-
Medical journals
- Career
Spinal epidural abscess – a rare complication of Crohn´s disease: case report
Authors: Karolina Poredska 1; Vladimír Zbořil 1; Lucie Prokopová 1; Lenka Kučerová 1; Milan Dastych 1; Svatopluk Richter 2; Petra Praksová 3; Jiří Dolina 1; Lumír Kunovský 1,4
Authors‘ workplace: Department of Gastroenterology and Internal Medicine, Faculty of Medicine, Masaryk University, and University Hospital Brno, Czech Republic 1; Department of Radiology and Nuclear Medicine, Faculty of Medicine, Masaryk University, and University Hospital Brno, Czech Republic 2; Department of Neurology, Faculty of Medicine, Masaryk University, and University Hospital Brno, Czech Republic 3; Department of Surgery, Faculty of Medicine, Masaryk University, and University Hospital Brno, Czech Republic 4
Published in: Vnitř Lék 2019; 65(11): 712-714
Category: Case reports
Overview
Spinal epidural abscess (SEA) is a rare disease that occurs mainly in immunocompromised patients after spinal surgery or spinal trauma and can lead to a severe neurological deficit or even death if diagnosed too late. However, cases of SEA have also been reported in patients with fistulising Crohn´s disease (CD). We present a case of a young patient with CD and a history of relapsing perianal disease followed by a complication of SEA in the thoracic spine. In close cooperation with the orthopedists and the neurologists, the gastroenterologists have successfully treated the SEA in this patient, allowing her to return back to biological treatment for CD.
Keywords:
biological treatment – Crohn´s disease – perianal fistulas – spinal epidural abscess
Introduction
Spinal epidural abscess (SEA) is a rare disease with incidence of 2–5/10 000 hospitalisations, which is however growing probably due to aging of the population, increases in the numbers of immunocompromised patients and spinal surgeries and improvements in the quality of radiological diagnostics [1,2]. Unfortunately, the mortality of SEA is up to 15 % if diagnosed too late. The location of SEA is mainly the lumbar spine and the etiology is mostly a hematogenous spread from a distant septic focus (such as skin furuncles, dental or tonsillar abscess, pneumonia, renal or psoas abscess) but it can also be direct after a trauma or even iatrogenic [1–3]. Typically, the causative organism cultivated from SEA is Staphylococcus aureus. The main presenting symptoms are back pain, fever and a variable degree of neurological deficit [2,3]. SEA is rare in patients with inflammatory bowel disease (IBD), with only a few cases reported – mostly in patients with fistulising Crohn´s disease (CD); however, a case of SEA has also been reported in a patient with ulcerative colitis after proctocolectomy with ileal pouche-anal anastomosis [4].
Case report
A 24-year-old woman was followed up at our department for CD diagnosed at the age of 14 and located in the colon and perianal region. She had been treated with adalimumab biologics already for 2 years. This therapy was discontinued in the third trimester of her first gravidity. During the pregnancy she was treated for relapsing perianal abscess with a need of drainage, where the last drainage was performed 14 days before the delivery. Eventually, she delivered a healthy child by a Caesarean section in general anesthesia. The woman´s family had a history of Bechterev disease. Three months after the delivery, she was referred to our department by her general practitioner for lower back pain and fever lasting for 3 weeks.
On examination she was asthenic, slightly hypotensive, tachycardic (with the heart rate of 120 beats per minute), with no apparent neurological deficit, her abdomen was not tender, with only mildly positive tappotement bilaterally. Rectal examination showed scars after healed abscesses but no signs of active disease.
Within the wide differential diagnosis, the following investigations were performed. In terms of laboratory findings, the C-reactive protein (115 mg/l) and border microcytic anaemia were identified; on the other hand, the urinary and stool samples did not show any pathology, and neither did the hemoculters, nor the X-ray and ultrasound of the abdomen, nor the X-ray of the lungs and thoracic and lumbar spine, nor the gynecological examination. Additionally, the neurologist concluded that there were slightly positive upper meningeal symptoms and therefore recommended an acute magnetic resonance imaging (MRI) of the spine to exclude an epidural abscess or other source of infection. The MRI (fig. 1a, fig. 1b, fig. 2) showed epidural abscess formation in the thoracic spine compressing the dural sac but not the spinal cord.
1. MRI – the SEA in thoracic spine, sagital scan. Department of Radiology, and Nuclear Medicine 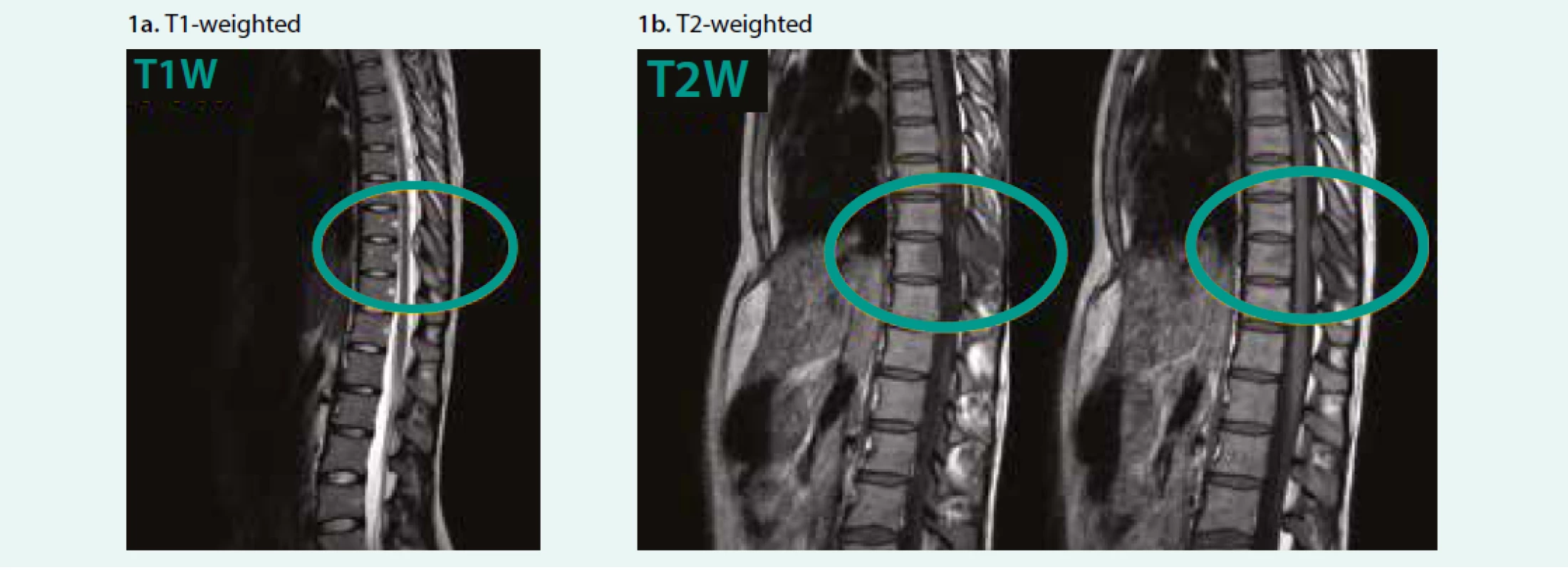
2. MRI – the SEA in thoracic spine, transversal scan. Department of Radiology, and Nuclear Medicine 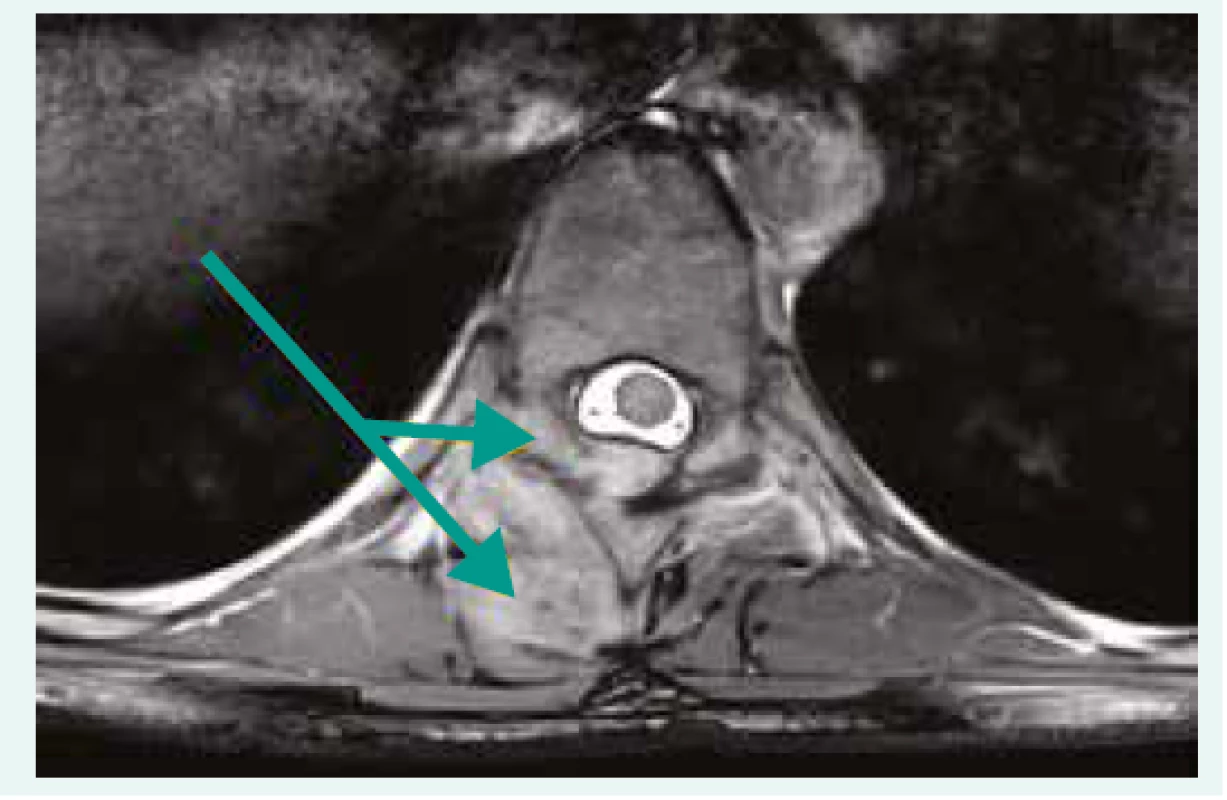
Given the mild neurological deterioration and quite favourable MRI findings, the patient was treated conservatively with antibiotics (oxacillin and cefotaxim) for two weeks, and subsequently with co-trimoxazol and rifampicin for two months. She was allowed to move with a spinal corset. After three months, she was completely asymptomatic, finished the antibiotic treatment and the control MRI of the spine (Fig. 3, 4) showed regression of the abscess. Considering the favorable results, the patient could return back to the biological treatment needed for CD.
3. Control MRI after 3 months showing regression of SEA, sagital scan. Department of Radiology, and Nuclear Medicine 
4. Control MRI after 3 months showing regression of SEA, transversal scan. Department of Radiology, and Nuclear Medicine 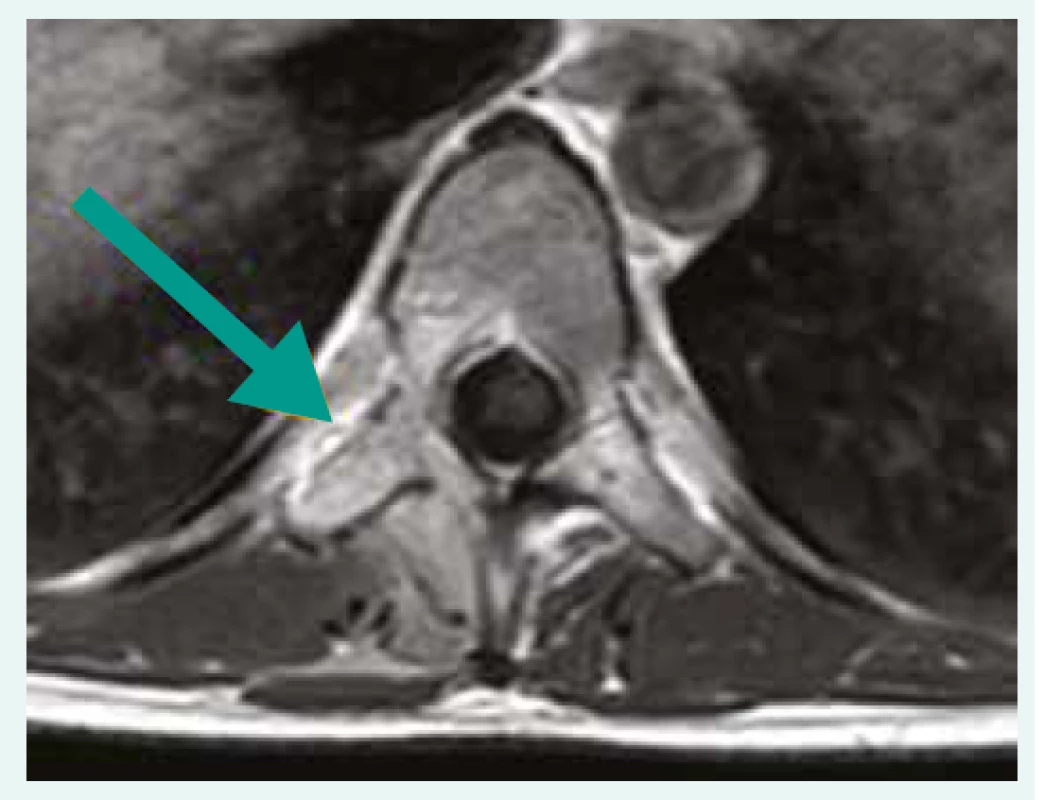
Discussion
SEA is a rare condition that can be fatal if underdiagnosed [1–3]. The most important factor in the therapeutic decision is the level and progression of neurological deterioration that can vary from simple back pain to signs of meningism, motor, sensor or sphincter dysfunction and even paraparesis [5]. The final diagnose is made by MRI. The findings then serve as a basis for therapy, which can be either conservative or surgical. As to the possibility of conservative therapy, it is possible to use antibiotics with a good penetration to the spine in neurologically stabilized patients. In contrast, in patients whose neurological deficit is worsening quickly, it is necessary to perform surgical decompression of the spine, sometimes even an urgent one. The most common procedure performed is a dorsal approach laminectomy [5].
Only a few cases of SEA in patients with CD have been reported, in which the etiology of SEA was mostly widespread from the perianal fistulas or abscess [4]. Fistulas can appear in patients with CD in 17–50 % of cases, with a recurrence in 1/3 of patients, moreover the cumulative incidence of developing a fistula in CD patients is approximately 20 % after 1 year and 50 % after 20 years [6–8]. Our patient was treated several times for perianal abscess during her pregnancy; however, when she was admitted for SEA, the perianal region was already healed (according to the MRI findings of the pelvis). The patients with CD and SEA reported in the literature were for their CD mostly treated with steroids or sulfasalazine whereas our patient was receiving with biological treatment, namely adalimumab, which can have an adverse effect of opportunistic infection [9–11]. A majority of patients with CD complicated by SEA had to be treated surgically (laminectomy); nonetheless, our patient was successfully treated conservatively with antibiotics [9,11]. Furthermore, in some surgically treated patients, early recurrence of SEA has been reported. Fortunately, this has not happened in our case and one year later, the patient shows no signs of recurrence of SEA. Moreover, she is able to continue with her biological treatment for CD.
Conclusion
We present a rare case of SEA of the thoracic spine in a 24-year-old woman as a complication of perianal CD that was successfully treated conservatively with antibiotics.
Supported by Ministry of Health, Czech Republic – conceptual development of research organization (FNBr, 65269705).
Doručeno do redakce 3. 9. 2018
Přijato po recenzi 3. 12. 2018
Lumír Kunovský, M.D., PhD.
Department of Gastroenterology and Internal Medicine, Faculty of Medicine, Masaryk University, and University Hospital Brno, Czech Republic
Sources
- 28. Dostupné z DOI: Dostupné z DOI: <http://dx.doi.org/10.1016/j.wneu.2016.05.074>.
- Schwartz D, Loftus EV, Tremaine W et al. The natural history of fistulizing Crohn‘s disease in Olmsted County, Minnesota. Gastroenterology 2002; 122(4): 875–880. Dostupné z DOI: <http://dx.doi.org/10.1053/gast.2002.32362>.
- Gesce K, Khanna R, Stoker J et al. Fistulizing Crohn’s disease: Diagnosis and management. United European Gastroenterol J 2013; 1(3): 206–213. Dostupné z DOI: <http://dx.doi.org/10.1177/2050640613487194>.
- Kunovsky L, Hemmelova B, Kala Z et al. Crohn disease and pregnancy: a case report of an acute abdomen. Int J Colorectal Dis 2016; 31(8): 1493–1494. Dostupné z DOI: <http://dx.doi.org/10.1007/s00384–016–2554–1>.
- Smith C, Kavar B. Extensive spinal epidural abscess as a complication of Crohn’s disease. J Clin Neurosci 2010; 17(1): 144–146. Dostupné z DOI: <http://dx.doi.org/10.1016/j.jocn.2009.02.038>.
- Kunovsky L, Kala Z, Marek F et al. The role of the NOD2/CARD15 gene in surgical treatment prediction in patients with Crohn‘s disease. Int J Colorectal Dis 2019; 34(2): 347–351. Dostupné z DOI: <http://dx.doi.org/10.1007/s00384–018–3122–7>.
- Brown CJ, Jaffer H, Jafer N et al. Spinal epidural abscess – a rare complication of inflammatory bowel disease. Can J Gastroenterol 2008; 22(2): 177–180. Dostupné z DOI: <http://dx.doi.org/10.1155/2008/893757>.
Labels
Diabetology Endocrinology Internal medicine
Article was published inInternal Medicine

2019 Issue 11-
All articles in this issue
- Functional gastrointestinal disorders and pain
- May warfarin prevent cancer?
- Immunodeficiency in the differential diagnosis of interstitial lung diseases
- Why rapid achievement of goal blood pressure is important in the treatment of arterial hypertension
- Interferon-alpha in the treatment of myeloproliferative diseases
- Pancytopenia, panhypopituitarism and liver cirrhosis: analysis of a difficult clinical case
- Vitamin D deficiency and its health effects
-
Sekundární prevence ischemické choroby srdeční a chorob periferních tepen kombinací antiagregační a antikoagulační léčby
Odborné stanovisko České kardiologické společnosti, České internistické společnosti ČLS J.E. Purkyně a České angiologické společnosti ČLS J.E. Purkyně k výsledkům studie COMPASS - Odešel profesor Ivo Dvořák
- Primář Jiří Spáčil oslavil 80. narozeniny
- Profesor Jan Petrášek slaví devadesáté narozeniny
- The myths and facts about arterial hypertension: do we really know everything about arterial hypertension?
- Spinal epidural abscess – a rare complication of Crohn´s disease: case report
- Internal Medicine
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Functional gastrointestinal disorders and pain
- Interferon-alpha in the treatment of myeloproliferative diseases
- Vitamin D deficiency and its health effects
- Immunodeficiency in the differential diagnosis of interstitial lung diseases
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

