-
Medical journals
- Career
Femtosecond Laser - assisted intrastromal corneal segment implantation - our experience
Authors: K. Kapitánová 1,2; J. Nikel 1
Authors‘ workplace: UVEA Mediklinik s. r. o., Martin prim. MUDr. Vida Rastislav 1; Očná klinika JLF UK a UN Martin prednosta MUDr. Žiak Peter, PhD. 2
Published in: Čes. a slov. Oftal., 74, 2018, No. 1, p. 31-36
Category: Original Article
Overview
Introduction:
The intrastromal corneal ring segments implantation is widely used as an effective method for keratoconus correction. Femtosecond laser technology represents very precise and modern approach in corneal tunnel creation. Nevertheless complication like an extrusion of the implanted ring segment rarely appears. There are few different types of intrastromal corneal segments available. Keraring (Mediphacos Ltd.) is primary designed for keratoconus treatment.Materials and methods:
We evaluated results of the Keraring implantations in 32 patients (48 eyes) with keratoconus or with marginal pellucid degeneration. We implanted 78 segments totally in the period from January 2015 to February 2017, with the assistance of femtosecond laser. We present our data collected after the 6 months follow up. Uncorrected visual acuity – UCVA and best corrected visual acuity – BCVA were evaluated. We scored the changes in the subjective and objective refraction. The complications were observed.Results:
Preoperative UCVA was in 44 (91,60%) eyes under or equal 0,3. Postoperative UCVA after 6 months was in 29 (60,41%) eyes over or equal 0,3. Visual acuity improved in 38 (79,16%) eyes totally with the gain of 1 to 9 lines, BCVA improved in 27 (56,25%) eyes and in 15 (31,25%) eyes stayed postoperatively unchanged. There was reduction of the spherical equivalent (SE), in the subjective and objective refraction. In our group there we detected 9 (18,75%) extrusions of the implanted ring segment, which occurred on average 7,3 months (range 2/ 16 months) after the surgery.Conclusion:
Intrastromal corneal ring segments implantation with the femtosecond laser assistance is an effective approach in the keratoconus treatment. Complications are not often observed. With careful selection of the suitable patient it is possible to avoid them.Key words:
keratoconus, intrastromal corneal ring segments, femtosecond laserIntroduction
Keratoconus is a bilateral, progressive, non-inflammatory pathology of the cornea. The estimated prevalence at present is approximately 1 per 2000 patients. The incidence of keratoconus is approximately 50 to 230 cases per 100 000 of the regular population. The pathology is of a multifactorial character. To date the etiology is not precisely known. A deterioration in the quality of vision occurs as a consequence of progressive thinning and buckling of the cornea, which leads to the development of irregular astigmatism, and potentially also to myopisation [4]. The local and topographic finding is generally asymmetrical, and as a result younger patients especially register a deterioration of central visual acuity only upon progression of the pathology to the second eye, in which vision is better [8].
Implantation of intrastromal corneal rings or corneal segments represents a mini-invasive surgical procedure in the correction of keratoconus or corneal ectasias (following laser refractive operations, post-traumatic states etc.). Long-term studies point to promising results in the adjustment of uncorrected and corrected visual acuity, and the topographic finding of the cornea [4].
Actual implantation takes place in two steps. The first is the creation of a intrastromal corneal tunnel, either manually [7, 9] or with the use of a femtosecond laser. Manual separation of the stroma is linked with a higher risk of occurrence of perioperative complications [1]. In 2003, the use of a femtosecond laser in the creation of a stromal tunnel therefore enabled the possibility of creating a precise intrastromal incision and attaining the same refractive results, but with a higher standard of safety in comparison with the conventional use of a standard separator [6]. According to a number of published studies, this technique for the implantation of corneal segments is a safe and effective method for the treatment of keratoconus. In addition, this method significantly shortens the duration of the procedure [1].
The used intrastromal segments are oval shaped sections of polymethyl methacrylate (PMMA), the dimensions, curvature, thickness and place of implantation (distance from centre of cornea) are variable parameters. At present a number of different types of intrastromal segments are available on the market. Intacs ® by Addition Technologies, Inc. are segments available in various thicknesses, from 0.210 to 0.500 mm. The variant Intacs ® SK has a design with rounded edges, which potentially reduces visual symptoms. Keraring by Mediphacos Ltd. is manufactured from PMMA with a UV blocker, and has a typical triangular profile, variable thickness and length of curvature up to 340° (note: in the past a 355° model was available). It is designed primarily for the correction of keratoconus [5].
MyoRing by DIOPTREX GmbH is a 360° continuous corneal ring implanted into the corneal sac. Its advantage is the possibility of postoperative adjustment of the position of the ring [9].Material and methods
In our study we engaged in a complex evaluation of the results of intrastromal implantation of Keraring corneal segments with the use of a femtosecond laser (Victus, Bausch and Lomb).
We evaluated a cohort of 48 eyes in 32 patients operated on at our clinic in the period from January 2015 to February 2017, for whom an observation period of at least 6 months was stipulated. In the cohort we examined best uncorrected and best corrected central visual acuity (UCVA and BCVA) on an LCD optotype Topcon CC – 100XP. We also evalauted changes of subjective and objective refraction, and observed the occurrence of adverse reactions. The observed cohort comprised a total of 23 men and 9 women aged between 21 and 73 years. Out of the total number of operated eyes, keratoconus was diagnosed in 42 eyes (87.5%). Of this number, in 31 eyes (73.8%) the type was paracentral “oval”, in 9 eyes (21.42%) from a morphological perspective it concerned the central or “nipple” type, and in 2 eyes (4.76 %) the morphological “bowtie” type.
According to the Amsler - Krumeich classification, we classified 15 eyes (31.25 %) with keratoconus in stage 2 and 27 eyes with keratoconus (56.25 %) in stage 3. None of the operated eyes corresponded to stage 1 or stage 4 of keratoconus according to the Amsler - Krumeich classification. In the remaining 6 eyes (12.5%) marginal pellucid degeneration was stated as the operational diagnosis.On the basis of the generally valid recommendations, minimal preoperative corneal thickness was stipulated at 380um, with the exception of one patient, in whom corneal thickness was 330um in one eye. Contraindication for the procedure was swelling of the cornea, central opacification of the cornea, inflammatory pathology of the cornea (infectious, immune altering), strong atopy, recurrent erosive corneal syndrome, as well as inappropriate expectations on the part of the patient.
The selection of the ring took place on the basis of the use of “nomograms”. This concerns calculators supplied by the manufacturer in the form of tables taking into account 3 factors. Type of corneal asymmetry on the basis of the topographical finding, corneal thickness and subjective refraction of the patient. Specifically for calculation of the Keraring segments we took as our basis 4 types of corneal asymmetry. Type 1 – 100% of the pathologically curved part of the cornea illustrated on colour corneal map as red zone located on 1 side of the referential meridian. Type 2 – distribution of red zone of pathologically curved part of cornea, with regard to meridian 20% to 80%. Type 3 – distribution corresponds to approximately a ratio of 60% to 40%, and in the case of type 4 the ratio is approximately 50% to 50% (Fig. 1). Nomogram A is designated for the types one and two of corneal asymmetry, for type three Nomogram B and for type four Nomogram C.
1. Types of corneal assymetry used for Keraring calculations 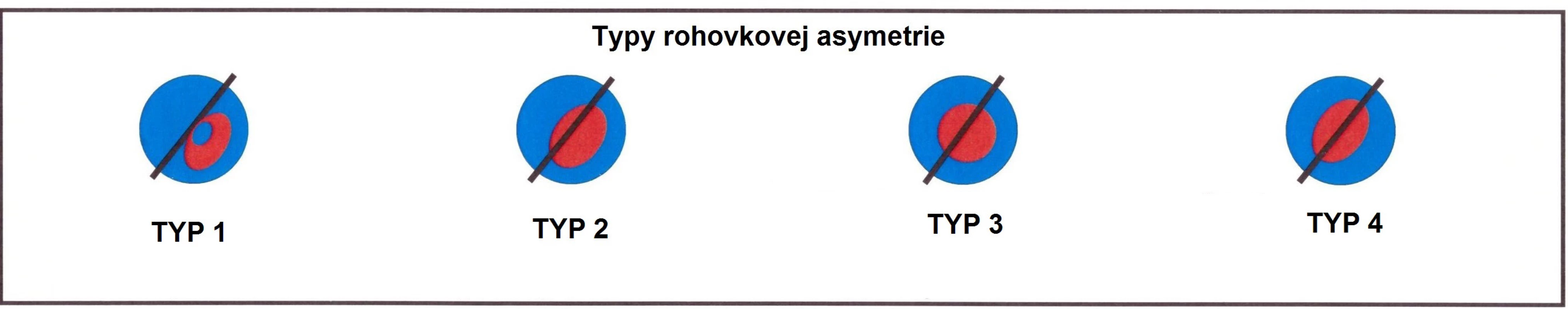
Before the operation, each patient was instructed in detail with regard to its course and consequences, and voluntarily signed an informed consent form in accordance with the valid law. The entire procedure took place under local anaesthesia (oxybuprocaine chloride) instilled into the conjunctival sac. A femtosecond laser was used on all eyes for the creation of a stromal corneal tunnel (Fig.2 and 3). The depth (base) of the tunnel was located at 74 to 80% of the minimum depth of the cornea in the trajectory of the tunnel. Other parameters (position, length, diameter, depth of tunnel and position of incision) were based on the characteristics of the specific implanted segment. They were supplied by the manufacturer in final form, together with the rings as such, and with their calculation according to the valid nomograms.
Fig. 2,3 Photo of anterior segment and an anterior segment optical coherence tomography scan showing result of stromal tunnel creation immediately after procedure 
After the actual implantation of the rings with the use of the micro-instruments recommended by the manufacturer, in certain cases (perioperative erosion of the corneal epithelium) a therapeutic contact lens was applied. We instilled 10% Braunol solution and a local wide spectrum antibiotic in liquid form (levofloxacin) into the conjunctival sac. It was recommended to all the patients to continue in the stated local antibiotic therapy. Subsequently a local corticosteroid preparation was also added in liquid form (fluorometholone), with simultaneous instruction of the patient regarding an adequate postoperative regime.
Results
In the period of January 2015 to February 2017 we implanted a total of 78 rings at our centre (Fig. 4). In the cohort of 48 evaluated eyes, in 44 eyes (91.6%) preoperative UCVA was lower or equal to 0.3, whereas postoperative UCVA after 6 months in 29 eyes (60.41%) was higher or equal to 0.3.
Average UCVA in the total evaluated cohort improved postoperatively from 0.14 (σ 0.056) to 0.39 (σ 0.318). In 4 eyes (8.33%) there was a postoperative loss of 1 to 2 rows (in 2 cases in connection with extrusion of the ring), and in 21 eyes (43.73%) we recorded a gain of 4 to 9 rows.
Average BCVA improved in the full cohort from preoperative 0.5 (σ 0.318) to 0.6 (σ 0.459) at the end of the 6 month observation period. In 6 eyes (12.50%) there was a postoperative loss of 1 to 3 rows (of which 4 cases again were in connection with extrusion of the ring), in 9 eyes (18.74%) there was an improvement of 4 to 7 rows. Overall UCVA improved in 38 eyes (79.16%) and BCVA in 27 eyes (56.25%) (Table 1).
In subjective refraction the average values of spherical equivalent (SE) were reduced from preoperative -3.64 (σ 0.353; range from +1.0 to -13.5) to -0.46 (σ 3.535; range from +3.0 to -5.0) after 6 months. In objective refraction the change of average SE was evaluated from an initial -5.15 (σ 1.944; range from +0.5 to -17.75) to -1.77 (σ 2.828; range from +5.75 to -11.75) (Table 2 and 3).
Of complications, in the postoperative period migration of the segment in a direction toward the primary incision was observed in 9 eyes (18.75%), of which in 7 eyes we proceeded with a repositioning of the segment (in 4 eyes repeatedly). However, eventually definitive extrusion occurred in all 9 eyes, with the necessity of explantation of the ring, on average 7.3 months (σ 4.949; from 2 to 16 months) after the primary implantation (Fig. 5). In this group of patients, 6 eyes (66.66%) were with keratoconus stage 3 according to the Amsler –Krumeich classification, 1 eye (11.11%) corresponded to stage 2 and in the last 2 eyes (2.22%) this concerned marginal pellucid degeneration with an advanced topographical finding. From a morphological perspective this predominantly (6 eyes) concerned a paracentral “oval” type. Two patients with this complication had very poor postoperative compliance. All the extruded rings had inferotemporal localisation, 8 of them were implanted in a pair with a superonasally localised shorter segment. The position of the incision in all the above cases was in the temporal to superotemporal part of the cornea.
Even after a thorough analysis of our cohort we did not find any common denominator which would be capable of explaining these extrusions. In all eyes with this complication the minimum corneal thickness in the trajectory of the ring was adhered to in accordance with the manufacturer's recommendation. The technical specifications from the femtosecond laser corresponded in all eyes with the manufacturer's recommendations, and did not differ in any way from the parameters applied in the eyes where extrusion did not occur. We did not record any other complications in our cohort of patients.1. Overview of the changes in UCVA and BCVA in our evaluated group. 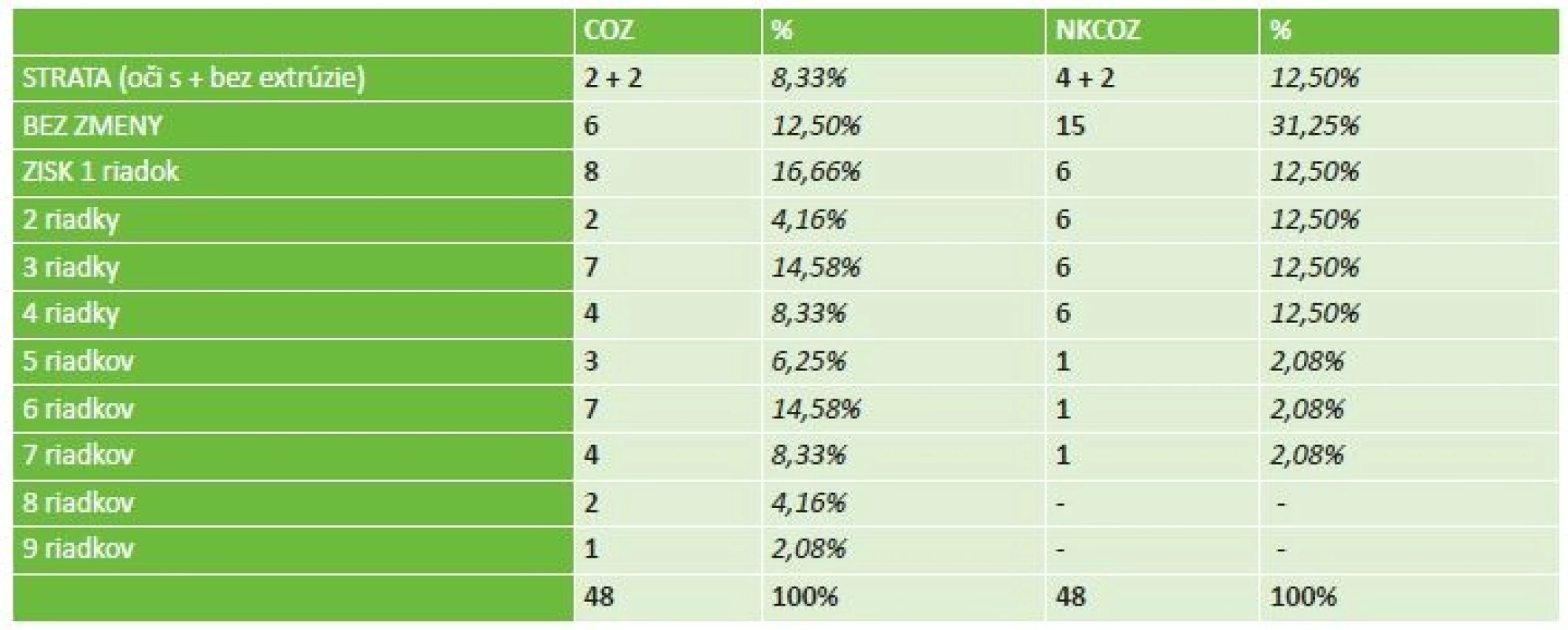
2. Postoperative reduction the subjective refraction values. 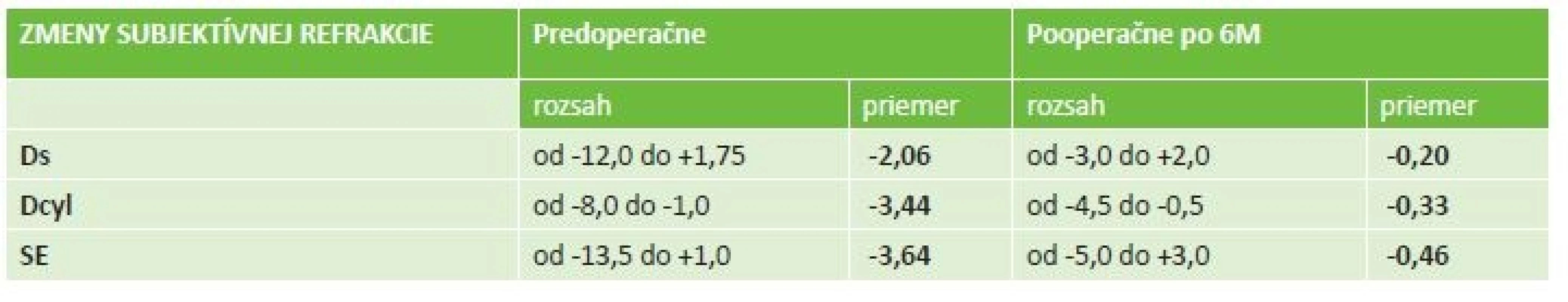
3. Postoperative reduction in the objective refraction values. 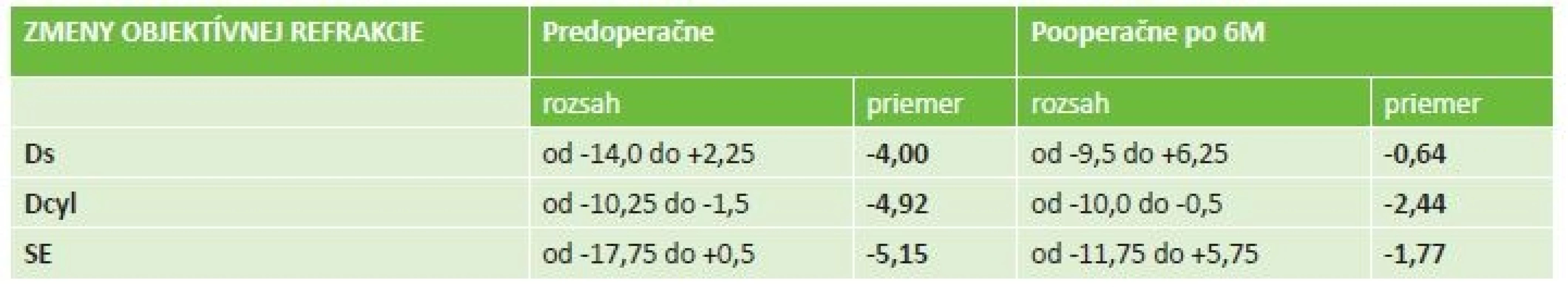
Fig. 4 Appearence 1 month after the implantation of intrastromal corneal segments Keraring 
Fig. 5 Extrusion of the temporal part of corneal segment through the primary incision with subsequent melting of corneal tissue. The explantation is necessary 
Discussion
Implantation of intrastromal corneal segments and rings represents a widespread procedure in today's correction and treatment of keratoconus. Its indisputable advantages are reversibility, high degree of dosing and the possibility of combining the condition after implantation with further treatment (cross – linking, intraocular surgery). Furthermore, the application of a femtosecond laser in creating an intrastromal tunnel is a safe and modern replacement for the manual method.
Wilde et al. evaluated a group of 66 eyes after implantation of intrastromal Keraring segments with the aid of the femtosecond laser Zeiss Visumax. In total, within the observed cohort BCVA improved in the sense of a gain of at least one row of Snellen's optotypes in 39 eyes (59.09%), and in 23 eyes (34.84%) remained unchanged postoperatively. In the observed cohort they proceeded with explantation of the ring in 4 eyes (6.06%), of which in 3 cases due to absence of improvement of vision and in 1 case due to the occurrence of corneal neovascularisation [10].
In a study from 2007 dealing with the effectiveness and safety of implantation of intrastromal corneal rings, Zare et al. state migration of the segment into the incision, with subsequent extrusion in 3 cases (13.63%) as a complication. This occurred 3 to 6 months after implantation, and always concerned an inferior-located segment. In one of the cases the condition was accompanied by melting of the corneal tissue, with the necessity of subsequent explantation of the segment, in two cases they proceeded with repositioning of the segment with suturing of the incision using a 10-0 Nylon mattress suture. At the same time they state in the study that in two cases (9.09%) repeated extrusions and significant thinning of the cornea around the segments eventually led to their inevitable removal [11].A shift of the intrastromal segment was observed by Coskunseven et al. in 11 cases (0.8%), of which in seven eyes they proceeded with repositioning of the segment and subsequent suture of the primary incision, by which they prevented any further undesirable movement of the segment and in the other four cases they chose explanation of the ring before melting of the cornea in the surrounding area of the ring took place [1].
In 2010 Ferrer et al. published a multicentric study in which they evaluated the incidence and causes of explantation of intrastromal corneal rings. In the observed cohort of 250 eyes they proceeded with explantation a total of 57 times (22.8%), out of which in 28 cases (11.2%) the reason was extrusion of the segment. In these cases a femtosecond laser was used 15 times for the creation of a corneal tunnel, and mechanical dissection was used 13 times [3].
Extrusion of the ring is one of the most frequent reasons for its explantation. The incidence varies markedly in the published studies (0.98 – 30%), in which the influence on it may have a number of factors. However, intrastromal corneal segments can be relatively easily removed, in which case as a rule healing of the cornea takes place to the extent that parameters such as visual acuity, refraction and the topographical finding return to a level close to the preoperative finding. In some cases explantation is not necessary, but only rotation or repositioning of the segment to the optimal position, thanks to which it is possible to avoid definitive expulsion of the ring [5].
According to a publication from 2012, extrusion most often takes place in patients with a thin stromal layer covering the segments, as well as in cases where the position of the ring is in the immediate vicinity of the incision. In general the rule should apply that the thickest part of the segment should not exceed 50% of the thickness of the cornea in the place of its implantation. If the thickness of the required segment is more than half the thickness of the stroma, a thinner segment should be selected, even at the cost of a lesser corrective effect on the resulting refraction. This represents the so-called rule of pachymetry upon implantation of intrastromal rings, upon the use of which the author states a significant reduction in the incidence of extrusions [2]. In our cohort of patients we did not use this procedure. We adhered strictly to the minimal corneal thickness as recommended by the manufacturer in the trajectory of the ring, as against the thickness of the ring itself. Despite this, upon retrospective evaluation we could state that only in 1 patient (11.1%) out of 9 with extrusion of the ring, did its thickness exceed 50% of the thickness of the cornea in the place of implantation, by 3.2%.
Conclusion
Implantation of intrastromal segments and rings is an effective treatment for ectatic dystrophies of the cornea in correctly indicated patients. It leads to an improvement of UCVA and BCVA, to a change of values of subjective and objective refraction in the patient, as well as to a stabilisation of the topographic corneal finding. In our evaluated group of patients, upon selection of a suitable ring we strictly adhered to the declared procedures of the manufacturer. With regard to the similar position of all 9 extruded segments, as well as the similar location of the initial incision in these cases, we evaluated inferotemporal localisation of the segment as of higher risk. In addition, we indicated habitual mechanical influences on the part of the patient (rubbing and wiping of eyes), which the majority of patients admitted to doing in the postoperative period, to be a partial factor which could have had a negative influence on the definitive extrusion of the ring. This theory is supported to a certain extent also by the fact that extrusion of the segment took place at very different time intervals from the primary implantation, as well as from the attempt at repositioning (interval 1 to 6 months).
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Delivered to the editorial board 11.12.2017
Received for printing 28.2.2018
Dr. Karolína Kapitánová
Eye Hospital UVEA MEDIKLINIK s.r.o., Zelená 1, 036 01 Martin – Priekopa
Department of Ophthalmology, Jessenius Faculty of Medicine, Comenius University and University Hospital Martin, Kollárova 2, 036 59 Martin
Sources
1. Coskunseven, E., G.D., Tsiklis, N.S., et al.: Complications of Intrastromal Corneal Ring Segment Implantation Using a Femtosecond Laser for Channel Creation: A Survey of 850 Eyes with Keratoconus. Acta Ophthalmologica 89, č. 1 (február 2011): 54–57. URL <https://doi.org/10.1111/j.1755-3768.2009.01605.x>
2. Ferrara, G., Torquetti, L., Ferrara, P., et al.: Intrastromal Corneal Ring Segments: Visual Outcomes from a Large Case Series. Clinical & Experimental Ophthalmology 40, č. 5 (júl 2012): 433–39. URL <https://doi.org/10.1111/j.1442-9071.2011.02698.x>
3. Ferrer, C., Alió, J.L., Montañés, A.U., et al.: Causes of Intrastromal Corneal Ring Segment Explantation: Clinicopathologic Correlation Analysis. Journal of Cataract and Refractive Surgery 36, č. 6 (jún 2010): 970–77. URL <https://doi.org/10.1016/j.jcrs.2009.12.042>
4. Jadidi, K., Mosavi, S.A., Nejat, F., et al.: Intrastromal Corneal Ring Segment Implantation (Keraring 355°) in Patients with Central Keratoconus: 6-Month Follow-Up. Research article. Journal of Ophthalmology, 2015. URL <https://doi.org/10.1155/2015/916385>
5. Piňero, D.P., Alio, J.L.: Intracorneal Ring Segments in Ectatic Corneal Disease – a Review. Clinical & Experimental Ophthalmology 38, č. 2 (01. marec 2010): 154–67. URL < https://doi.org/10.1111/j.1442-9071.2010.02197.x>
6. Ratkay - Traub, I., Ferincz, I.E., Juhasz, T., et al.: First Clinical Results with the Femtosecond Neodynium-Glass Laser in Refractive Surgery. Journal of Refractive Surgery 19, č. 2 (apríl 2003): 94–103. PMID: 12701713
7. Ruckhofer, J., Stoiber, J., Alzner, E., et al.: One Year Results of European Multicenter Study of Intrastromal Corneal Ring Segments. Part 2: Complications, Visual Symptoms, and Patient Satisfaction. Journal of Cataract and Refractive Surgery 27, č. 2 (február 2001): 287–96. PMID: 11226797
8. Strmeňová, E., Vlková, E., Hlinomazová, Z., et al.: Corneal cross-linking – moderná metóda liečby keratokónusu. Česká a slovenská oftalmologie 66, č. 6 (2010): 248-253. URL <http://www.prolekare.cz/pdf?id=33881>
9. Studený, P., Křížová, D., Straňák, Z., et al.: Výsledky implantace plného rohovkového kroužku (Myoring) v léčbě keratokonu. Česká a slovenská oftalmologie 71, č. 2 (2015): 87-91 URL <http://www.prolekare.cz/pdf?id=52078>
10. Wilde, C.L., Naylor, S.G., Varga, Z., et al.: Keraring Implantation Using the Zeiss Visumax Femtosecond Laser in the Management of Patients with Keratoconus. Eye (London, England) 31, č. 6 (jún 2017): 916–23. URL <https://doi.org/10.1038/eye.2017.13>
11. Zare, M.A., Hashemi, H., Salari, M.R., et al.: Intracorneal Ring Segment Implantation for the Management of Keratoconus: Safety and Efficacy. Journal of Cataract and Refractive Surgery 33, č. 11 (november 2007): 1886–91. URL https://doi.org/10.1016/j.jcrs.2007.06.055
Labels
Ophthalmology
Article was published inCzech and Slovak Ophthalmology

2018 Issue 1-
All articles in this issue
- Merkel cell carcinoma of the eyelid and orbit
- Change of tear osmolarity after refractive surgery
- Optic nerve orbital meningioma
- Pachychoroid disease of the macula
- Femtosecond Laser - assisted intrastromal corneal segment implantation - our experience
- Use of ex-press® implant in glaucoma surgery - retrospective study
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Pachychoroid disease of the macula
- Optic nerve orbital meningioma
- Use of ex-press® implant in glaucoma surgery - retrospective study
- Merkel cell carcinoma of the eyelid and orbit
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

