaemia, B = bone lesions) criteria, or other applicable biomarkers. The type of therapy depends on age, comorbidities and the risk profile of the patient. In patients younger than 70 years of age in an otherwise good general condition of health, it is recommended to administer high doses of biological therapy with subsequent transplantation of bone marrow stem cells [3,4].
Multiple myeloma may have manifestations in all ocular tissues, where it acts either directly through its infiltration and potential compression, or by indirect development of hyperviscous syndrome [5,6,7]. In the professional literature we also encounter cases with elevation of IOP and the development of glaucoma as complications of multiple myeloma [7,8,9,10].
The aim of the study is to present readers with a rare case of a patient with hyperlipidemic myeloma and its ocular manifestations in the form of masquerade syndrome with acute elevation of IOP and hyperviscous retinopathy.
CASE REPORT
A 55 year old man was acutely referred to the Glaucoma Centre of our department due to complaints in his left eye (LE). He stated pain, blurred vision and reddening of the LE. The patient had been examined previously by an outpatient ophthalmologist, who measured IOP of 44 mm Hg by contactless method, applied timolol locally and administered acetazolamide generally. This led to a reduction of IOP to 26 mm Hg.
From the patient’s medical history we determined that 3 months previously he had been hospitalised at the department of internal medicine for an examination for vertigo and state of collapse. During hospitalisation dislipidemia was diagnosed, which was unresponsive to hypolipidemic therapy. The highest values of lipids in the patient’s blood were as follows: cholesterol 22.81 mmol/l and triacylglycerols 34.05 mmol/l. Upon CT coronography there was a chance detection of osteolytic lesions of vertebral bodies. Trephpine biopsy of the right hip bone confirmed the presence of monotypic plasmocytes kappa, and thereby a diagnosis of multiple myeloma. Due to pronounced chylosis of blood serum it was not possible to perform electrophoresis of plasma proteins. Following plasmapheresis, which led to a reduction of chylosis of blood serum, the performance of electrophoresis detected the presence of short chains of immunoglobulins in class IgA kappa. The patient had therefore recently been diagnosed with multiple myeloma with hyperlipidemia, cryoprotein and hyperviscous syndrome, and the commencement of systemic therapy was planned.
The patient is being treated for type 2 diabetes mellitus, arterial hypertension, and has diagnosed dilated cardiomyopathy of ethylic etiology. In the past he had suffered acute pancreatitis, bronchial pneumonia, injury with fracture of the ribs and had undergone surgery for umbilical hernia. Since a young age the patient has smoked, previously he had consumed alcohol in large amounts, now he no longer drinks. His family ocular anamnesis is not significant. His mother underwent surgery for cancer of the throat and his father suffered a stroke.
Upon examination at our centre, visual acuity (VA) in the right eye (RE) for distance vision was determined at 0.9 with correction of -1.0 dioptre, VA LE 0.04 partim naturally, with clear light projection. IOP measured by applanation was 16 mm Hg in RE and 26 mm Hg in LE.
The finding on the anterior segment of the RE was physiological, LE (Fig. 1) had an appropriately deep anterior chamber with presence of whitish deposits on the corneal endothelium, in chamber fluid and in the iridocorneal angle (Fig. 2). Gonioscopy of the RE indicated open chamber angle with hyperpigmentation of the stroma and in front of the stroma, the chamber angle of the LE was occluded by blood, clusters of whitish deposits and accumulated blood elements.
1. (A) Finding on anterior segment of left eye in diffuse light: mixed injection, congested iris, wider, vertically oval, plegic pupil (B) Finding on anterior segment of left eye in light cross-section: mild corneal haze, finding of whitish deposits on corneal endothelium, appropriately deep anterior chamber with presence of moving whitish deposits 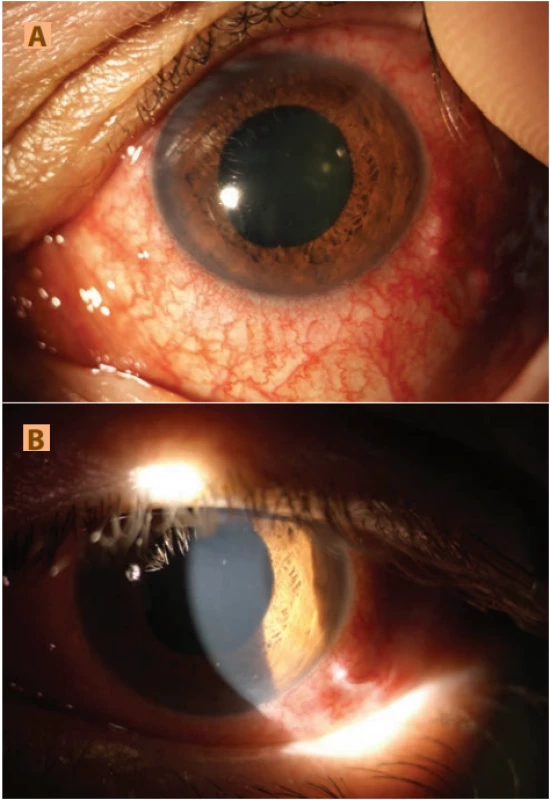
2. Gonioscopy of left eye: obturation of iridocorneal angle, in upper quadrant with clusters of whitish deposits 
The finding on the fundus of both eyes corresponded to hyperviscous retinopathy with typical haemorrhages, hard exudates and dilated tortuous blood vessels (Fig. 3).
3. Finding on fundus of right (A) and left (B) eye: fundus with blot, flame-shaped haemorrhages and Roth’s spots, from central periphery image of clusters of hard exudates, veins markedly dilated and tortuous with visible whitish deposits in blood, (B) more extensive haemorrhages and less hard exudates 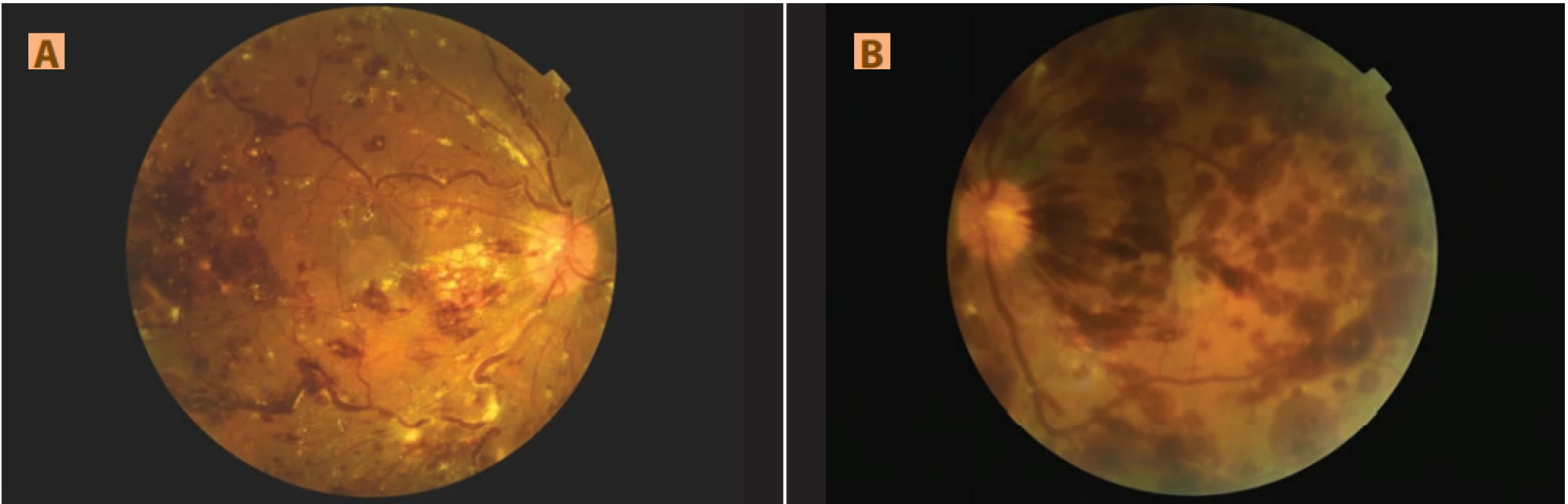
A video recording of the fundus was produced on optical coherence tomography (OCT), on which it is possible to observe blood circulation on the ocular fundus – slowly moving chylous blood column in the arteries and more in the veins (Fig. 4 – image from the video). The glaucoma perimeter (Fig. 5) manifested non-specific outages in the visual field of the RE, and diffuse decrease of sensitivity of visual field of the LE. Due to retinal changes, it was not possible to determine the thickness of the retinal nerve fibre layer on OCT (Fig. 6). OCT of the macula of the RE detected tractional changes of the fovea and intraretinal deposits, in the LE it was not possible to identify individual layers of the neuroretina (Fig. 7).
4. Image from video of fundus on optical coherence tomography of right eye: macula infiltrated, haemorrhages and hard exudates, pronounced dilation and tortuosity of blood vessels with visible whitish deposits in capillary lumen 
5. (A) Glaucoma perimeter of right eye: non-specific relative to absolute scotomas in visual field, high loss of fixation (B) Glaucoma perimeter of left eye: diffuse decrease of sensitivity of visual field 
6. Optical coherence tomography – retinal nerve fibre layer of right and left eye – circular linear scan: Thickness of nerve fibre layer could not be evaluated due to vitreoretinal traction, deposit changes of retina and imprecise demarcation of the layers 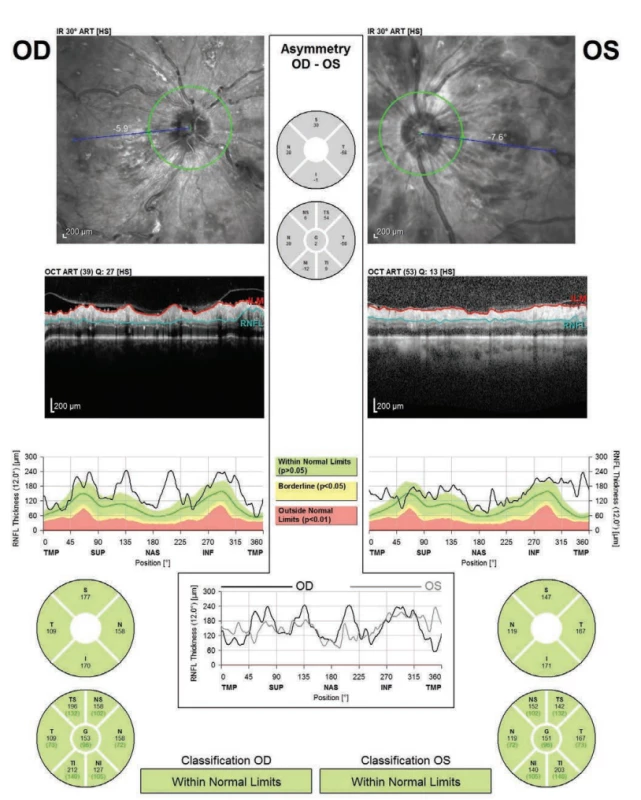
7. Optical coherence tomography of maculas of right and left eye – raster scan (map) and linear horizontal transfoveal scan: right eye: vitreomacular traction with ablation of foveola and intraretinal deposits, left eye: pronounced disorganisation of neuroretinal layers 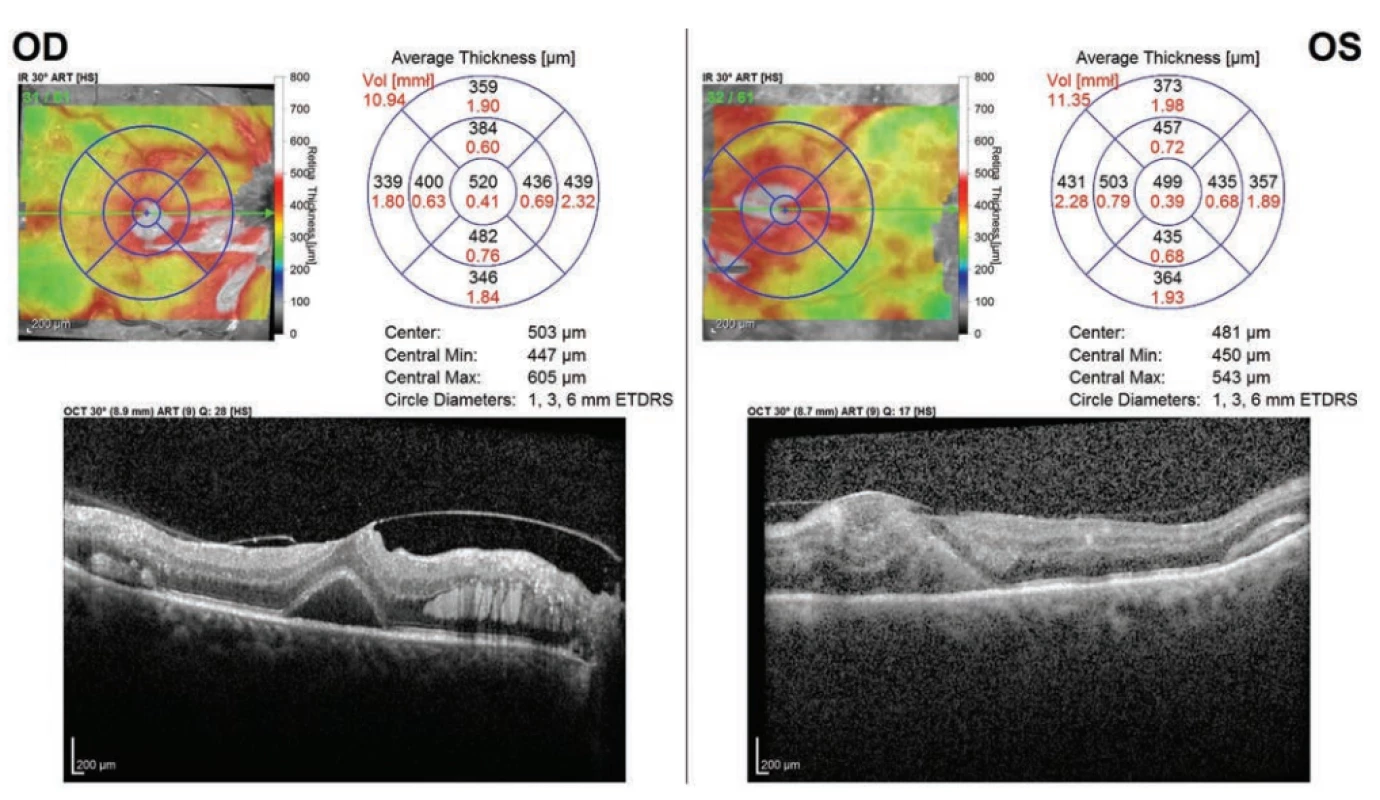
With regard to the finding, acute glaucoma attack was excluded, and a working diagnosis was determined of decompensated secondary glaucoma upon a background of hyperviscous syndrome. Anti-glaucomatous therapy was commenced, and diagnostic-therapeutic lavage of the anterior chamber of the LE was performed, with taking of samples for biochemical and cytological examination. During the course of the procedure haemorrhage occurred into the anterior chamber, upon aspiration large whitish crystalline deposits surfaced, which were subsequently drained off.
After the procedure there was an improvement of distance VA to 0.16 partim naturally with clear light projection and improvement of the ocular finding, with disappearance of the whitish deposits and blood from the anterior chamber.
Examination of the chamber angle of the LE after the procedure demonstrated medium-wide open chamber angle without the presence of blood and whitish deposits. A biochemical examination of the anterior chamber fluid confirmed the presence of a trace quantity of paraprotein class IgA, lipids and proteins. A mixture of cells was found in the cytological swabs (Fig. 8). Demonstration of the presence of paraprotein in the anterior chamber upon the background pathology, i.e. hyperviscous syndrome accompanying multiple myeloma, confirmed the diagnosis of ocular malignant masquerade syndrome.
8. Qualitative cytological examination of anterior chamber fluid of left eye – swab on glass, staining Hemacolor Rapid Staining, Merck, enlargement 63x: admixture of erythrocytes, monocytes and pigmentophages with granules – monocytic pleocytosis 
With regard to the finding on the ocular fundus, fluorescence angiography was subsequently performed, which detected extensive zones of non-perfusion in the periphery of the retina (Fig. 9). As a result, laser coagulation was performed in the area of these non-perfusion zones.
9. Fluorescein angiography of fundus of right eye: extensive zone of non-perfusion in retinal periphery and microaneurysms of retinal blood vessels 
During the course of our observation, the patient underwent repeated plasmapheresis, and systemic therapy was commenced.
After laser coagulation and during systemic therapy, the finding on the ocular fundus improved (Fig. 10). Now the patient has distance VA of 0.8 partim with correction of -1.0 dioptre in the RE, 0.32 partim naturally in the LE. For near vision RE reads 0.63 with difficulty, LE 0.5, both with addition of +2.0 dioptres. A test on an Amsler grid was negative, and IOP in RE is 15 mm Hg, in LE 16 mm Hg. Local therapy of LE incorporates a fixed dual combination of timolol and dorzolamide.
10. Finding on fundus of both eyes with time interval after laser coagulation of the retina: absorption of retinal haemorrhages, partially also of hard exudates, veins now less dilated and tortuous 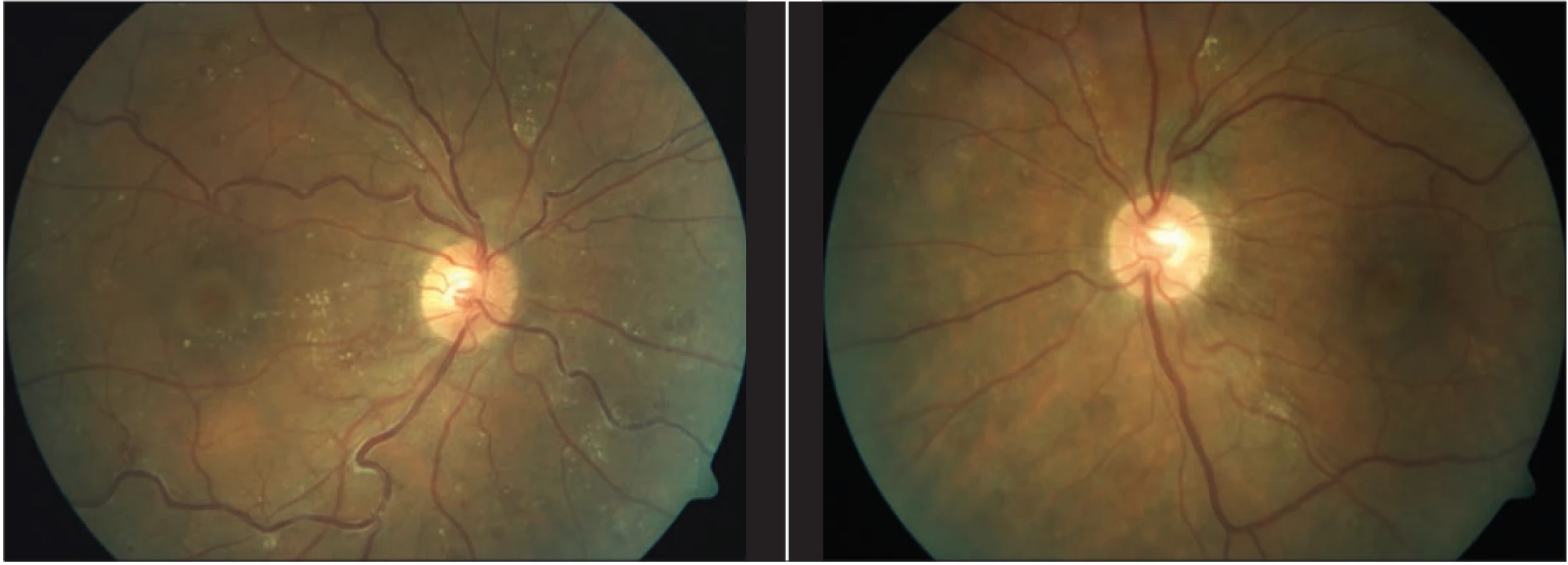
At a control OCT of the macula there was a pronounced improvement of the finding (Fig. 11). The control glaucoma perimeter manifested non-specific changes in the visual field of the RE and 2 absolute scotomas in the upper periphery of the visual field (Fig. 12A). Non-specific regions of reduced sensitivity of the visual field were recorded in the LE (Fig. 12B).
11. Follow-up examination image of macula of right eye: decrease of ablation of fovea, partial absorption of intraretinal deposits, in left eye individual layers of neuroretina can now be distinguished 
12. (A) Control perimeter of right eye: widened Mariott’s spot and small non-specific areas of reduced sensitivity of visual field, (B) Control perimeter of left eye: 2 absolute upper paracentral scotomas and non-specific areas of reduced sensitivity of visual field 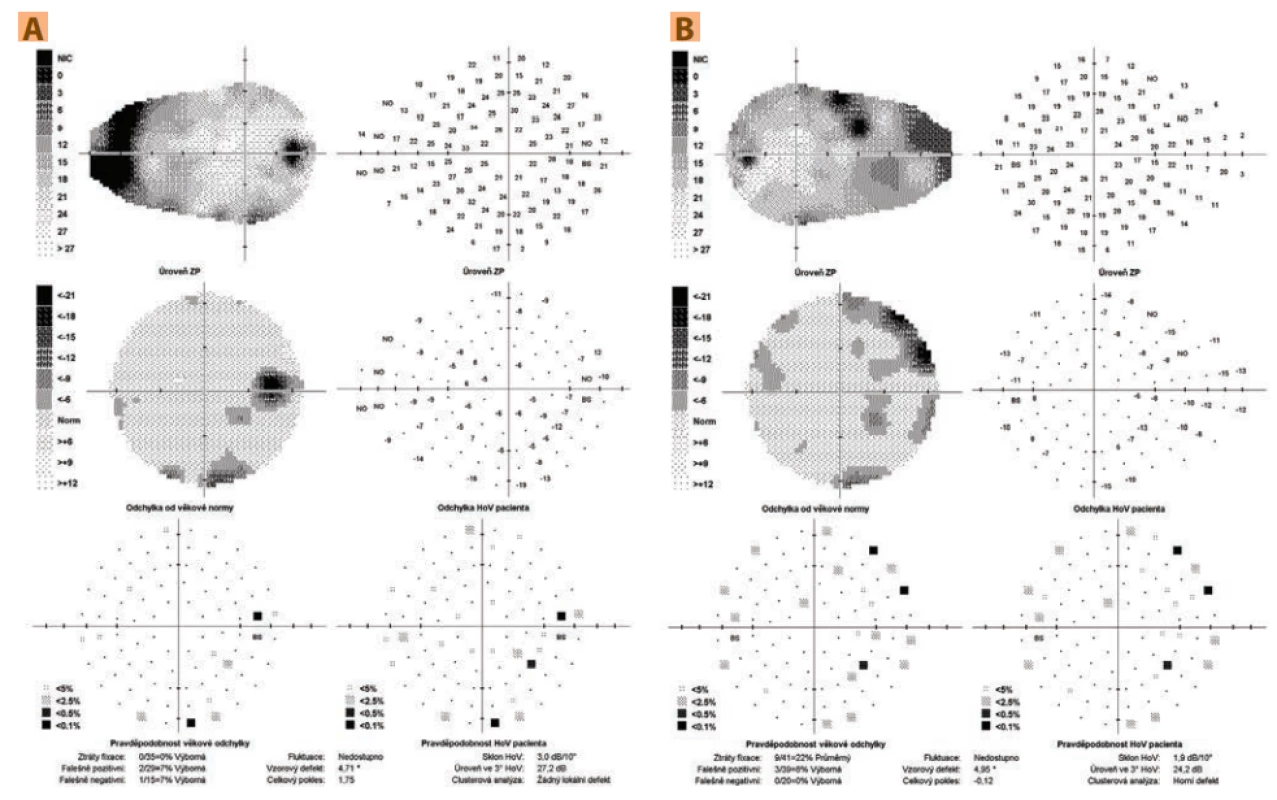
During the course of the observation, the patient underwent plasmapheresis 3 times, 4 cycles of CVD therapy (C = cyclophosphamide, V = Velcade = bortezomib, D = dexamethasone), and subsequently autologous transplantation of bone marrow stem cells for the basic pathology. The systemic pathology is now in complete remission.
DISCUSSION
Multiple myeloma may be manifested in the eye in several ways, which include: exophthalmos, diplopia, eyelid ecchymosis, xanthomatosis, edema of the eyelids, conjunctival or corneal crystalline and non-crystalline deposit, subconjunctival suffusion, manifestations of masquerade syndrome imitating scleritis, episcleritis, iritis, retinal vasculitis, also acute angle closure, debris in the iridocorneal angle, subluxation of the lens, deposit in the lens, cysts of ciliary body, ciliochoroidal effusion, uveal infiltration, hyperviscous retinopathy or dysproteinemic fundus, detachment of neurosensory retina or retinal pigment epithelium, subretinal deposit, central retinal artery occlusion, edema of optic nerve papilla or finding similar to retrobulbar neuritis [7,11].
In connection with hyperlipidemia and myeloma, the works published to date state the incidence of corneal deposits and haemorrhage on the ocular fundus, e.g. in the form of flame-shaped haemorrhages, and it is therefore possible to assume hyperviscous retinopathy or vein occlusion [12,13].
Glaucoma has not been described in these cases, and we are therefore of the opinion that in our case this probably concerns an isolated case of a patient with secondary glaucoma as a complication of hyperlipidemic myeloma.
Cases of secondary glaucoma as an ocular complication of multiple myeloma without hyperlipidemia have been described, in which there was an elevation of IOP. These concerned for example a case of a patient with metastasis of myeloma on the iris, in which trabulectomy was performed with cytological examination of a sample of anterior chamber fluid, confirming a diagnosis of unilateral masquerade syndrome [10]. In another patient there was an elevation of IOP upon a background of unilateral acute closure of the iridocorneal angle with bilateral subluxation of intraocular lenses, which may have been caused by a shift of the root of the iris by a present cyst of the ciliary body, a shift of the lens upon a loose suspension mechanism or the formation of peripheral anterior synechiae with chronic mild iritis [8]. Another case related to a patient with a unilateral deposit of myeloma of the iris, which circularly obturated the iridocorneal angle [3]. In the Czech literature a case of acute closure of the anterior chamber angle due to detachment of the choroid has been described in a patient with smouldering myeloma [5]. Also described are cases of secondary glaucomas originating as a consequence of myeloma therapy. After administration of the monocular antibody daratumumab, bilateral closure of the iriodocorneal angle developed with the influence of ciliochoroidal effusion [4]. Further examples were neovascular glaucomas, e.g. upon cytomegaloviral retinitis, which developed upon immunosuppressive therapy following bone marrow transplantation [14] or in the case of bilateral secondary ocular metastasis of myeloma, in which intravitreal application of bevacizumab led to the control and treatment of metastases of myeloma [15].
Among other mechanisms of the development of glaucoma we include indentation of the eyeball by an orbital deposit, obturation of the stroma of the iridocorneal angle by material of a protein nature, shift of the iris and ciliary body with the formation of peripheral anterior synechiae and closure of the iridocorneal angle [7,8].
In our case this concerned masquerade syndrome with obturation of the stroma by material composed of paraprotein class IgA, lipids, proteins and blood. Lavage of the anterior chamber, local and systemic therapy led to an improvement of the ocular finding and normalisation of IOP.
In addition, the condition in our patient was complicated by a finding of retinopathy upon a background of hyperviscous syndrome. Hyperviscous syndrome is a life-threatening complication. This concerns a state with increased blood viscosity. It is clinically manifested in neurological symptoms, ocular manifestations and haemorrhage. Of key importance is examination of the ocular fundus with a finding of hyperviscous retinopathy, typically manifested in the presence of haemorrhages, microaneurysms, hard deposits, dilation and tortuosity of veins. The finding on the fundus correlates very well with abnormally increased blood viscosity [16,17,18,19]. Increased viscosity causes increased concentration of proteins in the blood, large size of molecules, abnormal polymerisation and shape of immunoglobulin molecules [18]. Hyperviscous syndrome most often develops in Waldenström’s macroglobulinemia and multiple myeloma [19]. Timely diagnosis and therapy of the basic pathology is often insufficient, and as a result plasmapheresis is used, which reduces the concentration of paraprotein, alleviates symptoms and improves the condition of the general pathology and ocular finding [17].
In the literature we also encounter cases with bilateral central vein occlusion, in which hyperviscous syndrome and multiple myeloma were subsequently determined. Ocular complaints may therefore precede a diagnosis of a severe systemic pathology, and as a result it is necessary to perform a general internal and haematological examination in occlusive states of retinal veins [20,21,22,23].
In our patient ocular complaints appeared after the determination of the diagnosis of myeloma, the finding corresponded to hyperviscous retinopathy in both eyes. Systemic therapy led to a significant improvement of the finding on the ocular fundus and improvement of VA in both eyes.
Each patient with a diagnosis of multiple myeloma should undergo a consultancy ocular examination due to the possible identification of ocular manifestations, which could cause loss of sight or be an indication of the patient’s general condition [7].
According to the available literature only 53 cases of hyperlipidemic myeloma have been described. Characteristically this more often concerns myeloma with overproduction of IgA antibodies, hyperlipidemia unresponsive to hypolipidemic therapy, formation of xanthomas and blood hyperviscosity [2]. The mechanism of origin of hyperlipidemia has not been entirely clarified to date. Under consideration is the formation of complexes of paraproteins with lipoproteins, with an attendant inhibition of degradation of lipids by lipases [1,2,24]. The association of myeloma with hyperlipidemia is very rare, but clinically important, because it is always necessary to investigate the etiology of secondary hyperlipidemia [24].
Our case corresponds typically to the variant of myeloma with overproduction of paraprotein in class IgA, hyperlipidemia unresponsive to hypolipidemic therapy and hyperviscous syndrome.
CONCLUSION
In the presented patient there was an elevation of IOP upon a background of obturation of the stroma of the chamber angle by deposits containing paraprotein, lipids, proteins and blood. Lavage of the anterior chamber and examination of samples of intraocular fluid confirmed a diagnosis of ocular malignant masquerade syndrome with hyperlipidemic myeloma. Local and general therapy contributed to the resulting normalisation of IOP and improvement of the ocular finding.
This concerns a very rare case of myeloma with secondary hyperlipidemia, which documents the importance of inter-disciplinary co-operation.
Thanks
The authors thank Dr. Kateřina Mrázová from the Institute of Medical Biochemistry and Laboratory Diagnostics at the 1st Faculty of Medicine of Charles University and the General University Hospital in Prague for examination of samples of anterior chamber fluid.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of the professional communication entitled “Acute Elevation of Intraocular Pressure in Patient with Hyperlipidemic Myeloma”, and that it is not supported by any pharmaceuticals company.
The study has not been submitted to any professional journal or printed elsewhere.
Sources
1. Beaumont JL, Beaumont V. Autoimmune hyperlipidemia. Atherosclerosis. 1977;26(4):405-418.
2. Misselwitz B, Goede JS, Pestalozzi BC, Schanz U, Seebach JD. Hyperlipidemic myeloma: review of 53 cases. Ann Hematol. 2010;89(6):569-577.
3. Gerecke Ch, Fuhrmann S, Strifler S, Schmidt-Hieber M, Einsele H, Knop S. Diagnostik und Therapie des Multiplen Myeloms. [The Diagnosis and Treatment of Multiple Myeloma]. Dtsch Arztebl Int. 2016;113(27-28):470-476. German.
4. Lee AC, Greaves G, Lee R et al. Bilateral Angle Closure Following the Infusion of a Monoclonal Antibody to Treat Relapsing Multiple Myeloma. J Glaucoma. 2018;27(9):e145-e147.
5. Heissigerová J, Říhová E, Svozílková P, Kovařík Z, Špička I. Odchlípení cévnatky jako první příznak hematologické malignity. Prakt Lék. 2006;86(12):702-704. Czech.
6. Mehta J, Singhal S. Hyperviscosity Syndrome in Plasma Cell Dyscrasias. Semin Thromb Hemost. 2003;29(5):467-472.
7. Omoti AE, Omoti CE. Ophthalmic manifestations of multiple myeloma. West Afr J Med. 2007;26(4):265-268.
8. Baker TR, Spencer WH. Ocular Findings in Multiple Myeloma. Arch Ophthalmol. 1974;91(2):110-113.
9. Chin KJ, Kempin S, Milman T, Finger PT. Ocular manifestations of multiple myeloma: three cases and a review of the literature. Optometry - J Am Optom Assoc. 2011;82(4):224-230.
10. Guerriero S, Piscitelli D, Ciraci L, Carluccio P, Furino C, Specchia G. Hypertensive uveitis as a feature of multiple myeloma. Ocul Immunol Inflamm. 2010;18(2):104-106.
11. Maisel JM, Miller F, Sibony PA, Maisel LM. Multiple myeloma presenting with ocular inflammation. Ann Opthalmol. 1987;19(5):170-174.
12. Hurley IW, Brooks AM, Reinehr DP, Grant GB, Gillies WE. Identifiying anterior segment crystals. Br J Ophthalmol. 1991;75(6):329-331.
13. Roberts-Thompson PJ, Venables GS, Onitiri AC, Lewis B. Polymeric IgA myeloma, hyperlipidaemia and xanthomatosis: a further case and review. Postgrad Med J. 1975;51(591):44-51.
14. Cho J, Siegel N, Subramanian ML, Ying H, Ness S. Rapidly progressive neovascular glaucoma from cytomegalovirus retinitis in a non-human immunodeficiency virus patient. Retin Cases Brief Rep. 2018. Available from: https://journals.lww.com/retinalcases/Abstract/9000/RAPIDLY_PROGRESSIVE_NEOVASCULAR_GLAUCOMA_FROM.98844.aspx. doi:10.1097/ICB.0000000000000734.
15. Zhou Q, Liang J, Lu H. Intravitreal bevacizumab for ocular metastasis of multiple myeloma. Optom Vis Sci. 2013;90(9):236-240.
16. Carr RE, Henkind P. Retinal Findings Associated with Serum Hyperviscosity. Am J Ophthalmol. 1963;56 : 23-31.
17. Dumas G, Merceron S, Zafrani L et al. Hyperviscosity syndrome. Rev Med Interne. 2015;36(9):588-595.
18. Mehta J, Singhal S. Hyperviscosity Syndrome in Plasma Cell Dyscrasias. Semin Thromb Hemost. 2003;29(5):467-472.
19. Perez RA, Estes M. Hyperviscosity Syndrome. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK518963/
20. Borgman CJ. Concomitant multiple myeloma spectrum diagnosis in a central retinal vein occlusion: a case report and review. Clin Exp Optom. 2016;99(4):309-312.
21. Chiang CC, Begley S, Henderson SO. Central retinal vein occlusion due to hyperviscosity syndrome. J Emerg Med. 2000;18(1):23-26.
22. Golesic EA, Sheidow TG. An otherwise healthy young man presents with bilateral CRVO as the first sign of hyperviscosity syndrome in the setting of new multiple myeloma. Retin Cases Brief Rep. 2015;9(1):38-40.
23. Helal J, Malerbi FK, Melaragno FR. Bilateral central retinal vein occlusion associated with blood hyperviscosity syndrome--case report. Arq Bras Oftalmol. 2005;68(1):126-128.
24. Rahman S. Light Chain Myeloma induced Severe Hypertriglyceridemia. J Clin Diagn Res. 2017;11(3):1-3.
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2020 Issue 4-
All articles in this issue
- VEGF: A KEY PLAYER NOT ONLY IN MACULAR DEGENERATION. A REVIEW
- Recommendations for the Management of Uveitis Associated With Juvenile Idiopathic Arthritis: The Czech and Slovak adaptation of SHARE Initiative
- RESULTS OF 15 YEARS OF COLLABORATION BETWEEN THE DEPARTMENTS OF OPHTHALMOLOGY AND STOMATOLOGY IN ONCOLOGICAL SURGERY OF THE ORBIT: A DIAGNOSTIC AND THERAPEUTIC APPROACH
- USAGE OF DIGITAL D CHART TEST AS A MODIFICATION OF AMSLER GRID IN OPHTHALMOLOGY AND OPTOMETRY
- OCULAR COMPLICATIONS OF DIABETES MELLITUS IN PREGNANCY – CASE REPORT
- Acute elevation of intraocular pressure in patient with hyperlipidemic myeloma
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- OCULAR COMPLICATIONS OF DIABETES MELLITUS IN PREGNANCY – CASE REPORT
- Acute elevation of intraocular pressure in patient with hyperlipidemic myeloma
- Recommendations for the Management of Uveitis Associated With Juvenile Idiopathic Arthritis: The Czech and Slovak adaptation of SHARE Initiative
- RESULTS OF 15 YEARS OF COLLABORATION BETWEEN THE DEPARTMENTS OF OPHTHALMOLOGY AND STOMATOLOGY IN ONCOLOGICAL SURGERY OF THE ORBIT: A DIAGNOSTIC AND THERAPEUTIC APPROACH
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

