-
Medical journals
- Career
Sclerosis tuberosa and pregnancy
Authors: M. Gábor 1; V. Ferianec 1; I. Mečiarová 2; Peter Papcun 1; K. Holomáň 1
Authors‘ workplace: Department of pathology Ružinov, Alpha medical patológia, s. r. o., Bratislava, Slovak Republic, doc. MUDr. F. Ondriáš, CSc. 2; nd Department of Obstetrics and Gynaecology, University Hospital Bratislava, Comenius University, Bratislava, Slovak Republic, prof. MUDr. K. Holomáň, CSc. 12
Published in: Ceska Gynekol 2014; 79(3): 186-189
Overview
Objective:
To perform a review of Tuberous sclerosis complex and its complications during the pregnancy from up to date scientific literature. Design: Complex systematic review of the literature. Setting: 2nd Department of Obstetrics and Gynaecology, University Hospital Bratislava, Comenius University, Bratislava, Slovak Republic. Methods: Complex analysis of the syndrome, systematic search of MEDLINE and Slovak Medical Library. The reason to create a complex review of this syndrome was our clinical experience with one of the most acute lifethreatening condition of this syndrome – acute retroperitoneal haemorrhage in the pregnancy. Conclusion: Tuberous sclerosis can cause a rare, but potentially lifethreatening complications, especially during the pregnancy. These should be carefully dispesarized and in complicated cases acute radical management should be considered. Keywords: m. Bourneville-Pringle, sclerosis tuberosa, tuberous sclerosis, phacomatosis, pregnancy, angiomyolipoma, retroperitoneal haemorrhageSCLEROSIS TUBEROSA SYNDROME
Tuberous sclerosis (TS, synonym Epiloia seu Bourneville-Pringle disease) is a neurocutaneous syndrome and the second most frequent phacomatosis (gr. “phacos“ means birthmark).
It was described by Désiré-Magloire Bourneville for the first time in 1880. TS is a hereditary disease affecting ectodermal tissues. In childhood it has a slow progression with typical growth of benign tumours called hamarthomas in different anatomical locations. It is a rare disease with a prevalence in the population 1 : 10 000 and incidence 1 : 6000, occuring almost identically in all races, ethnic groups and both genders [6, 13, 27].
GENETICS, CLINICAL MANIFESTATIONS, DIAGNOSTICS AND THERAPY
From a genetic point of view, this is a tumoursupressor disease with variable expresivity, high penetrance and autosomal dominant inheritance. Two different genes whose mutations can cause this syndrome have been identified – TSC1 and TSC2. Both genes belong to the tumoursupressors gene group, which regulates proliferation of the cells. “De novo“ mutations are very frequent (up to 80 percent) and clinical manifestation is usually more serious [11, 18]. The clinical signs and symptoms depend on organ manifestation. Potentially, TS can affect every tissue in the body. Most frequent manifestations are hamarthomas in the skin, brain, kidneys, lungs, heart, endocrine glands, bones and the retina.[6,18] Primary diagnosis is usually made by pediatricians and neurologists in childhood. TS can vary from “only“ cosmetic skin defects, to severe organ damage.[13, 25]. The most important diagnostic criteria are cerebral lesions causing epileptic seizures, mental retardation, cerebral palsy and psychiatric disorders, skin lesions include facial angiofibromas called adenoma sebaceum, subungual and periungual fibromas called “pringle tumours“, rough spots of Schagren “pig-elephant“ skin, etc. Other common organ presentations are cardiac rhabdomyomas, retinal hamarthomas, renal angiomyolipomas, hamarthomatous rectal polyps, etc. Malignant change of these tumours is very rare [3, 8, 10]. The leading imaging modalities in diagnostics of TS lesions are computed tomography, magnetic resonance imaging and ultrasonography. Additional examinations by dermatologist, ophthalmologist and psychiatrist are useful [1, 2, 18, 27]. Some kidney tumours were incidentally diagnosed also during standard ultrasound examination in the pregnancy [19]. Final diagnosis is based on DNA analysis of the TSC1 or TSC2 gene mutations, clinically on main signs according to actual classification. Reliable methods used in diagnostics of mutations are PCR, quantitative PCR and gene sequencing. Useful modalities in the diagnosis of TS are described in table 1.
1. Diagnosis of tuberous sclerosis 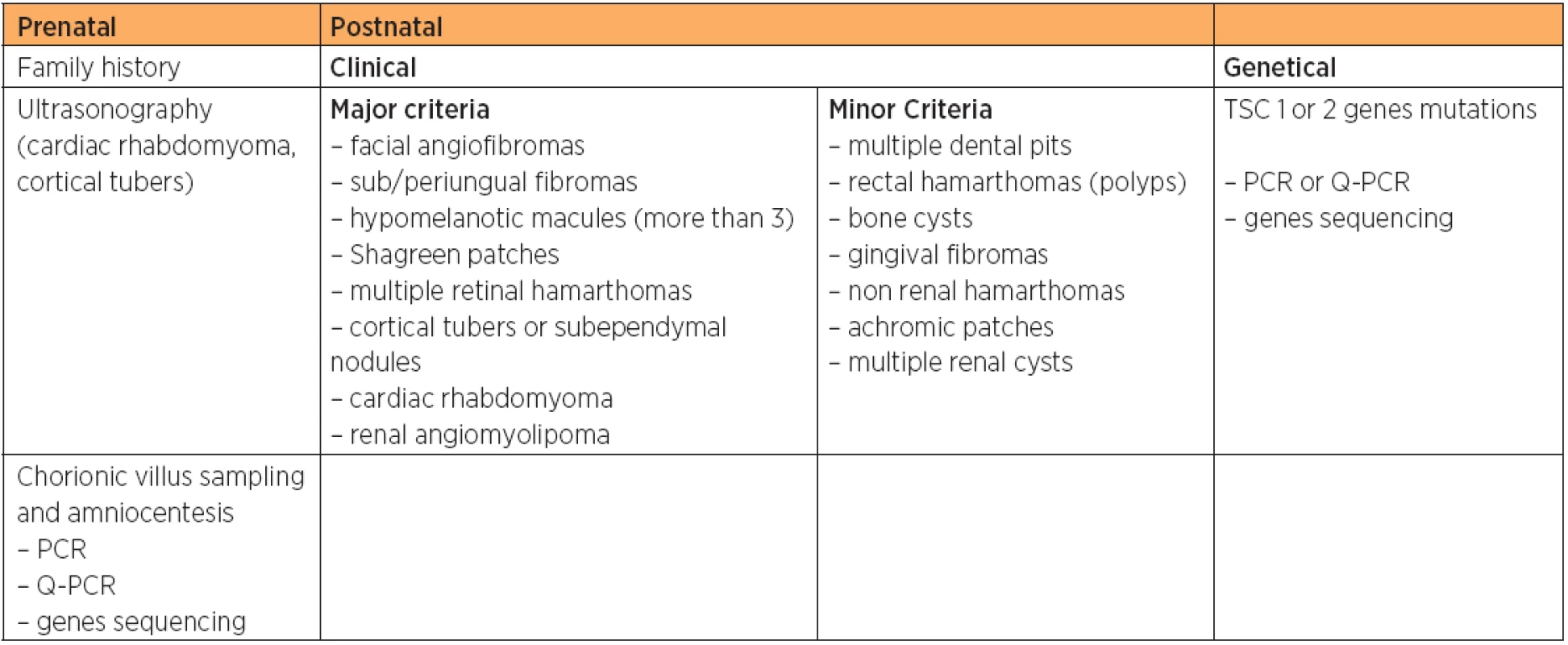
Causal therapy of TS is not yet available and treatment is only symptomatic. Tiberio et al. in 2011 described a case of significant regression of a cardiac rhabdomyoma after receiving Everolimus, an mTOR inhibitor (mammalian target of Repamycine inhibitor). This finding suggested a possible novel therapy for patients with clinically significant cardiac rhabdomyomas [26].
For subependymal giant-cell astrocytomas in patients with the TS the standard treatment is the neurosurgical resection. In the Kruegers study (2010) the Everolimus therapy was associated with marked reduction in the volume of subependymal giant-cell astrocytomas and seizure frequency and may be a potential alternative to neurosurgical resection in some cases, though long-term studies are more needed [17].
Dispensarisation of the patient is necessary. The prognosis depends on the localisation of the lesions. Slow progression, especially alteration of the cognitive functions, often leads to terminal state in early adulthood. Prognosis quad vitam for incomplete forms of the syndrome is better [18].
PRENATAL DIAGNOSTICS
Prenatal screening of TS is recommended if positive family history of TSC gene mutations has been identified [23]. The most frequent ultrasound marker of TS affected fetus is the presence of cardiac rhabdomyoma [15]. This benign tumour with poor prognosis is usually recognized after the 29th week of gestation by fetal ultrasound examination, especially fetal echocardiography. Despite its benign dignity, extensive tumours affecting cardiac outflow tracts can cause haemodynamic alteration of the fetus. Tumours totally involving outflow tracts and extensively expanding pericardium have been described. These severe cases are often related to fetal hydrops and intrauterine death in the second trimester is common [15, 29]. After primary in utero diagnosis of the left outflow tract obstruction, it is necessary to provide postpartal emergent surgical intervention [9, 20]. Prenatal diagnosis is recommended for fetuses in the high risk group – a positive family history or the presence of cardiac rhabdomyoma. The leading procedure is amniocentesis or chorionic villus sampling [7]. For a detailed image of cardiac lesions fetal magnetic resonance may be also beneficial. Prognosis and management should be consulted with pediatricians and cardiac surgeons. Fortunately, cardiac rhabdomyomas usually slowly regresses in the first year of life. Possible ultrasound markers of TS are also cerebral cortical tubers and cerebral astrocytomas. Unfortunately, these tumours do not tend to regress, on the contrary, there is progression in their growth and count [21, 30].
TUBEROUS SCLEROSIS IN THE PREGNANCY AND TYPICAL ACUTE COMPLICATIONS
In the management of early pregnancy, it is necessary to consider the influence of administred anticonvulsive drugs. Spontaneous abortion and fetal demise are very frequent. Except general complications of TS, the lifethreatening complication associated with pregnancy is retroperitoneal haemorrhage (figure 1). The high risk of retroperitoneal haemorrhage is associated with renal angiomyolipomas. Frequently the tumours can be very big, in the literature tumours weighing 5700 g or more have been described [22]. Physiological haemodynamic changes in pregnancy induce this complication, which threaten the patient mostly in the third trimester. Vaginal delivery is also considered as a risk factor [22]. In a retrospective study of these tumours and their associated complications in the period between 1952 and 2004, 72 cases were described. 58 cases were complicated in average gestational age at 27th week [16].
Fig. 1 Pacient after right radical nephrectomy (acute retroperitoneal haemorrhage in the 9th week of the multiple pregnancy). Smaller residual renal angiomyolipoma of the left kidney in situ (red arrow), transverse view, MRI in T1. Right fossa renalis is empty (green arrow) (st. Post in toto extirpationem renis l.dx cum angiomyolipomatosis). Archive 2<sup>nd</sup> Department of Obstetrics and Gynaecology, University Hospital Bratislava, Comenius University, Bratislava, Slovak Republic) 
In the surgical management of this complication, the total nephrectomy in 79 percent of cases was indicated [16], rarely polar nephrectomy or selective arterial embolisation were performed [16]. If possible, also a conservative management with strict monitoring can be applied. Another possibility to solve the complication is to perform the therapeutical selective arterial embolisation of the tumour vessels. In the cases of multiple angiomyolipomas, repeated early prophylactic embolisations are also suitable. If tumour embolisation does not tend to prevent or to stop the bleeding, radical surgery is indicated, after the 28th week with simultaneous caesarean section (SC) [12]. As a mode of delivery SC is recommended [12]. In the case of bilateral tumour masses, it is possible to succeed with nephron-sparing tumorectomy [5, 24]. Giant bilateral renal masses without signs of bleeding should be managed without radical surgical intervention, prophylactic embolisation and strict follow-up management is indicated [14]. Ferianec et al. in 2013 reported an unique acute complication of TS. He described severe retroperitoneal haemorrhage of the 30-year-old primigravida in the first trimester of a multiple pregnancy. The complication was presented after spontaneous rupture of renal angiomyolipoma caused by TS. The authors reported that acute renal lifethreatening complication of TS is not only typical for 2nd or 3rd trimester and the coincidence with multiple pregnancy can lead to its very early onset in the early pregnancy [4].
Martin Gábor, MD
University Hospital Bratislava
Ružinovská 6
826 06 Bratislava
Slovak Republic
e-mail: martingabormd@gmail.com
Sources
1. Bissler, JJ. Sirolimus for angiomyolipoma in tuberous sclerosis complex. N Engl J Med, 2008, 358, p. 140–151.
2. Caprez, C., Walling, AD., Reimer, CM. Tuberous sclerosis complex in a young woman diagnosed incidentally on the basis of pregnancy ultrasonography. South Med J, 2004, 97, 5, p. 512.
3. Curatolo, P. Tuberous sclerosis complex. From basic science to clinical phenotypes. Cambridge: University Press, 2003.
4. Ferianec, V., Gábor, M., Caňo, M., et al. Severe retroperitoneal haemorrhage in the first trimester of a multiple pregnancy after spontaneous rupture of renal angiomyolipoma. Arch Gynecol Obstet, 2013, published online in May 26. Available at. http://link.springer.com/article/10.1007%2Fs00404-013-2902-0.
5. Gimeno Argente, V., Bosquet Sanz, M., Bonillo García, MA., et al. Conservative surgery of bilateral renal angiomyolipoma during pregnancy. Actas Urol Esp, 2006, 30, 6, p. 633–637.
6. Gomez, MR. Tuberous sclerosis. New York: Ravenpress, 1999.
7. Gupta, N., Singh, N., Sarangi, S., et al. Fetal cardiac rhabdomyoma with maternal tuberous sclerosis complicating pregnancy. Arch Gynecol Obstet, 2008, 278, 2, p. 169–170.
8. Gurčík, L. Tuberózna skleróza. Levoča: Polypress, 2007.
9. Gurčík, L., Gašparíková, V. Tuberózna skleróza z pohľadu neurológa. Neurológia pre prax, 2008, 3, s. 161–164.
10. Habiňáková, J. Orgánové postihnutie pri m. Pringle. Laboratórna diagnostika, 1997, 2, 1, s. 12.
11. Hankey, J. Clinical neurology. Edinburgh UK: Manson Publishing, 2008.
12. Illescas Molina, T., Montalvo Montes, J., Contreras Cecilia, E., et al. Angiomyolipomas, tuberous sclerosis and pregnancy. Ginecol Obstet Mex., 2009, 77, 8, p. 380–386.
13. Jones, AC. Comprehensive mutation analysis of TSC1 TSC2 and phenotypic corelations in 150 families with tuberous sclerosis. Am J Hum Genet, 2008, 64, p. 1305–1315.
14. Khaitan, A., Hemal, AK., Seth, A., et al. Management of renal angiomyolipoma in complex clinical situations. Urol Int, 2001, 67, 1, p. 28–33.
15. King, JA., Stamilio, DM. Maternal and fetal tuberous sclerosis complicating pregnancy: a case report and overview of the literature. Am J Perinatol, 2005, 22, 2, p. 103–108.
16. Klein, M., Matal, M., Wagner, C., et al. Obstetrical management in maternal tuberous sclerosis Pringle-Bourneville syndrome – a case report. Wien: Hanusch-Krankenhaus, 2010.
17. Krueger, DA., Care, MM., Holland, K., Agricola, K., et al. Everolimus for subependymal giant-cell astrocytomas in tuberous sclerosis. N Engl J Med, 2010, 363, p. 1801–1811.
18. Lyczkowski, DA., Conant, KD., Pulsifer, MB., et al. Intrafamilial phenotypic variability in tuberous sclerosis complex. J Child Neurol, 2007, 22, 12, p. 1348–1355.
19. Li, W., Zhou, LH., Gao, BD., et al. Mutation screening and prenatal diagnosis of tuberous sclerosis complex. J Institute of Reproduction and Stem Cells Ingeneering China, 2011, 28, 4, p. 361–366.
20. Milunsky, A., Ito, M., Maher, TA. Prenatal molecular diagnosis of tuberous sclerosis complex. Am J Obstet Gynecol., 2009, 200, 3, p. 321.
21. Milunsky, A., Shim, SH., Ito, M., et al. Precise prenatal diagnosis of tuberous sclerosis by sequencing the TSC2 gene. Prenat Diagn, 2006, 26, 9, p. 867–869.
22. Raft, J., Lalot, JM., Meistelman, C., et al. Influence of pregnancy on renal angiomyolipoma. Gynecol Obstet Fertil, 2005, 33, 11, p. 898–906.
23. Sharma, J., Inglis, S., Cavalieri, R., et al. Fetal demise secondary to massive rhabdomyoma in the early second trimester of pregnancy. Pediatr Cardiol, 2011, 32, 2, p. 243–244.
24. Shiroyanagi, Y., Kondo, T., Tomita, E., et al. Nephron-sparing tumorectomy for a large benign renal mass: a case of massive bilateral renal angiomyolipomas associated with tuberous sclerosis. Int J Urol, 2002, 9, 2, p. 117–119.
25. Škvarlová, M. Morbus Bourneville-Pringle. Dermatológia pre prax, 2007, 4, 1, s. 18.
26. Tiberio, D., Franz, ND., Phillips, JR. Regression of a cardiac rhabdomyoma in a patient receiving everolimus. Pediatrics, 2011, 5, p. 127.
27. Varsík, P. Neurológia II – patogenéza a klinika nervových chorôb. Martin: Lufema, 1999.
28. Varsík, P. Neurokutánne syndrómy v MRI obraze. Slovenská rádiológia, 2005, 12, 1, s. 7–13.
29. Verhaaren, HA., Vanakker, O., De Wolf, D., et al. Left ventricular outflow obstruction in rhabdomyoma of infancy: meta-analysis of the literature. J Pediatr, 2003, 143, 2, p. 258–263.
30. Wortmann, SB., Reimer, A., Creemers, JW., et al. Prenatal diagnosis of cerebral lesions in tuberous sclerosis complex (TSC). Eur J Paediatr Neurol, 2008, 12, 2, p. 123–126.
Labels
Paediatric gynaecology Gynaecology and obstetrics Reproduction medicine
Article was published inCzech Gynaecology

2014 Issue 3-
All articles in this issue
- The INKA Program – “tailor-made” obstetric analgesia
-
Why do we still hesitate to accept the new international criteria for the diagnosis of gestational diabetes mellitus?
The current screening is non-uniform and does not correspondwith evidence-based medicine - The alarming incidence of gestational diabetes mellitus using currently used and new international diagnostic criteria
- HELLP syndrome complicated by liver rupture – case report
-
Importance of outpatient ultrasonografically guided transvaginal hydrolaparoscopy in the decision algorithm of care for the infertile couple.
The results of the Centre for Assisted Reproduction Gennet Liberec 2012–2013 - Diagnostic algorithm in pregnancies of uncertain viability or unknown location – a review of the latest recommendations
- Myo-inositol in the treatment of polycystic ovary syndrome
- Evolution of peripartal hysterectomy at our department – five years evaluations
- Hormonal replacement therapy by patientsafter treatment for gynecological cancer
- Thrombotic microangiopathy in pregnancy complicated by acute hemorrhagic-necrotic pancreatitis during early puerperium
-
Prenatal diagnosis of skeletal dysplasia in first trimester of pregnancy
X-linked dominant chondrodysplasia punctata - Sclerosis tuberosa and pregnancy
- Czech Gynaecology
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- Diagnostic algorithm in pregnancies of uncertain viability or unknown location – a review of the latest recommendations
- Myo-inositol in the treatment of polycystic ovary syndrome
-
Prenatal diagnosis of skeletal dysplasia in first trimester of pregnancy
X-linked dominant chondrodysplasia punctata - HELLP syndrome complicated by liver rupture – case report
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

