-
Medical journals
- Career
Screening Family and Sexual Contacts of HBsAg+ Persons in the Pilsen Region
Authors: Pazdiora Petr 1,2; Böhmová Zdenka 2; Kubátová Anna 2; Menclová Irena 2; Morávková Ivana 2; Průchová Jitka 2; Přechová Marie 2; Spáčilová Marika 2
Authors‘ workplace: Department of Epidemiology, Charles University Faculty Hospital, Pilsen 1; Regional Hygiene Centre of the Pilsen Region 2
Published in: Epidemiol. Mikrobiol. Imunol. 61, 2012, č. 3, s. 51-57
Overview
The aim of the study:
To detect HBsAg-positive persons and to offer their family and sexual contacts, after screening for viral hepatitis B (VHB) markers, free vaccination against the infection.Material and Methods:
In collaboration with laboratories, all persons with confirmed HBsAg in the Pilsen Region (549,618 population) were prospectively detected. From these persons, the following data were collected: reason for examination, clinical diagnosis, and ethnicity/nationality. Their family and sexual contacts were screened for serologic markers (HBsAg, anti-HBc, anti-HBs) and vaccinated.Results:
Between 1997–2005, 1,053 HBsAg+ persons were routinely detected by the laboratories in the Pilsen Region. The average age of the infected persons was 41.7 years (range 0–90 years). At the time of the detection, 63.4% of the HBsAg positives were clinically “healthy” carriers. Within the monitored period there was a considerable increase in the HBsAg positivity rate among immigrants (particularly from Vietnam). Of 908 family and sexual contacts, 18% were positive for hepatitis B markers. The highest seropositivity rates (33.9% and 27.7%) were found in siblings and parents, respectively, of the HBsAg+ persons. So far 77.5% of the susceptible contacts have used the opportunity for free vaccination.Conclusion:
The study has proven the importance of detecting HBsAg carriers and vaccinating their contacts. Special attention should be paid to immigrant families, particularly from Asia. Consistent vaccination of family and sexual contacts of HBsAg+ persons can contribute to a more rapid elimination of hepatitis B in the Czech Republic.Key words:
hepatitis B – intrafamilial transmission – vaccination – ethnic group – preventionINTRODUCTION
In the past, considerable attention has been paid to the spreading of hepatitis B in families, particularly in the areas with endemic incidence of this infection [1–3]. The results of a number of studies confirmed not only the significance of sexual transmission of the infection, but also a significant proportion of horizontal transmissions through contaminated objects either by a parenteral route or through contamination of mucous membranes. In most countries children and selected risk groups are being vaccinated against hepatitis B. Examining and vaccination of family and sexual contacts of the HBsAg positive is rarely regulated by law but usually purely recommended, therefore, official data in this matter are not available.
Vaccination against hepatitis B of medical staff, dialyzed persons and children born to HBsAg positive mothers has been performed in the Czech Republic since the 1980s. In 2001 regular vaccination against this infection was introduced for infants and children at the age of 12, the coverage of vaccination in the two age groups ranges between 97.6–99.7%, resp. 96.3–99.4% [non-published data of the Regional Hygiene Centre, Pilsen]. At the same time free vaccination for the family and sexual contacts of HBsAg positive carriers and patients were introduced. Even before the introduction of this legislation, the Regional Hygiene Centre decided in 1997 to improve measures in centres of contagion by offering free vaccination to the closest contacts of HBsAg persons. Our 9-year experience shows the significance of this measure, as well as the changes that occurred within a short period of time.
MATERIAL AND METHODS
Between 1997–2005 copies of the results of this marker’s positivity were obtained from laboratories diagnosing routinely HBsAg in the Pilsen Region. Rarely, HBsAg positivity was diagnosed in inhabitants of the region by laboratories in other regions in the Czech Republic. The diagnosis is performed with the ELISA test from various manufacturers. All laboratories are subject to quality control checks at least once a year (the checks are performed by the National Institute of Public Health in Prague). After obtaining the result, the addresses of positive persons were obtained at the appropriate centre (“index case”), together with the reason for their examination, diagnosis of possible hepatopathy and ethnic group (nationality). Positive persons were informed by the employees of the hygiene services about the mechanisms of infection transmission, the possibility of examining family and sexual contacts and of free vaccination. If the residence of these people was outside the Pilsen Region (549,618 citizens), the data were transferred to the particular out-of-region centre of hygiene services. HBsAg+ people who were in a psychiatric hospital (1,130 beds), social care institutions (5,143 beds), and a prison were not contacted. In cases of repeat detection of positivity the infected persons were not further informed.
Sampling for serologic markers for hepatitis virus type B (HBsAg, anti-HBc, anti-HBs) in the family and sexual contacts of HBsAg+ persons was performed by the employees of the Regional Hygiene Centre of the Pilsen Region or by particular general practitioners on legislative basis. In the sampled persons their relationship to the “index case” was determined, together with their membership of a particular ethnic or nationality group, and also the history of vaccination against hepatitis B (the people with the history of vaccination were not laboratory examined). Those people who had a positive result for at least one of the markers mentioned above were considered seropositive (anti-HBs antibodies themselves were only considered seropositive in persons who had not been vaccinated). The others, apart from the vaccinated ones, were considered susceptible to the infection by hepatitis B virus, and when they had been given the laboratory result, they were offered free vaccination with Engerix vaccine. The vaccination was performed by the employees of the hygiene services or by appropriate general practitioners.
Documentation about all the people included in the study (“index case” and their contacts) was done with the EPI-INFO program, v. 6.04d, and in this program statistical evaluation with the χ2 test was also performed.
The Research protocol of this study was reviewed and approved by the Ethics Committee of the Charles University Hospital, Pilsen, and it conforms to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh 2000) and was conducted according to the International Conference on Harmonisation Guidelines for Good Clinical Practice (ICH-GCP) and local and national requirements.
RESULTS
Between 1997–2005 HBsAg positivity was routinely detected in 1,053 persons (587 men and 466 women), out of whom 966 persons were inhabitants of the Pilsen Region. The average age of the positive persons (“index cases”) was 41.7 years (0–90 years), in men it was 41.3 years (0–87), in women 42.3 years (0–90 years). Out of the total number of detected persons 326 were examined during hospitalization, i. e. 31.0%. Table 1 and Figure 1 show the age breakdown and group membership according to ethnicity (nationality). Between 1997–2000, there were 27 immigrants detected among 532 HBsAg+ persons, i. e. 5.1%. Between 2001–2005 there were already 112 immigrants among 521 detected persons (21.5%). The difference is statistically highly significant (p = 0.0000; χ2 = 49.44).
1. Age distribution of HBsAg+ persons (index cases) (Pilsen Region, 1997-2005) Tabulka 1. Věkové rozložení HBsAg+ osob (indexových případů) (Plzeňský kraj, 1997–2005) 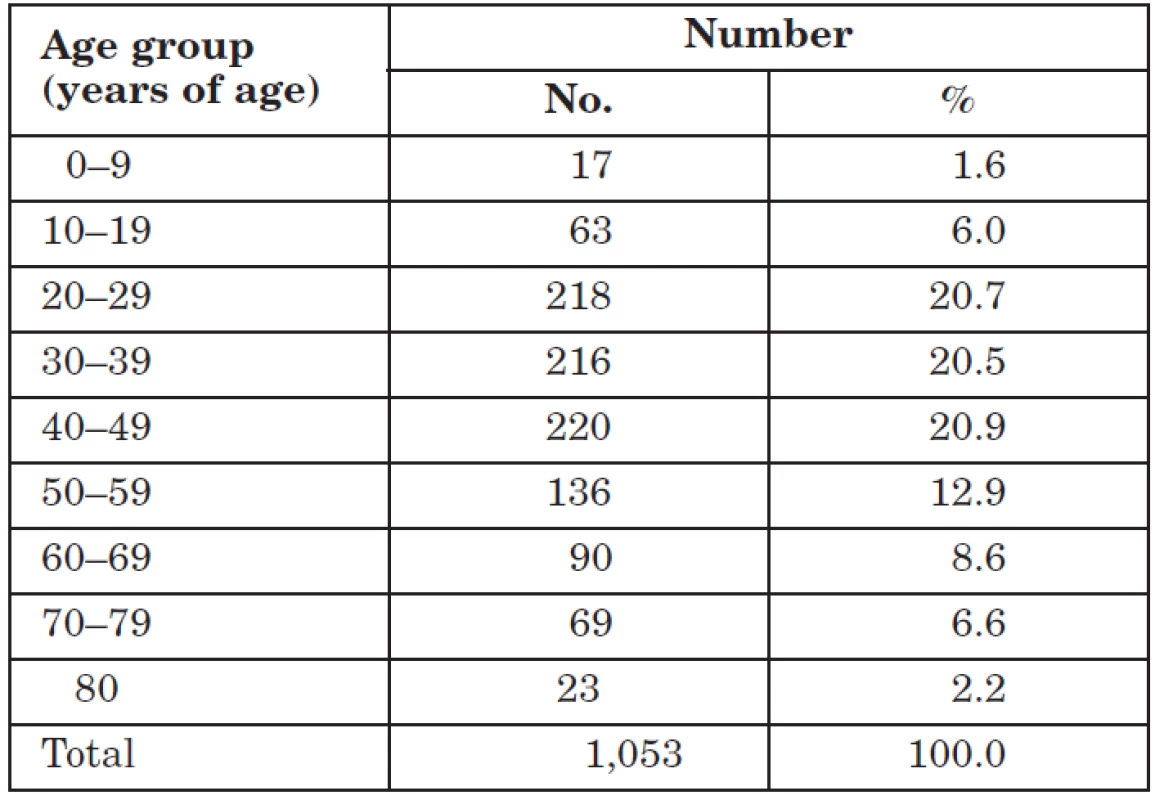
Figure. 1 Distribution of HBsAg+ persons by ethnic/nationality group (Pilsen Region, 1997–2005) Obr. 1. Rozložení HBsAg+ osob podle etnických/národnostních skupin (Plzeňský kraj, 1997–2005) 
The most common reason for HBsAg examination was screening – mostly in-patients, pregnant women, and blood donors (460times). Figure 2 summarises clinical diagnoses at the time of HBsAg positivity. Out of 1,053 HBsAg+ persons 868 were contacted again. Among their family and sexual contacts 1,017 persons were detected – 469 men and 548 women, average age 27.1 (0–81) or 29.6 (0–89).
Figure 2. Clinical diagnosis in HBsAg+ persons (Pilsen Region, 1997–2005) Obr. 2. Klinická diagnóza u HBsAg+ osob (Plzeňský kraj, 1997–2005) 
From individual families 0–13 persons turned up for the examination. Among those detected 53 individuals had already been vaccinated against hepatitis B (5.2%). In 55 out of 964 examined family and sexual contacts (5.7%) HBsAg positivity was detected, and in 161 out of 896 persons (18.0%) anti-HBc was detected (Table 2). Out of the total number of 1,017 family and sexual contacts, 908 were fully (HBsAg, anti-HBc or anti-HBs) examined, and of these 163 persons (18.0%) manifested signs of present or past hepatitis B infection. 12.7% of Czechs, 50.0% of Roma, 52.8% of Vietnamese and 34.2% of immigrants from other countries were suffering from the infection. These persons had not been vaccinated. The presence of serologic markers with reference to family relationship and nationality is summarized in Table 3. Positivity was detected in 22.2% of sexual partners and in 16.3% of other contacts. By June 30th 2007, we had administered 3 doses of Engerix to 621 persons out of 801 susceptible or completely unexamined and previously unvaccinated persons (77.5%).
2. Serologic HB markers in family and sexual contacts of HBsAg+ persons by age group (Pilsen Region, 1997–2005) Tabulka 2. Výskyt sérologických markerů HB u rodinných a sexuálních kontaktů HBsAg+ osob v jednotlivých věkových skupinách (Plzeňský kraj, 1997–2005) 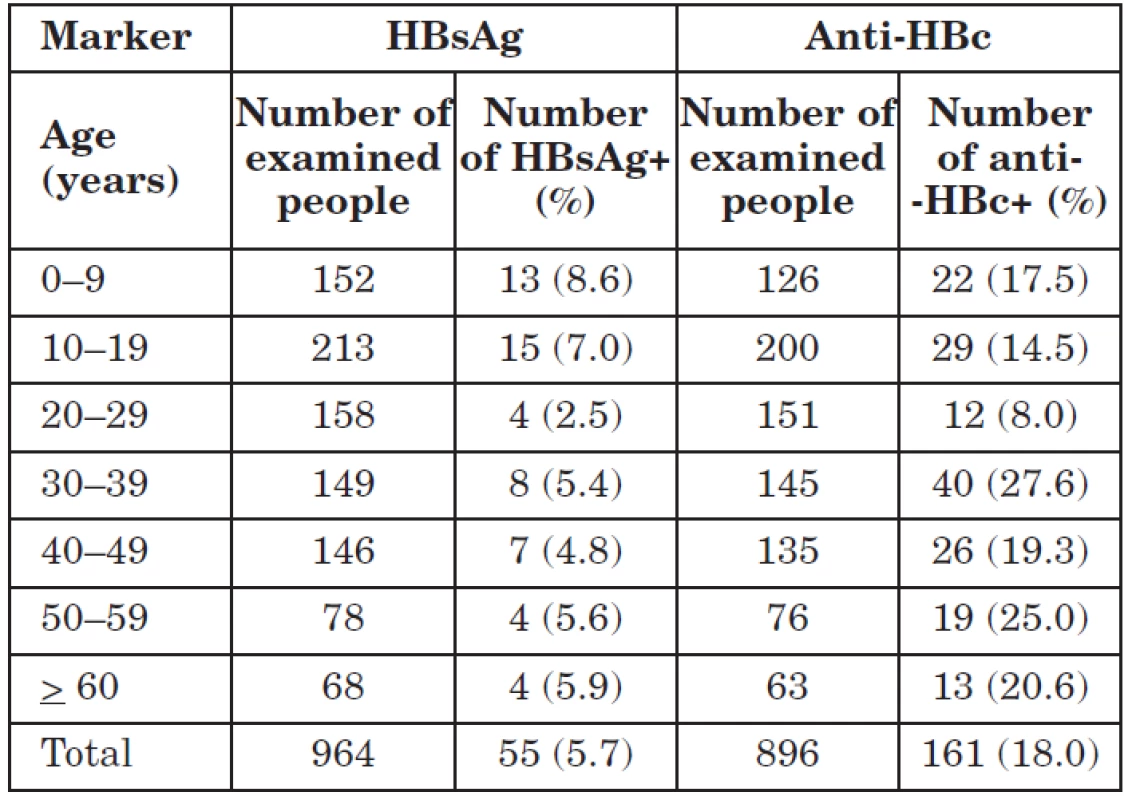
3. Table 3. Seropositivity in contacts of HBsAg+ persons by type of relative (Pilsen Region, 1997–2005) Tabulka 3. Výskyt séropozitivity u kontaktů HBsAg+ osob podle příbuzenského vztahu (Plzeňský kraj, 1997–2005) 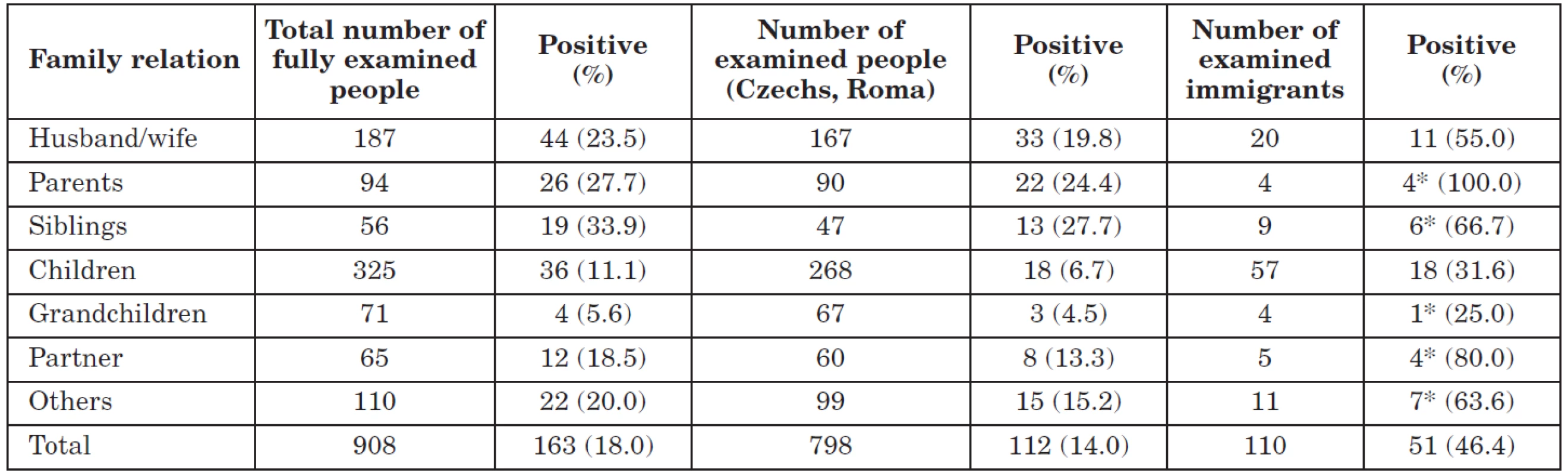
*(%) with the number of < 20 persons screened *(%) při počtu < 20 vyšetřovaných osob DISCUSSION
Nine years of experience with the improvement of targeted preventive activity in the environment of HBsAg positive persons or in the centre of an acute disease confirmed that with good collaboration between laboratory, clinical and epidemiology specialists it is also possible to contribute to a relatively rapid elimination of hepatitis B in the Czech Republic. So far, the vaccination of medical staff, persons included in chronic dialysis programs and children born to HBsAg positive mothers, has fulfilled its purpose. The recently introduced routine vaccination of children has also had a positive effect. Before the start of study, in 1996, morbidity of acute hepatitis B in the Czech Republic was reported to be 6.2/100,000 inhabitants, and in the Pilsen Region 4.1/100,000 inhabitants; in the end of study, in 2005, 3.4, resp. 2,7/100,000 inhabitants. Apart from decisive non-specific preventive measures, thanks to vaccination there has been a considerable reduction in professional infections, and observing asepsis, using disposable equipment and virucide disinfectant means has also had a positive effect on the incidence of nosocomial infections. The introduction of vaccination in children probably reduced the risk of the source of long-term carrier and chronic manifestation of the infection. The number of pregnant HBsAg+ women has diminished in recent years, and at present Vietnamese and Roma women constitute a significant proportion of them in the Pilsen Region (29.8 or 8.8%). Unfortunately, it turns out that not all pregnant women are repeatedly examined for HBsAg during pregnancy.
A certain disadvantage of selective vaccination is the fact that it affects only a particular, small section of the population. According to some authors success can be achieved in countries with a low incidence of contagion by using only selective vaccination programs [4]. In the Czech Republic, too, most hepatitis B infections occurred in a number of risk groups in the minority population, and so the strategy of vaccination reflected this situation. Thanks to non-specific and specific measures, particularly in health care, but also through the influence of socio-economic transformation, a number of changes have happened. Total numbers affected by the disease have reduced, maximum specific morbidity has moved to the lower age range, and infections connected with work or treatment in medical institutions represent only a minority of all diseases. The number of HBsAg positive persons in the population has also decreased considerably. At present it is estimated that in the whole of the Czech Republic there are about 60,000 HBsAg carriers [5]. Of these a certain percentage represents a potential source of infection in view of current detection of HBsAg. The prevalence of this marker is very different in the individual subpopulation of HBsAg carriers [6]. It is therefore desirable to reach as quickly as possible the persons who are at risk through contact with these people and in their case to try to use more intensive and effective preventive measures. Because of present prevailing modes of transmission, these people are in particular sexual partners and drug addicts [7, 8]. The proportion of hepatitis B as a sexually transmitted infection and a parenteral infection spreading outside the medical institution, with current reductions in nosocomial and professional transfer, is on the increase both in the Czech Republic and abroad [9]. Our results confirmed that sexual partners are infected in approximately 22% of cases. Some of these were probably also the first infected person in the centre of contagion. During long-term contact with an HBsAg carrier it is only a question of time before the infection is transmitted to the partner or a family member. That is why it is desirable that the doctor who first detects HBsAg positivity should inform the infected person not only about his/her further clinical prospects, but also about the possibilities of non-specific and specific prevention for his/her closest contacts. A number of detected persons complained, probably correctly, that in the past, both on detection of HBsAg and during their disease, nobody informed them about the risk of sexual or other transmission to other persons.
Most long-term carriers or their contacts were not offered this effective, although then not cost--free, specific measure after the introduction of vaccination. After the introduction of free vaccination for family and sexual contacts of HBsAg+ persons the situation changed, but an active approach by epidemiologists in hygiene centres remains essential. They not only collect information about laboratory results, but also distribute vaccine paid for by the state. Our results also show that even free vaccination does not attract all persons endangered through direct contact with a detected carrier. The risk of horizontal transmission by a non-sexual route, however, is still relevant. Infection spreading through blood, saliva and so on happens mainly through not observing basic rules of hygiene in the immediate environment of infected persons. The prevalence of infected persons close to the carrier or acutely sick people is several times higher than in the normal Czech population. The latest country serological overview from 2001 demonstrated HBsAg in 0.6% and anti-HBc in 5.6% of the examined persons [5]. The different distribution of these markers according to age, as we demonstrated, shows that hepatitis B transmission in families has totally different rules than in the normal population. In methodologically similar European studies, the prevalence of markers for this infection in family members of HBsAg positive persons fluctuates between 15–39% [10–14]. The high proportion of parents and siblings with infection markers undoubtedly testifies to early intrafamilial transmission in the past, and up-to-date studies from other countries also confirm a higher prevalence of markers in siblings and parents [13–19]. The risk of further spreading exists even in families where only the father is positive [20–22]. In this connection it is important to remember that the interruption of vertical transmission of the infection in Czech families could only recently be achieved, i. e. in 1989 with the introduction of vaccination for newborn babies from HBsAg positive mothers. This interruption did not happen in immigrants from the former Soviet Union and particularly from Vietnam, but the numbers of these immigrants in the Czech Republic have been growing in recent years (according to police data there are more than 70,000 Ukrainians and 30,000 Vietnamese living in the Czech Republic). Since Vietnam belongs to the zone with a high endemic incidence of hepatitis B and vaccination of children started there only in 2003, we have to expect considerable prevalence of the infection markers, particularly in persons not born in the Czech Republic, as well as a significant number of infected individuals in the children’s age groups. According to American data, serologic markers were found in 83.3% of examined Vietnamese immigrants, and 14% were HBsAg carriers [23, 24]. Experience from the USA confirmed that the population of Vietnamese immigrants does not have a basic knowledge about how the infection is spread and about possible modes of prevention [25]. A similar situation can also be expected in immigrants from other countries. The spreading of the infection in their communities thus continues even after their relocation. It is therefore necessary to ensure medical education among them, as well as to inform doctors who come into contact with them about their high rate of contamination with hepatitis B and also other infections (parasitic contagions, tuberculosis). The only possible targeted measure is a more frequent assessment of the infection markers and rapid additional vaccination of the immigrants by appropriate general practitioners. At the same time, it is necessary also to target grown up siblings and parents of the infected persons [13, 15–17, 26].
Horizontal transmission is described in the literature particularly in developing countries of Africa, Asia, and South America [2, 3,15–20, 22, 26–31]. This transmission is more common than the sexual transmission which is prevalent in the developed countries of Europe and North America. Although conditions and the epidemiological situation of these countries vary considerably, it is possible (on the basis of serologic markers prevalence) to estimate this infection after migration, particularly of Asians to central Europe. The differences between individual ethnic or nationality groups are considerable [1, 30].
At present, making contact-dispensarization with HBsAg positive persons is not sufficient in the Czech Republic. Only a small proportion of infected persons obtains the care of hepatic or gastroenterological centres. The high ratio of so called healthy carriers is undoubtedly a reflection of a low application of other available diagnosing methods or the orientation diagnosis during screening examinations of hospitalized persons, pregnant women, blood donors or prisoners. Their further monitoring is important for early identification of chronic conditions and their treatment. On the other hand, during our study we detected a relatively high number of persons with a previously confirmed diagnosis of chronic liver disease. With the gradual decrease in the incidence of hepatitis B in this country these chronic consequences should also decrease.
CONCLUSIONS
During our study we partially mapped the current distribution of HBsAg carriers in the Pilsen Region, the possibilities for their detection and their present clinical condition. We also managed to estimate what collaboration we can expect in the families of these persons in taking individual preventive measures. The high percentage of vaccinated persons is undoubtedly a result of organized free vaccination. It is clear that the usual passive way of detecting HBsAg carriers, in spite of the absence of new infections, does not allow us to detect all positive individualistic in a realistic time. On the other hand, it is obvious that through a short-term targeted measure, i. e. by screening the general population or its higher-risks groups, it would be possible to detect a considerable number of carriers in the Czech Republic and thus influence with specific measures their closest (family and sexual) contacts in all age groups. More attention needs to be paid to immigrant families particularly from Asia. Consistent vaccination of family and sexual contacts of HBsAg+ persons can contribute to a more rapid elimination of hepatitis B in the Czech Republic.
Acknowledgements
Our thanks go to all employees of all collaborating laboratories and head-attending doctors who were included in the study.
The study was supported by a financial grant from the Ministry of Education, the Czech Republic (VZ MSM 0021620819)
Adress:
Ass. Prof. Petr Pazdiora, M.D., Ph.D.
Department of Epidemiology
Dr. E. Beneše 13
305 99 Pilsen
Czech Republic
E-mail address: pazdiora@fnplzen.cz
Sources
1. Bisharat, N., Elias, M., Raz, R., Flatau, E. Familial pattern of infection with hepatitis B virus among immigrating Ethiopian Jews in Israel. Eur. J. Epidemiol., 1998, 14, p. 89–91.
2. Coursaget, P., Gharbi, Y., Khrouf, N., Deptil, N. et al. Familial clustering of hepatitis B virus infections and prevention of perinatal transmission by immunization with a reduced number of doses in an area of intermediate endemicity (Tunisia). Vaccine, 1994, 12, p. 275–278.
3. Kuru, U., Turan, O., Kuru, N., Saglam, Z. et al. Prevalence of hepatitis B virus infection in pregnant Turkish women and their families. Eur. J. Clin. Microbiol. Infect. Dis., 1996, 15, p. 248–251.
4. Poirriez, J. Is the strategy of universal hepatitis B vaccination necessary in low-endemic countries? Scand. J. Gastroenterol., 1998, 33, p. 897–899.
5. Nemecek, V., Castkova, J., Fritz, P., Linhartova, A. et al. The 2001 serological survey in the Czech Republic – viral hepatitis. Central Eur. J. Public Health, 2003, 11, p. 54–61.
6. Trmal, J., Jílková, E., Ondřej, J. Frequency of the occurrence of HBsAg in carriers of hepatitis B surface antigen. Cesk. Epidemiol. Mikrobiol. Imunol., 1990, 39, p. 321–326.
7. Mravčík, V., Šebáková, H., Kania, A. Seroprevalence of viral hepatitis A, B and C in intravenous drug users. Epidemiol. Mikrobiol. Imunol., 2000, 49, p. 19–23.
8. Pazdiora, P., Voltr, J., Topolčan, O. The occurrence of viral hepatitis markers among venereological patients. Prakt. Lék., 1997, 77, p. 284–285.
9. Arima, S., Michitaka, K., Horiike, N., Kawai, K. et al. Change of acute hepatitis B transmission routes in Japan. J. Gastroenterol., 2003, 38, p. 772–775.
10. Ivanovski, L. J., Dimitriev, D. Intra-familial spread of acute hepatitis B virus infection. Minerva Gastroenterol. Dietol., 2003, 49, p. 187–194.
11. Milas, J., Ropac, D., Mulic, R., Milas, V. et al. Hepatitis B in the family. Eur. J. Epidemiol., 2000, 16, p. 203–208.
12. Ordog, K., Szendroi, A., Szarka, K., Kugler, Z. et al. Perinatal and intrafamily transmission of hepatitis B virus in three generations of a low-prevalence population. J. Med. Virol., 2003, 70, p. 194–204.
13. Zervou, E. K., Gatselis, N. K., Xanthi, E., Ziciadis, K. et al. Intrafamilial spread of hepatitis B virus infection in Greece. Eur. J. Gastroenterol. Hepatol., 2005, 17, p. 911–915.
14. Salkic, N. N., Zerem, E ., Zildzic, M., Ahmetagic, S. et al. Risk factors for intrafamilial spread of hepatitis B in northeastern Bosnia and Herzegovina. Ann. Saudi Med., 2009, 29, p. 41–45.
15. Alizadeh, A. H., Ranjbar, M., Ansari, S., Alavian, S. M. et al. Intra-familial prevalence of hepatitis B virologic markers in HBsAg positive family members in Nahavand, Iran. World J. Gastroenterol., 2005, 11, p. 4857–4860.
16. Chakravarty, R., Chowdhury, A., Chaudhuri, S., Santra, A. et al. Hepatitis B infection in Eastern Indian families: need for screening of adult siblings and mothers of adult index cases. Public Health, 2005, 119, p. 647–654.
17. Lobato, C., Tavares-Neto, J., Rios-Leite, M., Trepo, C. et al. Intrafamilial prevalence of hepatitis B virus in Western Brazilian Amazon region: epidemiologic and biomolecular study. J. Gastroenterol. Hepatol., 2006, 21, p. 863–868.
18. Salkic, N. N., Zildzic, M., Muminhodzic, K., Pavlovic-Calic, N. et al. Intrafamilial transmission B in Tuzla region of Bosnia and Herzegovina. Eur. J. Gastroenterol. Hepatol., 2007, 19, p. 113–118.
19. Ucmak, H., Kokoglu, O. F., Celik, M., Ergun, U. G. Intra-familial spread of hepatitis B virus infection in eastern Turkey. Epidemiol. Infect., 2007, 135, p. 1–6.
20. Lin, C. L., Kao, J. H., Chen, B. F., Chen, P. J. et al. Application of hepatitis B virus genotyping and phylogenetic analysis in intrafamilial transmission of hepatitis B virus. Clin. Infect. Dis., 2005, 41, p. 1576–1581.
21. Takegoshi, K., Zhang, W. Hepatitis B virus infections in families in which the mothers are negative but the fathers are positive for HBsAg. Hepatol. Res., 2006, 36, p. 75–77.
22. Mu, S. C., Wang, G. M., Jow, G. M., Chen, B. F. Impact of universal vaccination on intrafamilial transmission of hepatitis B virus. J. Med. Virol., 2011, 83, p. 783–790.
23. Nelson, K. R., Bui, H., Samet, J. H. Screening in special populations: a „case study“ of recent Vietnamese immigrants. Am. J. Med., 1997, 102, p. 435–440.
24. Patel, P. A., Voigt, M. D. Prevalence and interaction of hepatitis B and latent tuberculosis in Vietnamese immigrants to the United States. Am. J. Gastroenterol., 2002, 97, p. 1198–1203.
25. Taylor, V. M., Choe, J. H., Yasui, Y., Li, L. et al. Hepatitis B awareness, testing, and knowledge among Vietnamese American men and women. J. Community Health, 2005, 30, p. 477–490.
26. Erol, S., Ozkurt, Z., Ertek, M., Tasyaran, M. A. Intrafamilial transmission of hepatitis B virus in the eastern Anatolian region of Turkey. Eur. J. Gastroenterol. Hepatol., 2003, 15, p. 345–349.
27. Zhuo, J., Tao, G., Ebrahim, S. H., Wang, S. et al. The relationship of hepatitis B virus infection between adults and their children in Guangxi Province, China. J. Hepatol., 2000, 33, p. 628–631.
28. Thakur, V., Kazim, S. N., Guptan, R. C., Malhotra, V. et al. Molecular epidemiology and transmission of hepatitis B virus in close family contacts of HBV-related chronic liver disease patients. J. Med. Virol., 2003, 70, p. 520–528.
29. Doganci, T., Uysal, G., Kir, T., Bakirtas, A. et al. Horizontal transmission of hepatitis B virus in children with chronic hepatitis B. World J. Gastroenterol., 2005, roč. 11, s. 418-420.
30. Ono-Nita, S. K., Carrilho, F. J., Cardoso, R. A., Nita, M. E. et al.: Searching for chronic hepatitis B patients in a low prevalence area—role of racial origin. BMC Fam. Pract., 2004, roč. 5, s. 7.
31. Jeong, S. H., Yim, H. W., Yoon, S. H., Jee, Y. M. et al. Changes in the intrafamilial transmission of hepatitis B virus after introduction of a hepatitis B vaccination programme in Korea. Epidemiol. Infect., 2010, roč. 138, p. 1090–1095.
Labels
Hygiene and epidemiology Medical virology Clinical microbiology
Article was published inEpidemiology, Microbiology, Immunology

2012 Issue 3
Most read in this issue- Chromosomal Integration of the Sixth Human Herpes Virus (HHV-6)
- The Rules for the Transport of Microorganisms
- 30 Years since the First AIDS Cases Were Reported: History and the Present Part II
- Screening Family and Sexual Contacts of HBsAg+ Persons in the Pilsen Region
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

