-
Medical journals
- Career
VACUUM-ASSISTED CLOSURE DOWNGRADES RECONSTRUCTIVE DEMANDS IN HIGH-RISK PATIENTS WITH SEVERE LOWER EXTREMITY INJURIES
Authors: D. Kakagia 1; E. Karadimas 2; G. Drosos 3; A. Ververidis 3; D. Kazakos 3; M. Lazarides 4; D. Verettas 3
Authors‘ workplace: Department of Plastic Surgery, 2NHS Orthopedic Department, 3Department of Orthopedic Surgery, 4Department of Vascular Surgery, Democritus University, Alexandroupolis University Hospital, Dragana, Alexandroupolis, Greece 1
Published in: ACTA CHIRURGIAE PLASTICAE, 51, 3-4, 2009, pp. 59-64
INTRODUCTION
Acute injuries of the lower extremities may be seriously debilitating and may co-exist with life-threatening conditions. Comprehensive patient care necessitates close collaboration between health professionals. Primary reconstruction of soft tissues, as part of the multidisciplinary management required, is the gold standard as it ensures protection of fixated, exposed bones and repaired nerves, tendons and / or vessels (10, 15). Immediate soft tissue reconstruction, however, may be precluded by the patients’ general clinical status or by unfavorable local wound conditions (10, 11, 17).
Patients in critical condition with serious medical co-morbidities, those who are elderly or have been admitted to an Intensive Care Unit (ICU) due to coexisting life-threatening injuries, may not be considered good candidates for primary soft tissue reconstruction (10). Many of these patients may have been referred by the District Hospitals where the initial surgical management was undertaken but Plastic Surgery Services may not always be readily available. Furthermore, heavily exuding or contaminated traumas with questionable viability of tissues on the wound bed – even after initial debridement – might benefit from delayed reconstruction. In such cases surgical debridement with or without irrigation and wound drainage followed by antibiogram-specific antibacterial medical treatment is advisable prior to any soft tissue reconstructive procedure (17).
Delayed closure offers the time for re-evaluation of the viability of already reconstructed deep structures such as bones, vessels, tendons and nerves as well as of remaining soft tissues. It also allows for optimal preparation of the wound bed, better planning of the reconstructive procedure and, even more importantly, for closure of the soft tissue deficit with a simpler procedure than originally required. Soft tissue reconstruction of the lower extremities with conventional or free flaps may be associated with complications that may compromise health in high-risk patients (10). Bearing in mind that this increased morbidity may be detrimental, simpler methods of reconstruction, such as the use of local flaps or skin grafting, may be preferable in order to maintain the fragile balance between effectiveness and safety.
Negative pressure is a non-invasive method that has been introduced in the management of complex wounds because it can reduce total wound volume and remove third space fluids, thus reducing oedema and improving oxygen delivery to the wound bed. There is also considerable literature to support the claim that it promotes angiogenesis and stimulates robust granulation tissue response (5, 12). Since first introduced in 1997 by Argenta and Morykwas (1, 12), negative pressure has been used in lower limb injuries in order to control wound exudate, reduce wound size, close escharotomies, relieve from venous congestion of muscular and free flaps and increase the skin graft take. (3, 6, 8, 9, 16).
However, as negative pressure has no effect on non - -viable tissues, meticulous debridement of the wound bed is required prior to application of the method.
The development of healthy granulation tissue and wound contraction result in spontaneous closure or – more frequently – allows for reconstruction of soft tissues with skin grafts or local flaps instead of the distant conventional or free flaps usually required for primary reconstruction.
This study aims to evaluate retrospectively the use of Vacuum Assisted Closure (VAC®, KCI, San Antonio, TX) in patients with lower limb trauma who were unsuitable for immediate soft tissue reconstruction.
PATIENTS AND METHODS
Between October 2005 and March 2009, 53 patients with 61 complex lower extremity traumas were treated with VAC®therapy as inpatients in Democritus University Hospital. Patients initially identified for inclusion in the study were either referred to the Plastic Surgery Unit from District Hospitals after initial management (n=41) or were unsuitable for immediate soft tissue reconstruction due to poor general condition or adverse local wound factors. Six of these patients failed to attend the follow up until final evaluation and five more were also excluded due to incomplete data. Eventually 42 patients with 49 complex lower limb traumas, who underwent delayed soft tissue reconstruction due to the conditions presented in Table 1, were included in the study.
1. Unfavorable conditions precluding primary soft tissue reconstruction. In some patients more than one factor were present 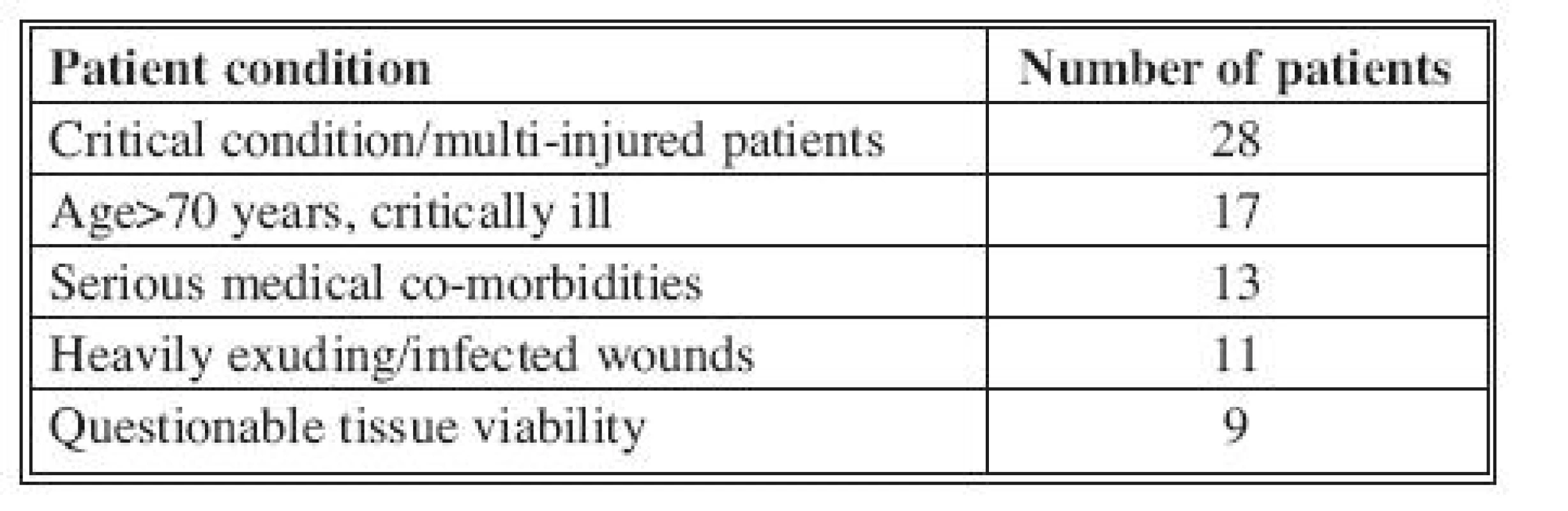
VAC® was applied 48 hours after bone fixation, vascular repair and surgical debridement of non viable tissues (Fig. 1). In 4 patients the wound had to be re-debrided before the application of negative pressure therapy, and in two of them therapy was delayed for two more days. In 7 patients who had two injury sites each both wounds were managed with VAC® with the use of the specially provided “Y” connector. VAC® pressure was set to 125 mm Hg, continuous mode, and the polyurethane sponges were changed every 48 hours or more frequently if indicated (i.e. heavily exuding wounds).
Fig. 1. Gustillo III c tibial injury: A: On the day of fracture stabilization, nerve and vascular repair, B: After 24 days of VAC therapy the tibial fracture line still protruding, C: After 39 days of VAC therapy and complete cover of the deficit bed with healthy granulation tissue, delayed reconstruction with a random local transpositional flap, and D: Final result six months postoperatively 
Wound swab cultures were obtained before the application of VAC® and before every change of sponge. Both wet swab quantitative cultures as described by Bill (2), and qualitative swab cultures were obtained. The duration of therapy, wound flora, final reconstructive technique required, outcome and follow up period were recorded for each patient.
RESULTS
Twenty-four male and eighteen female patients with a mean age of 47 years (range 21–82 years) were treated with VAC® therapy for a mean period of 28 days (range 15–42 days). Regarding topographic distribution of anatomic sites managed with VAC®, 8 were thigh wounds, 5 were located at the knee, 16 at the leg, 9 at the ankle and 11 at the foot (Fig. 2).
Fig. 2. Complex medial malleolus trauma in a multi-injured young hemophiliac patient: A: Before debridement and exploration revealing division of tibialis anterior tendon, flexor digitorum longus and abductor hallucis muscles as well as division of posterior tibial artery and nerve and of nerve to flexor digitorum brevis, B: After re-approximation of inner structures, application of VAC, C: Development of robust granulation treatment after 18 days of therapy, and D: Final soft tissue cover with a split thickness skin graft; appearance 3 weeks postoperatively 
Eighteen wounds were found to be colonized and nine were found to be infected prior to VAC®application. Five of them grew more than one bacteria: Pseudomonas aeriuginosa was found in 5, Staphylococcus aureus in 5, Acinetobacter baumannii in 2, Klebsiella pneumoniae in 2, Enterobacter in 2 and Proteus mirabilis in 2. Patients received antibiogram-specific intravenous antibacterial treatment. In all but one wound bacterial flora was progressively reduced during application of negative treatment, and all wound cultures were found to be negative before completion of VAC® therapy. In one patient with a wound infected by Klebsiella, before the third change of sponge the wound grew MRSA as well, and wound cultures remained positive until the sixth dressing change.
Patients were followed up for 90 to 895 days (mean = 458 days). Reconstructive methods applied after cessation of negative pressure treatment and outcomes are presented in Table 2.
2. Delayed reconstructive method and final outcome in 48 of a total of 49 wounds 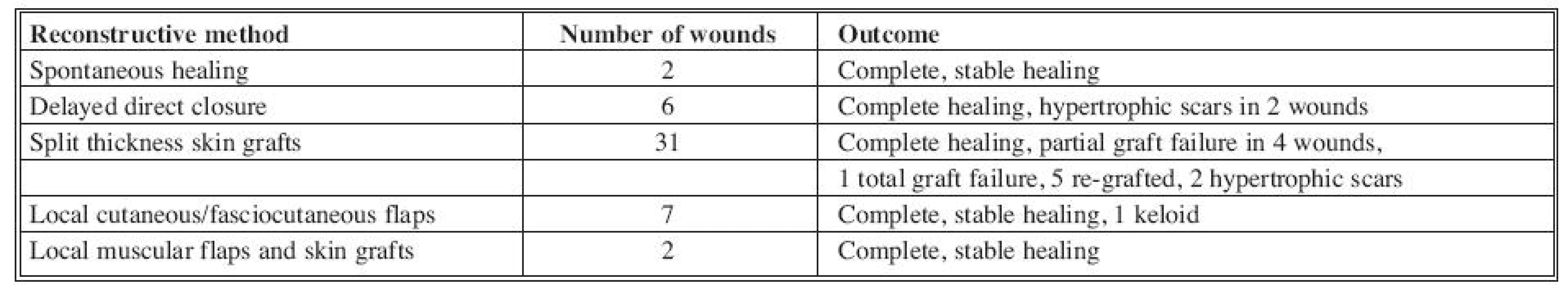
One patient died during therapy due to fat embolism. No significant bleeding occurred in any patient during negative pressure therapy.
In most patients an external fixation system was used for stabilization of fractured bones; however, the development of healthy granulation tissue permitted manipulations and revisions of fixation without any problems (Fig. 1, 3). The use of local flaps was reserved for patients with tendon or bone grafts and exposed bone fixation material. Four of the local flaps used were random cutaneous transpositional flaps, three were lateral calcaneal, one was abductor digiti minimi and one was medial gastrocnemius muscular flap. As expected, the functional outcome depended on the original bone, tendon and / or nerve injury.
Fig. 3. Circumferential crush-avulsion tibial injury with Gustillo III c fracture: A: After initial debridement, B: Radiological appearance of the injury, C: Four weeks after VAC® application, removal of rejected bone grafts and further debridement, D: After six weeks of VAC® application, E: Final soft tissue reconstruction with a random transpositional fasciocutaneous flap 
Scar formation was aesthetically acceptable by the patients; however, in 4 wounds hypertrophic scars developed, and in one wound keloid formation occurred 14 weeks postoperatively. In all 5 cases triamcinolone acetonide was intralesionally injected by Dermojet (MadaJet XL, Mada Inc., Carlstadt, NJ) for three to six times at monthly intervals and was combined with silicone sheeting in order to reduce scars and relieve the itching and burning sensation that characterizes keloids.
DISCUSSION
Delayed soft tissue reconstruction of complex lower extremity injuries is advisable in medically unstable patients or in poor wound bed injuries. In this study negative pressure was used prior to soft tissue reconstruction in order to control wound exudate and produce florid granulation tissue, thus optimizing the wound bed before definite closure in high-risk patients (10, 15).
Negative pressure therapy was applied doe to the fact that it is a non-invasive method and is well tolerated by patients (3, 6, 8, 9). Although adverse events related to the use of VAC® have been reported, such as pain, infection, bleeding and surrounding skin breakdown (4), no such complication occurred during therapy in the present study.
VAC® was applied two days after the initial procedure, in order to minimize the risk of bleeding and ensure viability of tissues in the wound bed. Continuous mode was preferred to intermittent, as it causes significantly less discomfort to the patients, who experience the vacuum effect once only and for a few seconds after application. VAC® was set to 125 mm Hg, as this pressure has been found to remove excess wound fluid effectively, promote angiogenesis and entail low risk of bleeding (1, 3, 5). Some recent studies suggesting that negative pressure of 80 mm Hg is as effective; however, this pressure has been tested only with gauze (7) instead of the foam sponge interface used in the present study. Certainly it would be worth applying and evaluating the efficacy of lower negative pressure in future studies, especially in patients in high risk of bleeding.
The polyurethane sponge was stabilized by the adhesive drape included in the kit. This occlusive membrane not only protects from contamination – which is especially valuable in Intensive Care Unit patients – but also promotes healing of the areas covered by creating a moist wound environment (4).
There has been a controversy in the literature regarding bacterial bioburden reduction by the use of VAC® (4, 14). Some authors in their retrospective study of 26 wounds demonstrated that VAC® therapy had actually increased bacterial bioburden, though this was found to be irrelevant to the healing progress of wounds. This study, however, included both acute and chronic wounds assessed by punch biopsies (14).
In our study wet quantitative swab cultures, as described by Bill et al (2), were preferred to punch biopsies, as they are non-invasive and thus better tolerated by patients while found to be equally reliable. More than half the participants were ICU patients, a fact that explains the bacterial flora revealed by wound cultures. In already infected wounds, colonies of mainly multiresistant stains were discovered, and yet the wound bed was cleared during VAC® therapy. This outcome may be attributed to the fact that aggressive debridement had preceded VAC® application and all wounds were acute. Furthermore, removal of excess wound fluids most probably acts synergistically with the systemic antibacterial treatment in eradicating wound infection, an effect probably enhanced by promotion of angiogenesis induced by negative pressure (5). However, as all patients were receiving antibiotics, the pure effect of negative pressure therapy on wound bacterial bioburden could not be reliably assessed in this study.
Negative pressure in this study is not suggested as a replacement for primary soft tissue reconstruction, which is the cornerstone of plastic surgery in severe lower extremity injuries (10, 11, 13, 15, 17). However, it can be a reasonable adjunct to delayed reconstruction, when this is necessary in order to decrease morbidity associated with acute primary reconstruction. Formation of seroma, hematoma, surgical wound dehiscence, delayed healing of the donor site and decreased flap survival are not uncommon in already compromised patients.
The accelerated development of robust granulation tissue induced by VAC® protects deep structures from infection and provides a stable wound bed for grafting (3, 8). In this study skin grafted areas were found to be stable during the follow-up period even in anatomic sites notorious for recurrence of skin deficit due to repeated mechanical irritation, such as the Achilles tendon area. Should primary reconstruction have been chosen, all patients would have been managed with local, distant or free flaps (10, 13, 17).
However, when tendon autologous grafts, allografts or fixation material have to be covered, it is crucial to use flaps – either fasciocutaneous or muscular – to provide cover which is reliable in volume and well-vascularized (13).
Meticulous assessment and careful selection of patients for delayed soft tissue reconstruction in lower limb acute injuries is fundamental. The use of negative pressure is a useful adjunct that enhances the scope, reliability, effectiveness and safety of delayed reconstruction in high-risk patients.
CONCLUSION
Negative pressure is a safe and effective way of preparing complex lower extremity traumas for delayed soft tissue reconstruction in high-risk patients. The development of healthy granulation tissue minimizes the need for major conventional reconstructive operations and therefore postoperative morbidity.
Conflict of Interest and Funding
No funds were received in support of this study.Address for correspondence:
Despoina D. Kakagia, M.D., PhD, EBOPRAS
Democritus University in Thrace
7, P. Kirillou Str.
68100 Alexandroupolis
Greece
E-mail: despoinakakagia@yahoo.com
Sources
1. Argenta LC., Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann. Plast. Surg., 38, 1997, p. 563–576.
2. Bill TJ., Ratliff CR., Donovan AM. Quantitative swab culture versus tissue biopsy: a comparison in chronic wounds. Ostomy Wound Manage, 47, 2001, p. 34–37.
3. Bollero D., Carnino R., Risso D. Acute complex traumas of the lower limbs: a modern reconstructive approach with negative pressure therapy. Wound Rep. Regen., 15, 2007, p. 589–594.
4. Campbell PE. Surgical wound case studies with the Versatile 1 wound vacuum system for negative pressure wound therapy. J. Wound Ostomy Continence Nurs., 33, 2006, p. 2–10.
5. Chen SZ., Li J., Li XY. Effects of vacuum-assisted closure on wound microcirculation: an experimental study. Asian J .Surg., 28, 2005, p. 211–217.
6. DeFranzo AJ., Argenta LC., Marks MW. The use of vacuum assisted closure therapy for the treatment of lower-extremity wounds with exposed bone. Plast. Reconstr. Surg., 108, 2001, p. 1184–1191.
7. Fife CE., Walker D., Thomson B. The safety of negative pressure wound therapy using vacuum-assisted closure in diabetic foot ulcers treated in the outpatient setting. Int. Wound. J. ,5 Suppl, 2008, p. 217–222.
8. Herscovici D. Jr., Sanders RW., Scaduto JM. Vacuum-assisted wound closure (VAC therapy) for the management of patients with high energy soft tissue injuries. J. Orthop. Trauma, 17, 2003, p. 683–688.
9. Hersh RE., Jack JM., Dahman MI. The vacuum-assisted closure device as a bridge to sternal wound closure. Ann. Plast. Surg., 46, 2001, p. 250–254.
10. Hertel R., Lambert SM., Muller S. On the timing of soft-tissue reconstruction for open fractures of the lower leg. Arch. Orthop. Trauma Surg. 119 ,1999, p.7–12.
11. Katsamouris AN., Steriopoulos K., Katonis P. Limbs arterial injuries associated with limb fractures: clinical presentation, assessment and management. Eur. J. Vasc. Endovasc. Surg., 9,1995, p. 964–970.
12. Morykwas MJ., Argenta LC., Shelton-Brown EI. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann. Plast. Surg., 38, 1997, p. 553–562.
13. Stewart KJ., Wilson Y., Keating M. Suction dressing are no substitute for flap cover in acute open fractures. Br. J. Plast. Surg., 3667, 2001, p. 652–653.
14. Weed T., Ratliff C., Drake DB. Quantifying bacterial bioburden during negative pressure wound therapy. Does the wound VAC enhance bacterial clearance? Ann. Plast. Surg., 52, 2004, p. 276–280.
15. Weitz-Marshall AD, Bosse MJ. Timing of closure of open fracture. J. Am. Acad. Orthop. Surg., 10, 2002, p. 379–384.
16. Wu SH., Zecha PJ., Feits R. Vacuum therapy as an intermediate phase in wound closure: a clinical experience. Eur. J. Plast. Surg., 23, 2000, p. 174–177.
17. Zalavras CG., Patzakidis MJ. Open fractures: evaluation and management. J. Am. Acad. Orthop. Surg., 11, 2003, p. 212–219.
Labels
Plastic surgery Orthopaedics Burns medicine Traumatology
Article was published inActa chirurgiae plasticae

2009 Issue 3-4-
All articles in this issue
- VACUUM-ASSISTED CLOSURE DOWNGRADES RECONSTRUCTIVE DEMANDS IN HIGH-RISK PATIENTS WITH SEVERE LOWER EXTREMITY INJURIES
- CORRELATION BETWEEN COMPLICATION RATE AND PERIOPERATIVE RISK-FACTORS IN SUPERIOR PEDICLE REDUCTION MAMMAPLASTY: OUR EXPERIENCE IN 127 PATIENTS
- ONE-YEAR EXPERIENCE WITH TIGECYCLINE IN TREATING SERIOUS INFECTIONS IN SEVERELY BURNED PATIENTS
- BREAST DESMOID TUMOR AFTER AUGMENTATION MAMMOPLASTY: TWO CASE REPORTS
- FREE LATISSIMUS DORSI MUSCLE FLAP FOR CHRONIC BRONCHOPLEURAL FISTULA
- UNSUCCESSFUL THERAPY OF COMBINED MYCOTIC INFECTION IN A SEVERELY BURNED PATIENT: A CASE STUDY
- THE HISTORY OF CLEFT LIP OPERATIONS AT THE DEPARTMENT OF PLASTIC SURGERY IN PRAGUE
- THE HISTORY OF CLEFT PALATE SURGERY AT THE DEPARTMENT OF PLASTIC SURGERY IN PRAGUE
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- Online only
- About the journal
Most read in this issue- BREAST DESMOID TUMOR AFTER AUGMENTATION MAMMOPLASTY: TWO CASE REPORTS
- VACUUM-ASSISTED CLOSURE DOWNGRADES RECONSTRUCTIVE DEMANDS IN HIGH-RISK PATIENTS WITH SEVERE LOWER EXTREMITY INJURIES
- THE HISTORY OF CLEFT PALATE SURGERY AT THE DEPARTMENT OF PLASTIC SURGERY IN PRAGUE
- UNSUCCESSFUL THERAPY OF COMBINED MYCOTIC INFECTION IN A SEVERELY BURNED PATIENT: A CASE STUDY
Login#ADS_BOTTOM_SCRIPTS#Forgotten passwordEnter the email address that you registered with. We will send you instructions on how to set a new password.
- Career

