-
Medical journals
- Career
Bifocal bone transport in the treatment of infected nonunion of the tibia - case report
Authors: Radek Veselý; Libor Paša; Vladimír Krass
Authors‘ workplace: Klinika traumatologie Lékařské fakulty Masarykovy Univerzity Brno Úrazová nemocnice v Brně
Published in: Úraz chir. 25., 2017, č.3
Overview
INTRODUCTION:
The rate of infection complications after intramedullary nailing of long bone is 1-4 %. After high energy open fractures is considerably higher.
CASE REPORT:
This is case of 20 – year man with infected nonunion of the tibia following intramedullary nailing of open tibia fracture. We present a series of sequential surgical procedures such as nail removal, debridement of fracture site, stabilisation by external fixation and fibular osteotomy. The final treatment of infected nonunion of the tibia was radical bone resection and reconstruction by bifocal segmental transport using monolateral external fixation. We describe complications of segmental transport such as pin-tract infection and necessity of revision and bone grafting at the docking site. The pacient was healed to full weight bearing after 30 months.
DISCUSSION:
The classic techniques for the treatment of a tibial nonunion associated with chronic osteomyelitis include the resection of the infected and nonviable, avascular bone and soft tissue following reconstructive procedures such as bone transport or grafting.
CONCLUSION:
Bone transport is indicated for segmental bone defects. The treatment of infected tibial nonunion need a series of sequential surgical procedures.
KEY WORDS:
Bifocal bone transport, external fixation, nonunion, bone defect.
INTRODUCTION
Intramedullary nailing is a treatment of choice in patients with diaphyseal tibial fractures. The percentage of infectious complications following intramedullary nailing procedures varies between 1 and 4 per cent [5,12]. Open fractures caused with high-energy injuries are associated with even higher occurrence of infections (4–20 %) [2].
Treatment of infections following intramedullary nailing is difficult, and includes a number of successive surgical procedures. After removal of the nail and debridement of the medullary cavity, it is often necessary to perform a revision of the fractured area and remove necrotic bone fragments. Treatment of infected non-unions is even more demanding. The basic principle of treatment of infected non-unions is eradication of the infection with a radical resection of the infected bone and soft tissues, providing a sufficient cover for the soft tissues using a local, or more frequently free muscle flap, and subsequent reconstruction of the skeleton. The techniques used for management of secondary defects of the skeleton include autologous spongioplasty, callus distraction, or the use of a vascularized bone graft. Spongioplasty is suitable for patients with incomplete bone defects, or in cases of small bone defects. Vascularized bone graft may be used in extreme situations, namely in complex defects [11]. Callus distraction makes treatment of injuries with tissue loss possible, without the need to use bone grafts. Partial steps of this technique include osteotomy and gradual, controlled distraction of the callus using an external fixator or intramedullary nail. The newly formed bone bridges over the appearing defect, is remodelled, and matures into a new bone structure, which is macroscopically and biomechanically identical with the original bone. This technique eliminates the morbidity at the site of graft harvesting, and enables a partial, or even complete management of soft tissue defects [10,11].
Callus distraction may be performed, apart from using an intramedullary nail, also with a circular or unilateral external fixator. Circular external fixator is popular due to its ability to modulate the callus in all directions, including the possibility to correct deviations [7,13]. However, this type of external fixator is less well tolerated by the patients, due to its bulkiness and more complicated postoperative care. A suitable alternative are unilateral external fixators, which enable not only callus modulation in all directions but also a telescopic dynamization of the system, which is important for the period of callus maturing [10].
The aim of this work is to present, on a case report of complicated treatment of an open fracture in a young male, various possibilities of reconstruction procedures of soft tissues and the skeleton, specifically a management of a bone defect with the technique of bifocal segmental transport using an unilateral external fixator.
CASE REPORT
A 20-year-old motorcyclist was hit by a car at the speed of 60 km/h. The fully-conscious patient was transported by ambulance and admitted to the Trauma Hospital Brno, with the diagnoses of concussion, chest contusion, closed fracture of the distal radium on the left side, and open diaphyseal fracture of the right tibia (Fig. 1).
1. Trauma radiograph of open tibial fracture 
2. Infectious complications of intramedullary nailing 
In the middle part of the tibia, there was a 5-cm wound located medially, without denudation of the bone. The extremity periphery was without alteration. After necessary preparation, the patient was transported to the operating theatre. The patient received antibiotic therapy, toilet of the lacerated and contused wound was performed, with subsequent introduction of an unreamed locked tibial nail. All wounds healed per primam intentionem.
Six weeks after the primary surgical procedure, a fistula opened in the distal pole of the wound, with smear serous secretion. Further treatment was on outpatient basis, with local changes of dressings, excochleation and per oral administration of antibiotics. After two months of unsuccessful outpatient treatment, extraction of the nail and debridement of the medullary cavity were indicated, with introduction of lavage and stabilization of the tibia with an external fixator (Fig. 2).
The fistula, including the original wound, was excised, and the newly formed defect in the antero-medial area in the middle third of the tibia was covered with a free sliding flap. Nevertheless, healing was not achieved, not even after a resection osteotomy of the fibula and compression applied at the fracture site (Fig. 3).
3. Antero-posterior projection of the tibia following conversion to external fixator 
On contrary, this procedure resulted in a formation of an infected non-union. The authors decided to manage the non-union with a radical resection of 7 cm of the tibia, together with a radical resection of soft tissues. The defect of soft tissues was managed in cooperation with a plastic surgeon, using a transfer of a free muscle flap from m serratus anterior. The bone defect was treated with administration of a unilateral external fixator, bifocal osteotomy of the tibia, and gradual segmental transport (Figs. 4, 5).
4. Situation after two tibial osteotomies and initiation of the segmental bifocal transport 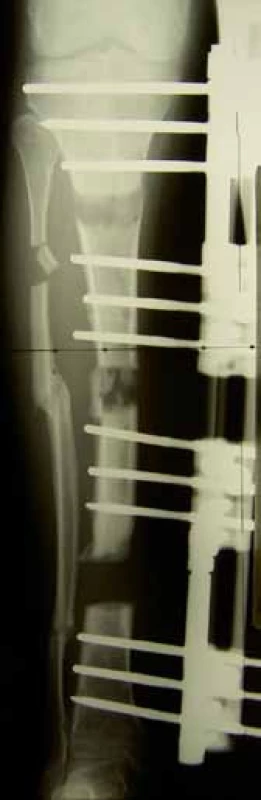
5. Lateral projection, after initiation of the segmental bifocal transport 
The first days of segmental transport were complicated with transient paresthesias, due to which it was necessary to slow down the speed of segmental transport. The paresthesias receded, and the segmental transport was continued until the desired length was achieved, at the speed of 1 mm/24 hours, divided into four turnings. After completion of the transport, we observed an unhealed area at the docking site. An osteotomy of the fibula was performed, with revision of the docking site and spongioplasty. Further course of treatment was uncomplicated. The total period of healing reached 30 months. The patient is capable of full load bearing and walks without any support or prosthetic aid. Movements in the knee and ankle are in full extent. Soft tissues are healed, and peripheral areas are without any neurocirculatory disorders (Figs. 6, 7).
6. Situation after accomplishment of the segmental transport and healing, anteroposterior projection 
7. Situation after healing, lateral projection 
Treatment of infected non-unions of long bones is rather complicated. Although it is often necessary to prepare an individual treatment plan, there exist some common principles of treatment of infected non-unions [3, 6]. First of them is eradication of the infection. This includes a sufficiently radical debridement, with removal of sequesters, loosened implants and foreign bodies. Our strategy is governed by the fact that it is less difficult to replace a bone segment than to treat a persisting infection with retained necroses. It may be difficult to differentiate between a vital and avital bone; that is why highly radical debridement is usually required. The associated radicality of bone resection is justifiable in these cases [8].DISCUSSION
The process of restoration of high-quality cover of soft tissues presents a range of possibilities, from dermoepidermal graft, local and stem flaps, up to microsurgical flaps. It is not possible to expect healing without a quality restoration of the skin cover [1]. For skeletal reconstructions, external fixator is most often used. This will provide sufficient stability. It is possible to use circular or unilateral constructions. In order to perform reconstruction of the bone defect, it is possible to use the techniques of autologous spongioplasty, callus distraction, and vascularized bone graft. After the defect has healed, and the levels of inflammatory markers have dropped, it is possible to perform a conversion to internal osteosynthesis, which improves the comfort of healing and, when correctly indicated, accelerates the healing of the non-union. The use of antibiotics in the treatment of infected non-unions is only adjuvant. Surgical procedure remains the basis of the procedure. Postoperatively, it is advantageous to administer local antibiotics on resorbable carriers.
In our case, callus distraction was realized with a unilateral external fixator. The authors consider using this type of fixation advantageous, due to the possibility of telescopic dynamization of the system, without the need to change the construction. Dynamization is important in the stage of callus maturing [9]. The reason why we performed two osteotomies with subsequent segmental transport was to shorten the period of healing. Using this treatment procedure was carefully considered in a young sportsman with a good condition of soft tissues over the osteotomy sites. In the expert literature, there are certain discussions regarding the placement of osteotomy. In our case, we did not observe any complications in the course of formation and maturation of muscles after osteotomy. After all, even large studies did not prove any statistically significant difference in the placement of osteotomy [9]. The course of callus distraction technique is associated with a high occurrence of complications. The most frequent one is pin-tract infection. Also in our patient it was necessary to perform two replacements of the nail in the course of treatment due to pin-tract infection. According to our experience, the incidence of this complication may be reduced by using 6 mm Schanz nails, coated with hydroxyapatite [10]. Another complication is the prolonged treatment at the docking site during the performed segmental transport [4]. Also in our case, we managed this complication with a revision of the docking site, with subsequent spongioplasty and change of the fixator construction with compression.
CONCLUSION
Treatment of infected non-unions of long bones requires an individual plan. It is necessary to assess the patient in a complex way. No only the local condition is important, it is also necessary to evaluate psychological and social factors. It is important to perform a radical resection of the tissues affected by infection, even at the price of a bone defect. This is manageable with callus distraction technique, using a unilateral external fixator. Segmental bone transport, together with a free transfer of a muscle flap, provides good outcomes in the treatment of these complicated cases in traumatology.
Sources
1. GLASS, G., PEARSE, M., NANCHACHAL, J. Improving lower limb salvage following fractures with vascular injury: a systematic review and new management algorithm. J Plast Reconstr Anesthet Surg. 2009, 62, 571–579. ISSN 1748-6815
2. KOUZELIS, A., KOUREA, H., MEGAS, P. et al. Does graded reaming affect the composition of reaming products in intramedullary nailing of long bones? Orthopedics. 2004, 27, 852–856. ISSN 0147-7447
3. LASANIANOS, NG., KANARAKIS, NK., GIANNOUDIS, PV. Current management og long bone large segmental defects. Orthop Trauma. 2010, 24,149–163. ISSN 0890-5339
4. LAVINI, F., DALLOCA, C., BARTOLOZZI, P. Bone transport and compression - distraction in the treatment of bone loss of the lower limbs. Injury. 2010, 41,1191–1195. ISSN 0020-1383
5. MALIK, MH., HARWOOD, P., DIGGLE, P. et al. Factors affecting rates of infection and nonunion in intramedullary nailing. J Bone Jt Surg. 2004, 86-B, 556–560. ISSN 0021-9355
6. MEGAS, P., SARIDIS, A., KOUZELIS, A. et al. The treatment of infected nonunion of the tibia following intramedullary nailing by the Ilizarov method. Injury. 2010, 41, 294–299. ISSN 0020-1383
7. MORASIEWICZ, L., ORZECHOWSKI, W., KULEJ, M. et al. The results of treatment of bone defects and non-union within the femoral shaft with shortening of femur using Ilizarov method. Ortop Traumatol Rehabil. 2007, 9, 366–376. ISSN 2210-4917
8. SALA, F., THABET, A., CASTELLI, F. et al. Bone transport for postinfectious segmental tibial bone defects with a combined Ilizarov/ Taylor spatial frame technique. J Orthop Trauma. 2011, 25, 162–168. ISSN 0890-5339
9. VESELÝ, R., SUCHOMEL, R., TRÁVNÍK, J. Léčení otevřené zlomeniny bérce typu IIIB opakovaným segmentálním transportem. Ortopedie. 2016, 10, 43–46. ISSN 1802-1727
10. VESELÝ, R., PROCHÁZKA, V. Kalusdistrakce v léčení poúrazových defektů femuru a tibie. Acta Chir Orthop Traumatol Cech. 2016, 83, 6, 388–392. ISSN 0001-5415
11. WEI, FC., EL-GAMMAL, TA. LIN, C., UENG, WN. Free fibula osteoseptocutaneous graft for reconstruction of segmental femoral shaft defects. J Trauma. 1997, 43,784–792. ISSN 2163-0755
12. WENDSCHE, P., VESELÝ, R. et al. Traumatologie. Galén: Praha, 2015. 344 s. ISBN 978-80-7492-211-4.
13. WINGUIST, RA., HANSEN, ST., CLAWSON, DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Jt Surg. 2001, 83-A, 1984. ISSN 0021-9355
Labels
Surgery Traumatology Trauma surgery
Article was published inTrauma Surgery

2017 Issue 3-
All articles in this issue
- Therapeutic algorithm in a patient with open tibial fracture with extensive laceration of the soft tissue coverage – case report contribution to the discussion about limb salvage
- Bifocal bone transport in the treatment of infected nonunion of the tibia - case report
- Osteosynthesis of dislocated calcaneal fractures at our centre using the intramedullary C-Nail
- The Treatment of Comminutive Intraarticular Calcaneal Fractures by External Fixation
- Trauma Surgery
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- The Treatment of Comminutive Intraarticular Calcaneal Fractures by External Fixation
- Therapeutic algorithm in a patient with open tibial fracture with extensive laceration of the soft tissue coverage – case report contribution to the discussion about limb salvage
- Osteosynthesis of dislocated calcaneal fractures at our centre using the intramedullary C-Nail
- Bifocal bone transport in the treatment of infected nonunion of the tibia - case report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

