-
Medical journals
- Career
Uterovesical fistula and its treatment in Sub-Saharan Africa
Authors: Tomáš Brtnický 1; A. M. Simono Charadan 2; Peter Koliba 1; Markéta Polková 1; Olga Dubová 1; Petr Hubka 1; Michal Zikán 1
Authors‘ workplace: Department of Obstetrics and Gynaecology, First Faculty of Medicine and Bulovka Hospital, Prague, Czech Republic 1; Department of Obstetrics and Gynaecology, Tamale Teaching Hospital, Ghana 2
Published in: Ceska Gynekol 2024; 89(1): 56-60
Category:
doi: https://doi.org/10.48095/cccg202456Overview
Aim: Aim of the study to summarize the current information on diagnostic and treatment options for uterovesical fistula as a consequence of iatrogenic complication. Methods: Literature review of available information on surgical treatment options for uterovesical fistula resulting from previous caesarean section and comparison with our own experience in the developing world. Conclusion: Uterovesical fistula is an abnormal communication between the bladder and uterus. The cause of this pathology in most cases is an iatrogenic complication, most commonly arising after a caesarean section. The incidence of this pathology varies significantly geographically. In developed countries, these fistulas are rather rare. On the other hand, in developing countries, uterovesical fistulas are more common with a significant impact on the subsequent life of the patient due to generally inaccessible health care.
Keywords:
urinary incontinence – caesarean section – uterovesical fistula
Introduction
Urogenital fistulas are characterized by abnormal communication between the genital tract and bladder, urethra or ureters. The aetiology and incidence of urogenital fistulas vary geographically. In developed countries, these types of fistulas are relatively rare and are most commonly associated with complications following gynaecological surgery or as a consequence of radiotherapy in the pelvic region [1]. In developing countries, on the other hand, urogenital fistulas are a relatively common complication after prolonged obstructed labour [2] or as a consequence of the increasing number of caesarean sections performed [3]. In developed countries, patients with these complications are often referred to centralized sites for surgical management, where in most cases they are successfully treated and thus have no residual problems. In developing countries, however, the situation is reversed. Women affected in this manner can hardly seek professional help. In many African countries, there is no health insurance and the economic situation of women with such impairments often makes it impossible to cover the necessary care. The psychosocial impact of this health complication is devastating, both for the patient herself and often for the whole family. The World Health Organization (WHO) estimates that there are approximately 3 million women with untreated vesico-vaginal fistula in poor countries worldwide. On the African continent, there are 30–100,000 new cases every year [4]. From sub-Saharan Africa, we have limited data sources; however, these data show that in more than 90% of women, the cause of urogenital fistula is obstructed labour. Uterovesical (or also vesicouterine) fistula most commonly occurs as a postpartum complication. However, it represents only 1–4% of all urogenital fistulas [5]. This type of fistula is most commonly described in the literature as a complication of a caesarean section, a caesarean scar defect, a complication of placenta percreta, or a fistula resulting from the insertion of an intrauterine device. Patients with this type of fistula suffer from urinary incontinence with leakage of urine from the bladder through the uterine cervix into the vagina. Some patients express Youssef syndrome, which is characterized by cyclic haematuria (menorrhagia), amenorrhea, urinary incontinence, and recurrent urinary infection [6]. Spontaneous healing of the fistula has been described in only 5% of patients in whom a permanent urinary catheter was inserted for 3 to 8 weeks [7,8]. Successful surgical repair requires resection of the entire fistula tract, i.e. both from the bladder and uterus, followed by suturing of the excised fistula margins in the anatomical layers. The insertion of the omentum or peritoneum between the bladder and uterus suture is recommended. Fistula recurrence is described in 7 to 20% of cases [9].
1. Red arrow – uterus, yellow arrow – urinary bladder, green arrow – vagina dilated with fluid – urine (published with the patient's permission). // Červená šipka – děloha, žlutá šipka – močový měchýř, zelená šipka – pochva dilatovaná tekutinou – močí (publikováno se svolením pacientky). 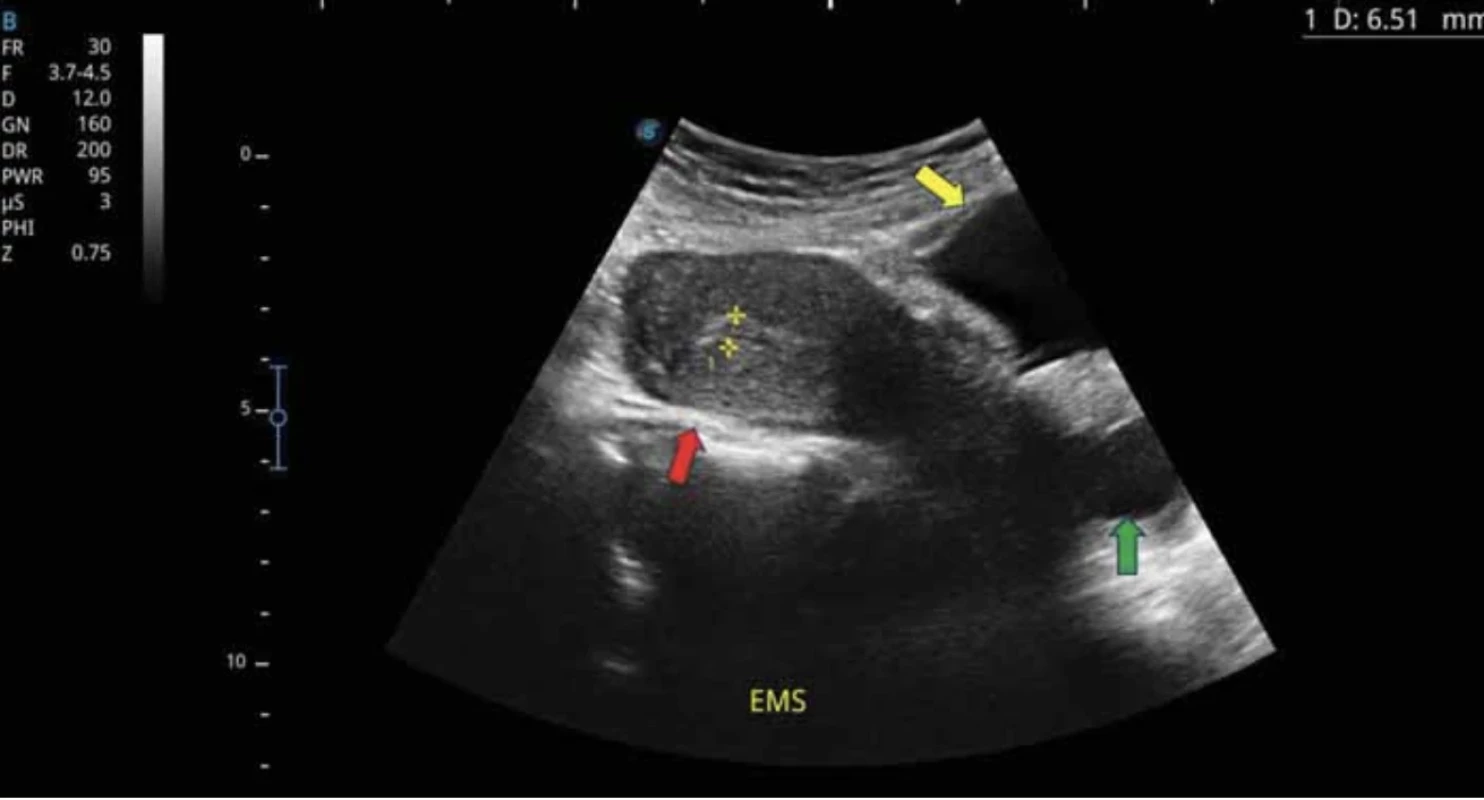
2. Yellow arrows show the uterovesical fistula tract, CX – cervix and U – urinary bladder (published with the patient's permission). // Žluté šipky znázorňují trakt uterovezikální píštěle, CX – děložní hrdlo a U – močový měchýř (publikováno se svolením pacientky). 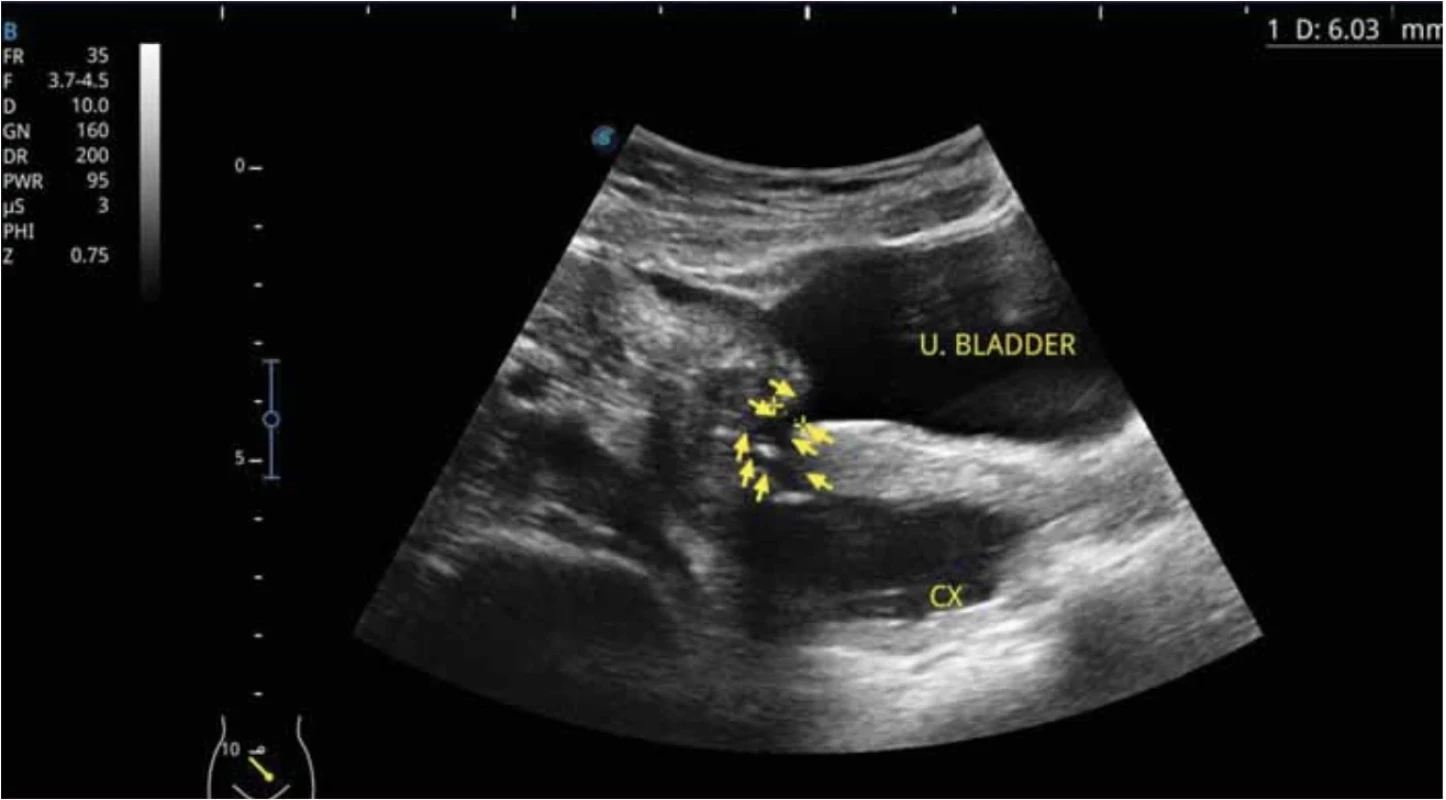
3. Yellow arrows show the fistula orifice with the Foley catheter in the opening (published with the patient's permission). // Žluté šipky zobrazují ústí píštěle se zavedeným foleyovým katetrem (publikováno se svolením pacientky). 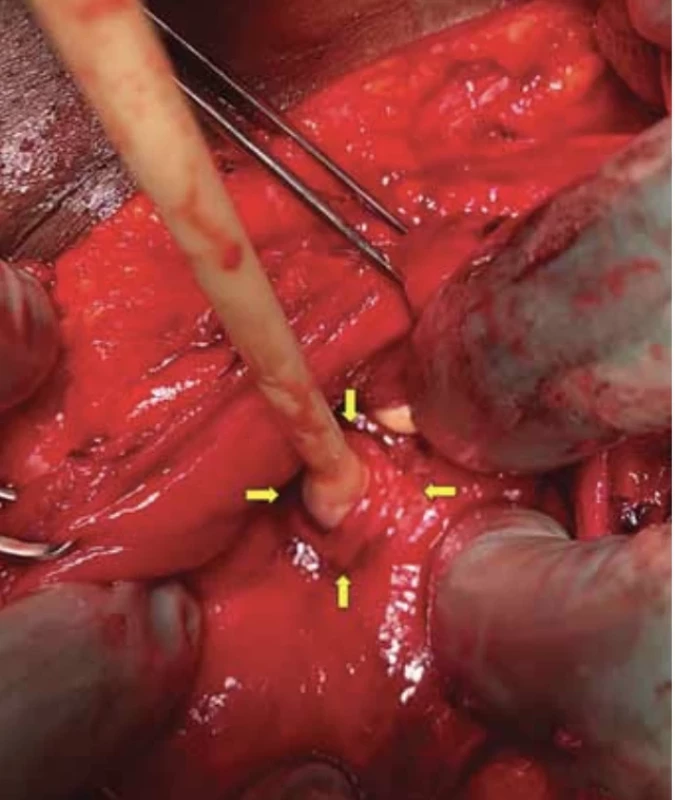
4. Yellow arrows show the defect in the bladder wall after excision of the fistula margins (published with the patient's permission). // Žluté šipky zobrazují defekt ve stěně močového měchýře po excizi okrajů píštěle (publikováno se svolením pacientky). 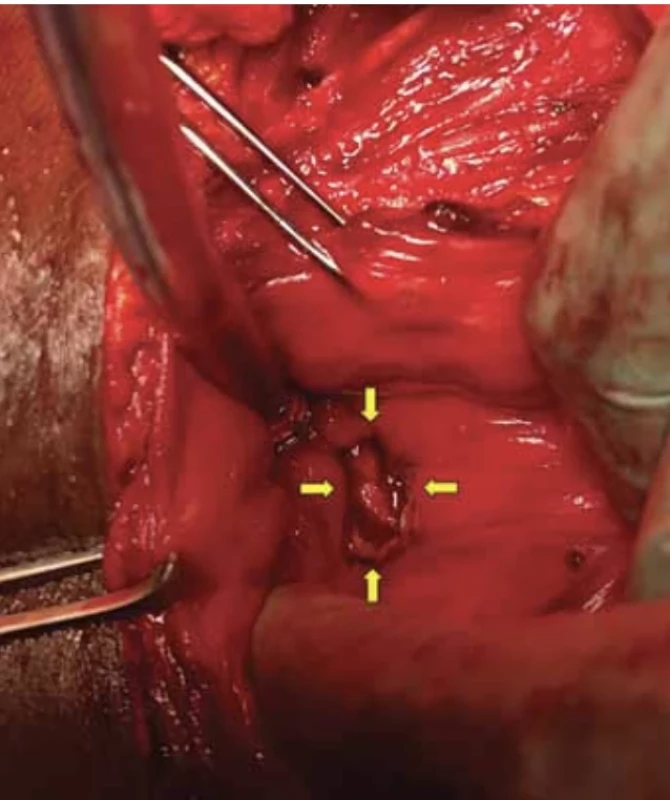
Case report
A 43-year-old woman underwent an acute caesarean section three years ago for the indication of acute foetal hypoxia during prolonged labour. Shortly in the postoperative period, she noticed leakage of urine. She therefore visited the nearby hospital in Koforidua (Eastern Region of Southern Ghana) where the suspicion of urogenital fistula was expressed. However, she could not afford surgery for financial reasons. Nevertheless, she heard about Medevac Czech‘s humanitarian mission and decided to travel about 600 km north to Tamale (northern region of Ghana). Her gynaecological history revealed a total of 10 pregnancies, including two spontaneous abortions at 8 and 12 weeks of gestation respectively, and a total of six spontaneous vaginal deliveries at term and two caesarean sections. Of the total eight deliveries, one was stillborn and the other three died at the ages of 3, 4 and 8 years. Her laboratory tests revealed she was positive for hepatitis C antibodies. Preoperative ultrasound examination was suggestive of the diagnosis of uterovesical fistula (Fig. 1, 2).
The day before surgery, a blue dye test was performed with a positive result, and dye leakage was evident from the bladder through the cervix into the vagina. Surgery was performed from a laparotomy approach through an incision in the scar from a previous Pfannenstiel. After lysis of adhesions in the pelvic area, the bladder was opened through a sagittal incision. Dissection of the vesicouterine space was then performed and the bladder descended caudally. The tract of the fistula between the uterus and bladder was opened and a Foley catheter was placed in the defect. An excision of the fistula was subsequently made from the posterior wall of the bladder into healthy tissue (Fig. 3, 4).
5. Yellow arrows – bladder fundus suture, blue arrows – omentum fixed between the bladder suture and anterior uterine wall suture (published with the patient's permission). // Žluté šipky – sutura fundu močového měchýře, modré šipky – omentum fixované mezi suturu močového měchýře a suturu přední stěny děložní (publikováno se svolením pacientky). 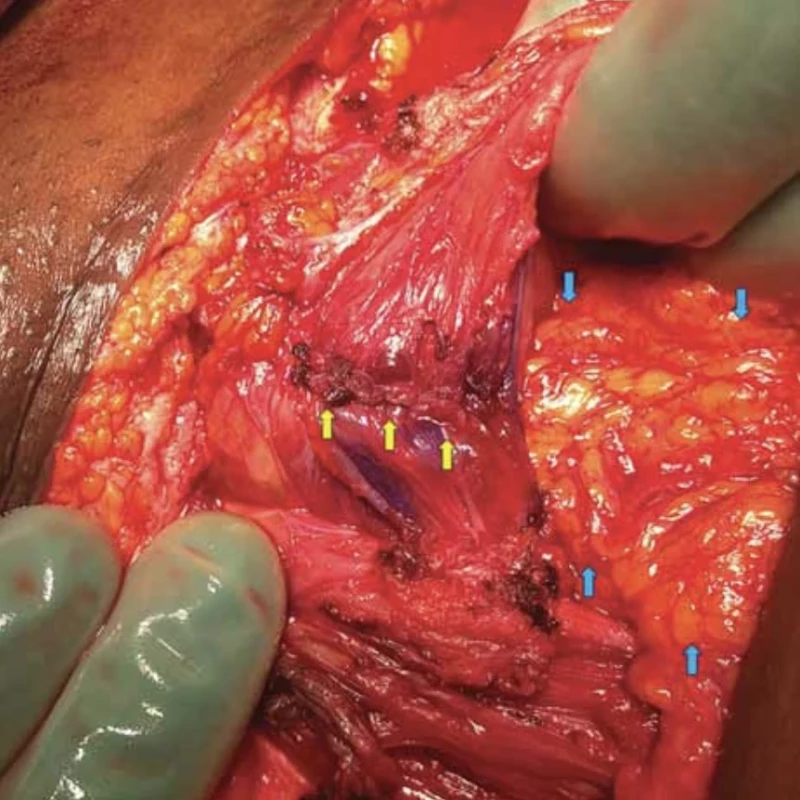
Then, a suture of the posterior wall after excision of the fistula and a suture of the bladder fundus in two layers with a continuous absorbable stitch were performed. Subsequently, the fistula was removed from the lower uterine segment at the site of the caesarean scar and the defect was sutured in two layers with a continuous absorbable stitch. At the end of the procedure, the omentum was mobilized and its caudal portion was fixed by two stitches in the space between the bladder and anterior uterine wall. Bladder tightness test was performed using a blue dye test with no sign of leakage (Fig. 5).
Urinary catheter was left in situ for 3 weeks after surgery. Upon its extraction, the patient urinated spontaneously and was fully continent. At follow-up two weeks after discharge, the relaparotomy had healed per primam and the patient was urinary continent.
Discussion
Urogenital fistula resulting as a postpartum complication is a problem particularly in sub-Saharan Africa. The prevalence of this complication correlates with maternal mortality rates, which are the highest here worldwide. However, high prevalence is also seen in other parts of the world with low levels of health care such as Afghanistan, Pakistan, Bangladesh and certain parts of India [10]. A prospective study of maternal morbidity in sub-Saharan Africa reported an annual incidence of 33,000 obstetric fistulas [11]. The prevalence of obstetric vesicovaginal fistula is directly related to the prevalence of obstructed labour and the availability of emergency obstetric care. In industrialized countries, this obstetric fistula is rare and the prevalence of vesicovaginal fistula as a subsequent surgical complication after simple or radical hysterectomy is predominant [12]. In a 20-year cohort study of urogenital fistulas from Norway, only four obstetric care-related urogenital fistulas occurred in 116,389 deliveries, and these were related to complications of caesarean section, cerclage and uterine rupture, and not from neglected prolonged labour [13]. In Ghana, where our humanitarian mission took place, a retrospective study was conducted between 1977 and 1992 to assess the epidemiology of urogenital fistulas. Almost 92% of urogenital fistulas were due to obstetric complications and only 7% were complications after hysterectomy, mostly for large uterine fibroids. The remaining 1% of causes of urogenital fistula were complications after female circumcision or a result of sexual violence against women (especially in conflict areas) [14]. Similar data were found in Nigeria, where a total of 932 cases of urogenital fistulas were documented between 1992 and 1999, of which 899 cases (96.5%) were associated with prolonged obstructed labour. The typical patient was of short stature and low body mass index, married early (average age around 15.5 years) but already divorced or separated at the time of fistula occurrence; uneducated, without financial resources and from a rural area. The fistula most often developed immediately after the first delivery, which lasted at least two days and resulted in stillbirth [2]. However, there are exceptions in sub-Saharan Africa. Rwanda‘s strong economic growth over the past two decades has been accompanied by a significant improvement in the living standards of its people. The mortality rate of children under the age of five has declined significantly between 2000 and 2020, and maternal mortality and total fertility rates have also fallen (thanks to increased availability of modern contraception). A published study from Kigali, Rwanda in 2021 illustrates the changes that took place between 2013 and 2017. There has been a dramatic increase in the availability of emergent procedures in obstetric care, particularly in the ability to perform caesarean sections. Of the 630 urogenital fistulas diagnosed, 392 (62%) were vesicovaginal, 185 (29%) were vesicouterine or vesicocervical, and 56 (9%) were ureterovaginal fistulas. Over the 5-year period, there was a significant increase in the proportion of vesicouterine, vesicocervical and ureterovaginal fistulas (time period: 29.6% in 2013; 34.6% in 2014; 43.0% in 2015; 42.9% in 2016; and 45.3% in 2017), with the majority occurring after caesarean section [3]. In our case report, vesicouterine fistula was treated from an open laparotomy approach, which offered the surgeon the advantage of good visibility of the operative field, rapid identification of the fistula and its subsequent repair. However, there are papers reporting successful closure of a vesicouterine fistula from the vaginal approach [15].
Conclusion
Vesicouterine fistula is not a common complication and is a minority among urogenital fistulas. Nevertheless, its incidence is increasing due to changes in health care, especially in developing countries. It should always be kept in mind in the case of young patients with a history of caesarean section who suffer from urinary incontinence combined with menorrhagia, infertility or repeated spontaneous abortions in the 1sttrimester of pregnancy.
Submitted/Doručeno: 17. 8. 2023
Accepted/Přijato: 1. 9. 2023Tomáš Brtnický, MD, PhD
Department of Gynecology and Obstetrics
First Medical Faculty
Charles University
Bulovka University Hospital
Budínova 2
180 00 Prague
tomas.brtnicky@bulovka.cz
Sources
1. Tancer ML. Observations on prevention and management of vesicovaginal fistula after total hysterectomy. Surg Gynecol Obstet 1992; 175 (6): 501–506.
2. Wall LL, Karshima JA, Kirschner C et al. The obstetric vesicovaginal fistula: characteristics of 899 patients from Jos, Nigeria. Am J Obstet Gynecol 2004; 190 (4): 1011–1019. doi: 10.1016/j.ajog.2004.02.007.
3. Richter LA, Lee H, Nishimwe A et al. Characteristics of genitourinary fistula in Kigali, Rwanda; 5-year trends. Urology 2021; 150 : 165–169. doi: 10.1016/j.urology.2020.05.077.
4. Wall LL. Obstetric vesicovaginal fistula as an international public-health problem. Lancet 2006; 368 (9542): 1201–1209. doi: 10.1016/S0140-67 36 (06) 69476-2.
5. Yip SK, Leung TY. Vesicouterine fistula: an updated review. Int Urogynecol J Pelvic Floor Dysfunct 1998; 9 (5): 252–256. doi: 10.1007/BF01901500.
6. Birge O, Ozbey EG, Erkan MM et al. Youssef’s syndrome following cesarean section. Case Rep Obstet Gynecol 2015; 2015 : 605325. doi: 10.1155/2015/605325.
7. Porcaro AB, Zicari M, Zecchini Antoniolli S et al. Vesicouterine fistulas following cesarean section: report on a case, review and update of the literature. Int Urol Nephrol 2002; 34 (3): 335–344. doi: 10.1023/a: 1024443822378.
8. Novi JM, Rose M, Shaunik A et al. Conservative management of vesicouterine fistula after uterine rupture. Int Urogynecol J Pelvic Floor Dysfunct 2004; 15 (6): 434–435. doi: 10.1007/s00192-004-1165-5.
9. Leng WW, Amundsen CL, McGuire EJ. Management of female genitourinary fistulas: transvesical or transvaginal approach? J Urol 1998; 160 (6 Pt 1): 1995–1999. doi: 10.1097/000053 92-199812010-00013.
10. Wall LL. Obstetric fistula is a „neglected tropical disease”. PLoS Negl Trop Dis 2012; 6 (8): e1769. doi: 10.1371/journal.pntd.0001769.
11. Vangeenderhuysen C, Prual A, Ould el Joud D. Obstetric fistulae: incidence estimates for sub-Saharan Africa. Int J Gynaecol Obstet 2001; 73 (1): 65–66. doi: 10.1016/s0020-7292 (00) 003 74-x.
12. Hilton P, Cromwell DA. The risk of vesicovaginal and urethrovaginal fistula after hysterectomy performed in the English National Health Service – a retrospective cohort study examining patterns of care between 2000 and 2008. BJOG 2012; 119 (12): 1447–1454. doi: 10.1111/j.1471-0528.2012.03474.x.
13. Trovik J, Thornhill HF, Kiserud T. Incidence of obstetric fistula in Norway: a population-based prospective cohort study. Acta Obstet Gynecol Scand 2016; 95 (4): 405–410. doi: 10.1111/aogs.12845.
14. Danso KA, Martey JO, Wall LL et al. The epidemiology of genitourinary fistulae in Kumasi, Ghana, 1977–1992. Int Urogynecol J Pelvic Floor Dysfunct 1996; 7 (3): 117–120. doi: 10.1007/BF01894198.
15. Cao M, Zhang J, Chen Y et al. Transvaginal repair of vesicouterine fistulae: our experience of three cases. Int Urogynecol J 2022; 33 (3): 737–740. doi: 10.1007/s00192-021-04973-x.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicine
Article was published inCzech Gynaecology

2024 Issue 1-
All articles in this issue
- Preoperative and postoperative staging in endometrial cancer – a prospective study
- Importance of vaginal packing after laparoscopic sacrocolpopexy – retrospective study
- Discrepancies in staging and perioperative classification of pelvic endometriosis according to #Enzian 2021
- Pandemic fear and psychological resilience in pregnant women after the pandemic – a study in Turkey
- Occurrence of acute retrobulbar hemorrhage during birth
- Occult invasive cervical cancer, FIGO stage III, with a negative Pap smear test – clinical presentation and brief review of the literature
- Primary perineal endometriosis – a case report and literature review
- Ultrasound finding of endometrial polyp and factors increasing risk of malignancy
- Female orgasm, reproduction and couple relationships
- Uterovesical fistula and its treatment in Sub-Saharan Africa
- Birth plan – legal and medical aspects
- New recommendations for informing patients and gamete donors in assisted reproduction
- Diagnostika a léčba endometriózy
- Czech Gynaecology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Ultrasound finding of endometrial polyp and factors increasing risk of malignancy
- Diagnostika a léčba endometriózy
- Importance of vaginal packing after laparoscopic sacrocolpopexy – retrospective study
- Female orgasm, reproduction and couple relationships
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

